Cyanosis Dr Kevin Zammit MD FRCEM Emergency Medicine

- Slides: 25
Cyanosis Dr Kevin Zammit MD FRCEM Emergency Medicine Consultant Lister Hospital, Stevenage
Cyanosis
Cyanosis
What is Cyanosis?
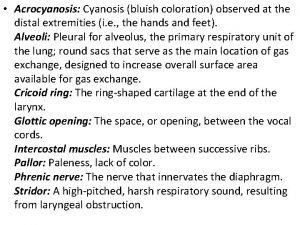
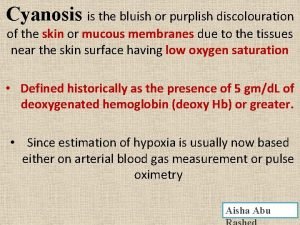
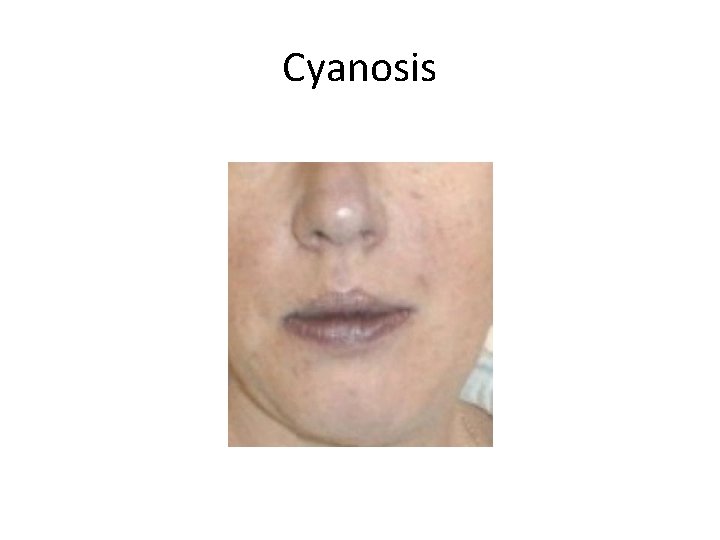
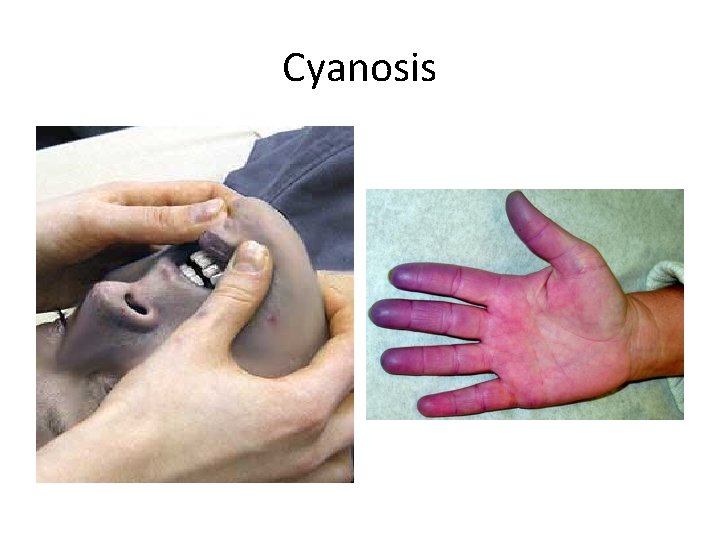
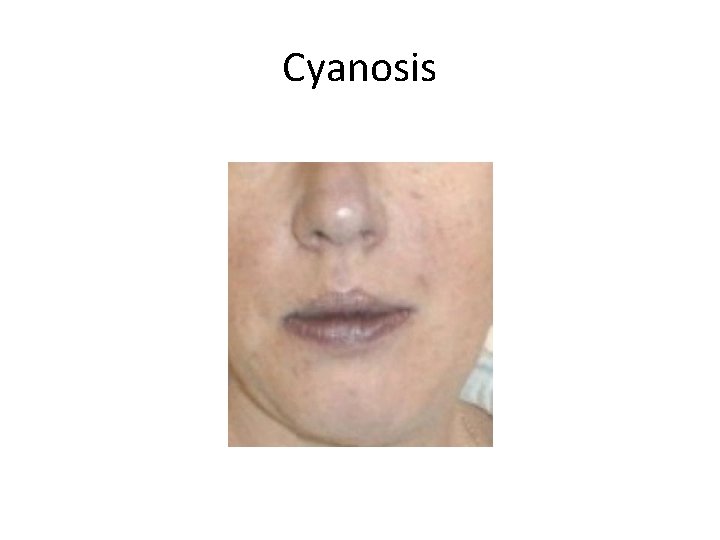
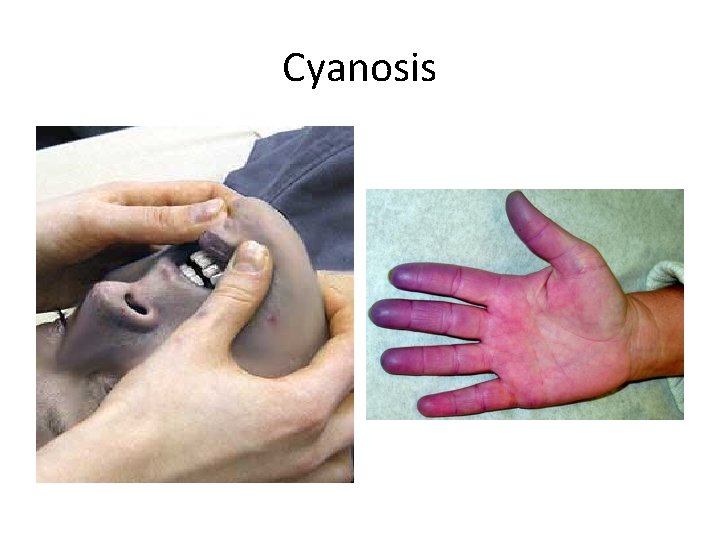
Cyanosis • Abnormal bluish discolouration of the skin and mucous membranes. • Increased amounts of bluish-coloured haemoglobin – deoxygenated haemoglobin. • Superficial vessels of the skin. • Best appreciated – lips, nose, cheeks, oral cavity (vessels abundant and overlying dermis is thin). • Central vs Peripheral – bedside decision – implies different aetiologies.
History • 1761 – Morgagni described cyanosis first in relation to pulmonary stenosis. • 1869 – Bernard described the qualitative difference in blood gases between blue venous blood and red arterial blood. • 1919 – Lundsgaard quantified how much deoxygenated haemoglobin is needed to produce cyanosis.
The blue colour • Minimal amount of deoxygenated blood is reached (2. 38 g/d. L in arterial blood). • Blue blood can be seen through the opaque dermis. • Cyanosis will remain if absolute amount of deoxygenated blood stays the same – oxyhaemoglobin concentration irrelevant. • Colour of skin depends on colour of blood flowing through dermal capillaries. • Blanches in response to pressure on skin.
The blue colour • Appearance of cyanosis depends on the absolute quantity of deoxyhaemoglobin NOT the relative amount. • If anaemic, a patient has less haemoglobin and will reach the minimal amount of deoxyhaemoglobin later than a polycythaemic patient! • Cyanosis appears later in anaemic patients than in polycythaemic patients. • Anaemic patient will be more hypoxic once cyanosis appears.
