www rrnmf com Pattern Recognition of Myopathic Disorders



- Slides: 12

www. rrnmf. com Pattern Recognition of Myopathic Disorders Richard J. Barohn, MD Chair, Department of Neurology Gertrude and Dewey Ziegler Professor of Neurology University Distinguished Professor Vice Chancellor for Research University of Kansas Medical Center Kansas City, KS

Pattern Recognition of Myopathic Disorders Pattern MP 1: • Proximal “limb-girdle” weakness – Acute/subacute – acquired • Inflammatory (PM/DM) - pain/rash/CTD • Endocrine • Toxic drugs – Chronic/congenital/painless – hereditary • Most dystrophies • Congenital • Mitochondrial • Pompe’s disease • Carnitine deficiency • Neuromuscular junction • Overlap with SMA
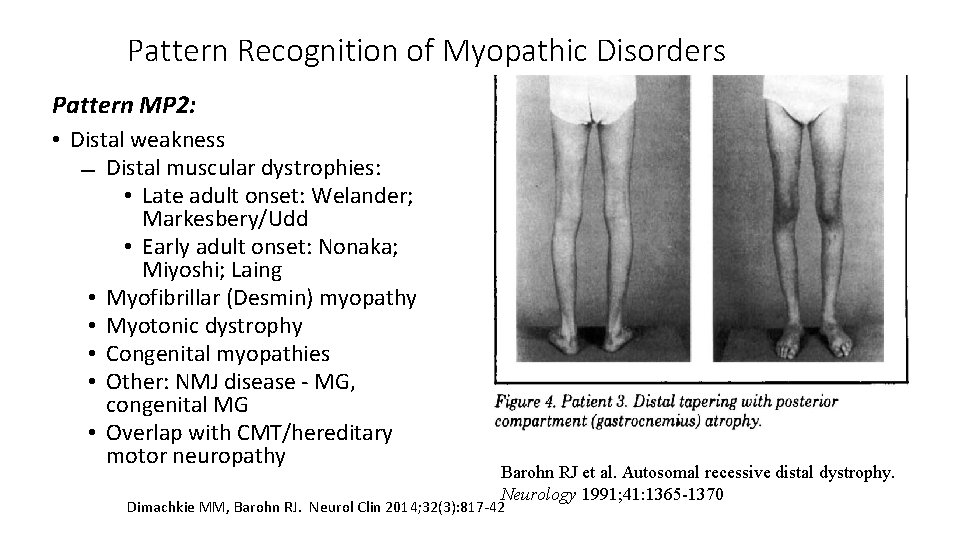
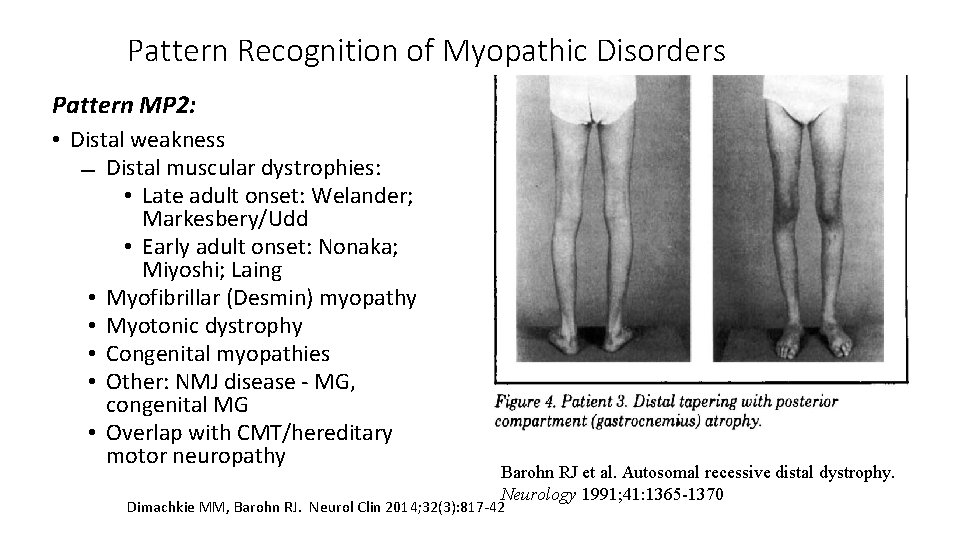
