Pharmacodynamics cont Graded Doseresponse Relationships Agonist drugs mimic
- Slides: 21
Pharmacodynamics (cont. )
• Graded Dose-response Relationships • Agonist drugs mimic the action of the original endogenous ligand for the receptor (for example, isoproterenol mimics norepinephrine on β 1 receptors of the heart). The magnitude of the drug effect depends on the drug concentration at the receptor site, which, in turn, is determined by both the dose of drug administered and by the drug’s pharmacokinetic profile, such as rate of absorption, distribution, metabolism, and elimination. • As the concentration of a drug increases, its pharmacologic effect also gradually increases until all the receptors are occupied (the maximum effect). When the response of a particular receptoreffector system is measured against increasing concentrations of a drug, the graph of the response versus the drug concentration or dose is called a graded dose-response curve. The curve can be described as a rectangular hyperbola. Two important properties of drugs, potency and efficacy, can be determined by graded dose– response curves.
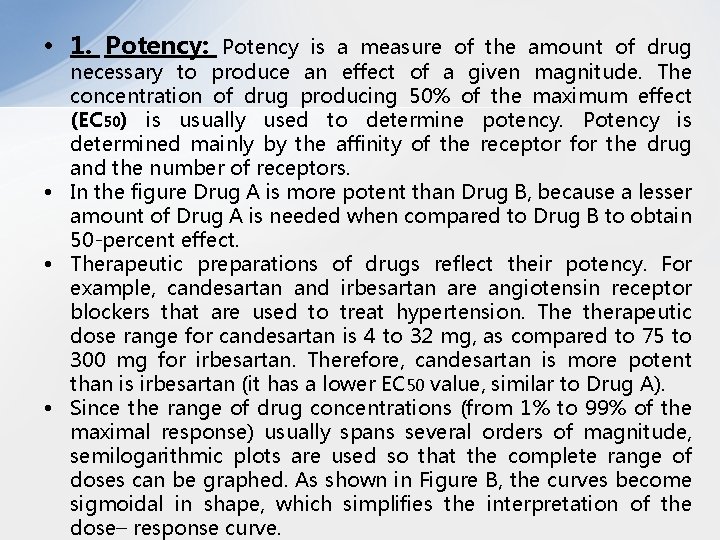
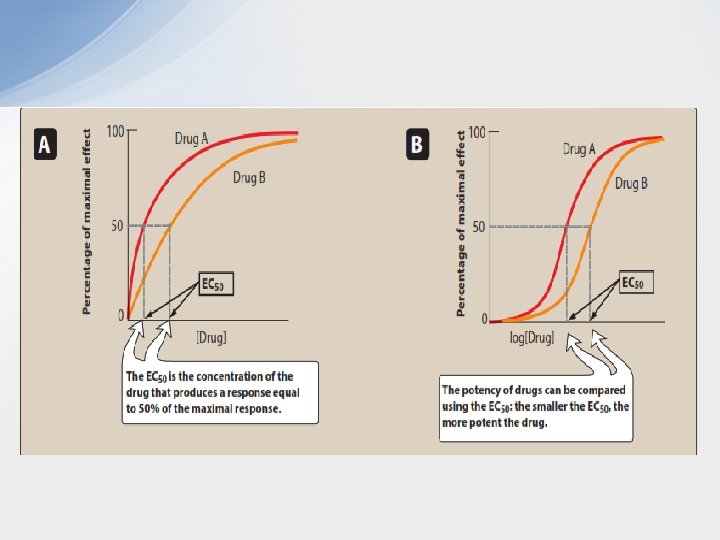
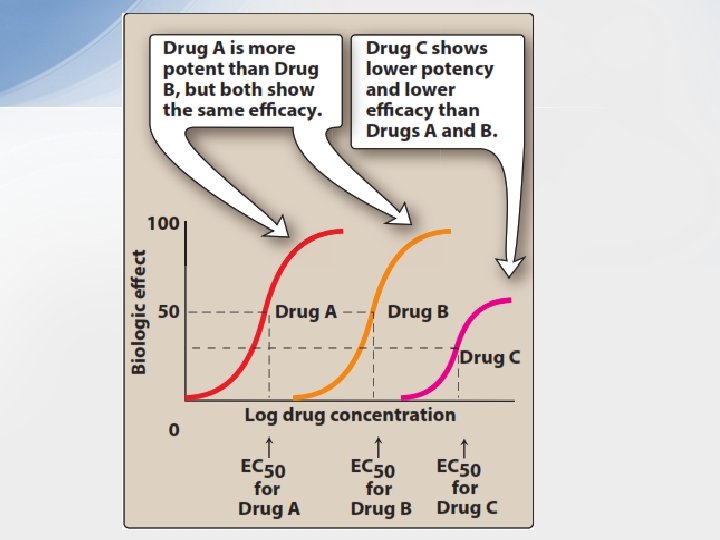
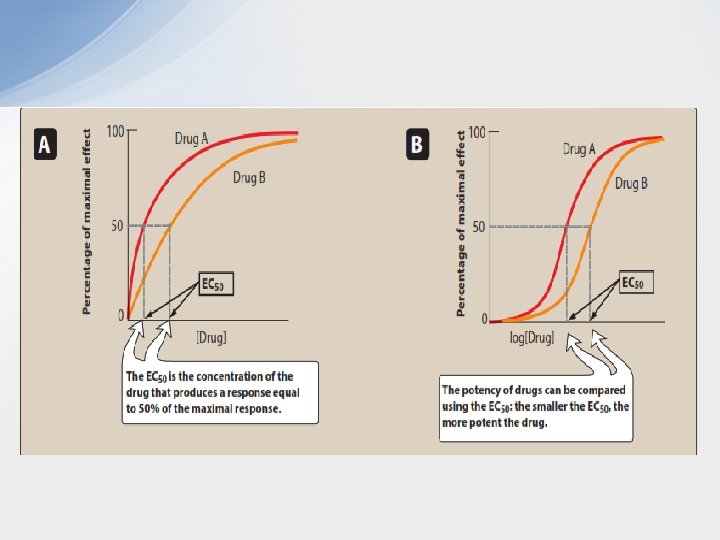
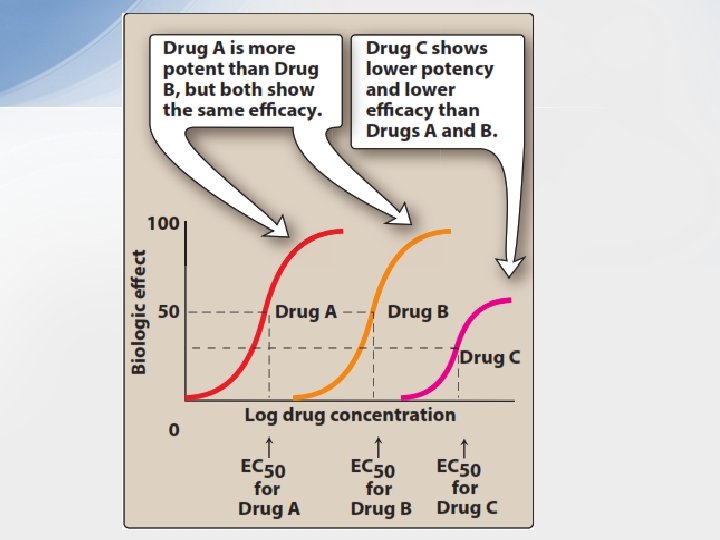
• 1. Potency: Potency is a measure of the amount of drug necessary to produce an effect of a given magnitude. The concentration of drug producing 50% of the maximum effect (EC 50) is usually used to determine potency. Potency is determined mainly by the affinity of the receptor for the drug and the number of receptors. • In the figure Drug A is more potent than Drug B, because a lesser amount of Drug A is needed when compared to Drug B to obtain 50 -percent effect. • Therapeutic preparations of