Treatment Principles Alzheimers Disease AD Treatment goals in


- Slides: 32

Treatment Principles Alzheimer’s Disease (AD)
Treatment goals in AD
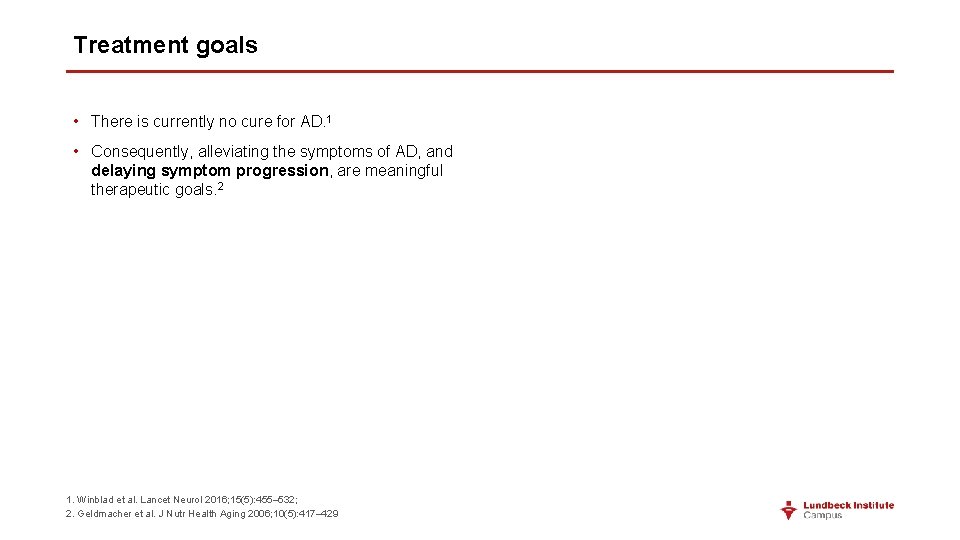
Treatment goals • There is currently no cure for AD. 1 • Consequently, alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. 2 1. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 2. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429
Treatment goals • There is currently no cure for AD. 1 • Consequently, alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. 2 • Ideally, the patient should be maintained as close as possible to their cognitive, functional, and behavioral status at diagnosis, for as long as possible. 2 • In mild AD, treatment outcomes should focus on memory functions. 1 In more severe AD, effects on activities of daily living (ADLs) and psychiatric and behavioral disturbances are more clinically relevant. 