Pattern Recognition of Myopathic Disorders Pattern MP 2: • Distal weakness Distal muscular dystrophies: • Late adult onset: Welander; Markesbery/Udd • Early adult onset: Nonaka; Miyoshi; Laing • Myofibrillar (Desmin) myopathy • Myotonic dystrophy • Congenital myopathies • Other: NMJ disease - MG, congenital MG • Overlap with CMT/hereditary motor neuropathy Barohn RJ et al. Autosomal recessive distal dystrophy. Neurology 1991; 41: 1365 -1370 Dimachkie MM, Barohn RJ. Neurol Clin 2014; 32(3): 817 -42
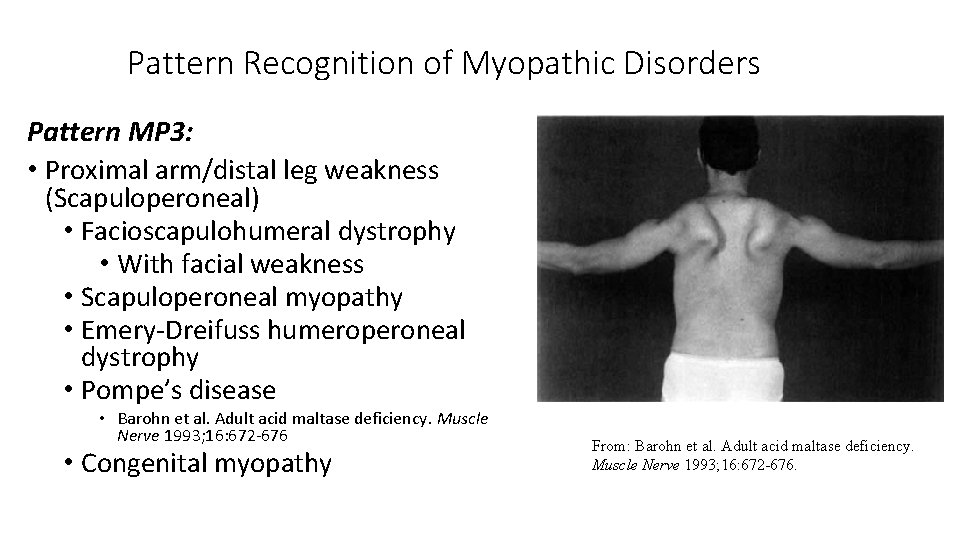
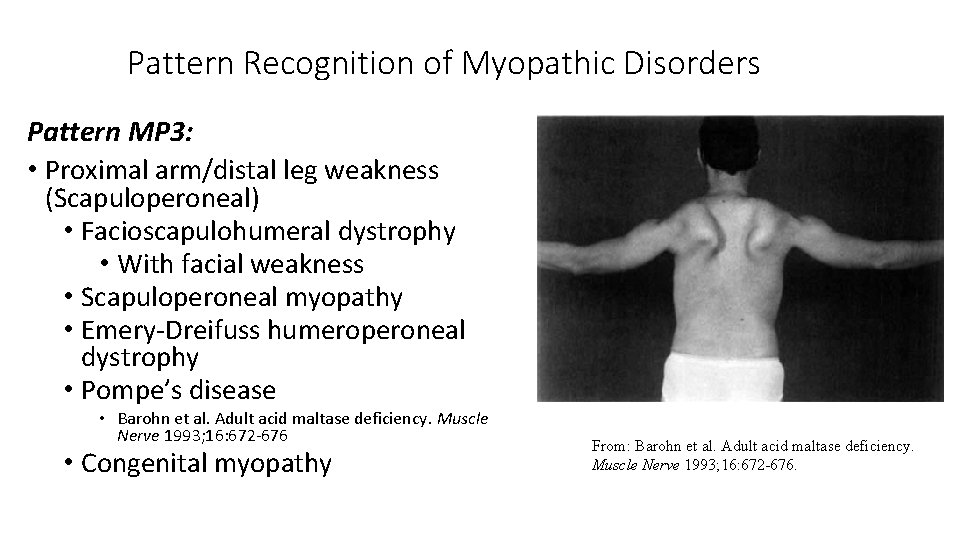
Pattern Recognition of Myopathic Disorders Pattern MP 3: • Proximal arm/distal leg weakness (Scapuloperoneal) • Facioscapulohumeral dystrophy • With facial weakness • Scapuloperoneal myopathy • Emery-Dreifuss humeroperoneal dystrophy • Pompe’s disease • Barohn et al. Adult acid maltase deficiency. Muscle Nerve 1993; 16: 672 -676 • Congenital myopathy From: Barohn et al. Adult acid maltase deficiency. Muscle Nerve 1993; 16: 672 -676.