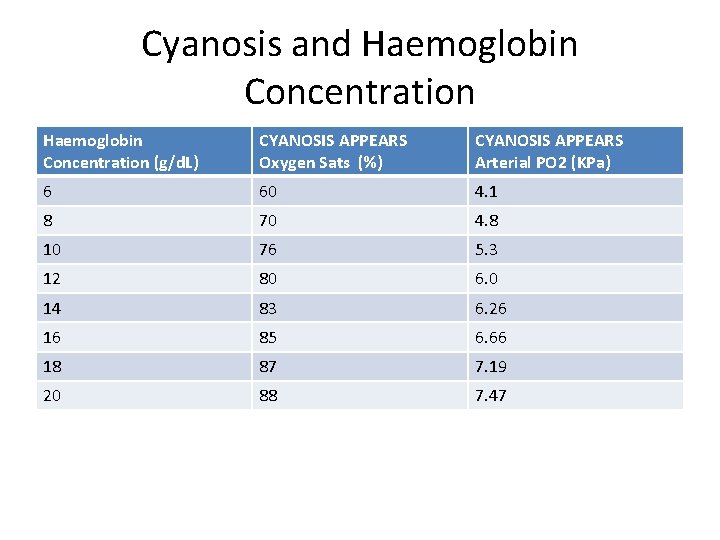
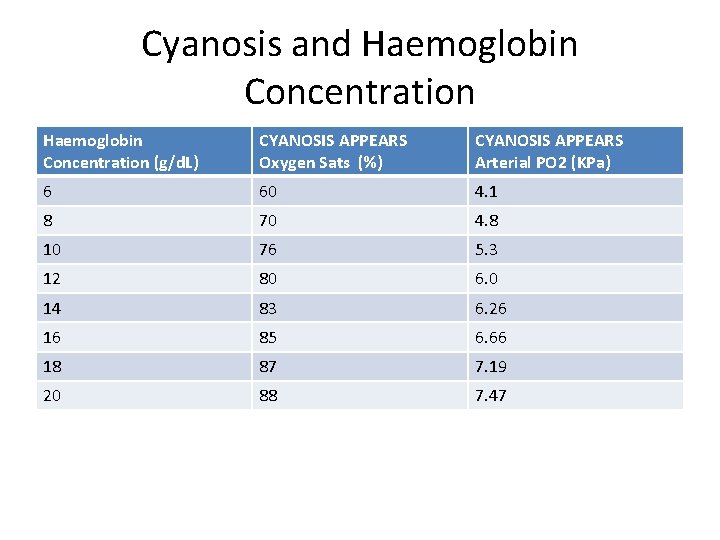
Cyanosis and Haemoglobin Concentration (g/d. L) CYANOSIS APPEARS Oxygen Sats (%) CYANOSIS APPEARS Arterial PO 2 (KPa) 6 60 4. 1 8 70 4. 8 10 76 5. 3 12 80 6. 0 14 83 6. 26 16 85 6. 66 18 87 7. 19 20 88 7. 47
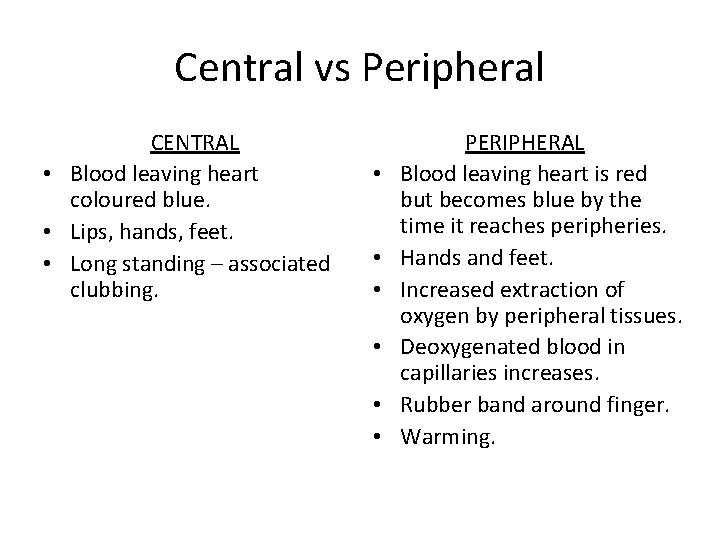
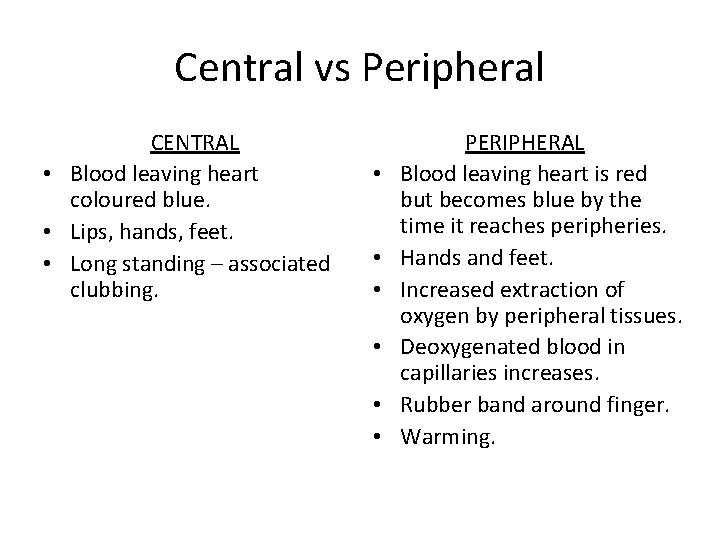
Central vs Peripheral CENTRAL • Blood leaving heart coloured blue. • Lips, hands, feet. • Long standing – associated clubbing. • • • PERIPHERAL Blood leaving heart is red but becomes blue by the time it reaches peripheries. Hands and feet. Increased extraction of oxygen by peripheral tissues. Deoxygenated blood in capillaries increases. Rubber band around finger. Warming.
