A Multi national Multi institutional Study Comparing Efficacy


- Slides: 19

A Multi national, Multi institutional Study Comparing Efficacy of Stereotactic Body Radiation Therapy and Radiofrequency Ablation for Hepatocellular Carcinoma 1 Jinsil Seong**, 1 Nalee Kim, 2 Jason Cheng, 3 Wen Yen Huang, 4 Tomoki Kimura, 5 Victor HF Lee, 6 Zhao Chong Zeng, 7 Chul Seung Kay 1 Yonsei Cancer Center, Yonsei University College of Medicine, Republic of Korea 2 National Taiwan University Hospital, Taiwan 3 Tri-Service General Hospital, Taiwan 4 Hiroshima University Hospital, Japan 5 The University of Hong Kong, Hong Kong 6 Zhongshan Hospital, Fudan University, China 7 Incheon St. Mary Hospital, Republic of Korea 13 th Annual Conference of International Liver Cancer Association 20 -22 September 2019, Chicago, USA
DISCLOSURE i. Research funding from Accuray Inc.
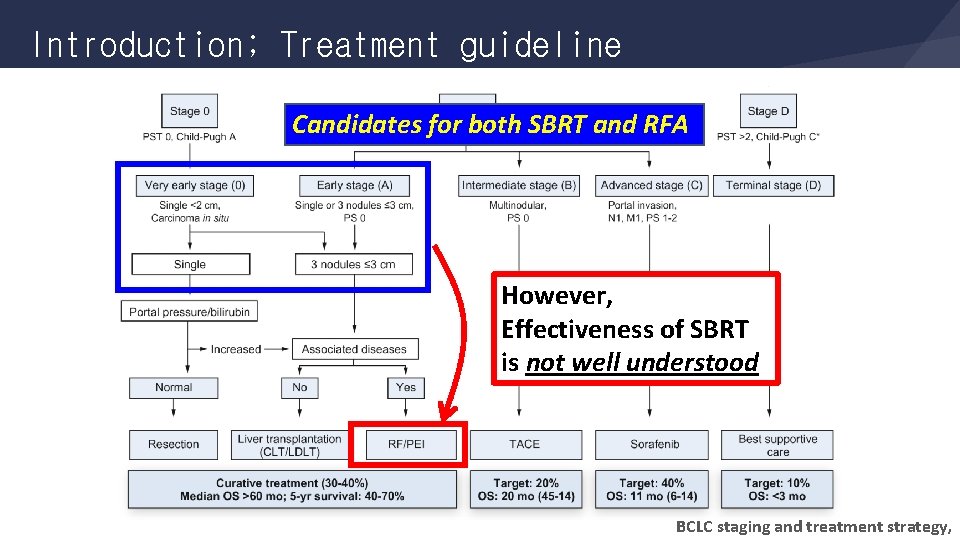
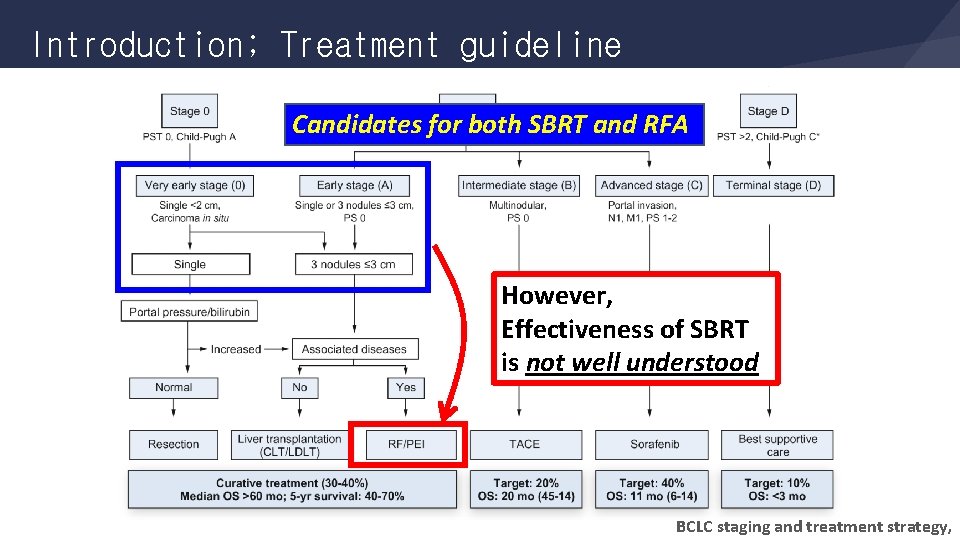
Introduction; Treatment guideline Candidates for both SBRT and RFA However, Effectiveness of SBRT is not well understood BCLC staging and treatment strategy,
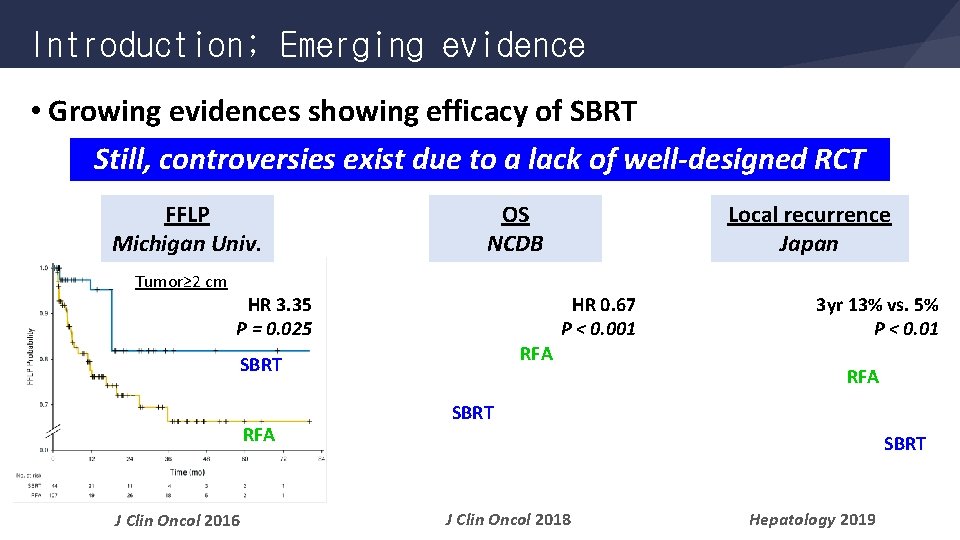
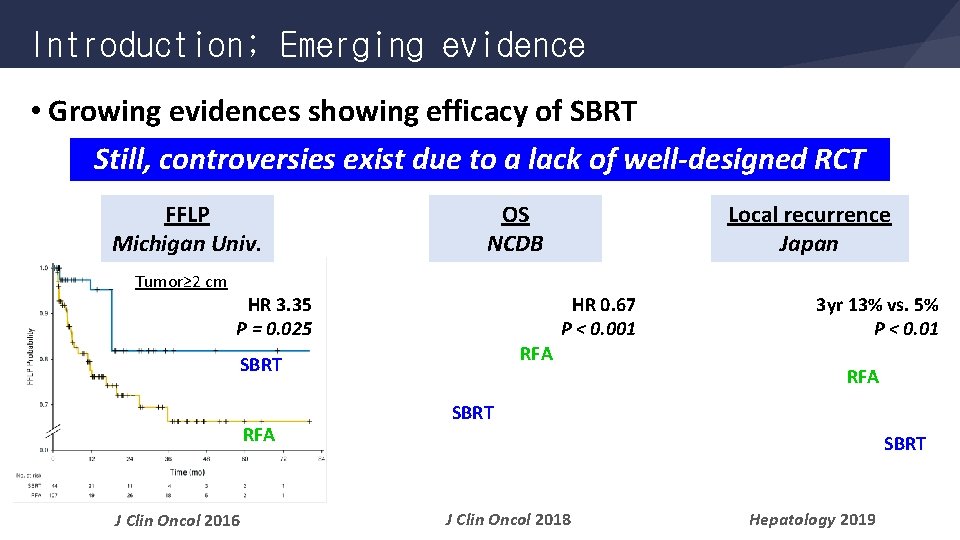
Introduction; Emerging evidence • Growing evidences showing efficacy of SBRT Still, controversies exist due to a lack of well-designed RCT FFLP Michigan Univ. Tumor≥ 2 cm HR 0. 67 P < 0. 001 HR 3. 35 P = 0. 025 RFA SBRT RFA J Clin Oncol 2016 Local recurrence Japan OS NCDB 3 yr 13% vs. 5% P < 0. 01 RFA SBRT J Clin Oncol 2018 Hepatology 2019