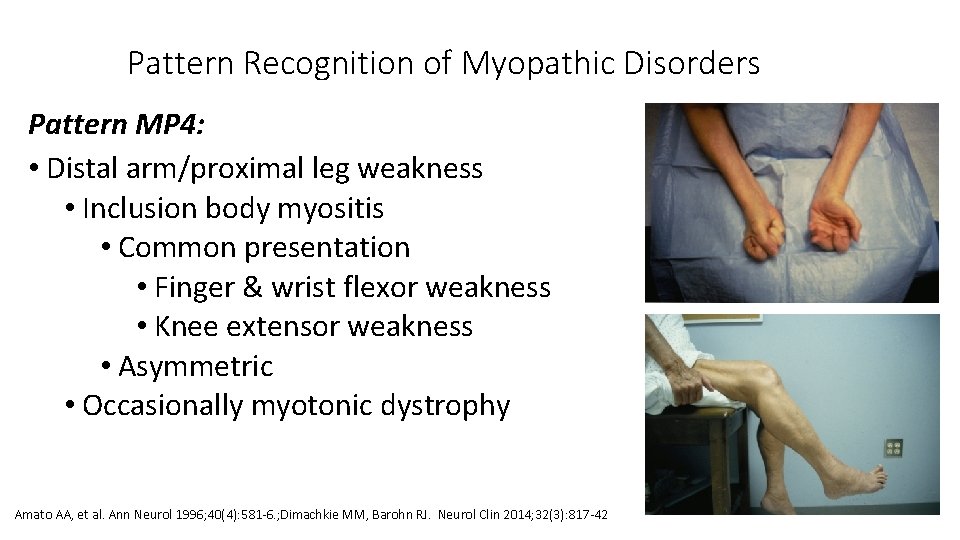
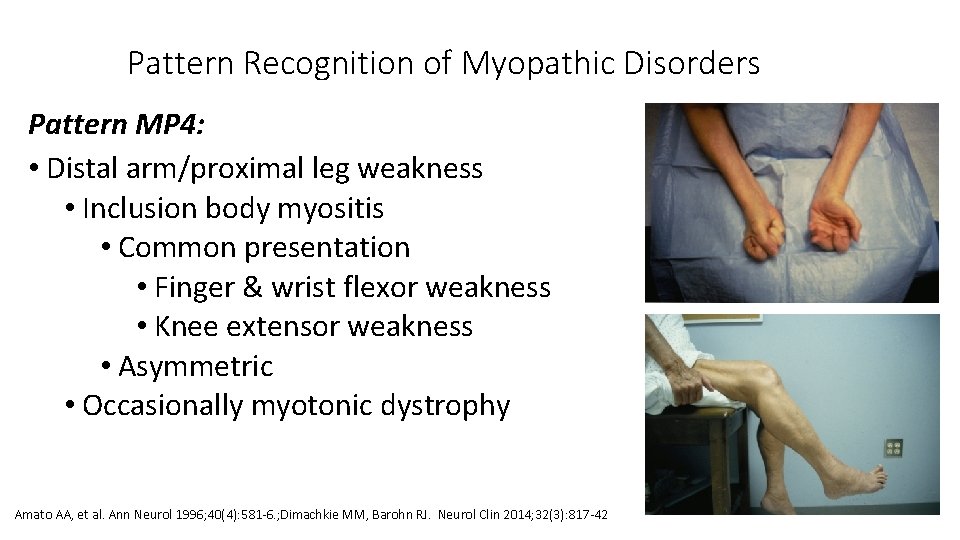
Pattern Recognition of Myopathic Disorders Pattern MP 4: • Distal arm/proximal leg weakness • Inclusion body myositis • Common presentation • Finger & wrist flexor weakness • Knee extensor weakness • Asymmetric • Occasionally myotonic dystrophy Amato AA, et al. Ann Neurol 1996; 40(4): 581 -6. ; Dimachkie MM, Barohn RJ. Neurol Clin 2014; 32(3): 817 -42
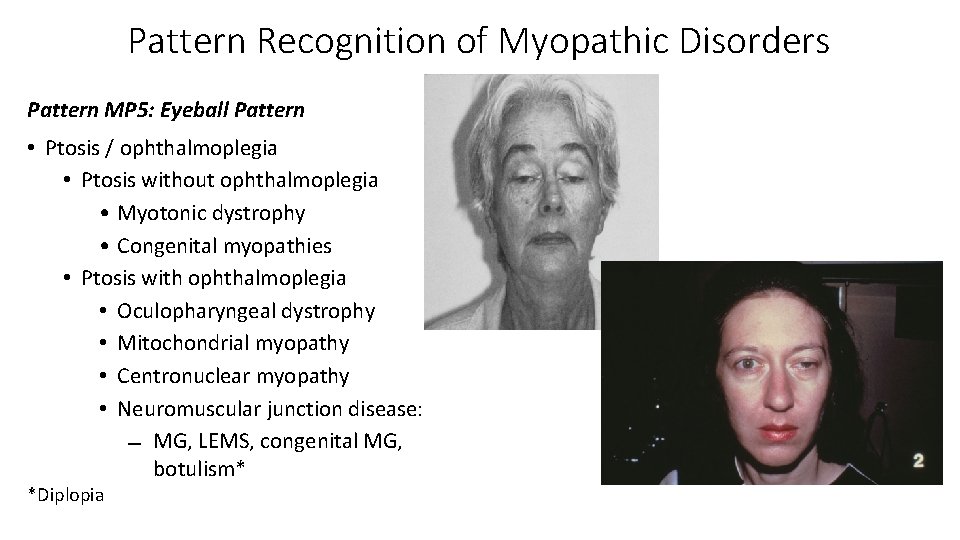
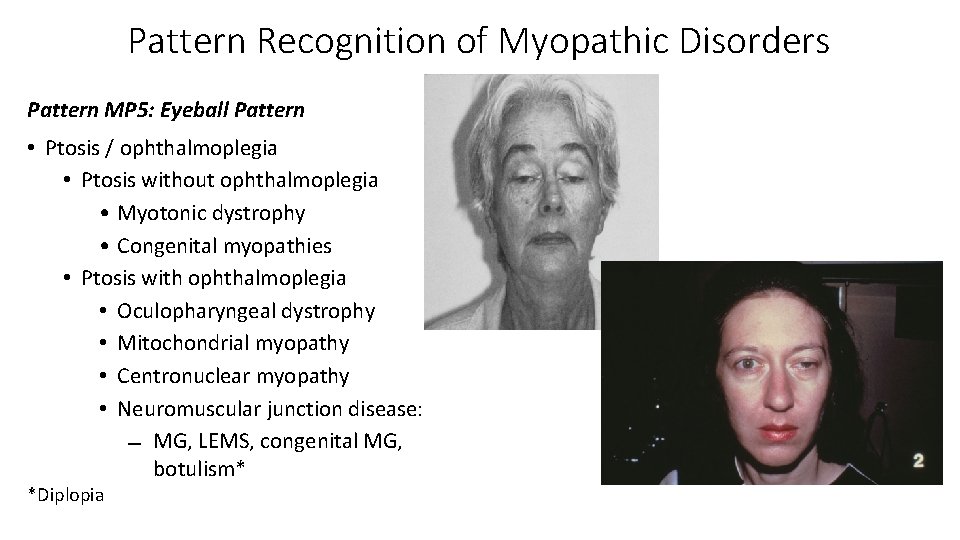
Pattern Recognition of Myopathic Disorders Pattern MP 5: Eyeball Pattern • Ptosis / ophthalmoplegia • Ptosis without ophthalmoplegia • Myotonic dystrophy • Congenital myopathies • Ptosis with ophthalmoplegia • Oculopharyngeal