Whats the matter here Sudden Unexpected Infant Deaths




- Slides: 19
What’s the matter here? Sudden Unexpected Infant Deaths in Connecticut Kirsten Bechtel MD Associate Professor of Pediatrics and of Emergency Medicine Yale School of Medicine Co-Chairperson Connecticut Child Fatality Review Panel AAP Executive Committee, Section of Child Death Review
Disclosures • I have no relevant disclosures.
Objectives • What is Child Fatality Review? • What are the demographics of infants who die in suddenly and unexpectedly in Connecticut? • What steps can be taken to reduce these preventable deaths?

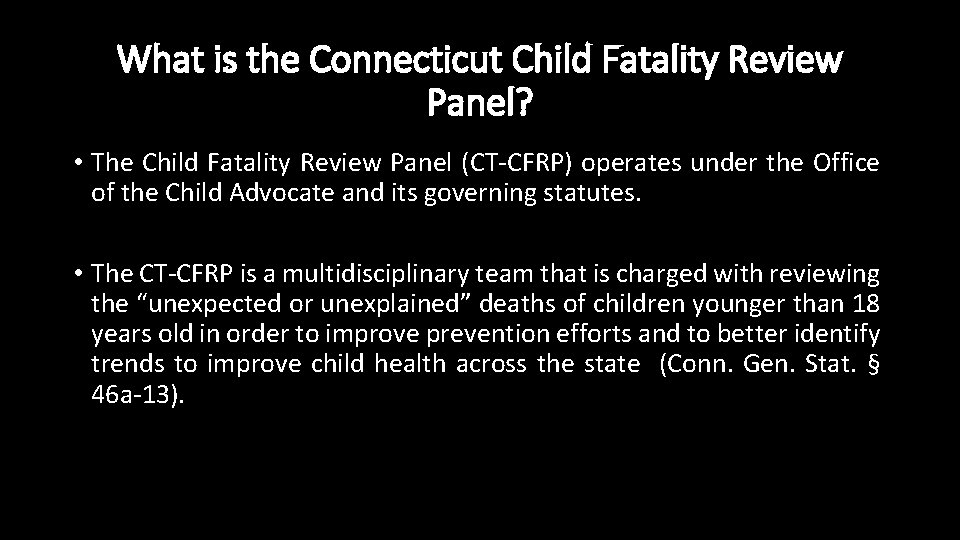
What is the Connecticut Child Fatality Review Panel? • The Child Fatality Review Panel (CT-CFRP) operates under the Office of the Child Advocate and its governing statutes. • The CT-CFRP is a multidisciplinary team that is charged with reviewing the “unexpected or unexplained” deaths of children younger than 18 years old in order to improve prevention efforts and to better identify trends to improve child health across the state (Conn. Gen. Stat. § 46 a-13).
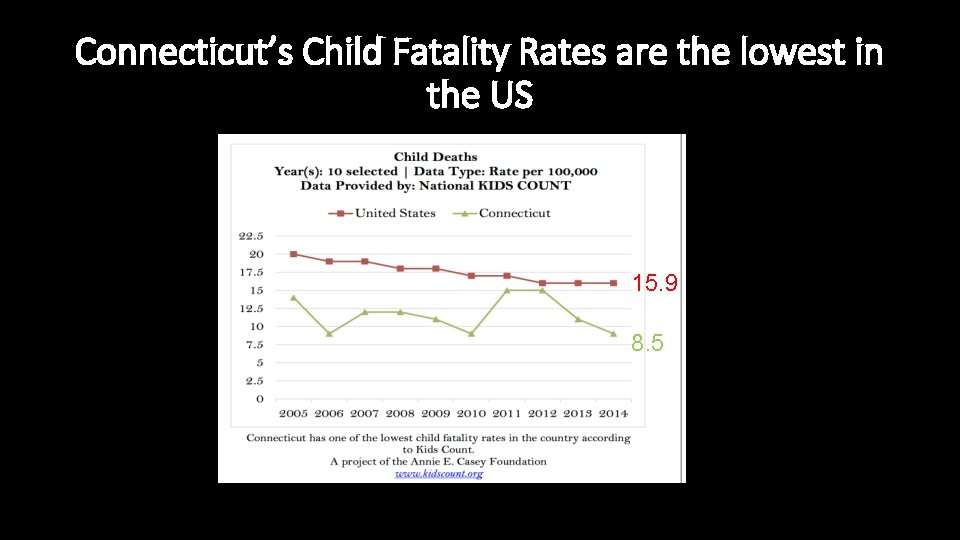
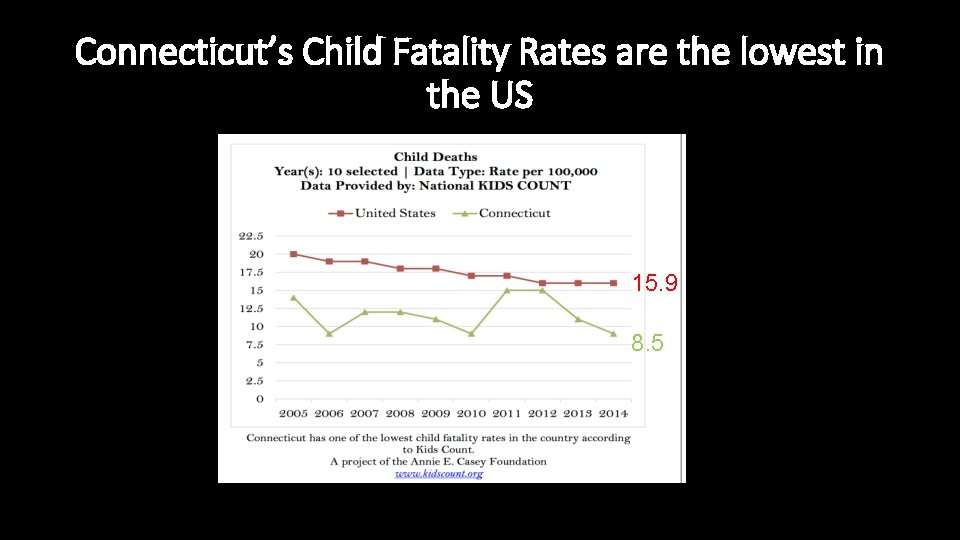