1 • Patients and families may find the real-life benefits of treatment to be the most meaningful, such as the ability to complete household tasks, to enjoy hobbies, and to participate in family activities. 2 1. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 2. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429
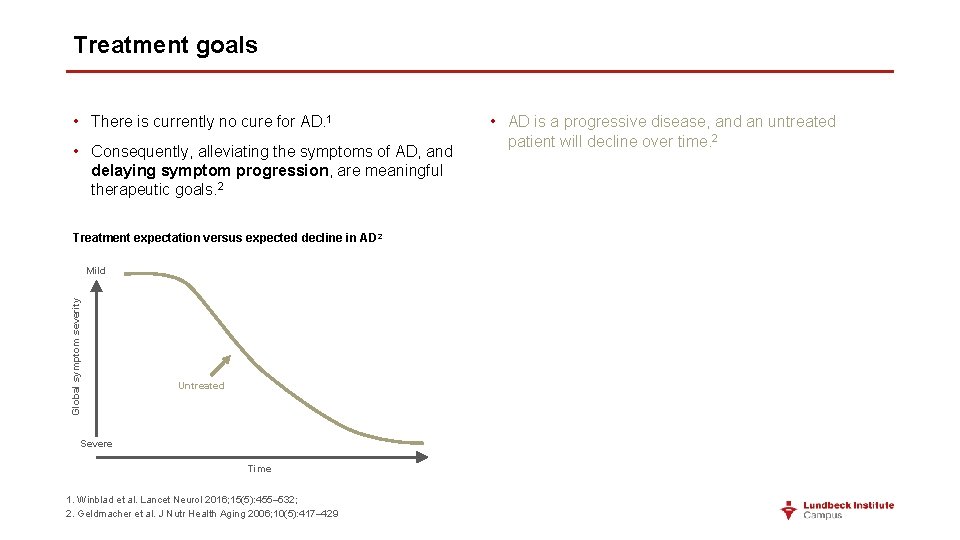
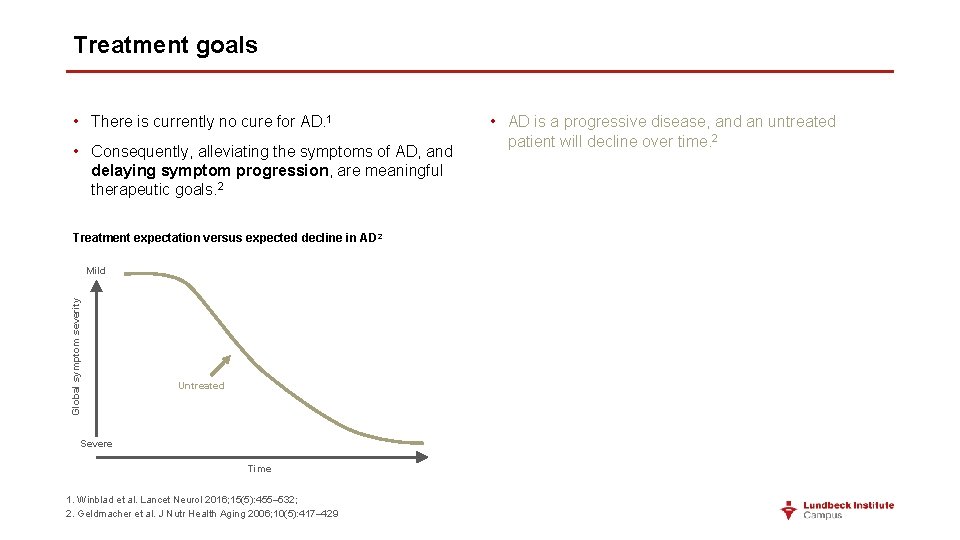
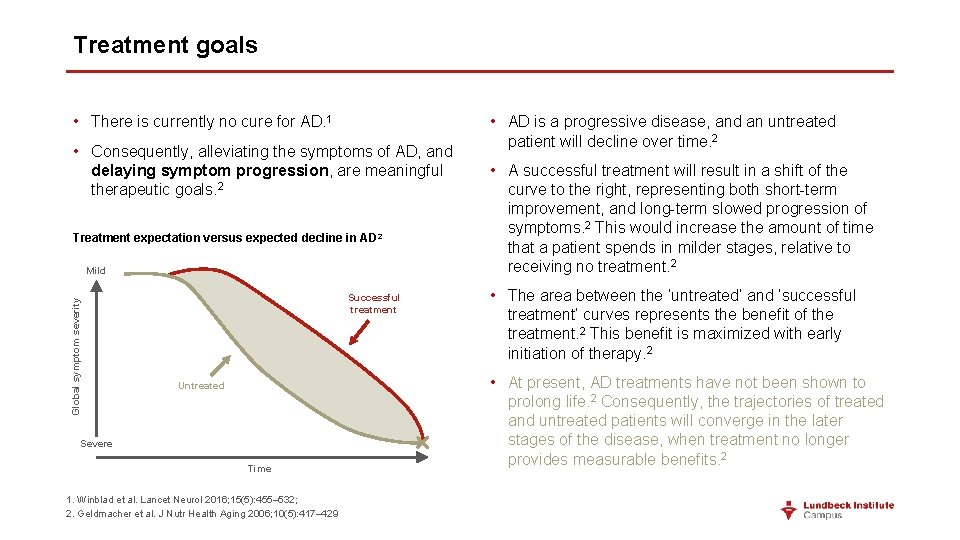
Treatment goals • There is currently no cure for AD. 1 • Consequently, alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. 2 Treatment expectation versus expected decline in AD 2 Global symptom severity Mild Untreated Severe Time 1. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 2. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429 • AD is a progressive disease, and an untreated patient will decline over time. 2