Pulse oximetry / ABGs • Central cyanosis – abnormal ABGs and pulse oximetry readings. • Peripheral cyanosis – normal ABGs (proximal sampling) BUT abnormal oximetry readings.
What causes Cyanosis?
Causes of cyanosis • ANY DISORDER CAUSING HYPOXAEMIA enough to achieve the minimum absolute amount of abnormal haemoglobin (>2. 38 g/d. L arterial deoxyhaemoglobin). • INTRACARDIAC RIGHT TO LEFT SHUNTS • PERIPHERAL – low cardiac output, arterial disease, Raynaud’s disease, venous disease. • ABNORMAL HAEMOGLOBINS
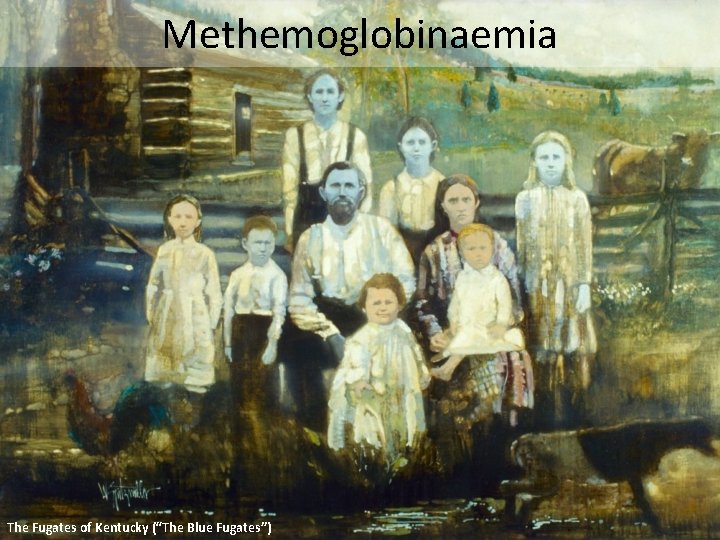
Methemoglobinaemia The Fugates of Kentucky (“The Blue Fugates”)
Methemoglobinaemia • Congenital or Acquired • Chocolate cyanosis (brownish hue) • ABGs will show normal Pa. O 2. • Does not improve with oxygen therapy. • Severity of symptoms depends on quantity, rapidity of onset and presence of comorbidities. • Reversible with Methylene blue.