dystrophy • Mitochondrial myopathy • Centronuclear myopathy • Neuromuscular junction disease: MG, LEMS, congenital MG, botulism* *Diplopia
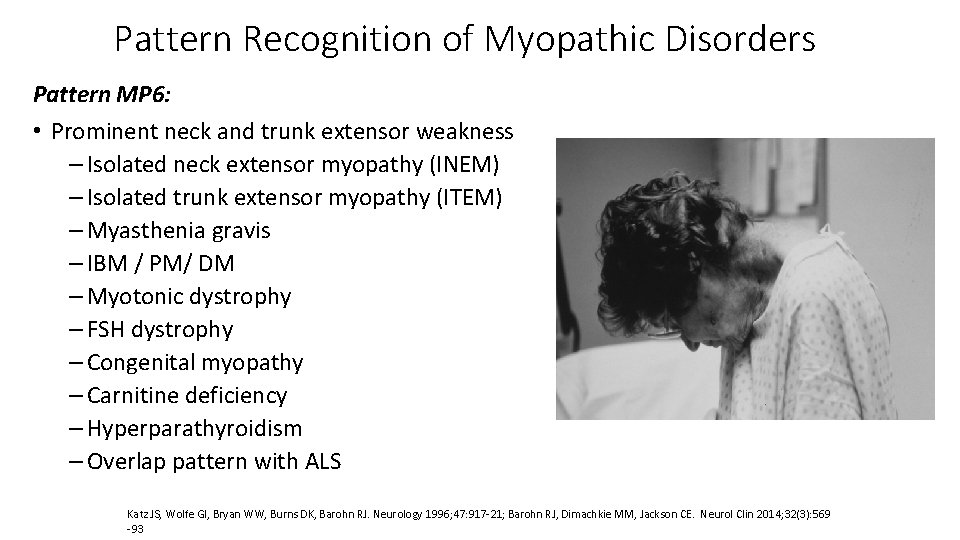
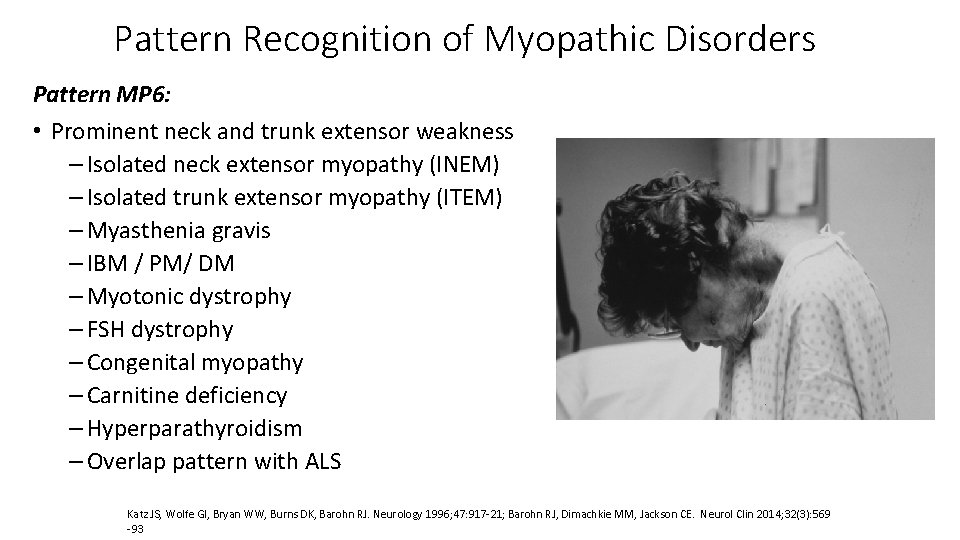
Pattern Recognition of Myopathic Disorders Pattern MP 6: • Prominent neck and trunk extensor weakness – Isolated neck extensor myopathy (INEM) – Isolated trunk extensor myopathy (ITEM) – Myasthenia gravis – IBM / PM/ DM – Myotonic dystrophy – FSH dystrophy – Congenital myopathy – Carnitine deficiency – Hyperparathyroidism – Overlap pattern with ALS Katz JS, Wolfe GI, Bryan WW, Burns DK, Barohn RJ. Neurology 1996; 47: 917 -21; Barohn RJ, Dimachkie MM, Jackson CE. Neurol Clin 2014; 32(3): 569 -93