drugs reflect their potency. For example, candesartan and irbesartan are angiotensin receptor blockers that are used to treat hypertension. The therapeutic dose range for candesartan is 4 to 32 mg, as compared to 75 to 300 mg for irbesartan. Therefore, candesartan is more potent than is irbesartan (it has a lower EC 50 value, similar to Drug A). • Since the range of drug concentrations (from 1% to 99% of the maximal response) usually spans several orders of magnitude, semilogarithmic plots are used so that the complete range of doses can be graphed. As shown in Figure B, the curves become sigmoidal in shape, which simplifies the interpretation of the dose– response curve.
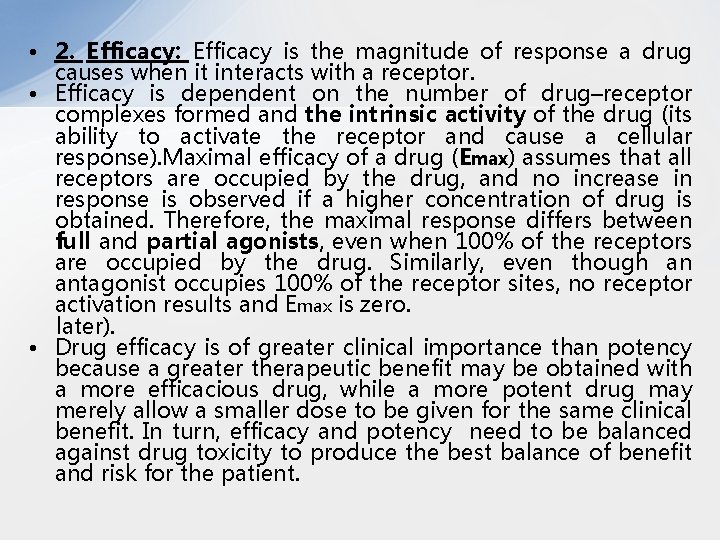
• 2. Efficacy: Efficacy is the magnitude of response a drug causes when it interacts with a receptor. • Efficacy is dependent on the number of drug–receptor complexes formed and the intrinsic activity of the drug (its ability to activate the receptor and cause a cellular response). Maximal efficacy of a drug (Emax) assumes that all receptors are occupied by the drug, and no increase in response is observed if a higher concentration of drug is obtained. Therefore, the maximal response differs between full and partial agonists, even when 100% of the receptors are occupied by the drug. Similarly, even though an antagonist occupies 100% of the receptor sites, no receptor activation results and Emax is zero. later). • Drug efficacy is of greater clinical importance than potency because a greater therapeutic benefit may be obtained with a more efficacious drug, while a more potent drug may merely allow a smaller dose to be given for the same clinical benefit. In turn, efficacy and potency need to be balanced against drug toxicity to produce the best balance of benefit and risk for the patient.