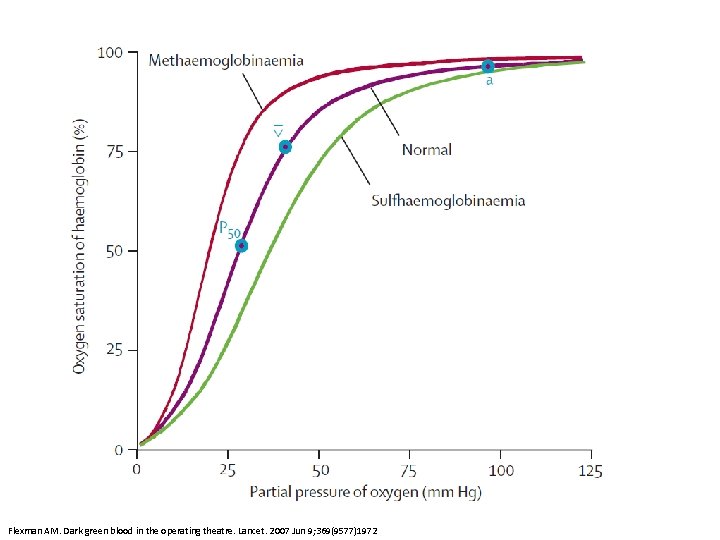
Sulfhemoglobinaemia
Causes Sulfhemoglobinaemia • Phenacetin • Industrial aniline compounds • Rare due to improved occupational health standards • Irreversible. • • Methemoglobinaemia Hereditary – NADH methemoglobin reductase Benzocaine Nitrates Nitrites
Carboxyhaemoglobinaemia • Does not cause real cyanosis • Cherry red colour of the skin?
