WEAKNESS PARALYSIS Sigismund Wilkey FRCS FRCEM Pg C




- Slides: 22
WEAKNESS &PARALYSIS Sigismund Wilkey FRCS FRCEM Pg. C Med. ED
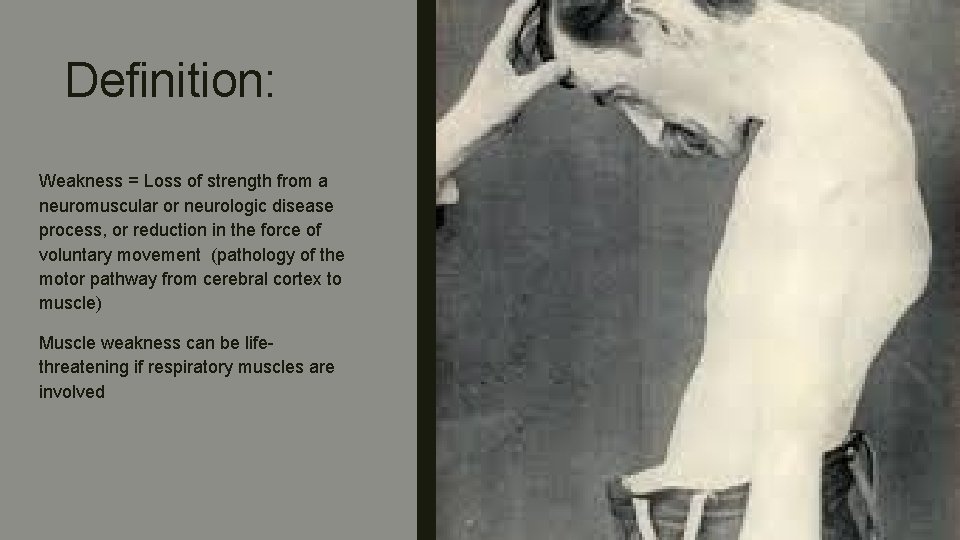
Definition: Weakness = Loss of strength from a neuromuscular or neurologic disease process, or reduction in the force of voluntary movement (pathology of the motor pathway from cerebral cortex to muscle) Muscle weakness can be lifethreatening if respiratory muscles are involved
Objectives – Summary of RCEM Curriculum (Overview of Curriculum CAP 37) ■ 45 minute overview of CAP 37 from a pragmatic ED perspective ■ Quick Revision of Anatomy & Physiology ■ Revise features and the differences between UMN, LMN and NMJ lesions ■ Explore interactively recognised approaches to the structured management of undifferentiated weakness in the ED ■ Discuss common presentations, such as Stroke and TIA ■ Classification of Stroke & Prognosis ■ National Guidelnes for TIAs and strokes ■ Emergent Investigations ■ Respiratory & Bulbar muscle weakness ■ Airway protection and Ventilatory Support ■ Discuss differential diagnoses and mimics ■ MDT Approach ■ Physiology & Neuro anatomy Revision
Upper Motor Neurone lesion ■ A lesion of the cerebral cortex or corticospinal tract – Spasticity of extension in the upper limbs and spasticity of flexion in the lower limbs – Hyperreflexia – Pronator drift – Evoked paraesthesia – Babinski positive – Normal muscle bulk
Lower Motor Neurone ■ Lesion from anterior horn to muscle – Flaccidity – Hyporeflexia – Fasciculation – Loss of muscle bulk
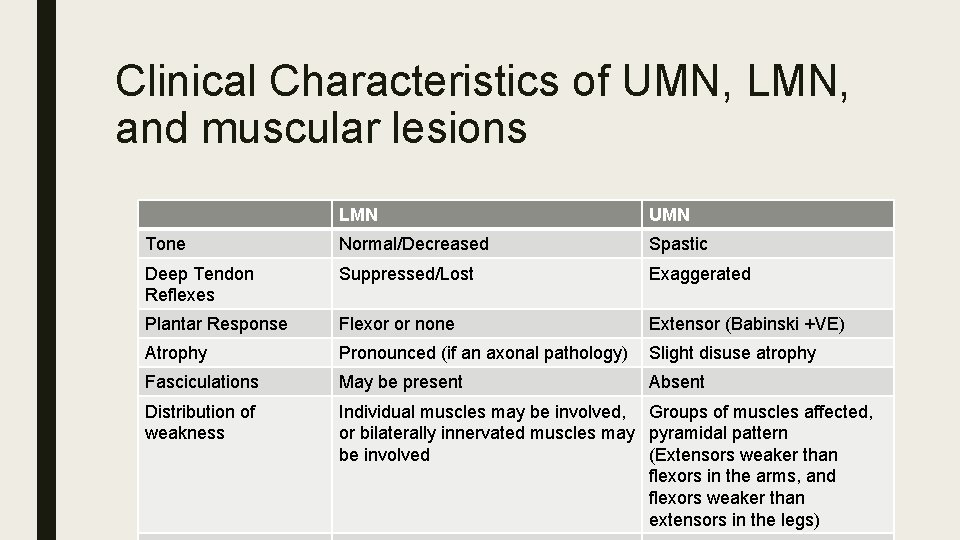
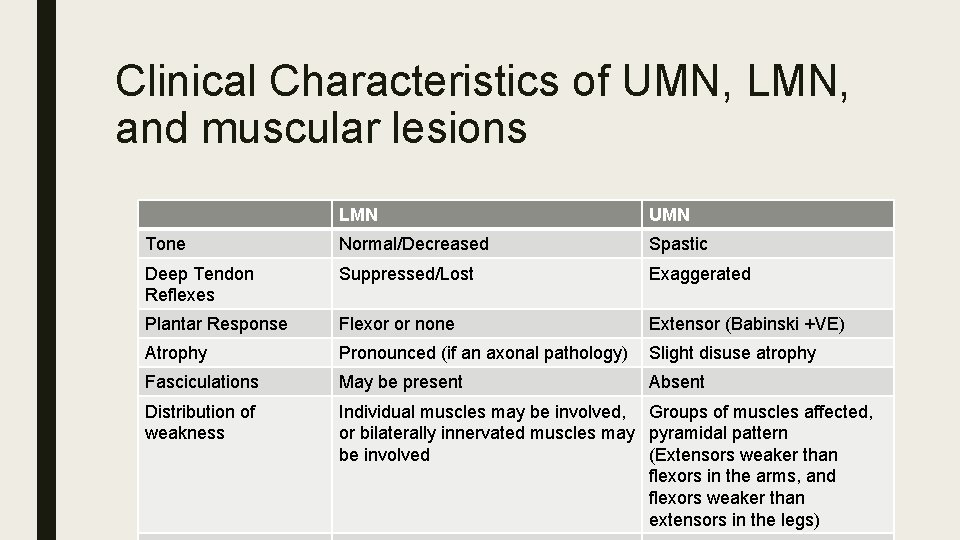