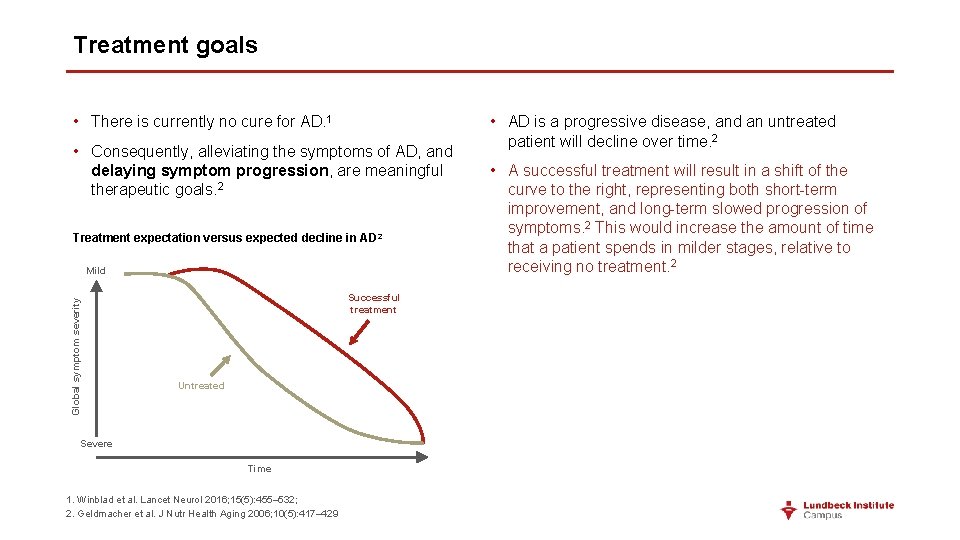
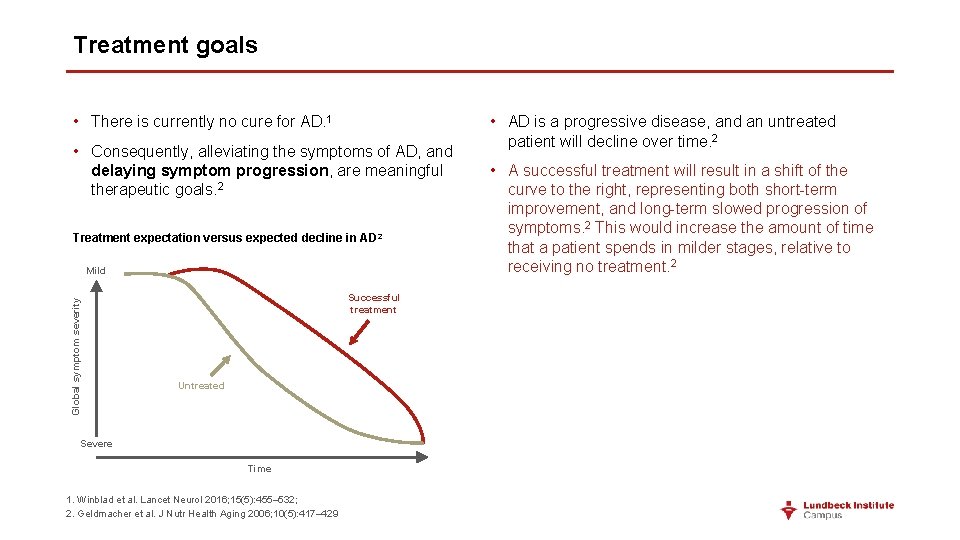
Treatment goals • There is currently no cure for AD. 1 • Consequently, alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. 2 Treatment expectation versus expected decline in AD 2 Global symptom severity Mild Successful treatment Untreated Severe Time 1. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 2. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429 • AD is a progressive disease, and an untreated patient will decline over time. 2 • A successful treatment will result in a shift of the curve to the right, representing both short-term improvement, and long-term slowed progression of symptoms. 2 This would increase the amount of time that a patient spends in milder stages, relative to receiving no treatment. 2
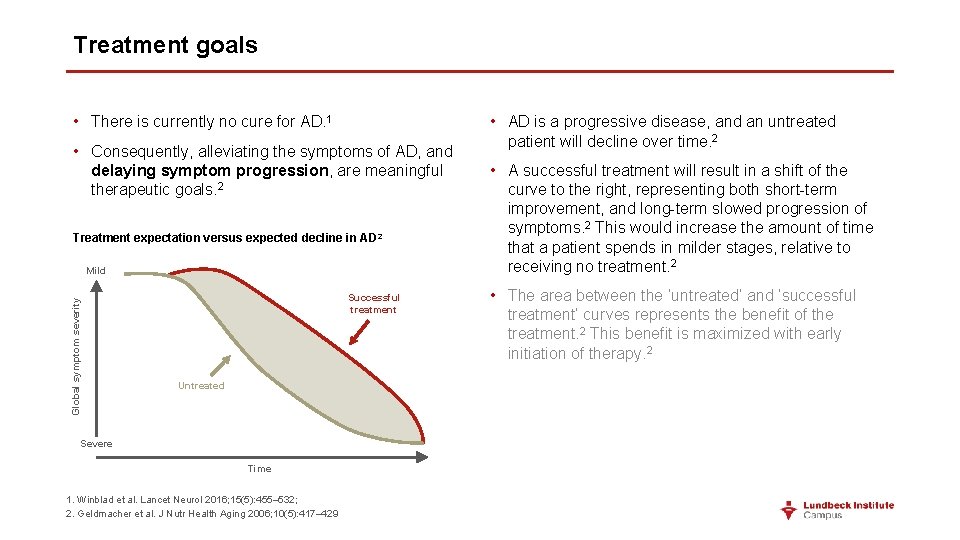
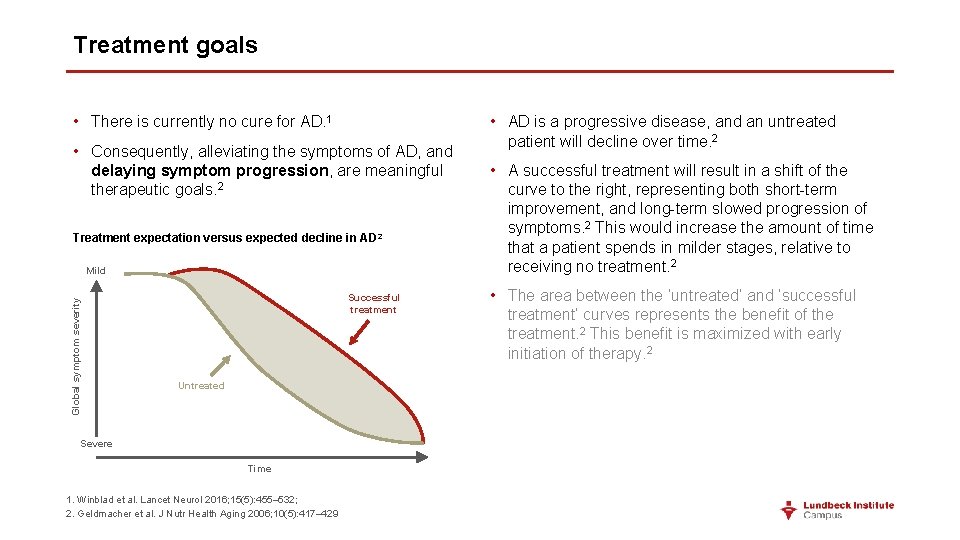