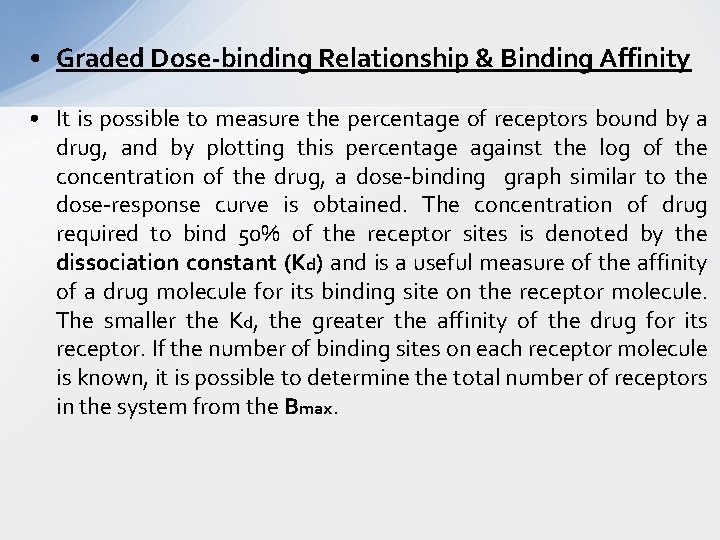
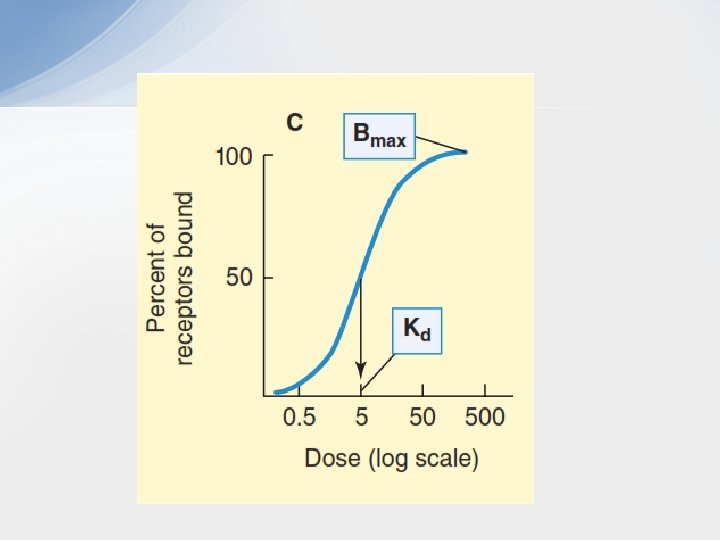
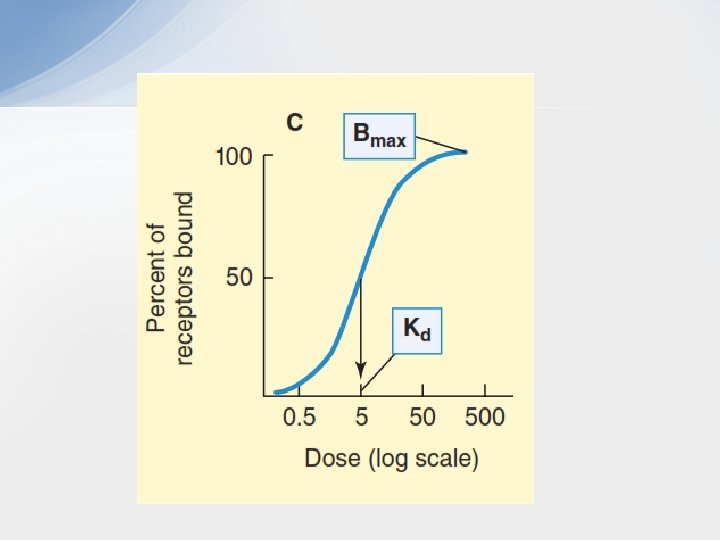
• Graded Dose-binding Relationship & Binding Affinity • It is possible to measure the percentage of receptors bound by a drug, and by plotting this percentage against the log of the concentration of the drug, a dose-binding graph similar to the dose-response curve is obtained. The concentration of drug required to bind 50% of the receptor sites is denoted by the dissociation constant (Kd) and is a useful measure of the affinity of a drug molecule for its binding site on the receptor molecule. The smaller the Kd, the greater the affinity of the drug for its receptor. If the number of binding sites on each receptor molecule is known, it is possible to determine the total number of receptors in the system from the Bmax.