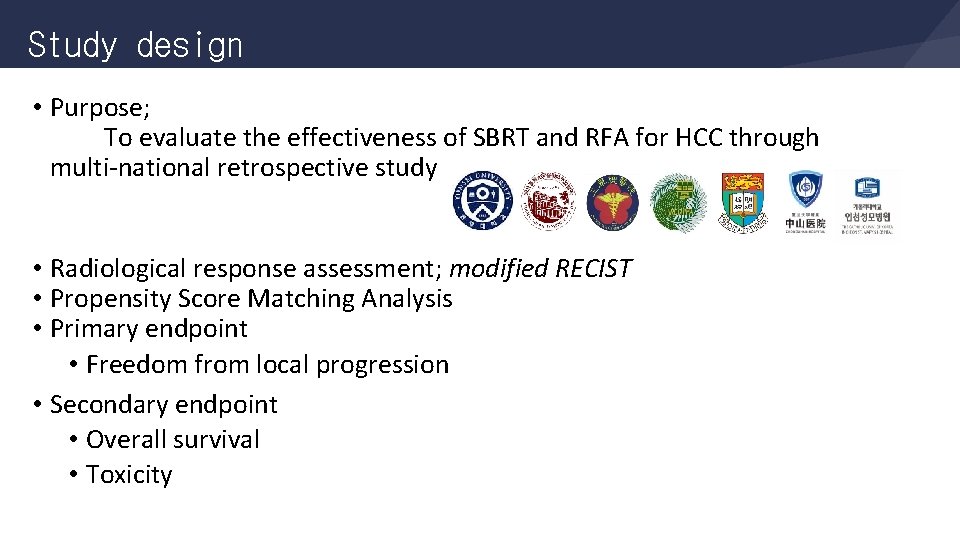
Study design • Purpose; To evaluate the effectiveness of SBRT and RFA for HCC through multi-national retrospective study • Radiological response assessment; modified RECIST • Propensity Score Matching Analysis • Primary endpoint • Freedom from local progression • Secondary endpoint • Overall survival • Toxicity
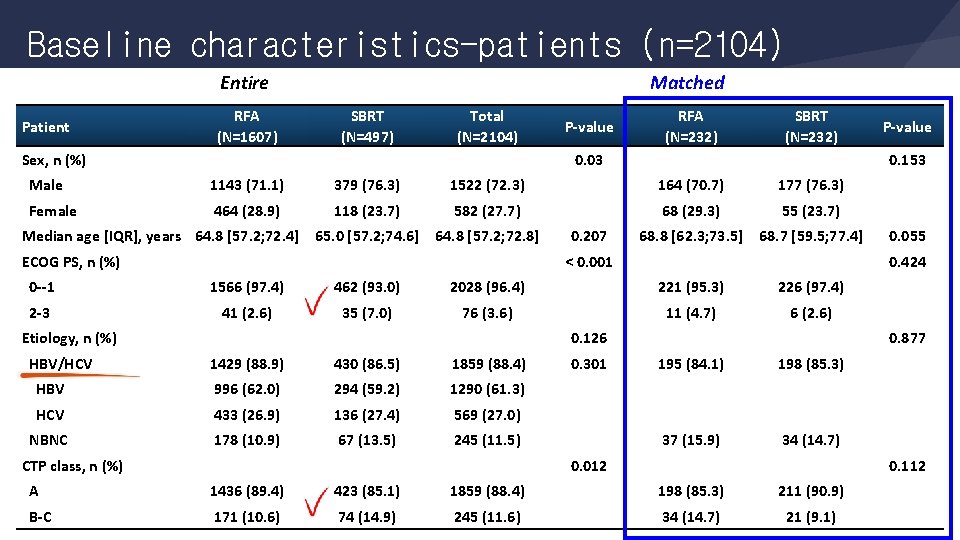
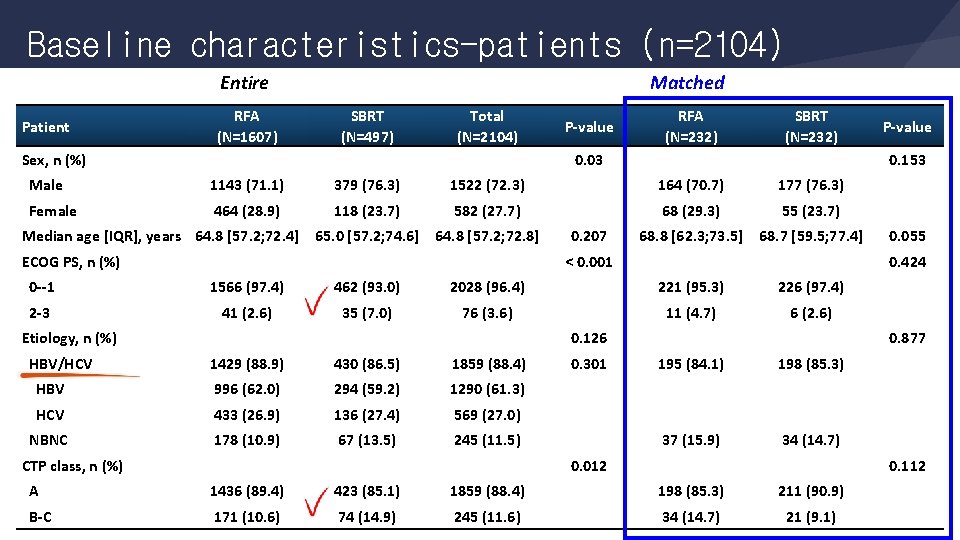
Baseline characteristics-patients (n=2104) Entire Patient RFA (N=1607) Matched SBRT (N=497) Total (N=2104) Sex, n (%) P value RFA (N=232) SBRT (N=232) 0. 03 0. 153 Male 1143 (71. 1) 379 (76. 3) 1522 (72. 3) 164 (70. 7) 177 (76. 3) Female 464 (28. 9) 118 (23. 7) 582 (27. 7) 68 (29. 3) 55 (23. 7) 65. 0 [57. 2; 74. 6] 64. 8 [57. 2; 72. 8] 68. 8 [62. 3; 73. 5] 68. 7 [59. 5; 77. 4] Median age [IQR], years 64. 8 [57. 2; 72. 4] ECOG PS, n (%) 0. 207 < 0. 001 1566 (97. 4) 462 (93. 0) 2028 (96. 4) 221 (95. 3) 226 (97. 4) 2 3 41 (2. 6) 35 (7. 0) 76 (3. 6) 11 (4. 7) 6 (2. 6) 0. 126 HBV/HCV 1429 (88. 9) 430 (86. 5) 1859 (88. 4) HBV 996 (62. 0) 294 (59. 2) 1290 (61. 3) HCV 433 (26. 9) 136 (27. 4) 569 (27. 0) NBNC 178 (10. 9) 67 (13. 5) 245 (11. 5) CTP class, n (%) 0. 301 0. 055 0. 424 0 1 Etiology, n (%) P value 0. 877 195 (84. 1) 198 (85. 3) 37 (15. 9) 34 (14. 7) 0. 012 0. 112 A 1436 (89. 4) 423 (85. 1) 1859 (88. 4) 198 (85. 3) 211 (90. 9) B C 171 (10. 6) 74 (14. 9) 245 (11. 6) 34 (14. 7) 21 (9. 1)
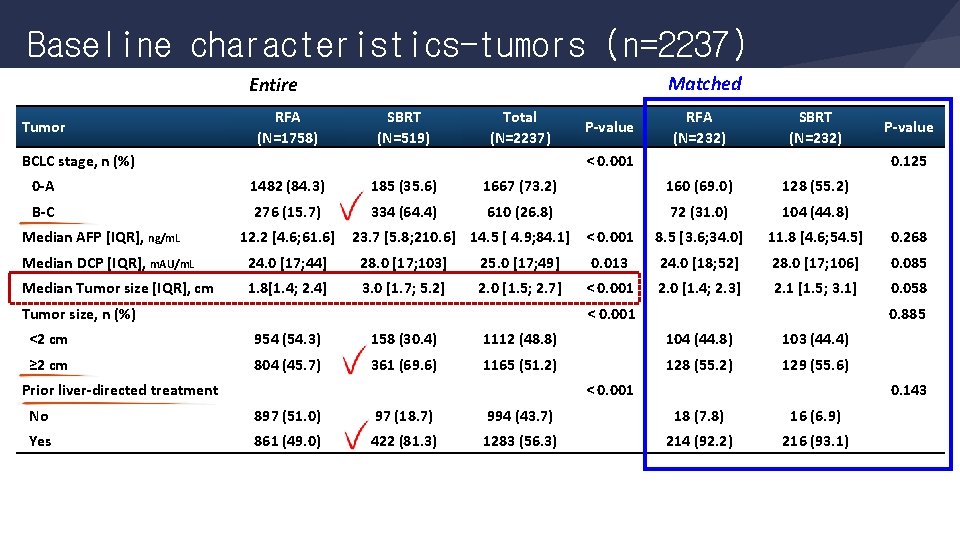
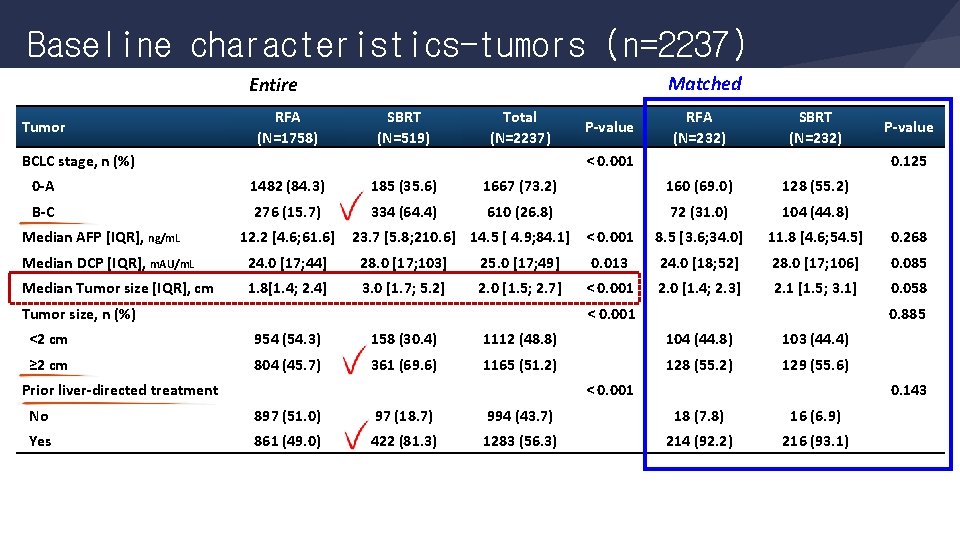