Treatment goals • There is currently no cure for AD. 1 • Consequently, alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. 2 Treatment expectation versus expected decline in AD 2 Global symptom severity Mild Successful treatment Untreated Severe Time 1. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 2. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429 • AD is a progressive disease, and an untreated patient will decline over time. 2 • A successful treatment will result in a shift of the curve to the right, representing both short-term improvement, and long-term slowed progression of symptoms. 2 This would increase the amount of time that a patient spends in milder stages, relative to receiving no treatment. 2 • The area between the ‘untreated’ and ‘successful treatment’ curves represents the benefit of the treatment. 2 This benefit is maximized with early initiation of therapy. 2
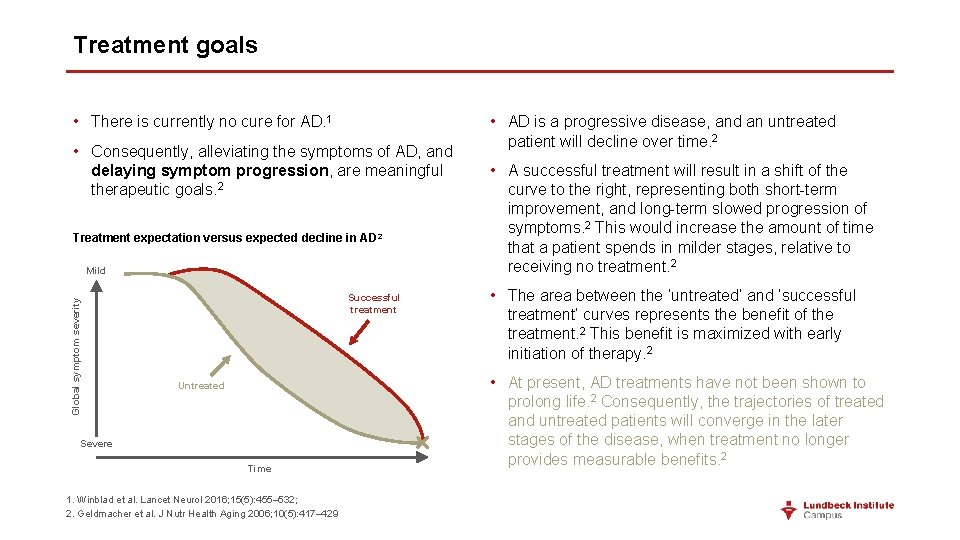
Treatment goals • There is currently no cure for AD. 1 • Consequently, alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. 2 Treatment expectation versus expected decline in AD 2 Global symptom severity Mild Successful treatment Untreated Severe Time 1. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 2. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429 • AD is a progressive disease, and an untreated patient will decline over time. 2 • A successful treatment will result in a shift of the curve to the right, representing both short-term improvement, and long-term slowed progression of symptoms. 2 This would increase the amount of time that a patient spends in milder stages, relative to receiving no treatment. 2 • The area between the ‘untreated’ and ‘successful treatment’ curves represents the benefit of the treatment. 