WUSM Pediatrics Leadership Development Series Difficult Conversations January
- Slides: 16
WUSM Pediatrics Leadership Development Series Difficult Conversations January 25, 2017 Dawn M. Newman, Ph. D. dawn. m. newman@wustl. edu Human Resources – Applied Leadership & OD
Introductions • Anyone in the class who was not here last week? If so, please introduce yourself, tell us your role, and what you’d like to accomplish in today’s session. 2
Effective Communication Quick Recap • What did you apply since last week? • Did you connect with an accountability partner? • What did you learn? 3
Objectives 1. Learn techniques/methods for holding difficult conversations. 2. Identify difficult/sensitive situations and steps to take to manage. 3. Know how to obtain receptivity from the other person. 4
Difficult Conversations • Think of a conversation you had recently (or plan to have soon) that was (is) “difficult” • Write down 3 -4 attributes that make the conversation “difficult” • Indicate your preference on the continuum Avoiding Addressing • Discuss your answers in your small group then share with the larger group 5
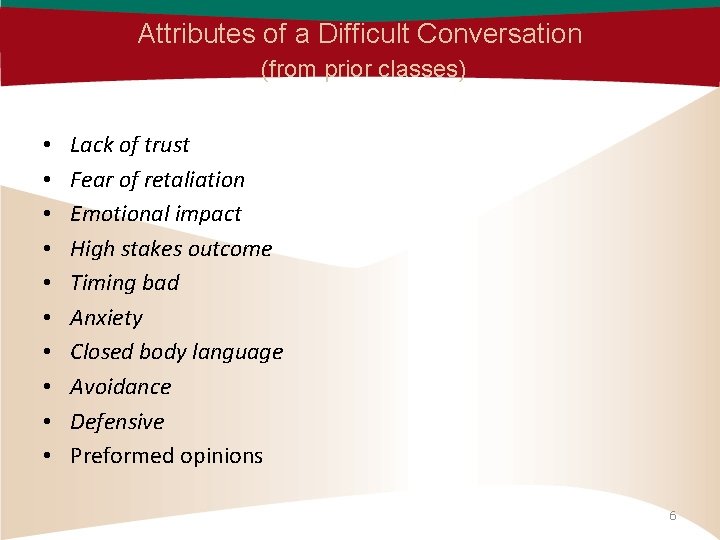
Attributes of a Difficult Conversation (from prior classes) • • • Lack of trust Fear of retaliation Emotional impact High stakes outcome Timing bad Anxiety Closed body language Avoidance Defensive Preformed opinions 6
Video • http: //smartbyt. es/7 R 6 OM • Why We Avoid Difficult Conversations • by Dr. Marcia Reynolds 7
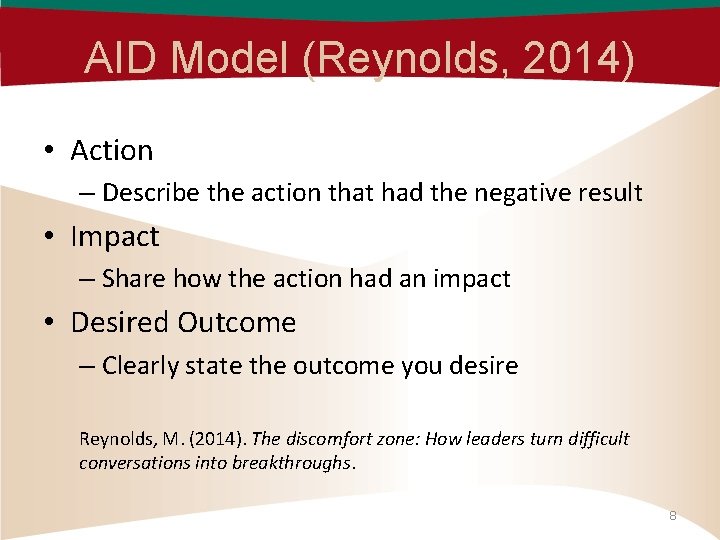
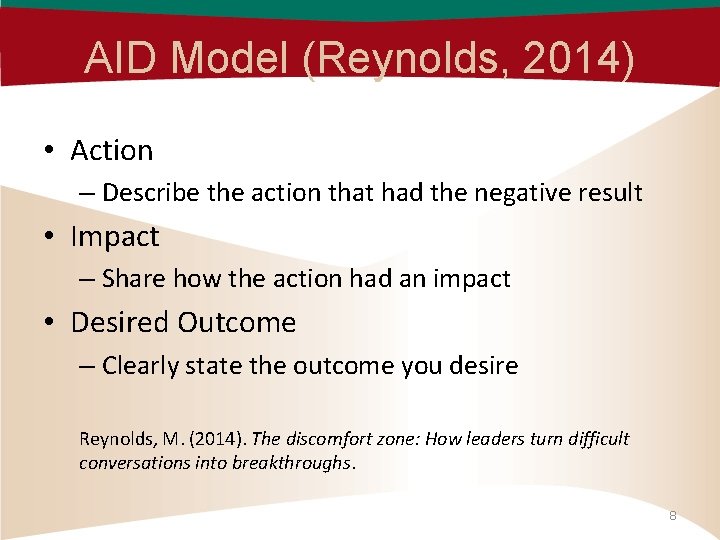
AID Model (Reynolds, 2014) • Action – Describe the action that had the negative result • Impact – Share how the action had an impact • Desired Outcome – Clearly state the outcome you desire Reynolds, M. (2014). The discomfort zone: How leaders turn difficult conversations into breakthroughs. 8
Tips & Resources • We Have to Talk (Ringer, 2017) • http: //www. judyringer. com/resources/article s/we-have-to-talk-a-stepbystep-checklist-fordifficult-conversations. php • Handout: Six Step Checklist (Ringer, 2017) • http: //www. judyringer. com/perch/resources/ six-step-checklist-for-diff-conv-2. pdf 9
Let’s try…. Practice Round 1 • Choose a situation for a conversation • Prepare by using the AID model and/or Six Step Checklist (3 -5 minutes) • Pair up and practice (5 minutes) • We’d like two volunteers to demonstrate the approach in our safe environment • Others observe to capture what works 10
Giving & Receiving Feedback What works? Giving Receiving 11