Clinical Characteristics of UMN, LMN, and muscular lesions LMN UMN Tone Normal/Decreased Spastic Deep Tendon Reflexes Suppressed/Lost Exaggerated Plantar Response Flexor or none Extensor (Babinski +VE) Atrophy Pronounced (if an axonal pathology) Slight disuse atrophy Fasciculations May be present Absent Distribution of weakness Individual muscles may be involved, Groups of muscles affected, or bilaterally innervated muscles may pyramidal pattern be involved (Extensors weaker than flexors in the arms, and flexors weaker than extensors in the legs)




Neuromuscular Junction ■ Presents with slowly progressive or fluctuating signs. It may also present with bulbar palsy or ocular signs – Bulbar palsy refers to a range of different signs and symptoms linked to impairment of function of the cranial nerves IX, X, XI and XII, which occurs due to a lower motor neuron lesion in the medulla oblongata or from lesions of the lower cranial nerves outside the brainstem – – – Mixed upper and lower motor neurone pattern Bilateral proximal muscle weakness Loss of muscle bulk
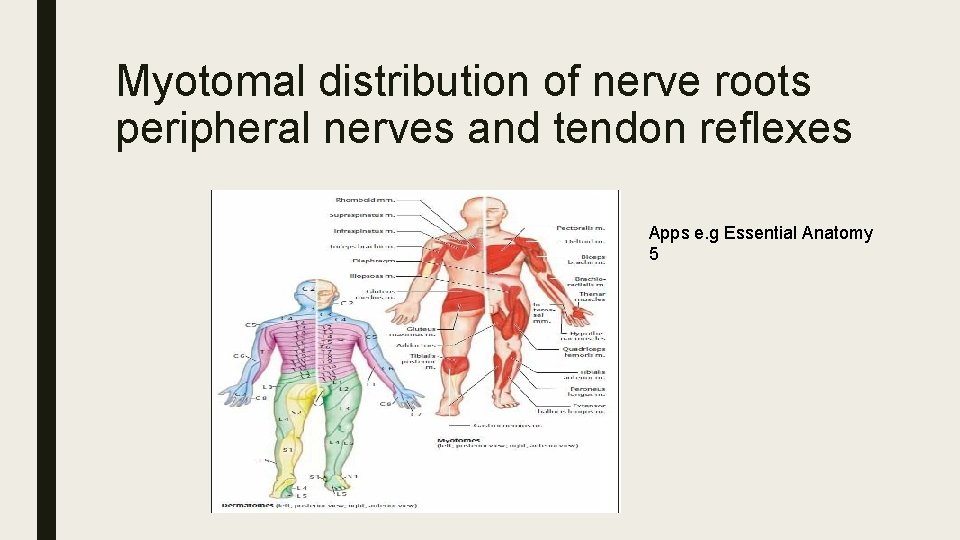
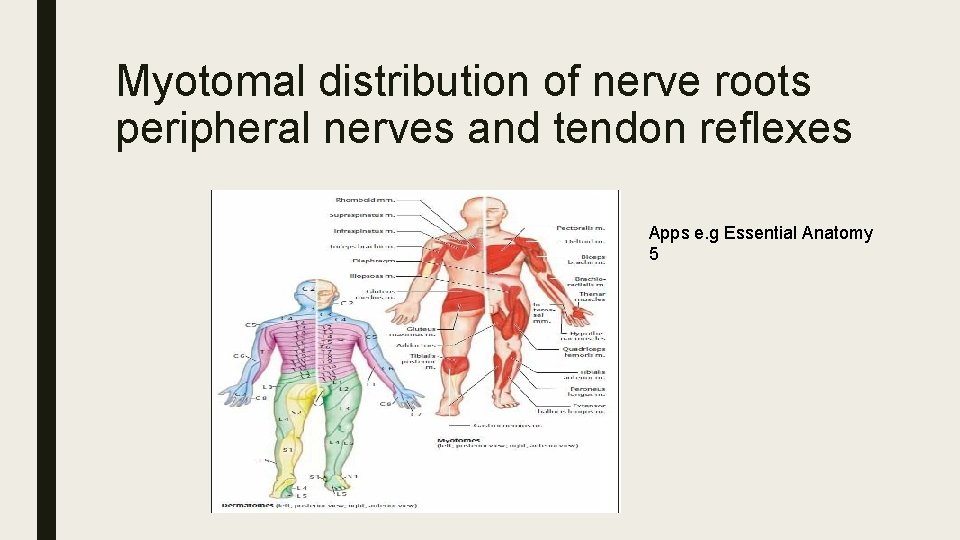
Myotomal distribution of nerve roots peripheral nerves and tendon reflexes Apps e. g Essential Anatomy 5
Structured Approach to weakness ■ Clarify what patient actually means by the term weakness ■ What muscle groups are affected ■ Timing and speed of onset ■ Associated findings ■ Exposure to medications, toxins or infectious agents? ■ Test to identify lower or upper motor neurone lesions or NMJx ■ Specialised tests (Not really for the ED)
History ■ Differentiate weakness from fatigue (general lack of energy) – ask objective questions Spatial distribution of weakness – Proximal muscle weakness, tends to be myopathic(direct damage of muscles) – Distal weakness is more likely to be a generalised polyneuropathy Associated symptoms (e. g cauda equina-like) Temporal characteristics (compare myasthenia gravis, entrapment neurpoathy or radiculopathy) Family History ■ e. g Familial Periodic Paralysis, can be associated with inherited ion chanelopathies,