2 This benefit is maximized with early initiation of therapy. 2 • At present, AD treatments have not been shown to prolong life. 2 Consequently, the trajectories of treated and untreated patients will converge in the later stages of the disease, when treatment no longer provides measurable benefits. 2
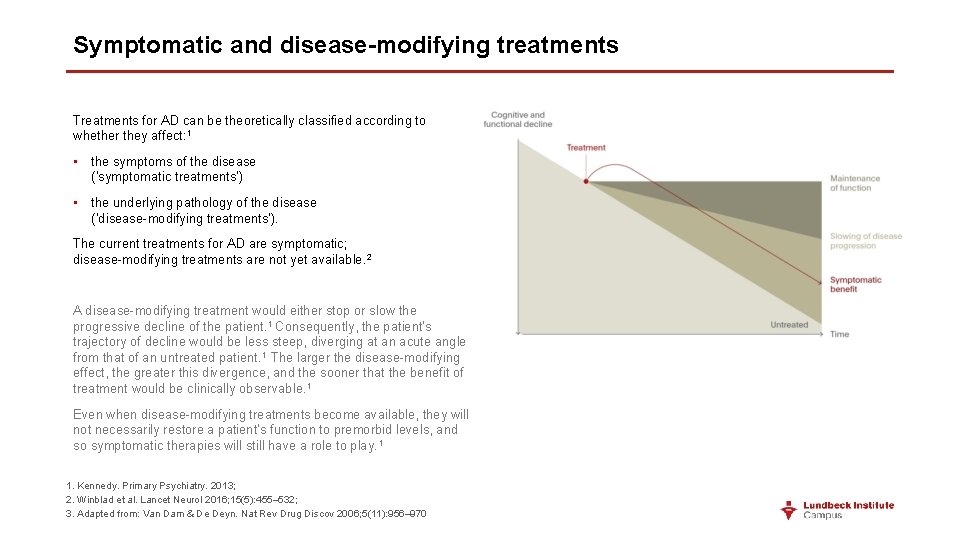
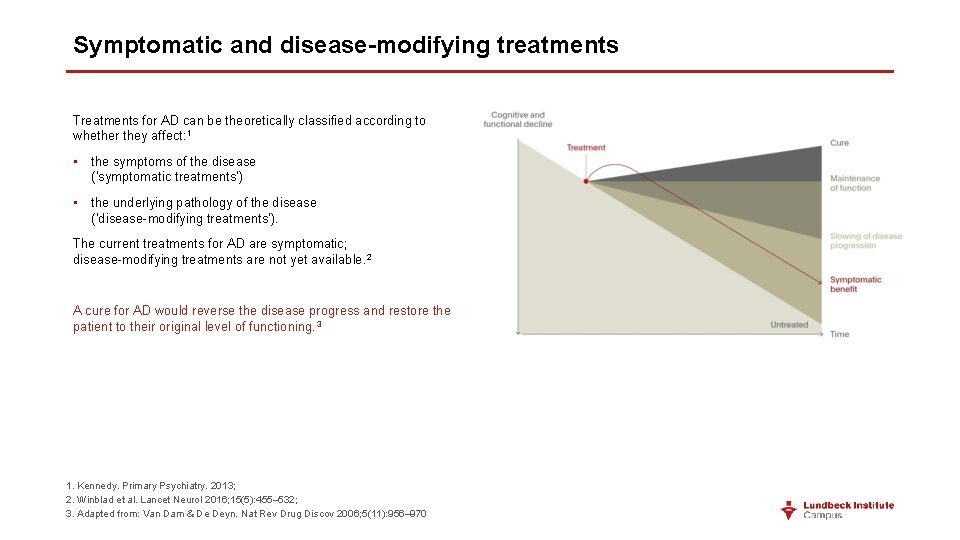
Symptomatic and disease-modifying treatments Treatments for AD can be theoretically classified according to whether they affect: 1 • the symptoms of the disease (‘symptomatic treatments’) • the underlying pathology of the disease (‘disease-modifying treatments’). The current treatments for AD are symptomatic; disease-modifying treatments are not yet available. 2 1. Kennedy. Primary Psychiatry. 2013; 2. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 3. Adapted from: Van Dam & De Deyn. Nat Rev Drug Discov 2006; 5(11): 956– 970