Video • http: //smartbyt. es/GE 10 F IMS video • Three C's of a Difficult Conversation • by Dr. Marcia Reynolds • 3 C’s: Calm, Curious, Care (Reynolds, 2014) 12
Practice Round 2 • Choose a conversation you plan to have in the next week • Prepare using the tips & resources • Practice the conversation • Discuss what went well and what you will do in the “real” conversation • Please share a learning point 13
Additional Resources Rosenstein, A. H. (2012). Physician Communication and Care Management: The Good, the Bad and the Ugly. Physician Executive, 38(4), 34 -37. http: //libproxy. wustl. edu/login? url=http: //search. ebscohost. com/login. aspx? direct=tr ue&db=bth&AN=78855042&site=ehost-live&scope=site Shannon, D. (2012). Effective Physician-to-Physician Communication: An Essential Ingredient for Care Coordination. Physician Executive, 38(1), 16 -21. http: //libproxy. wustl. edu/login? url=http: //search. ebscohost. com/login. aspx? direct=tr ue&db=bth&AN=70548724&site=ehost-live&scope=site 14
“Difficult” Patients • A study of internists and family practitioners noted several characteristics* – Patients with mental health problems or >5 somatic symptoms – Patients who brought a list of complaints to the visit/frequent users of the health care system • In the pediatric population, it is often the parent who is the contributor to a difficult patient encounter • http: //pediatrics. aappublications. org/content/pediatrics/127/ 1/163. full. pdf *2010 Cora Breuner and Megan Moreno to the Difficult Patient/Parent Encounter Approaches 15
Difficult Conversations • Today I learned. . . 16
 Archibus training
Archibus training Difficult conversations ppt
Difficult conversations ppt Types of difficult conversations
Types of difficult conversations Difficult conversations role play
Difficult conversations role play Vital signs normal range for pediatrics
Vital signs normal range for pediatrics Normal vital signs of newborn
Normal vital signs of newborn Post hepatic jaundice
Post hepatic jaundice Clove hitch restraints
Clove hitch restraints Pediatric medication administration guidelines
Pediatric medication administration guidelines Costochondritis
Costochondritis Vital signs normal range pediatrics
Vital signs normal range pediatrics Nips scale
Nips scale Differential diagnosis of jaundice in pediatrics
Differential diagnosis of jaundice in pediatrics Define modern concept of child care
Define modern concept of child care Modern concept of pediatrics
Modern concept of pediatrics Family medicine shelf percentiles
Family medicine shelf percentiles Chest pain in pediatrics
Chest pain in pediatrics