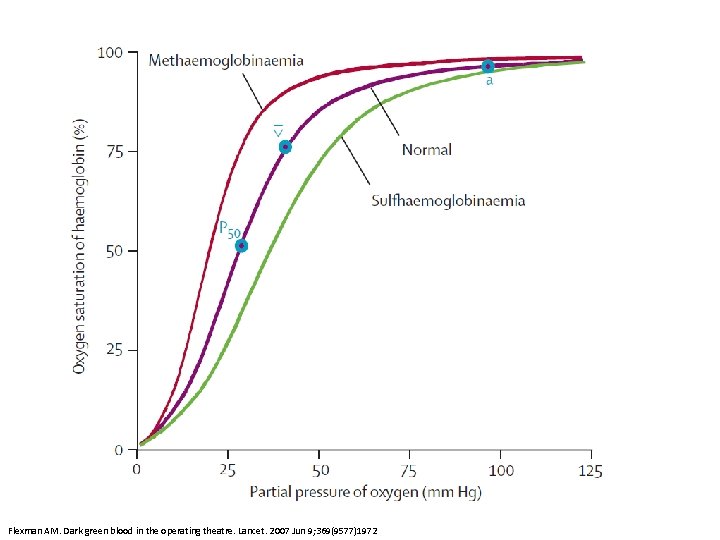
Flexman AM. Dark green blood in the operating theatre. Lancet. 2007 Jun 9; 369(9577)1972
Pseudocyanosis
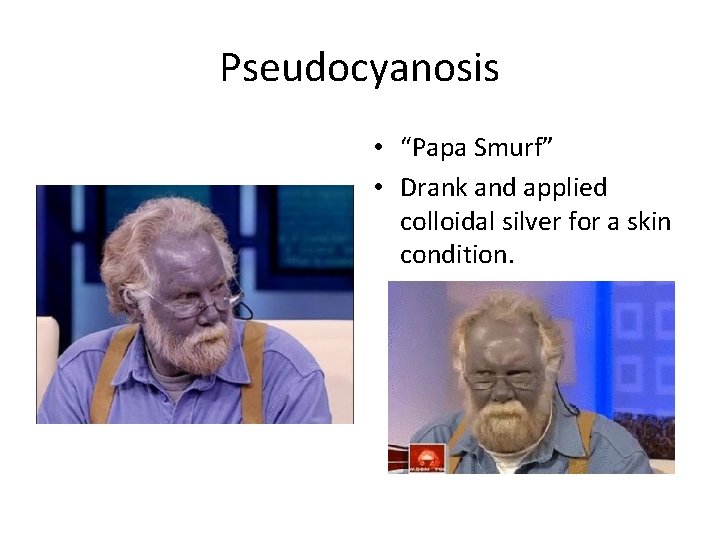
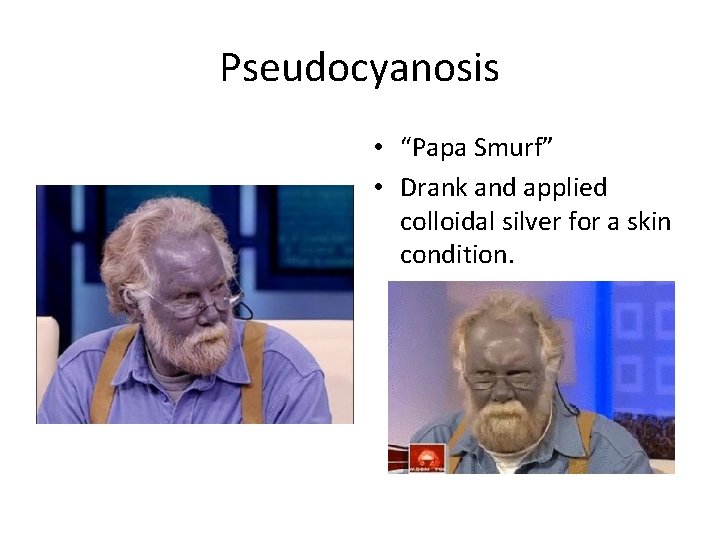
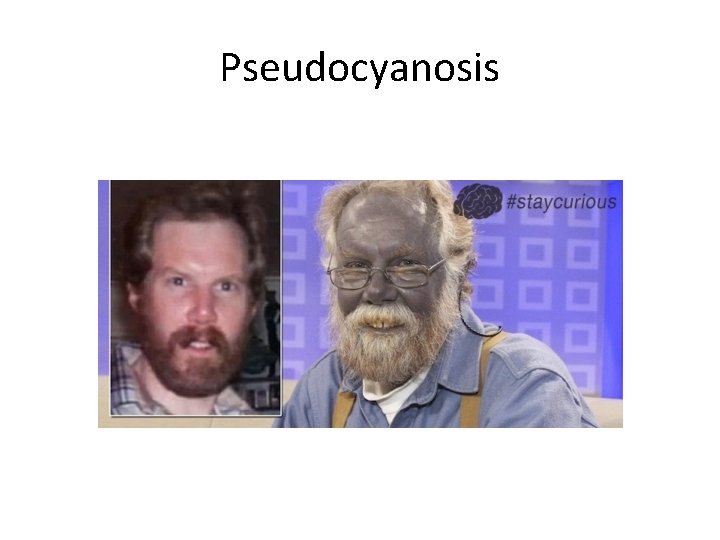
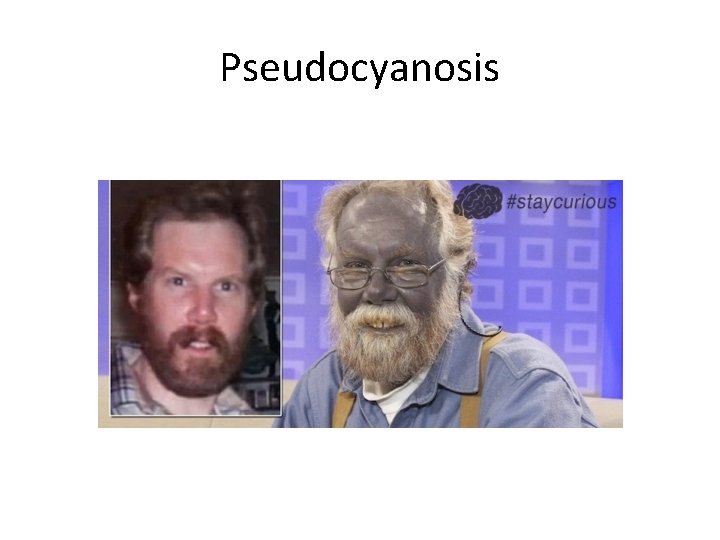
Pseudocyanosis • “Papa Smurf” • Drank and applied colloidal silver for a skin condition.