Baseline characteristics-tumors (n=2237) Matched Entire Tumor RFA (N=1758) SBRT (N=519) Total (N=2237) BCLC stage, n (%) P value RFA (N=232) SBRT (N=232) < 0. 001 P value 0. 125 0 A 1482 (84. 3) 185 (35. 6) 1667 (73. 2) 160 (69. 0) 128 (55. 2) B C 276 (15. 7) 334 (64. 4) 610 (26. 8) 72 (31. 0) 104 (44. 8) 8. 5 [3. 6; 34. 0] 11. 8 [4. 6; 54. 5] 0. 268 Median AFP [IQR], ng/m. L 12. 2 [4. 6; 61. 6] Median DCP [IQR], m. AU/m. L 24. 0 [17; 44] 28. 0 [17; 103] 25. 0 [17; 49] 0. 013 24. 0 [18; 52] 28. 0 [17; 106] 0. 085 Median Tumor size [IQR], cm 1. 8[1. 4; 2. 4] 3. 0 [1. 7; 5. 2] 2. 0 [1. 5; 2. 7] < 0. 001 2. 0 [1. 4; 2. 3] 2. 1 [1. 5; 3. 1] 0. 058 < 0. 001 0. 885 <2 cm 954 (54. 3) 158 (30. 4) 1112 (48. 8) 104 (44. 8) 103 (44. 4) ≥ 2 cm 804 (45. 7) 361 (69. 6) 1165 (51. 2) 128 (55. 2) 129 (55. 6) No 897 (51. 0) 97 (18. 7) 994 (43. 7) 18 (7. 8) 16 (6. 9) Yes 861 (49. 0) 422 (81. 3) 1283 (56. 3) 214 (92. 2) 216 (93. 1) Tumor size, n (%) Prior liver directed treatment 23. 7 [5. 8; 210. 6] 14. 5 [ 4. 9; 84. 1] < 0. 001 0. 143
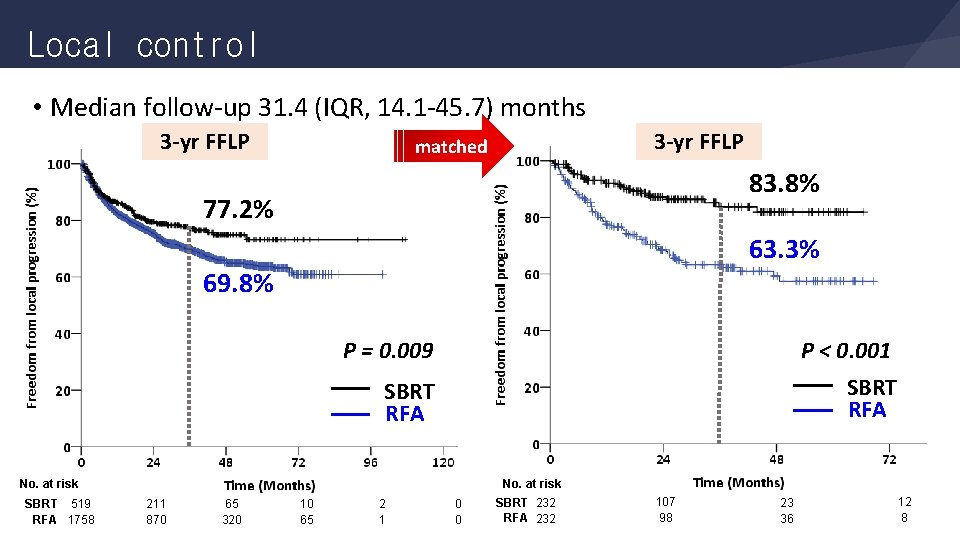
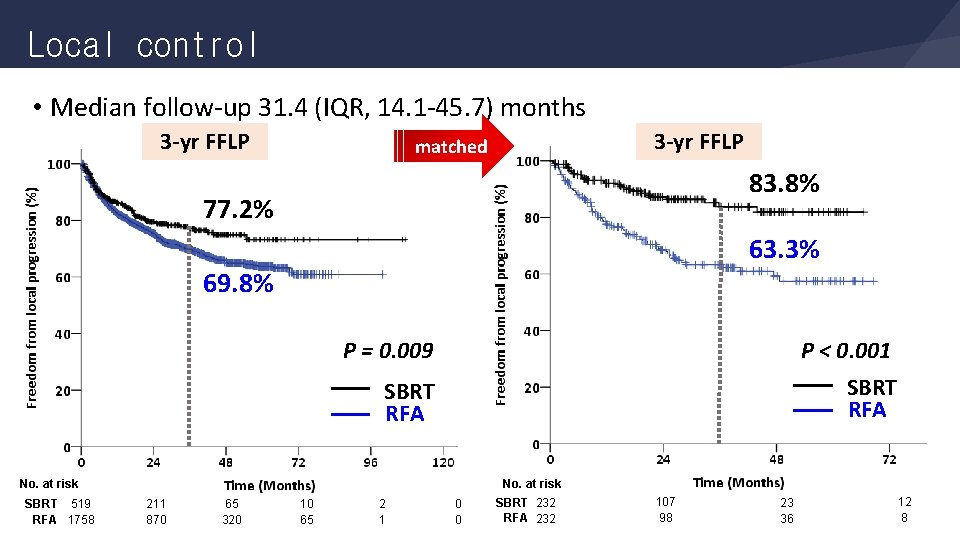
Local control • Median follow-up 31. 4 (IQR, 14. 1 -45. 7) months 3 yr FFLP matched 83. 8% 77. 2% 63. 3% 69. 8% P = 0. 009 P < 0. 001 SBRT RFA No. at risk SBRT 519 RFA 1758 211 870 65 320 10 65 2 1 0 0 SBRT 232 RFA 232 107 98 23 36 12 8
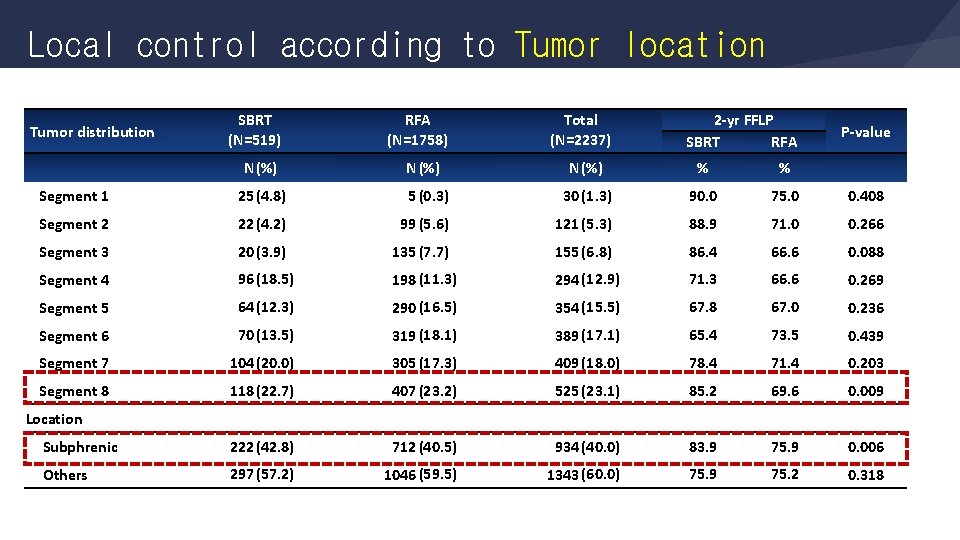
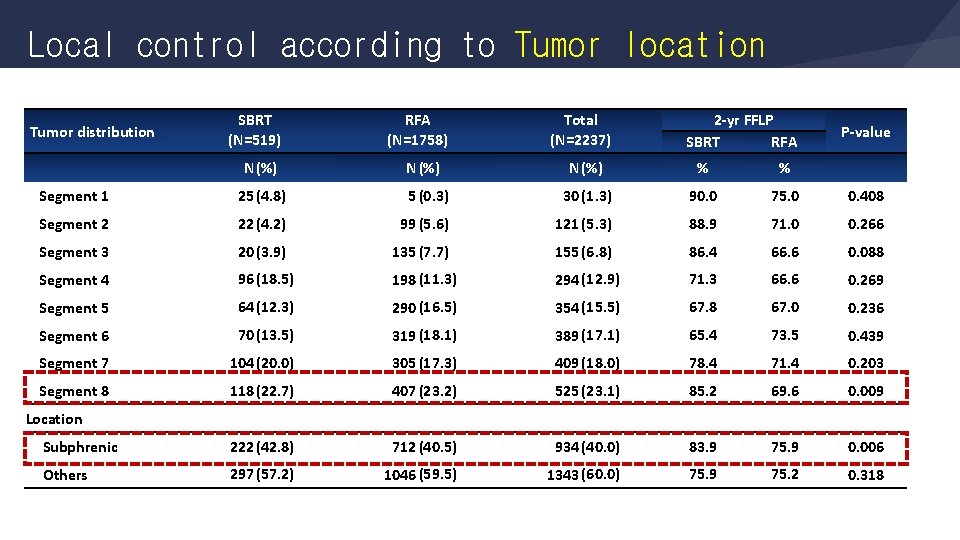