Connecticut’s Child Fatality Rates are the lowest in the US 15. 9 8. 5
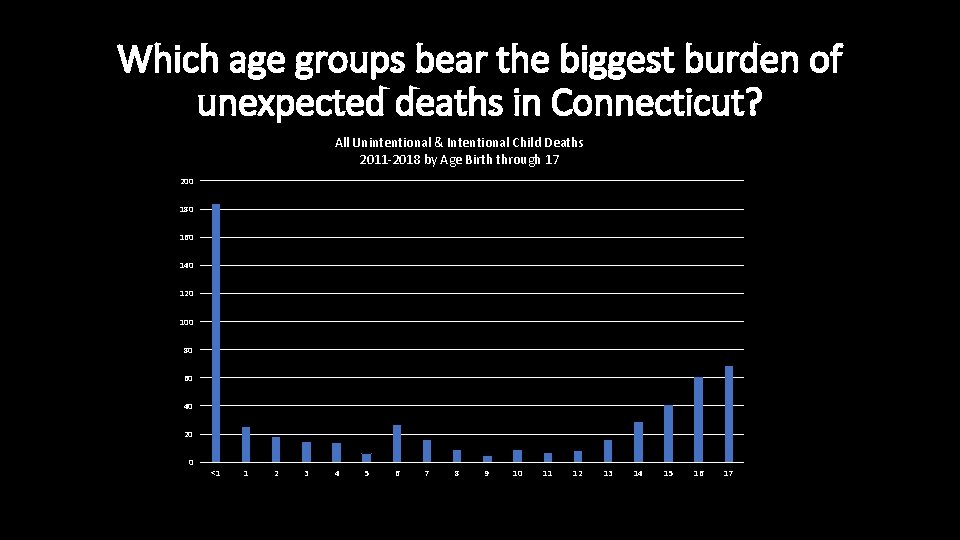
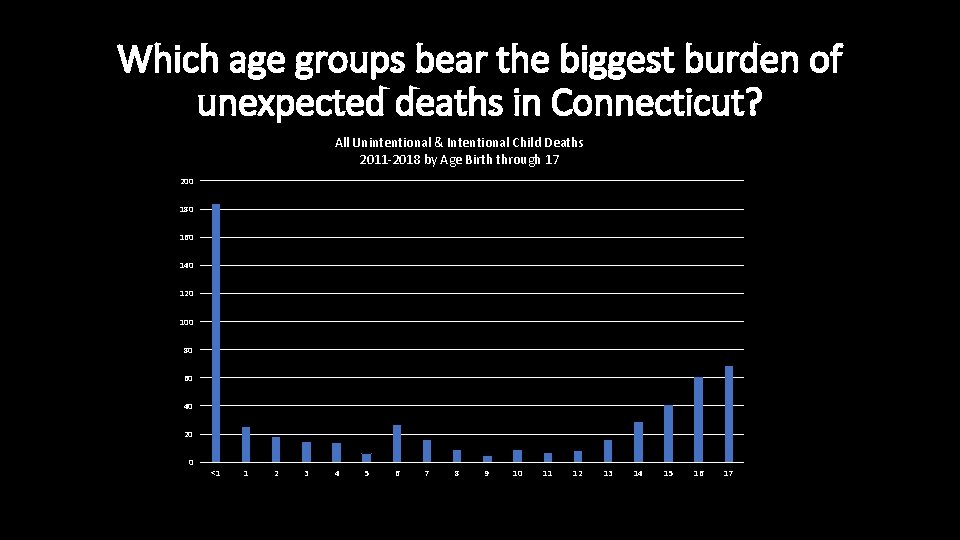
Which age groups bear the biggest burden of unexpected deaths in Connecticut? All Unintentional & Intentional Child Deaths 2011 -2018 by Age Birth through 17 200 180 160 140 120 100 80 60 40 20 0 <1 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17

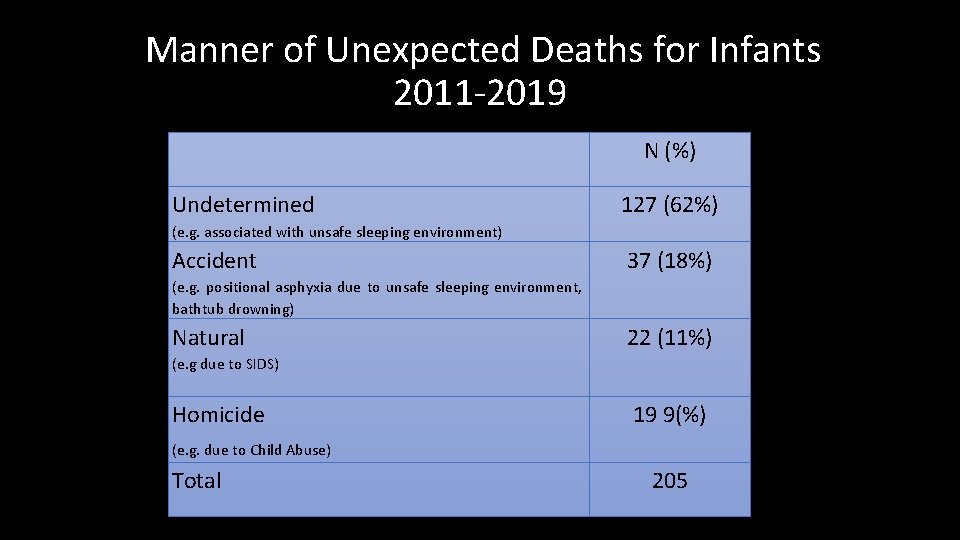
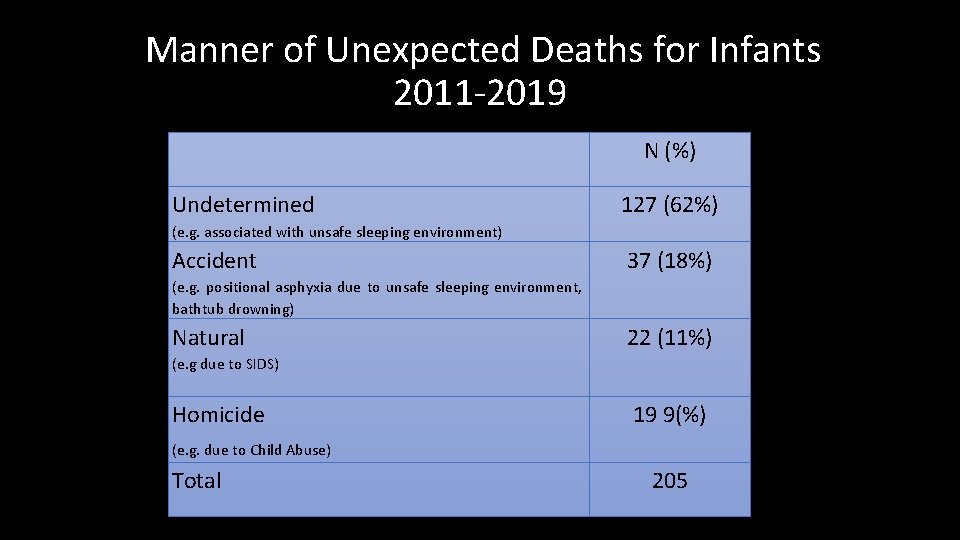
Manner of Unexpected Deaths for Infants 2011 -2019. Undetermined N (%) 127 (62%) (e. g. associated with unsafe sleeping environment) Accident 