Pattern Recognition of Myopathic Disorders Pattern MP 7: • Bulbar weakness – tongue/pharyngeal/ diaphragm (dysarthria or dysphagia, SOB) • MG, LEMS • Oculopharyngeal dystrophy • LGMD 1 A myotilinopathy • Myotonic dystrophy • IBM • Pompe (respiratory) • Overlap pattern with: ALS, Kennedy’s
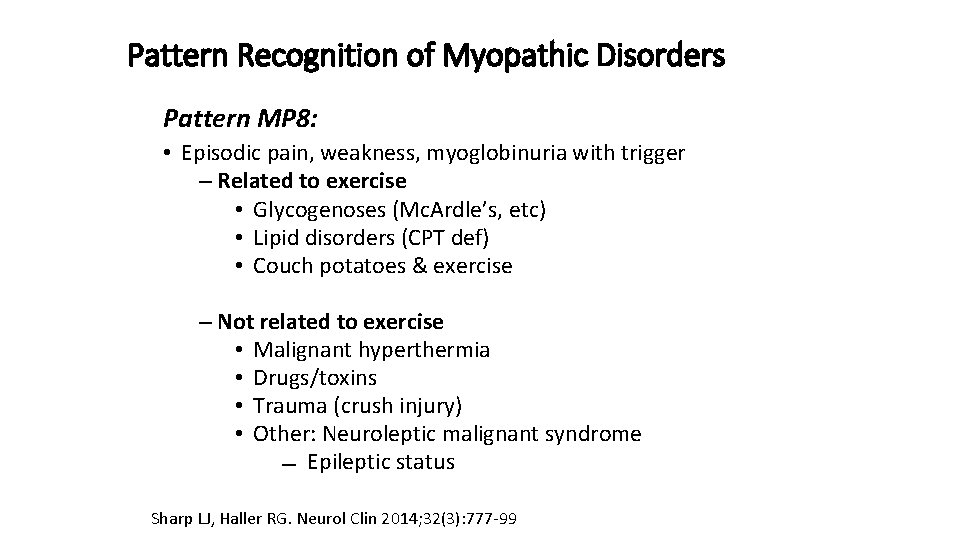
Pattern Recognition of Myopathic Disorders Pattern MP 8: • Episodic pain, weakness, myoglobinuria with trigger – Related to exercise • Glycogenoses (Mc. Ardle’s, etc) • Lipid disorders (CPT def) • Couch potatoes & exercise – Not related to exercise • Malignant hyperthermia • Drugs/toxins • Trauma (crush injury) • Other: Neuroleptic malignant syndrome Epileptic status Sharp LJ, Haller RG. Neurol Clin 2014; 32(3): 777 -99