Local control according to Tumor location Tumor distribution SBRT (N=519) N(%) RFA (N=1758) N (%) Total (N=2237) 2 yr FFLP SBRT RFA N (%) % % P value Segment 1 25(4. 8) 5 (0. 3) 30 (1. 3) 90. 0 75. 0 0. 408 Segment 2 22(4. 2) 99 (5. 6) 121 (5. 3) 88. 9 71. 0 0. 266 Segment 3 20(3. 9) 135 (7. 7) 155 (6. 8) 86. 4 66. 6 0. 088 Segment 4 96(18. 5) 198 (11. 3) 294 (12. 9) 71. 3 66. 6 0. 269 Segment 5 64(12. 3) 290 (16. 5) 354 (15. 5) 67. 8 67. 0 0. 236 Segment 6 70(13. 5) 319 (18. 1) 389 (17. 1) 65. 4 73. 5 0. 439 Segment 7 104(20. 0) 305 (17. 3) 409 (18. 0) 78. 4 71. 4 0. 203 Segment 8 118(22. 7) 407 (23. 2) 525 (23. 1) 85. 2 69. 6 0. 009 Subphrenic 222(42. 8) 712 (40. 5) 934 (40. 0) 83. 9 75. 9 0. 006 Others 297(57. 2) 1046 (59. 5) 1343 (60. 0) 75. 9 75. 2 0. 318 Location
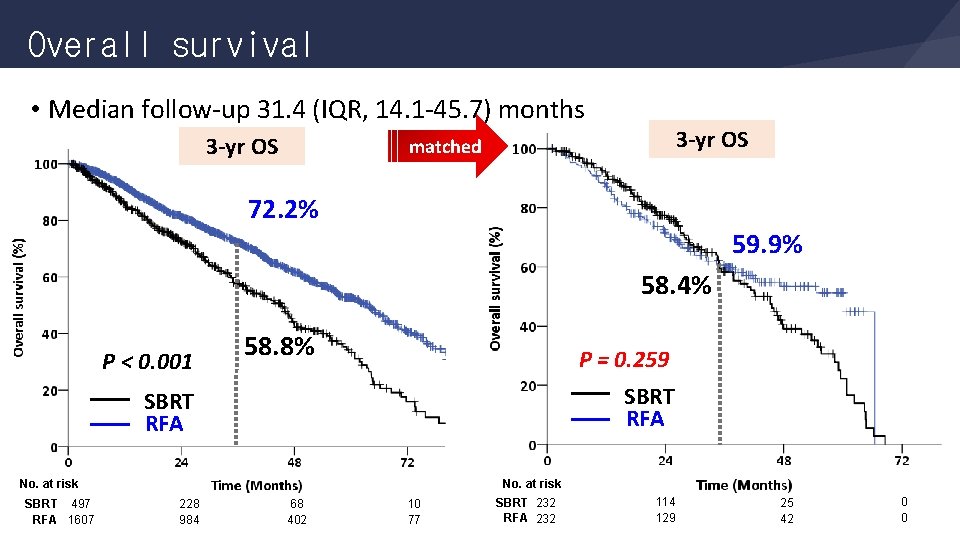
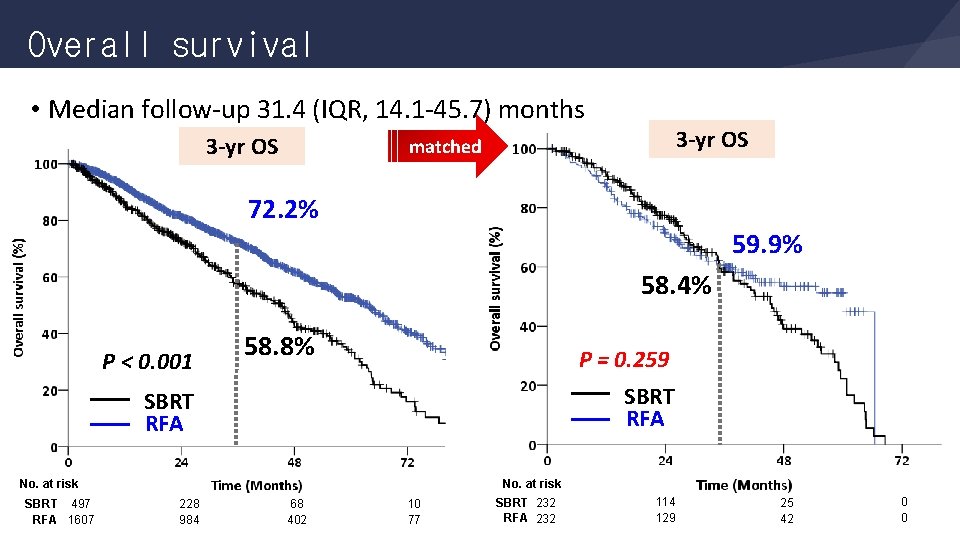
Overall survival • Median follow-up 31. 4 (IQR, 14. 1 -45. 7) months 3 yr OS matched 72. 2% 59. 9% 58. 4% P < 0. 001 58. 8% P = 0. 259 SBRT RFA No. at risk SBRT 497 RFA 1607 228 984 68 402 10 77 SBRT 232 RFA 232 114 129 25 42 0 0
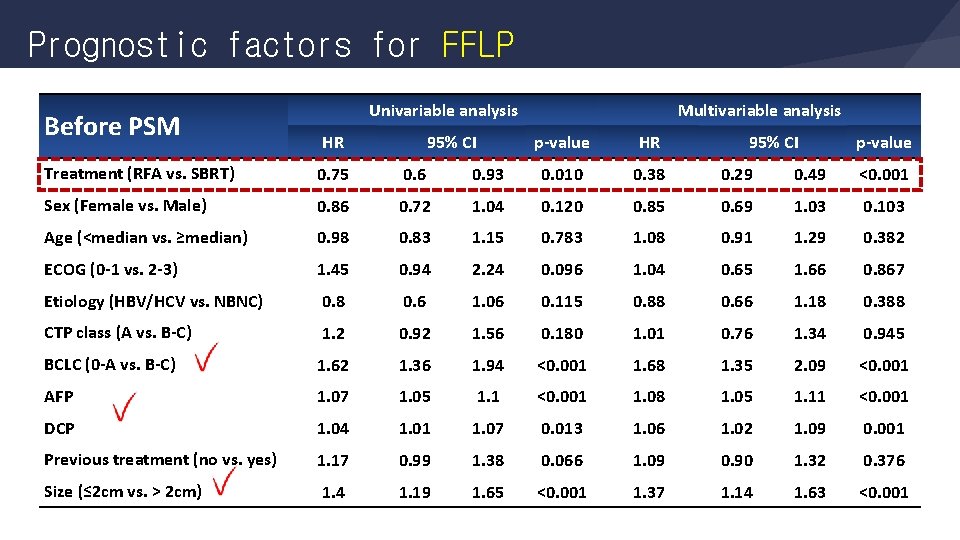
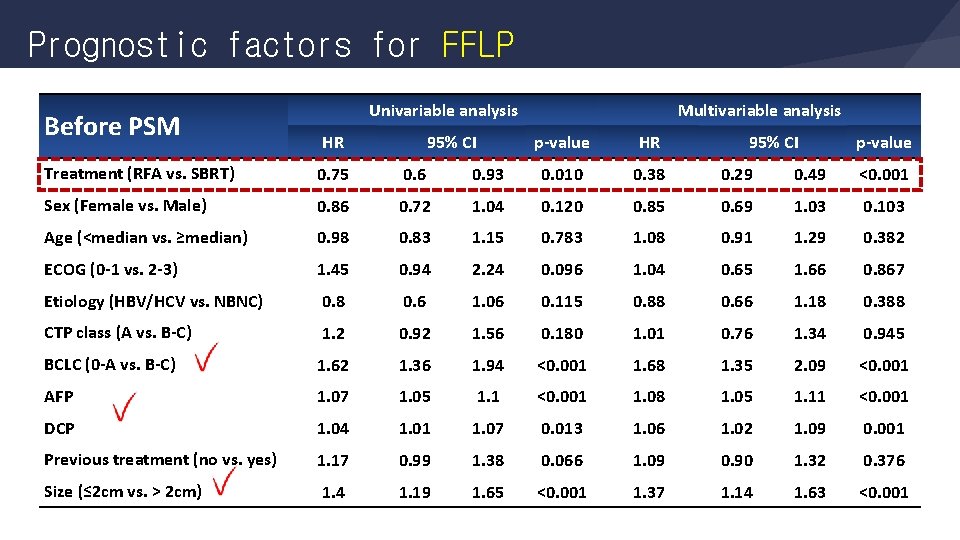
Prognostic factors for FFLP Before PSM Univariable analysis HR 95% CI Multivariable analysis p value HR 95% CI p value Treatment (RFA vs. SBRT) 0. 75 0. 6 0. 93 0. 010 0. 38 0. 29 0. 49 <0. 001 Sex (Female vs. Male) 0. 86 0. 72 1. 04 0. 120 0. 85 0. 69 1. 03 0. 103 Age (<median vs. ≥median) 0. 98 0. 83 1. 15 0. 783 1. 08 0. 91 1. 29 0. 382 ECOG (0 1 vs. 2 3) 1. 45 0. 94 2. 24 0. 096 1. 04 0. 65 1. 66 0. 867 Etiology (HBV/HCV vs. NBNC) 0. 