Tools for the classification of stroke and it’s prognosis ■ – Stroke Teams available in most hospitals (Hyperacute stroke Guidelines) There may be 24 hour Stroke specialist nurse services, coupled with Telemedicine support out of hours – In hours there may be a stroke physician available Rosier Score should be calculated for all suspected strokes – Loss of consciousness (-1) – Syncope (-1) – New asymmetricalfacial weakness (+1) – Arm weakness (+1) – Leg Weakness (+1) – Speech disturbance (+1) – Visual field defect (+1) If the score is >= 1 treat as astroke
NIHSS Score ■ Done by stroke nurse in Hyperacute sroke units mostly ■ See proforma ■ Urgent CT scan within 1 hour ■ Ensure that plan to assess swallowing and feeding instituted ■ Manage very high systolic pressures if thrombolysis anticipated ■ Ischaemic Strokes - Thrombolyse as per local protocol ■ TIA and non-disabling strokes - Doppler and vasular surgery input ■ Haemmoragic strokes, reverse anticoagulants if possible
Implications of muscular weakness affecting the respiratory and bulbar muscles ■ Be on high alert, as respiratory failure needs to be anticipated ■ Call anaesthesia/ITU if capability not available in your ED ■ Not the ideal candidate for a stroke unit bed ■ Will need airway support to go for CT scan if needed
Airway Protection and Ventilatory support Warning signs of impending respiratory failures: Early premptive intubation needed ■ Rising Carbon dioxide ■ Decreased sensorium ■ Tachypnoea ■ Increased work of breathing, with shallow resps ■ Accessory muscle use
Timely Diagnosis and disposition Suggestions ■ Impending respiratory failure, - prepare for PPV ■ Sudden onset of focal weakness, is a stroke until proven otherwise ■ Severe headache with unilateral weakness is an SOL till proven otherwise ■ Patients with UMN that localise to the spinal cord or CST need urgent imaging (MRI) ■ If this is combined with sphincter abnormalities – Think Cauda Equina (saddle anaesthesia/paraesthesia), urinary retention, and faecal incontinennce [Beware incomplete lesions)