37 (18%) (e. g. positional asphyxia due to unsafe sleeping environment, bathtub drowning) Natural 22 (11%) (e. g due to SIDS) Homicide 19 9(%) (e. g. due to Child Abuse) Total 205
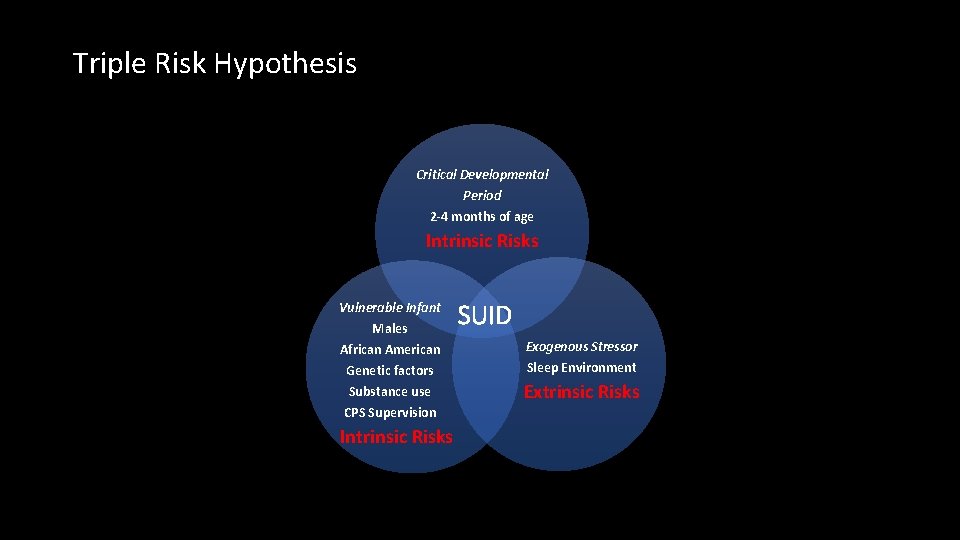
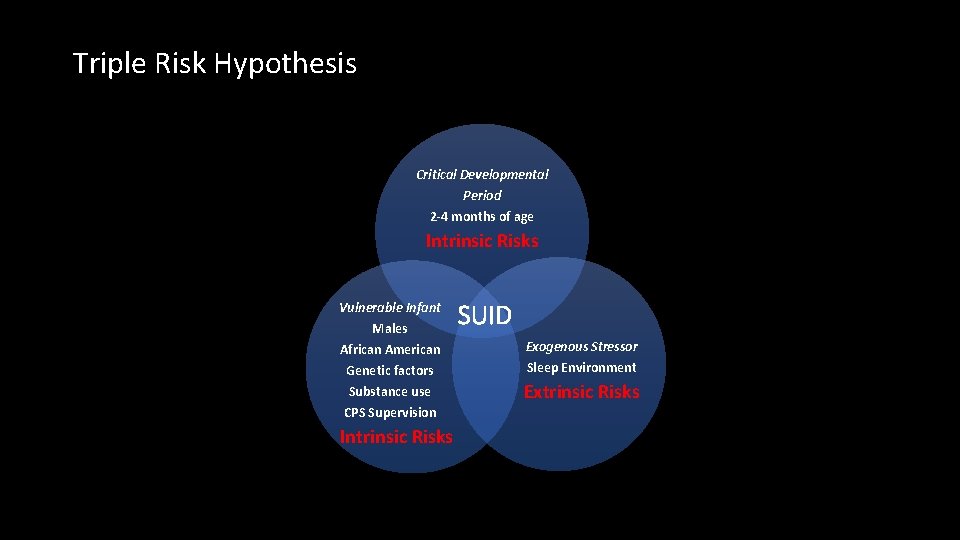
Triple Risk Hypothesis Critical Developmental Period 2 -4 months of age Intrinsic Risks Vulnerable Infant Males SUID African American Genetic factors Exogenous Stressor Substance use CPS Supervision Extrinsic Risks Intrinsic Risks Sleep Environment
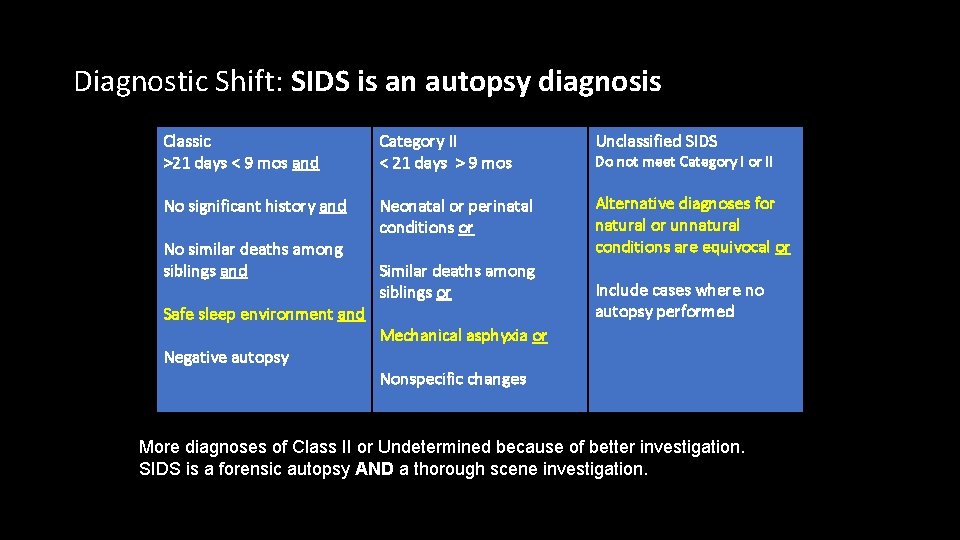
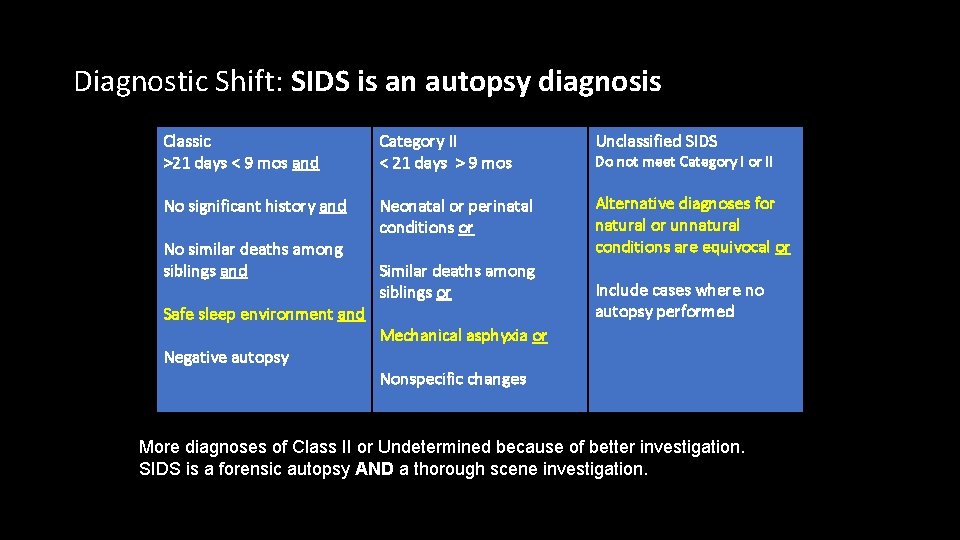