8 0. 6 1. 06 0. 115 0. 88 0. 66 1. 18 0. 388 CTP class (A vs. B C) 1. 2 0. 92 1. 56 0. 180 1. 01 0. 76 1. 34 0. 945 BCLC (0 A vs. B C) 1. 62 1. 36 1. 94 <0. 001 1. 68 1. 35 2. 09 <0. 001 AFP 1. 07 1. 05 1. 1 <0. 001 1. 08 1. 05 1. 11 <0. 001 DCP 1. 04 1. 01 1. 07 0. 013 1. 06 1. 02 1. 09 0. 001 Previous treatment (no vs. yes) 1. 17 0. 99 1. 38 0. 066 1. 09 0. 90 1. 32 0. 376 Size (≤ 2 cm vs. > 2 cm) 1. 4 1. 19 1. 65 <0. 001 1. 37 1. 14 1. 63 <0. 001
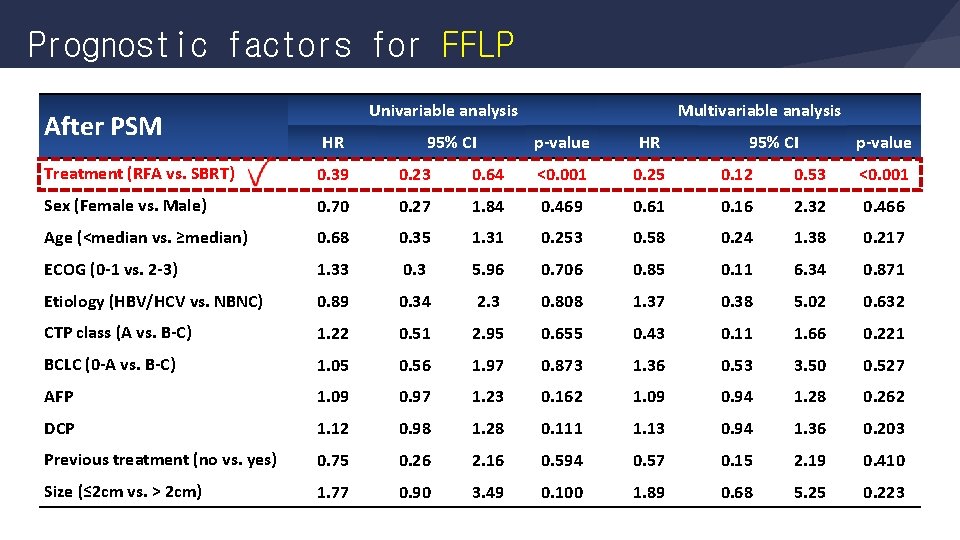
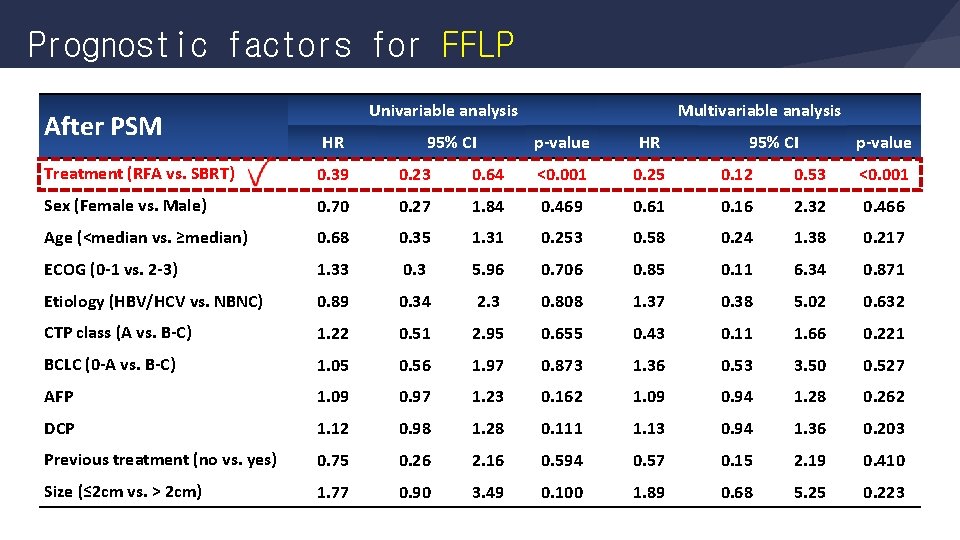
Prognostic factors for FFLP After PSM Univariable analysis HR 95% CI Multivariable analysis p value HR 95% CI p value Treatment (RFA vs. SBRT) 0. 39 0. 23 0. 64 <0. 001 0. 25 0. 12 0. 53 <0. 001 Sex (Female vs. Male) 0. 70 0. 27 1. 84 0. 469 0. 61 0. 16 2. 32 0. 466 Age (<median vs. ≥median) 0. 68 0. 35 1. 31 0. 253 0. 58 0. 24 1. 38 0. 217 ECOG (0 1 vs. 2 3) 1. 33 0. 3 5. 96 0. 706 0. 85 0. 11 6. 34 0. 871 Etiology (HBV/HCV vs. NBNC) 0. 89 0. 34 2. 3 0. 808 1. 37 0. 38 5. 02 0. 632 CTP class (A vs. B C) 1. 22 0. 51 2. 95 0. 655 0. 43 0. 11 1. 66 0. 221 BCLC (0 A vs. B C) 1. 05 0. 56 1. 97 0. 873 1. 36 0. 53 3. 50 0. 527 AFP 1. 09 0. 97 1. 23 0. 162 1. 09 0. 94 1. 28 0. 262 DCP 1. 12 0. 98 1. 28 0. 111 1. 13 0. 94 1. 36 0. 203 Previous treatment (no vs. yes) 0. 75 0. 26 2. 16 0. 594 0. 57 0. 15 2. 19 0. 410 Size (≤ 2 cm vs. > 2 cm) 1. 77 0. 90 3. 49 0. 100 1. 89 0. 68 5. 25 0. 223
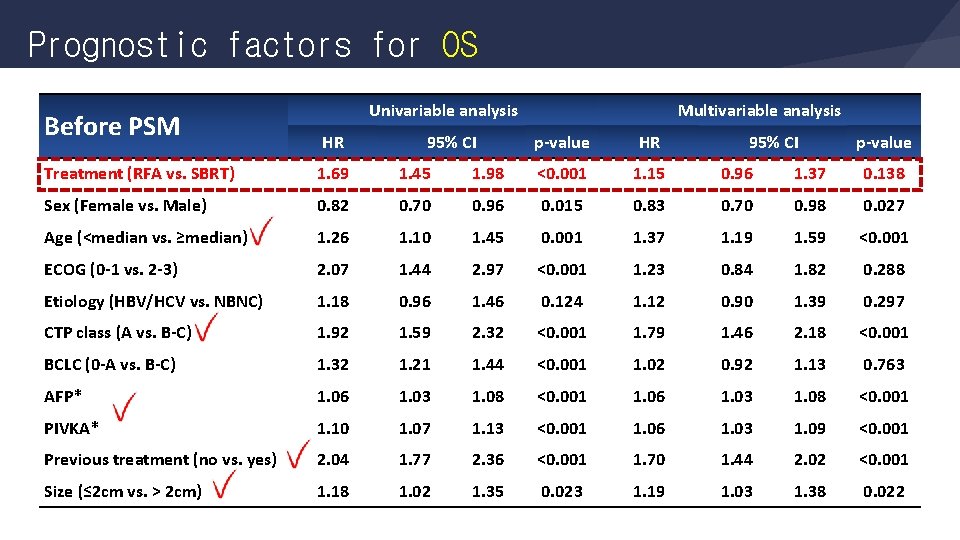
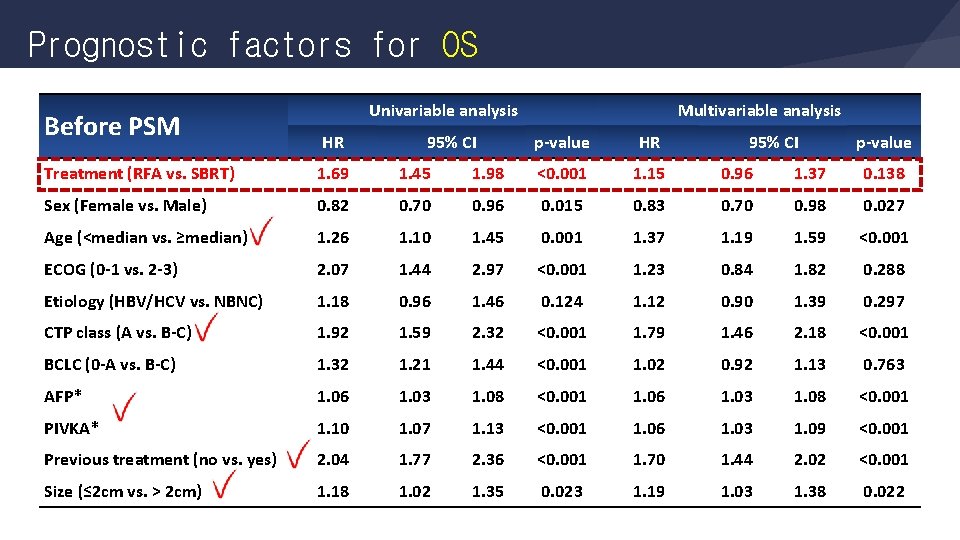