Pseudocyanosis
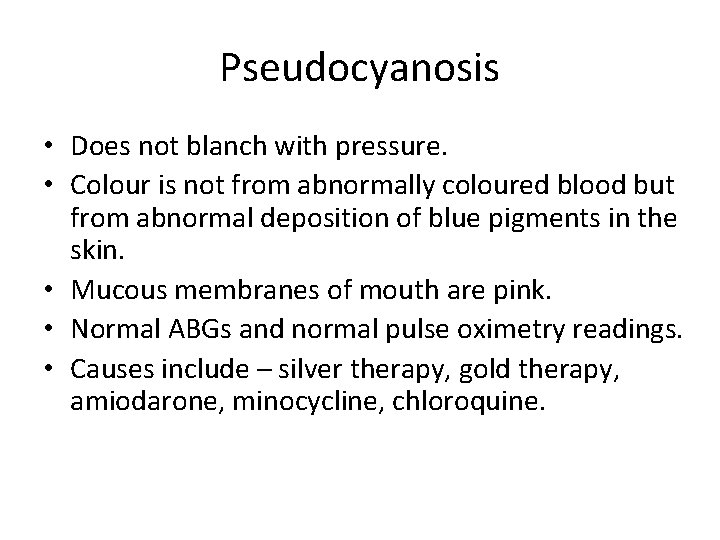
Pseudocyanosis • Does not blanch with pressure. • Colour is not from abnormally coloured blood but from abnormal deposition of blue pigments in the skin. • Mucous membranes of mouth are pink. • Normal ABGs and normal pulse oximetry readings. • Causes include – silver therapy, gold therapy, amiodarone, minocycline, chloroquine.

Summary • LATE SIGN – prevent it if possible. • OXYGEN! • If no improvement with oxygen, think of differential diagnosis.
 Verbe crire
Verbe crire Samantha zammit
Samantha zammit Cyanosis types
Cyanosis types Causes of cyanosis
Causes of cyanosis Two types of cyanosis
Two types of cyanosis Central cyanosis in newborn when crying
Central cyanosis in newborn when crying Cyanotic congenital heart disease
Cyanotic congenital heart disease Cyanosis causes
Cyanosis causes Cyanosis
Cyanosis Pallor cyanosis
Pallor cyanosis Dutch north sea emergency medicine conference
Dutch north sea emergency medicine conference Unm emergency medicine residents
Unm emergency medicine residents Cmc vellore emergency medicine
Cmc vellore emergency medicine University of arizona emergency medicine
University of arizona emergency medicine Emergency medicine case presentation
Emergency medicine case presentation Kevin schwendemann
Kevin schwendemann Kevin salcido asu
Kevin salcido asu Kevin paprocki
Kevin paprocki Kevin torres muerte
Kevin torres muerte Adcb inr rate
Adcb inr rate Kevin lin cmu
Kevin lin cmu Kevin murphy color wheel
Kevin murphy color wheel Kevin himpe
Kevin himpe Kevin debow
Kevin debow Kevin robinson millersville
Kevin robinson millersville Pgm
Pgm