Diagnostic Shift: SIDS is an autopsy diagnosis Classic >21 days < 9 mos and Category II < 21 days > 9 mos Unclassified SIDS No significant history and Neonatal or perinatal conditions or Alternative diagnoses for natural or unnatural conditions are equivocal or No similar deaths among siblings and Safe sleep environment and Negative autopsy Similar deaths among siblings or Do not meet Category I or II Include cases where no autopsy performed Mechanical asphyxia or Nonspecific changes More diagnoses of Class II or Undetermined because of better investigation. SIDS is a forensic autopsy AND a thorough scene investigation.

SUID is the new SIDS.
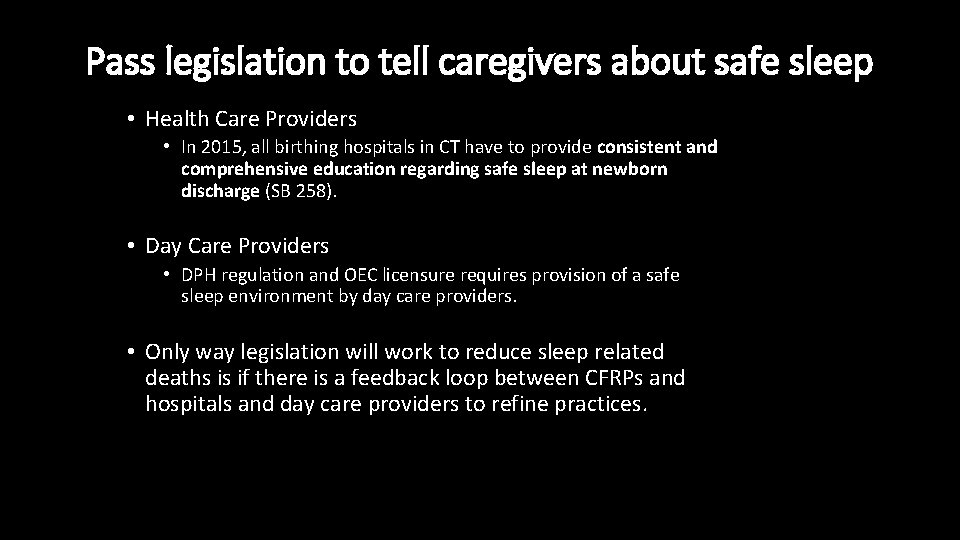
Pass legislation to tell caregivers about safe sleep • Health Care Providers • In 2015, all birthing hospitals in CT have to provide consistent and comprehensive education regarding safe sleep at newborn discharge (SB 258). • Day Care Providers • DPH regulation and OEC licensure requires provision of a safe sleep environment by day care providers. • Only way legislation will work to reduce sleep related deaths is if there is a feedback loop between CFRPs and hospitals and day care providers to refine practices.