Prognostic factors for OS Before PSM Univariable analysis HR 95% CI Multivariable analysis p value HR 95% CI p value Treatment (RFA vs. SBRT) 1. 69 1. 45 1. 98 <0. 001 1. 15 0. 96 1. 37 0. 138 Sex (Female vs. Male) 0. 82 0. 70 0. 96 0. 015 0. 83 0. 70 0. 98 0. 027 Age (<median vs. ≥median) 1. 26 1. 10 1. 45 0. 001 1. 37 1. 19 1. 59 <0. 001 ECOG (0 1 vs. 2 3) 2. 07 1. 44 2. 97 <0. 001 1. 23 0. 84 1. 82 0. 288 Etiology (HBV/HCV vs. NBNC) 1. 18 0. 96 1. 46 0. 124 1. 12 0. 90 1. 39 0. 297 CTP class (A vs. B C) 1. 92 1. 59 2. 32 <0. 001 1. 79 1. 46 2. 18 <0. 001 BCLC (0 A vs. B C) 1. 32 1. 21 1. 44 <0. 001 1. 02 0. 92 1. 13 0. 763 AFP* 1. 06 1. 03 1. 08 <0. 001 PIVKA* 1. 10 1. 07 1. 13 <0. 001 1. 06 1. 03 1. 09 <0. 001 Previous treatment (no vs. yes) 2. 04 1. 77 2. 36 <0. 001 1. 70 1. 44 2. 02 <0. 001 Size (≤ 2 cm vs. > 2 cm) 1. 18 1. 02 1. 35 0. 023 1. 19 1. 03 1. 38 0. 022
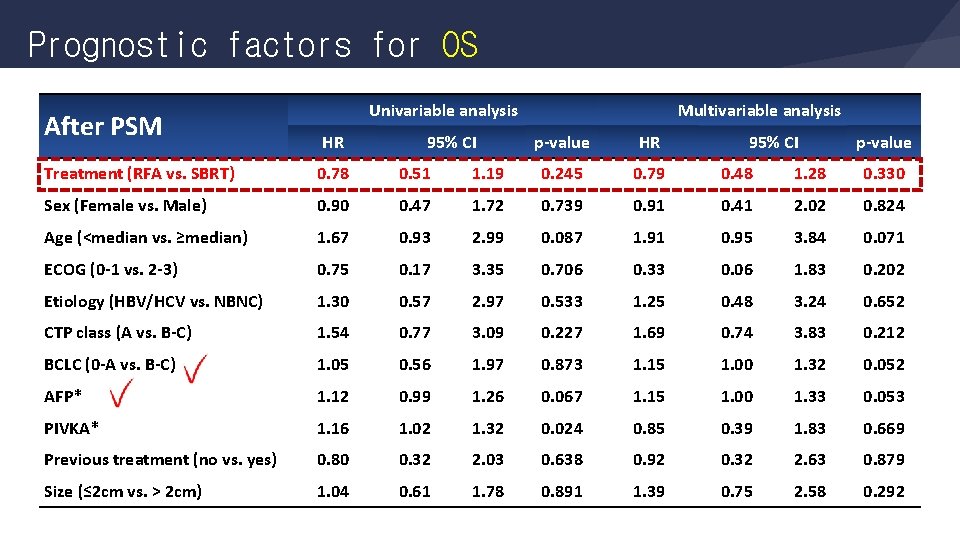
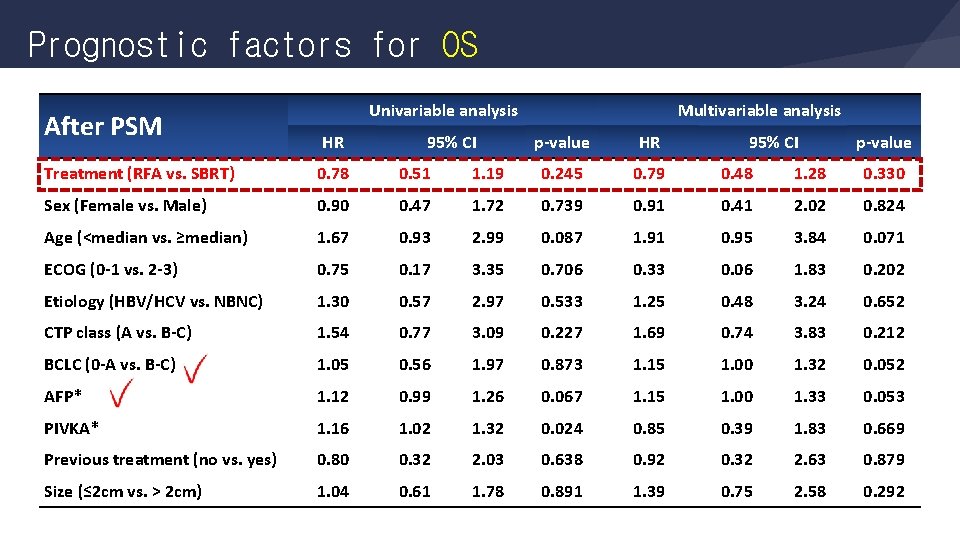
Prognostic factors for OS After PSM Univariable analysis HR 95% CI Multivariable analysis p value HR 95% CI p value Treatment (RFA vs. SBRT) 0. 78 0. 51 1. 19 0. 245 0. 79 0. 48 1. 28 0. 330 Sex (Female vs. Male) 0. 90 0. 47 1. 72 0. 739 0. 91 0. 41 2. 02 0. 824 Age (<median vs. ≥median) 1. 67 0. 93 2. 99 0. 087 1. 91 0. 95 3. 84 0. 071 ECOG (0 1 vs. 2 3) 0. 75 0. 17 3. 35 0. 706 0. 33 0. 06 1. 83 0. 202 Etiology (HBV/HCV vs. NBNC) 1. 30 0. 57 2. 97 0. 533 1. 25 0. 48 3. 24 0. 652 CTP class (A vs. B C) 1. 54 0. 77 3. 09 0. 227 1. 69 0. 74 3. 