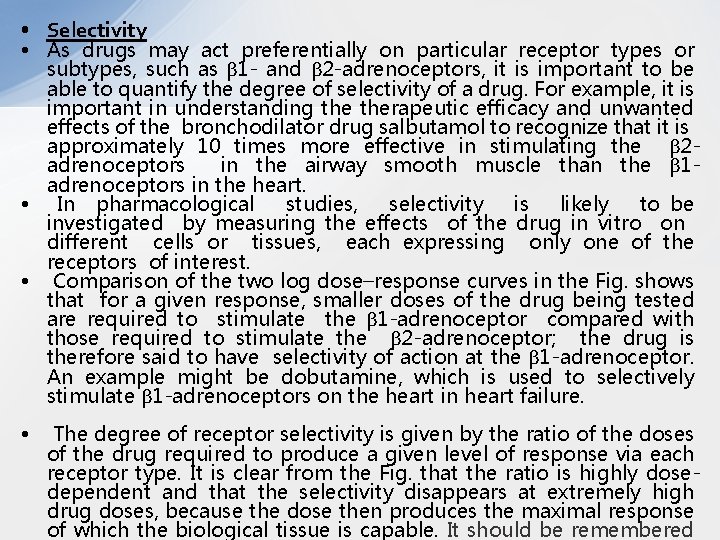
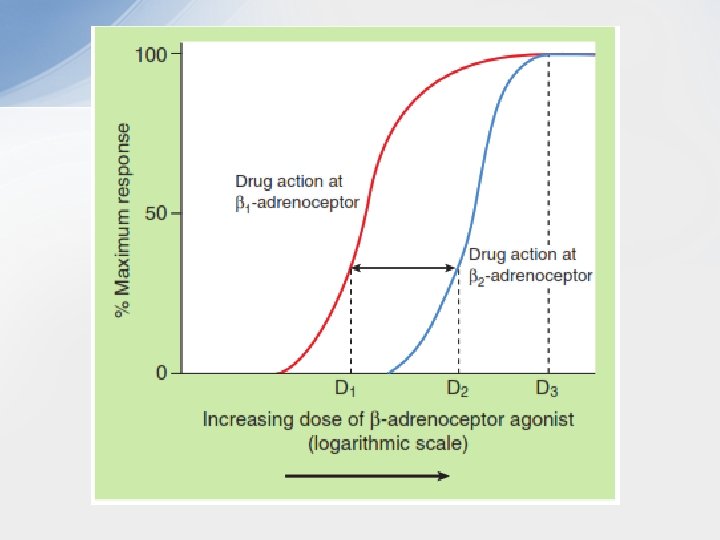
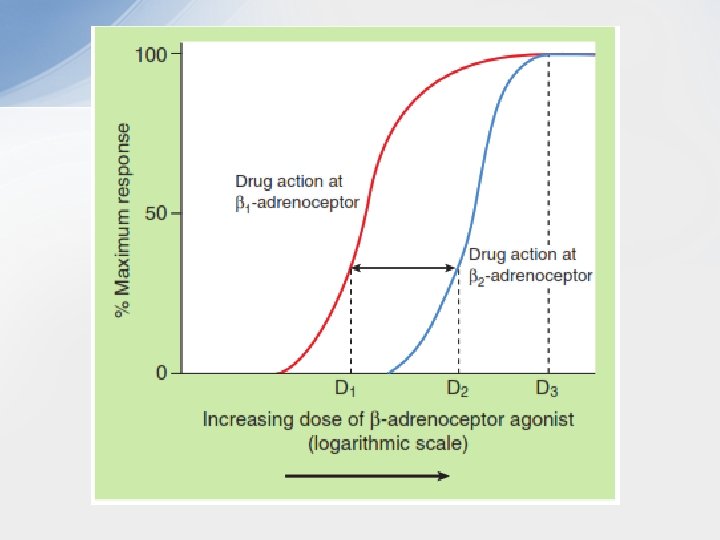
• Selectivity • As drugs may act preferentially on particular receptor types or subtypes, such as β 1 - and β 2 -adrenoceptors, it is important to be able to quantify the degree of selectivity of a drug. For example, it is important in understanding therapeutic efficacy and unwanted effects of the bronchodilator drug salbutamol to recognize that it is approximately 10 times more effective in stimulating the β 2 adrenoceptors in the airway smooth muscle than the β 1 adrenoceptors in the heart. • In pharmacological studies, selectivity is likely to be investigated by measuring the effects of the drug in vitro on different cells or tissues, each expressing only one of the receptors of interest. • Comparison of the two log dose–response curves in the Fig. shows that for a given response, smaller doses of the drug being tested are required to stimulate the β 1 -adrenoceptor compared with those required to stimulate the β 2 -adrenoceptor; the drug is therefore said to have selectivity of action at the β 1 -adrenoceptor. An example might be dobutamine, which is used to selectively stimulate β 1 -adrenoceptors on the heart in heart failure. • The degree of receptor selectivity is given by the ratio of the doses of the drug required to produce a given level of response via each receptor type. It is clear from the Fig. that the ratio is highly dosedependent and that the selectivity disappears at extremely high drug doses, because the dose then produces the maximal response of which the biological tissue is capable. It should be remembered
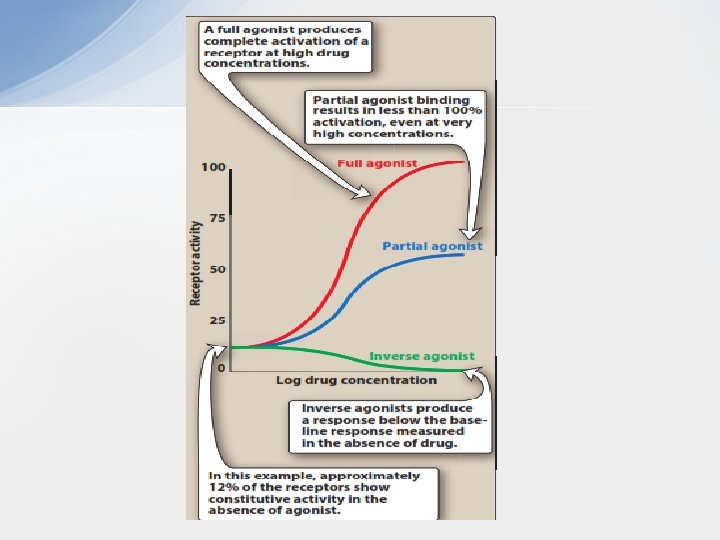
• Intrinsic Activity • Intrinsic activity describes the ability of the bound drug to induce the conformational changes in the receptor that induce receptor signalling. It determines drug ability to fully or partially activate the receptors. • Although affinity is a prerequisite for binding to a receptor, a drug may bind with high affinity but have low intrinsic activity. A drug with zero intrinsic activity is an antagonist. A. Full agonists • If a drug binds to a receptor and produces a maximal biologic response that mimics the response to the endogenous ligand, it is a full agonist Full agonists bind to a receptor, stabilizing the receptor in its active state and are said to have an intrinsic activity of one. • All full agonists for a receptor population should produce the same Emax. For example, phenylephrine is a full agonist at α 1 adrenoceptors, because it produces the same Emax as does the endogenous ligand, norepinephrine. Upon binding to α 1 adrenoceptors on vascular smooth muscle, phenylephrine stabilizes the receptor in its active state. This leads to the mobilization of intracellular Ca 2+, causing interaction of actin and myosin filaments and shortening of the muscle cells. The diameter of the arteriole decreases, causing an increase in resistance to blood flow through the vessel and an increase in blood pressure.