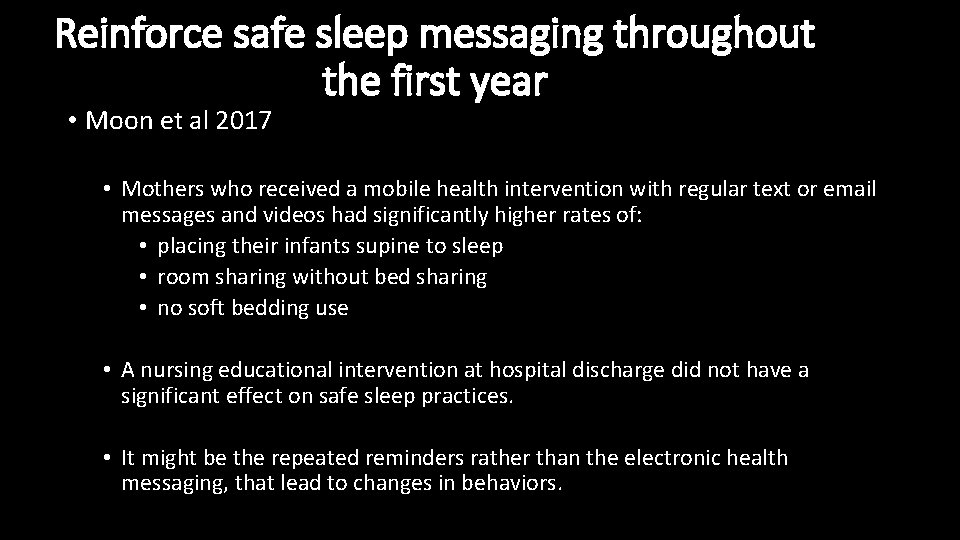
Reinforce safe sleep messaging throughout the first year • Moon et al 2017 • Mothers who received a mobile health intervention with regular text or email messages and videos had significantly higher rates of: • placing their infants supine to sleep • room sharing without bed sharing • no soft bedding use • A nursing educational intervention at hospital discharge did not have a significant effect on safe sleep practices. • It might be the repeated reminders rather than the electronic health messaging, that lead to changes in behaviors.
Give parents a crib or pack & play • Crib distribution programs improve knowledge and change practices in the majority of high-risk participants in placing an infant supine in a crib to sleep. • Crib distribution programs are helpful for newly arrived and transient families.
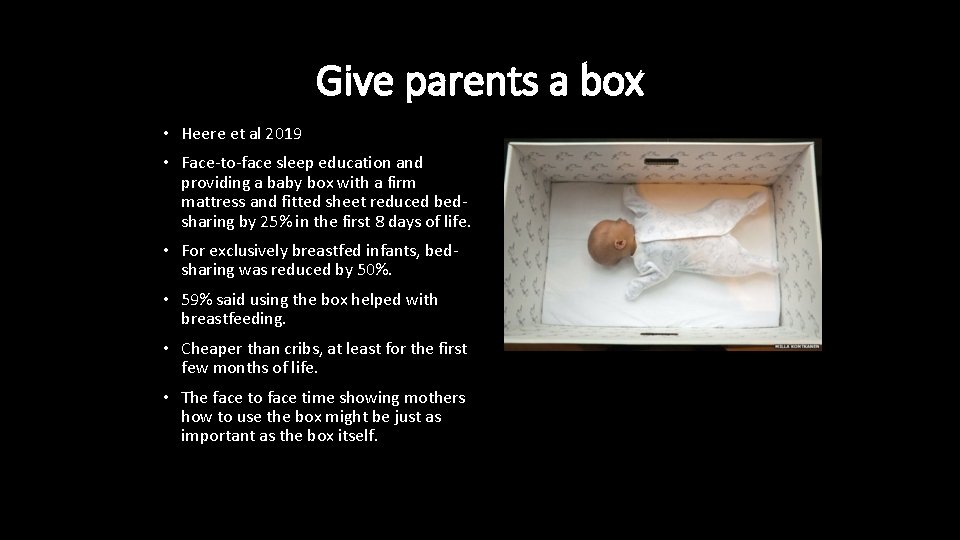
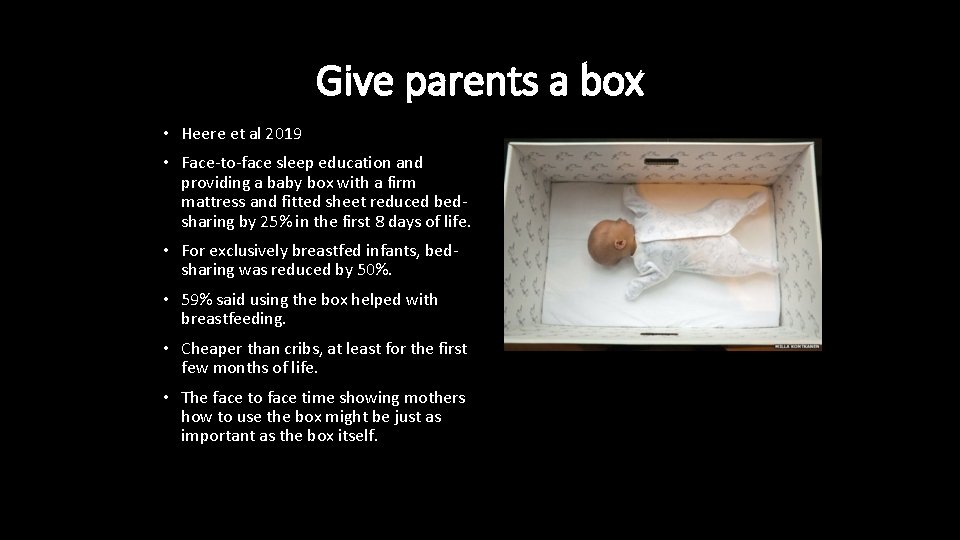
Give parents a box • Heere et al 2019 • Face-to-face sleep education and providing a baby box with a firm mattress and fitted sheet reduced bedsharing by 25% in the first 8 days of life. • For exclusively breastfed infants, bedsharing was reduced by 50%. • 59% said using the box helped with breastfeeding. • Cheaper than cribs, at least for the first few months of life. • The face to face time showing mothers how to use the box might be just as important as the box itself.
Increasing Face to Face Time Home visiting and safe sleep • CPS involvement is associated with a 3 fold increased risk for sleep related death (Putnam Hornstein et al 2014) • Infants reported to CPS have unique risks (prenatal alcohol or drug exposure, maternal behavioral health concerns) • Infants reported to CPS