83 0. 212 BCLC (0 A vs. B C) 1. 05 0. 56 1. 97 0. 873 1. 15 1. 00 1. 32 0. 052 AFP* 1. 12 0. 99 1. 26 0. 067 1. 15 1. 00 1. 33 0. 053 PIVKA* 1. 16 1. 02 1. 32 0. 024 0. 85 0. 39 1. 83 0. 669 Previous treatment (no vs. yes) 0. 80 0. 32 2. 03 0. 638 0. 92 0. 32 2. 63 0. 879 Size (≤ 2 cm vs. > 2 cm) 1. 04 0. 61 1. 78 0. 891 1. 39 0. 75 2. 58 0. 292
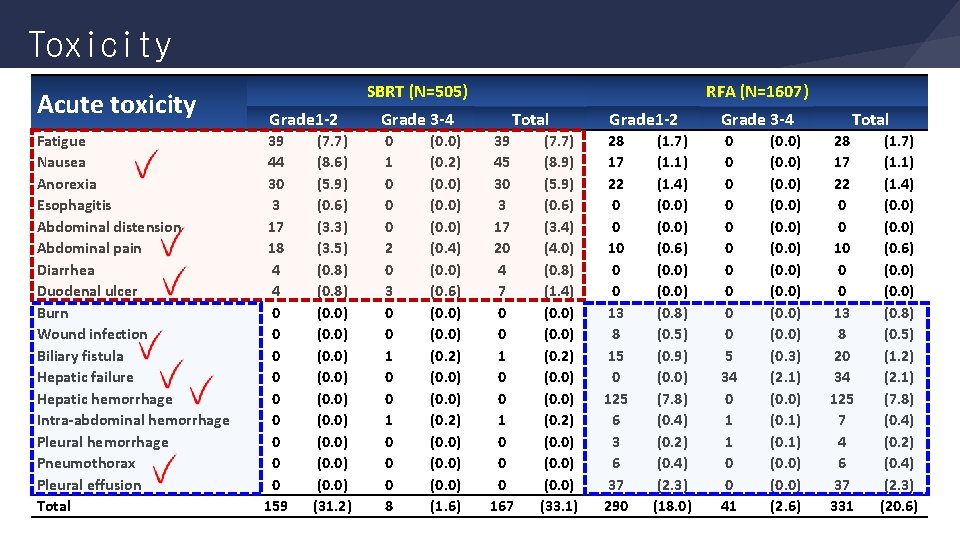
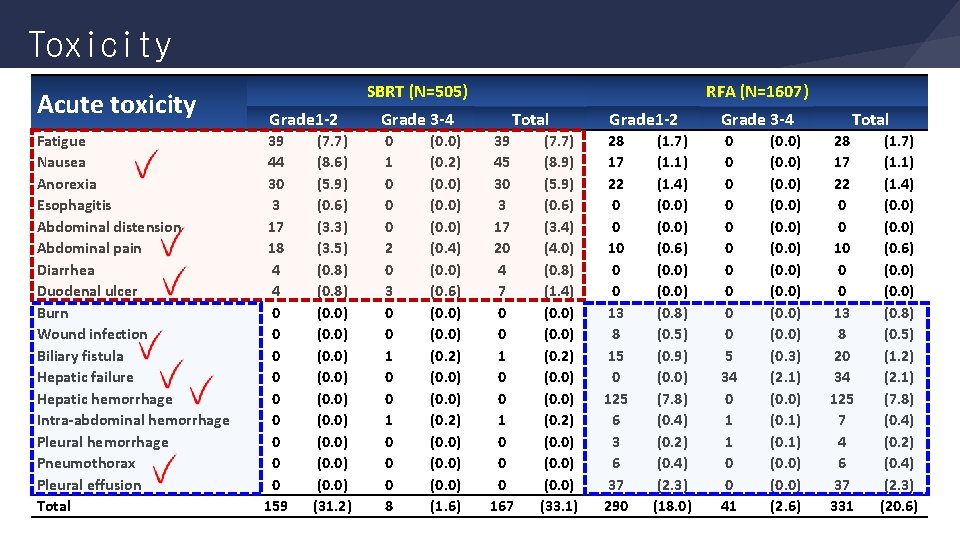
Toxicity Acute toxicity Fatigue Nausea Anorexia Esophagitis Abdominal distension Abdominal pain Diarrhea Duodenal ulcer Burn Wound infection Biliary fistula Hepatic failure Hepatic hemorrhage Intra abdominal hemorrhage Pleural hemorrhage Pneumothorax Pleural effusion Total SBRT (N=505) Grade 1 2 39 44 30 3 17 18 4 4 0 0 0 0 0 159 (7. 7) (8. 6) (5. 9) (0. 6) (3. 3) (3. 5) (0. 8) (0. 0) (0. 0) (31. 2) Grade 3 4 0 1 0 0 0 2 0 3 0 0 1 0 0 0 8 (0. 0) (0. 2) (0. 0) (0. 4) (0. 0) (0. 6) (0. 0) (0. 2) (0. 0) (1. 6) RFA (N=1607) Total 39 45 30 3 17 20 4 7 0 0 1 0 0 0 167 (7. 7) (8. 9) (5. 9) (0. 6) (3. 4) (4. 0) (0. 8) (1. 4) (0. 0) (0. 2) (0. 0) (33. 1) Grade 1 2 28 17 22 0 0 10 0 0 13 8 15 0 125 6 37 290 (1. 7) (1. 1) (1. 4) (0. 0) (0. 6) (0. 0) (0. 8) (0. 5) (0. 9) (0. 0) (7. 8) (0. 4) (0. 2) (0. 4) (2. 3) (18. 0) Grade 3 4 0 0 0 0 0 5 34 0 1 1 0 0 41 (0. 0) (0. 3) (2. 1) (0. 0) (0. 1) (0. 0) (2. 6) Total 28 17 22 0 0 10 0 0 13 8 20 34 125 7 4 6 37 331 (1. 7) (1. 1) (1. 4) (0. 0) (0. 6) (0. 0) (0. 8) (0. 5) (1. 2) (2. 1) (7. 8) (0. 4) (0. 2) (0. 4) (2. 3) (20. 6)