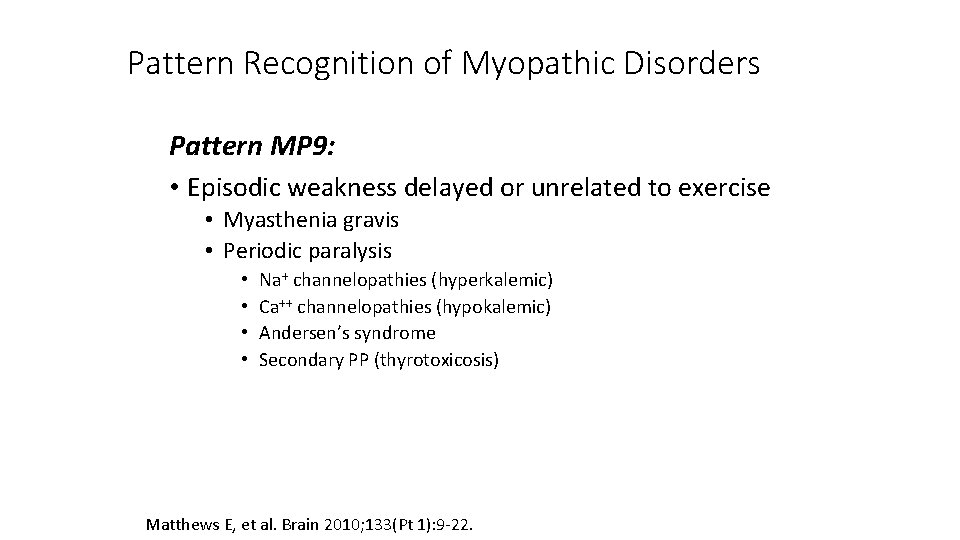
Pattern Recognition of Myopathic Disorders Pattern MP 9: • Episodic weakness delayed or unrelated to exercise • Myasthenia gravis • Periodic paralysis • • Na+ channelopathies (hyperkalemic) Ca++ channelopathies (hypokalemic) Andersen’s syndrome Secondary PP (thyrotoxicosis) Matthews E, et al. Brain 2010; 133(Pt 1): 9 -22.

Pattern Recognition of Myopathic Disorders Pattern MP 10: • Stiffness/decreased ability to relax – Improves with exercise • Myotonia – usually Cl- channelopathy – Worsens with exercise/cold sensitivity • Paramyotonia - Na+ channelopathy • Brody’s disease – With fixed weakness • Myotonic dystrophy (DM 1) • Proximal myotonic myopathy (DM 2) • Becker’s disease (AR