• B. Partial agonists • Partial agonists have intrinsic activities greater than zero but less than one. Even if all the receptors are occupied, partial agonists cannot produce the same Emax as a full agonist. However, a partial agonist may have an affinity that is greater than, less than, or equivalent to that of a full agonist. When a receptor is exposed to both a partial agonist and a full agonist, the partial agonist may act as a weak antagonist of the full agonist because it prevents access to the receptor of a molecule with higher intrinsic ability to initiate receptor signalling; this results in a reduced response. • This potential of partial agonists to act as both an agonist and antagonist may be therapeutically utilized. For example, aripiprazole, an atypical antipsychotic, is a partial agonist at selected dopamine receptors. Dopaminergic pathways that are overactive tend to be inhibited by aripiprazole, whereas pathways that are underactive are stimulated. This might explain the ability of aripiprazole to improve symptoms of schizophrenia, with a small risk of causing extrapyramidal adverse effects. • So, partial agonists can act as stabilizers of the variable activity of the natural ligand, as they enhance receptor activity when the endogenous ligand levels are low or zero, but block receptor activity when endogenous ligand levels are high.
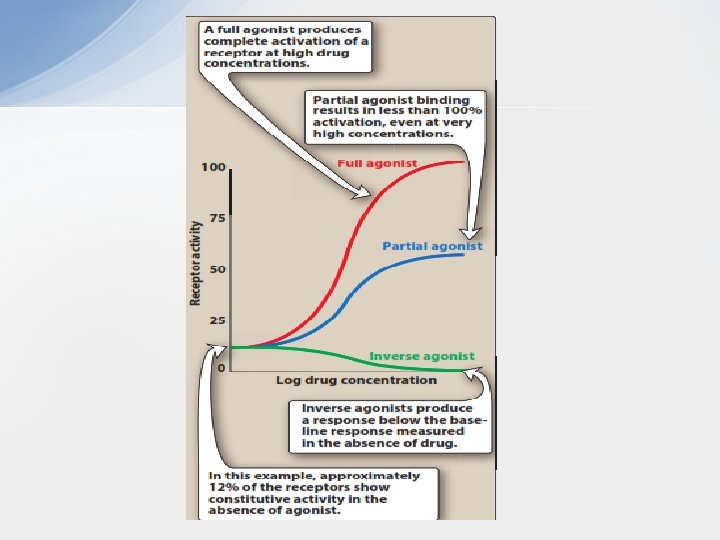
• C. Inverse agonists • Typically, in the absence of ligand, a receptor might be fully active or completely inactive. However, many receptor systems exhibit some activity in the absence of ligand, suggesting that some fraction of the receptor is always in the activated state. Activity in the absence of ligand is called constitutive activity. • Inverse agonists, unlike full agonists, stabilize the inactive R form and cause Ra to convert to Ri. This decreases the number of activated receptors to below that observed in the absence of drug. Thus, inverse agonists have an intrinsic activity less than zero, reverse the activity of receptors, and exert the opposite pharmacological effect of agonists. • An inverse agonist can be distinguished from the typical antagonists, which, on their own, bind to the receptor without affecting receptor signalling, as they have zero intrinsic activity (‘neutral’ or ‘silent’ antagonists). The action of a neutral antagonist depends on depriving the access of agonists to the receptor.