Investigations/Bedside tests ■ CT or CT angiogram ■ Urgent MRI ■ Residual Bladder volumes ■ CK to check for inflammatory myositis and Medication induced problems (statins) ■ Pottasium levels in suspected chanelopathies ■ High index of suspicion for strokes and SOL
Multidisciplinary Approach ■ Stroke team in Hyperacute stroke units ■ Swallow testing by ENT or other services ■ Prompt radiological input e. g CT or MRI ■ Anaesthesia/ITU ■ Rehabilitation services ■ In some cases neurolgy
Questions
 Titul frcs(t)
Titul frcs(t) Alpine course frcs
Alpine course frcs Frcsed meaning
Frcsed meaning Tympania
Tympania Chapter 23 political paralysis in the gilded age
Chapter 23 political paralysis in the gilded age Chapter 23 political paralysis in the gilded age
Chapter 23 political paralysis in the gilded age Decorticate
Decorticate Alternatives to surgery for laryngeal paralysis in dogs
Alternatives to surgery for laryngeal paralysis in dogs Cranial nerve 4 function
Cranial nerve 4 function Paralysis agitans
Paralysis agitans Chapter 23: political paralysis in the gilded age
Chapter 23: political paralysis in the gilded age Paralysis homeopathic treatment
Paralysis homeopathic treatment Paralysis cerebralis
Paralysis cerebralis Laryngeal nerve damage treatment
Laryngeal nerve damage treatment Strength and weakness of family business
Strength and weakness of family business Define sast
Define sast Disadvantages of processor
Disadvantages of processor Weakness
Weakness Grading of reflexes
Grading of reflexes A company resource weakness or competitive deficiency
A company resource weakness or competitive deficiency Strengths of marketing manager
Strengths of marketing manager Weakness of protoplanet hypothesis
Weakness of protoplanet hypothesis Nonparticipant observation
Nonparticipant observation