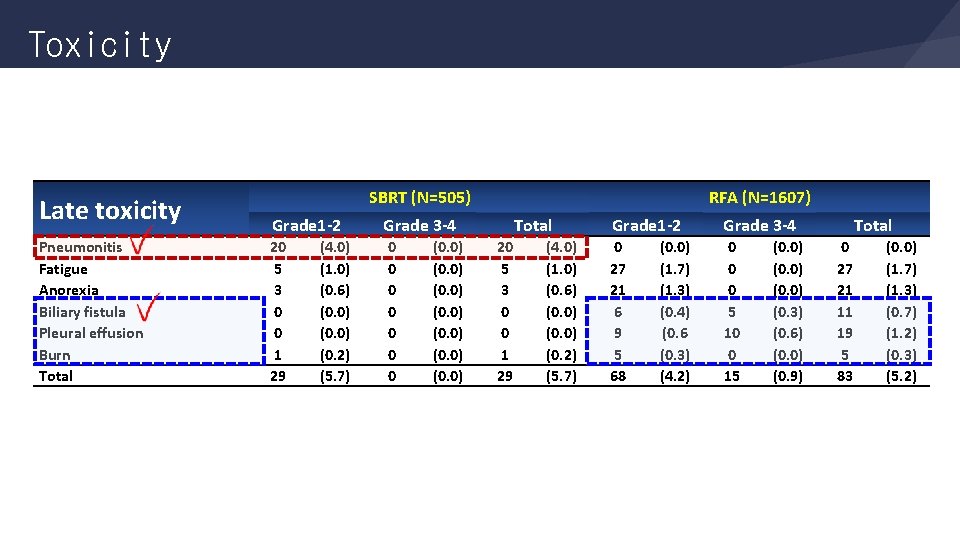
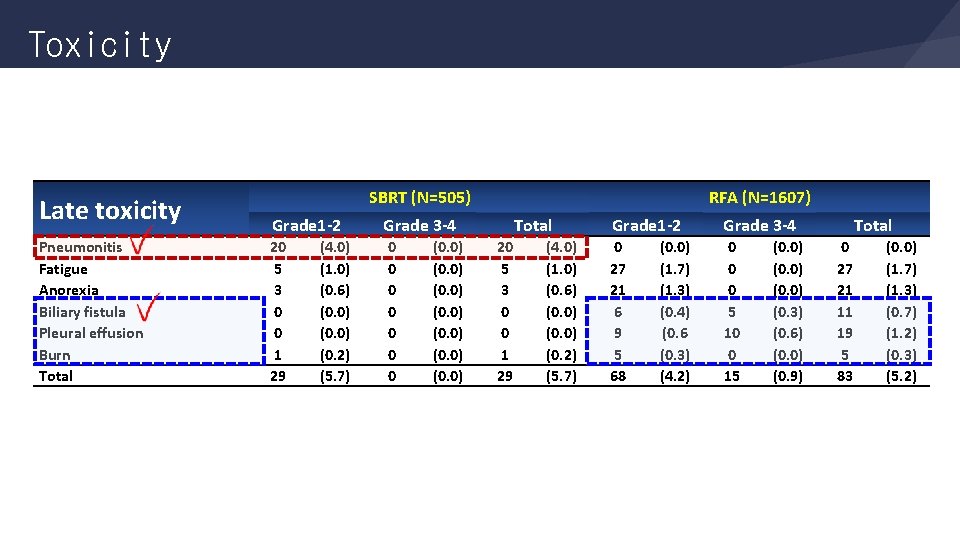
Toxicity Late toxicity Pneumonitis Fatigue Anorexia Biliary fistula Pleural effusion Burn Total SBRT (N=505) Grade 1 2 Grade 3 4 20 5 3 0 0 1 29 0 0 0 0 (4. 0) (1. 0) (0. 6) (0. 0) (0. 2) (5. 7) (0. 0) (0. 0) RFA (N=1607) Total 20 5 3 0 0 1 29 (4. 0) (1. 0) (0. 6) (0. 0) (0. 2) (5. 7) Grade 1 2 Grade 3 4 0 27 21 6 9 5 68 0 0 0 5 10 0 15 (0. 0) (1. 7) (1. 3) (0. 4) (0. 6 (0. 3) (4. 2) (0. 0) (0. 3) (0. 6) (0. 0) (0. 9) Total 0 27 21 11 19 5 83 (0. 0) (1. 7) (1. 3) (0. 7) (1. 2) (0. 3) (5. 2)
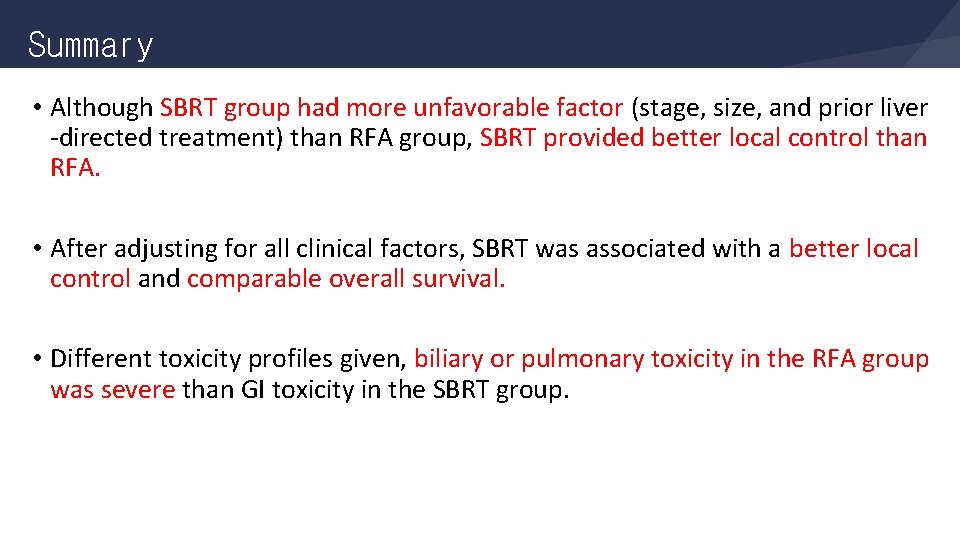
Summary • Although SBRT group had more unfavorable factor (stage, size, and prior liver -directed treatment) than RFA group, SBRT provided better local control than RFA. • After adjusting for all clinical factors, SBRT was associated with a better local control and comparable overall survival. • Different toxicity profiles given, biliary or pulmonary toxicity in the RFA group was severe than GI toxicity in the SBRT group.
Conclusion • Both SBRT and RFA could achieve comparable local control for localized inoperable HCC. • SBRT could be an effective alternative treatment modality when RFA is not feasible due to tumor location or size.

Acknowledgement Radiation Oncology - Jinsil Seong (MD, PI) Internal Medicine - Kwang-Hyub Han (Pf) - Do Young Kim (Pf) Intervention Radiology - Jong Yun Won (Pf) Dr. Jason Cheng Dr. Wen Yen Huang Dr. Tomoki Kimura Dr. Victor HF Lee Dr. Zhao Chong Zeng Dr. Chul Seung Kay