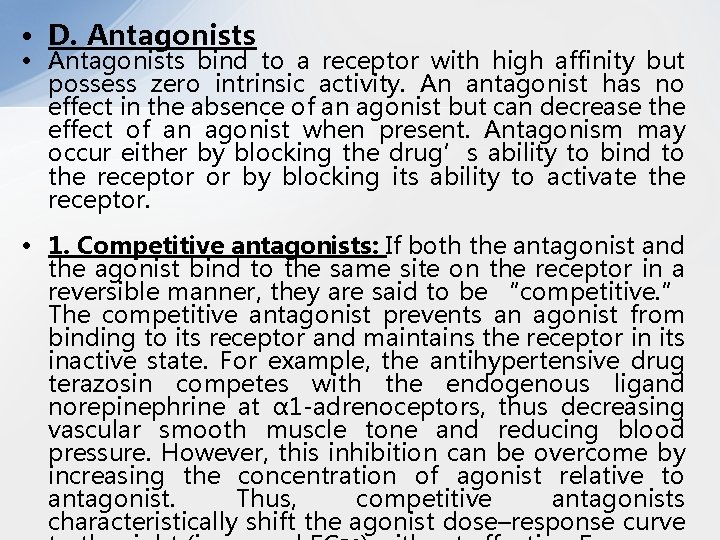
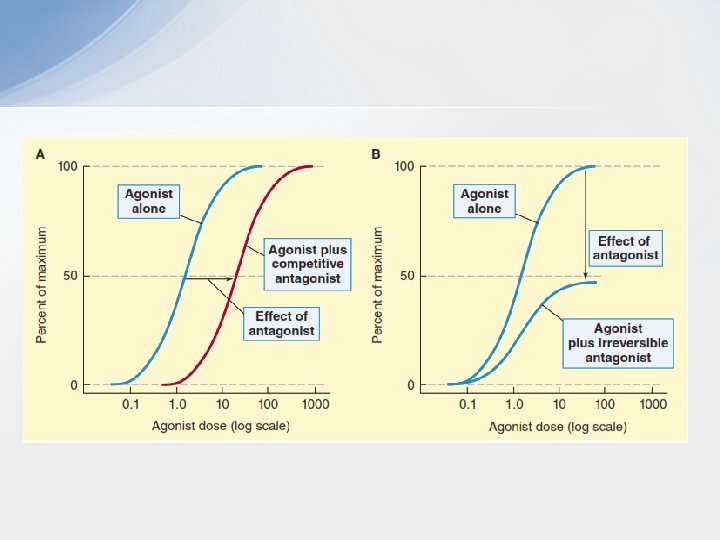
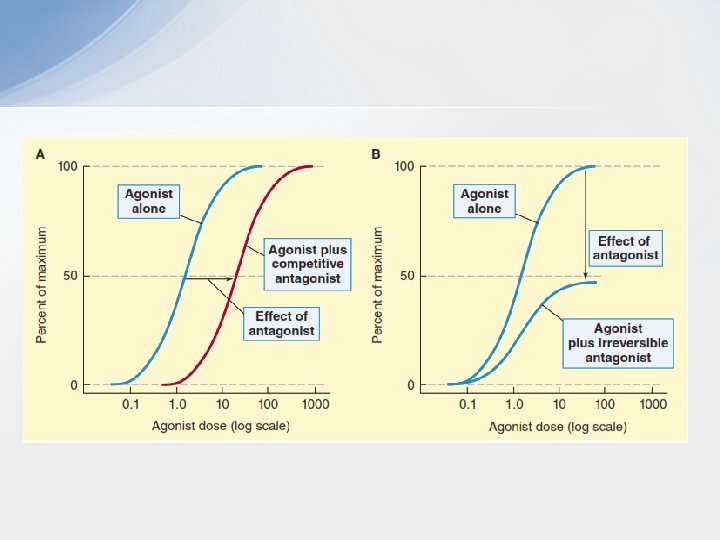
• D. Antagonists • Antagonists bind to a receptor with high affinity but possess zero intrinsic activity. An antagonist has no effect in the absence of an agonist but can decrease the effect of an agonist when present. Antagonism may occur either by blocking the drug’s ability to bind to the receptor or by blocking its ability to activate the receptor. • 1. Competitive antagonists: If both the antagonist and the agonist bind to the same site on the receptor in a reversible manner, they are said to be “competitive. ” The competitive antagonist prevents an agonist from binding to its receptor and maintains the receptor in its inactive state. For example, the antihypertensive drug terazosin competes with the endogenous ligand norepinephrine at α 1 -adrenoceptors, thus decreasing vascular smooth muscle tone and reducing blood pressure. However, this inhibition can be overcome by increasing the concentration of agonist relative to antagonist. Thus, competitive antagonists characteristically shift the agonist dose–response curve
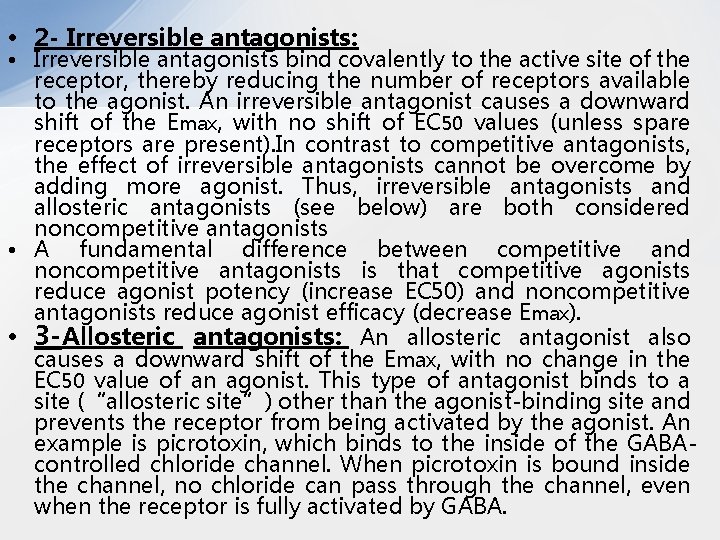
• 2 - Irreversible antagonists: • Irreversible antagonists bind covalently to the active site of the receptor, thereby reducing the number of receptors available to the agonist. An irreversible antagonist causes a downward shift of the Emax, with no shift of EC 50 values (unless spare receptors are present). In contrast to competitive antagonists, the effect of irreversible antagonists cannot be overcome by adding more agonist. Thus, irreversible antagonists and allosteric antagonists (see below) are both considered noncompetitive antagonists • A fundamental difference