Cl- channelopathy) – Other: rippling muscle, neuromyotonia, stiff-person Statland JM, et al. JAMA 2012; 308: 1357 -1365; Trivedi JR, et al. Brain 2013; 136(Pt 7): 2189 -2200; Statland J, Phillips L, Trivedi JR. Neurol Clin 2014; 32(3): 801 -815
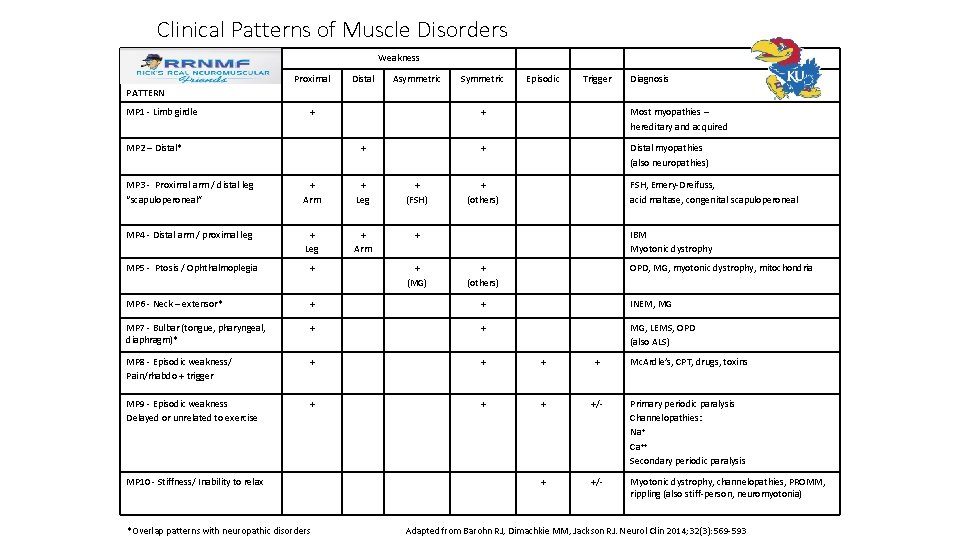
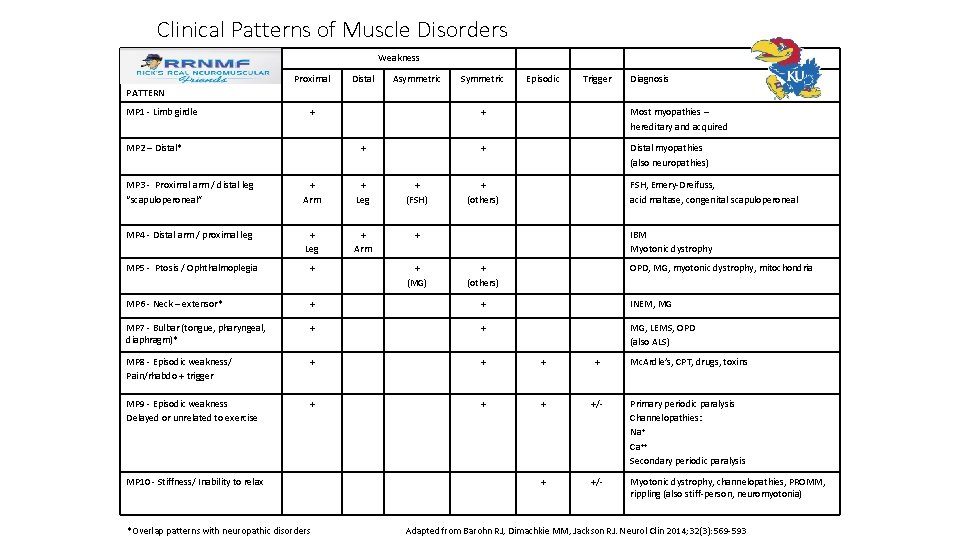
Clinical Patterns of Muscle Disorders Weakness Proximal Distal Asymmetric Symmetric Episodic Trigger Diagnosis PATTERN MP 1 - Limb girdle + MP 2 – Distal* + + Most myopathies – hereditary and acquired + Distal myopathies (also neuropathies) MP 3 - Proximal arm / distal leg “scapuloperoneal” + Arm + Leg + (FSH) MP 4 - Distal arm / proximal leg + Leg + Arm + MP 5 - Ptosis / Ophthalmoplegia + MP 6 - Neck – extensor* + + INEM, MG MP 7 - Bulbar (tongue, pharyngeal, diaphragm)* + + MG, LEMS, OPD (also ALS) MP 8 - Episodic weakness/ Pain/rhabdo + trigger + + Mc. Ardle’s, CPT, drugs, toxins MP 9 - Episodic weakness Delayed or unrelated to exercise + +/- Primary periodic paralysis Channelopathies: Na+ Ca++ Secondary periodic paralysis + +/- Myotonic dystrophy, channelopathies, PROMM, rippling (also stiff-person, neuromyotonia) MP 10 - Stiffness/ Inability to relax *Overlap patterns with neuropathic disorders + (MG) + (others) FSH, Emery-Dreifuss, acid maltase, congenital scapuloperoneal IBM Myotonic dystrophy + (others) OPD, MG, myotonic dystrophy, mitochondria Adapted from Barohn RJ, Dimachkie MM, Jackson RJ. Neurol Clin 2014; 32(3): 569 -593