reflect a very high risk subset of infants born into families where there is an inadequate penetration of public health safe sleep messages. • Home Visiting by DCF is a key opportunity for face to face time for caregivers for supporting safe caregiving practices throughout the first year of life. • DCF Safe Sleep Education Curriculum
Increasing Face to Face Time Home visiting and safe sleep • Home Visiting (e. g. Nurturing Families) might be a key opportunity for face to face time to support safe caregiving practices for those not under CPS supervision. • Office of Early Childhood • Safe Sleep Curriculum for home visiting • RCT of which curriculum works best • Feedback loop via CFRP to DCF and OEC

 Livedo mortis
Livedo mortis There's a place where mercy reigns
There's a place where mercy reigns Chapter 1 an unexpected party
Chapter 1 an unexpected party Innovation and invention
Innovation and invention Unexpected challenges 1995
Unexpected challenges 1995 Terduga adalah
Terduga adalah Expected vs unexpected behaviors
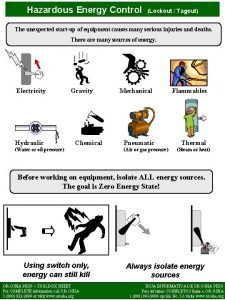
Expected vs unexpected behaviors Unexpected startup
Unexpected startup Never be predictable
Never be predictable Taste roald dahl
Taste roald dahl Lamb to the slaughter idiom
Lamb to the slaughter idiom The hobbit chapter 1
The hobbit chapter 1 Expect the unexpected
Expect the unexpected When to use polling or interrupts
When to use polling or interrupts An unexpected directx error occurred present failed
An unexpected directx error occurred present failed Sekutu perang dunia 2
Sekutu perang dunia 2 Heart of darkness part 1 analysis
Heart of darkness part 1 analysis Heart of darkness deaths
Heart of darkness deaths Bulimia face
Bulimia face Tas bdm
Tas bdm