between competitive and noncompetitive antagonists is that competitive agonists reduce agonist potency (increase EC 50) and noncompetitive antagonists reduce agonist efficacy (decrease Emax). • 3 -Allosteric antagonists: An allosteric antagonist also causes a downward shift of the Emax, with no change in the EC 50 value of an agonist. This type of antagonist binds to a site (“allosteric site”) other than the agonist-binding site and prevents the receptor from being activated by the agonist. An example is picrotoxin, which binds to the inside of the GABAcontrolled chloride channel. When picrotoxin is bound inside the channel, no chloride can pass through the channel, even when the receptor is fully activated by GABA.
• 4. Functional antagonism: • An antagonist may act at a completely separate receptor, initiating effects that are functionally opposite those of the agonist. A classic example is the functional antagonism by epinephrine to histamine-induced bronchoconstriction. Histamine binds to H 1 histamine receptors on bronchial smooth muscle, causing bronchoconstriction of the bronchial tree. Epinephrine is an agonist at β 2 adrenoceptors on bronchial smooth muscle, which causes the muscles to relax. This functional antagonism is also known as “physiologic antagonism. ” • 5. Chemical Antagonists: • A chemical antagonist interacts directly with the drug being antagonized to remove it or to prevent it from binding to its target. A chemical antagonist does not depend on interaction with the agonist’s receptor (although such interaction may occur). Common examples of chemical antagonists are dimercaprol, a chelator of lead and some other toxic metals, and pralidoxime, which combines with the phosphorus in organophosphate cholinesterase inhibitors.
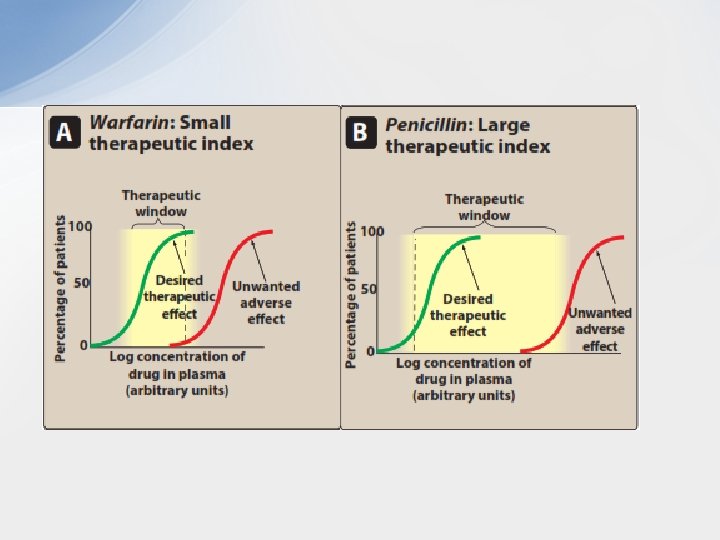
• Quantal Dose-response Relationships • Another important dose–response relationship is that between the dose of the drug and the proportion of a population that responds to it. These responses are known as quantal responses, because, for any individual, the effect either occurs or it does not. Graded responses can be transformed to quantal responses by designating a predetermined level of the graded response as the point at which a response occurs or not. For example, a quantal dose– response relationship can be determined in a population for the antihypertensive drug atenolol. A positive response is defined as a fall of at least 5 mm Hg in diastolic blood pressure. • Quantal dose–response curves are useful for determining doses to which most of the population responds. They have similar shapes as log dose–response curves, and the ED 50 is the drug dose that causes a therapeutic response in half of the population. • Therapeutic index • Quantal relationships can be defined for both toxic and therapeutic drug effects to allow calculation of therapeutic index (TI). TI of a drug is the ratio of the dose that
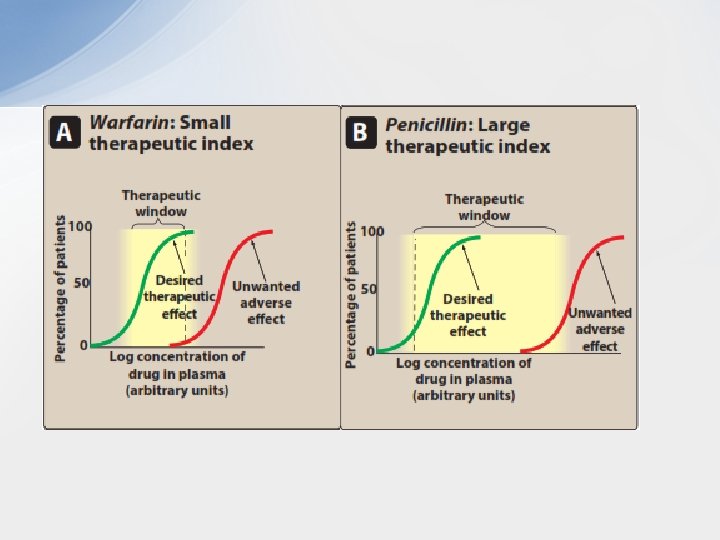
• The TI is a measure of a drug’s safety, because a larger value indicates a wide margin between doses that are effective and doses that are toxic. • The therapeutic window, a more clinically useful index of safety, describes the dosage range between the minimum effective therapeutic concentration or dose, and the minimum toxic concentration or dose. For example, if the average minimum therapeutic plasma concentration of theophylline is 8 mg/L and toxic effects are observed at 18 mg/L, therapeutic window is 8– 18 mg/L. • Although high TI values are required for most drugs, some drugs with low therapeutic indices are routinely used to treat serious diseases. In these cases, the risk of experiencing side effects is not as great as the risk of leaving the disease untreated. • Warfarin , oral anticoagulant (example of a drug with a small therapeutic index): As the dose of warfarin is increased, a greater fraction of the patients respond (for this drug, the desired response is a two- to threefold increase in the international normalized ratio [INR]) until, eventually, all patients respond. However, at higher doses of warfarin, anticoagulation resulting in hemorrhage. • Penicillin, an antimicrobial (example of a drug with a large therapeutic index): For drugs such as penicillin, it is safe and common to give doses in excess of that which is minimally required to achieve a desired response without the risk of adverse side effects.
 Ambenomium
Ambenomium Cholinomimetic agents
Cholinomimetic agents Debriefing report
Debriefing report Cont or cont'd
Cont or cont'd Define pharmacodynamics
Define pharmacodynamics Iontropic
Iontropic Pharmacodynamics
Pharmacodynamics Pharmacodynamics
Pharmacodynamics Graded dose response curve
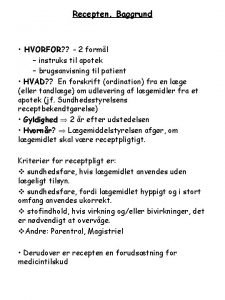
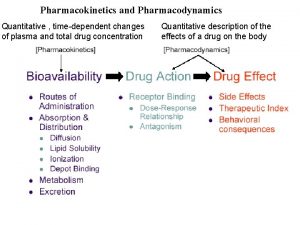
Graded dose response curve Difference between pharmacodynamics and pharmacokinetics
Difference between pharmacodynamics and pharmacokinetics Van rossums formel
Van rossums formel Pharmacokinetic definition
Pharmacokinetic definition Pharmacodynamics
Pharmacodynamics Pharmacokinetics vs pharmacodynamics
Pharmacokinetics vs pharmacodynamics Mimic microwave
Mimic microwave Octopus tf tg
Octopus tf tg Alpha-2 adrenergic
Alpha-2 adrenergic Biceps brachii prime mover
Biceps brachii prime mover Glp-1 agonist
Glp-1 agonist Mimic poison dart frog
Mimic poison dart frog Benzodiazépines
Benzodiazépines Alpha 2 agonist
Alpha 2 agonist