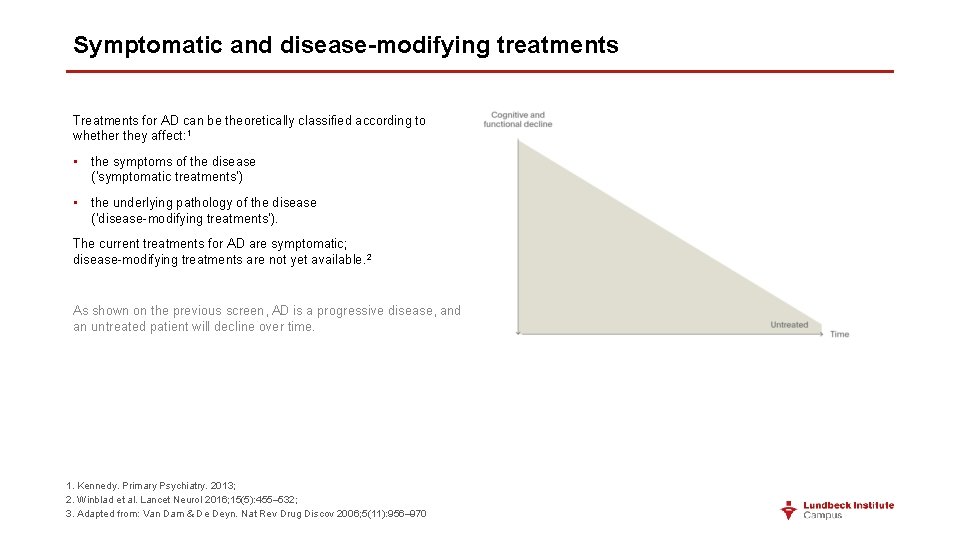
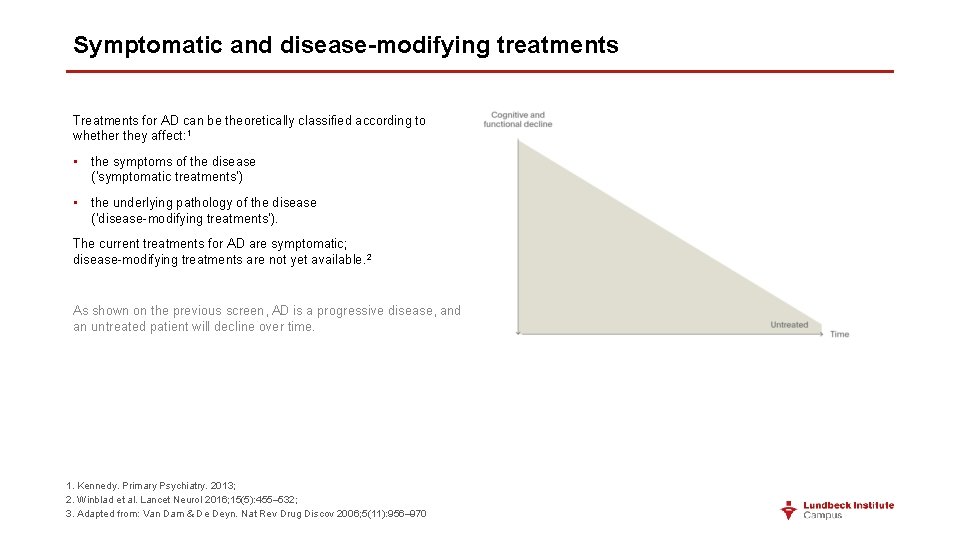
Symptomatic and disease-modifying treatments Treatments for AD can be theoretically classified according to whether they affect: 1 • the symptoms of the disease (‘symptomatic treatments’) • the underlying pathology of the disease (‘disease-modifying treatments’). The current treatments for AD are symptomatic; disease-modifying treatments are not yet available. 2 As shown on the previous screen, AD is a progressive disease, and an untreated patient will decline over time. 1. Kennedy. Primary Psychiatry. 2013; 2. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 3. Adapted from: Van Dam & De Deyn. Nat Rev Drug Discov 2006; 5(11): 956– 970
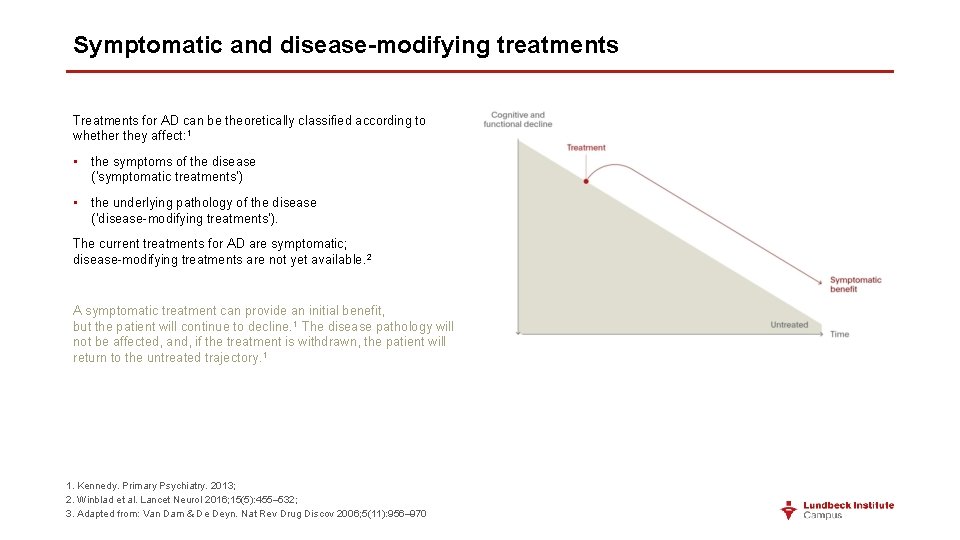
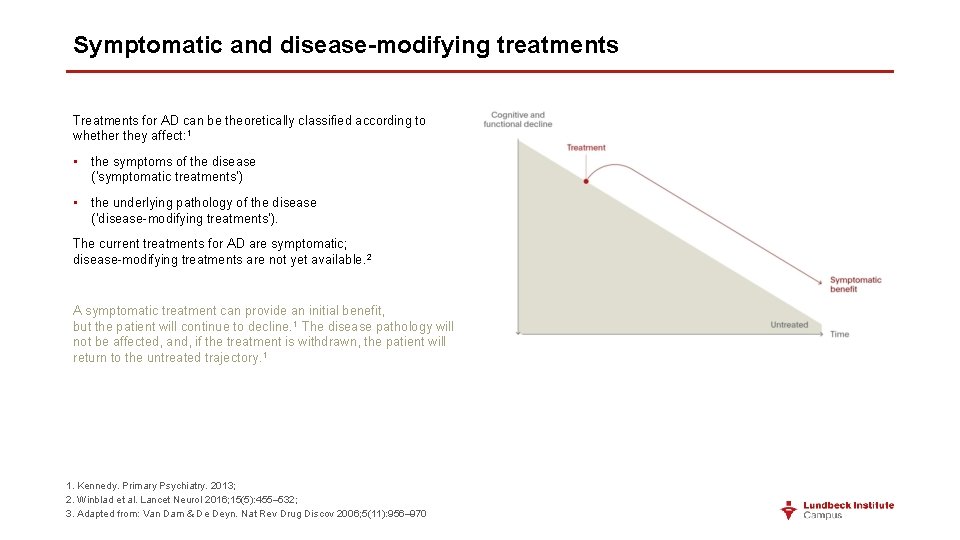
Symptomatic and disease-modifying treatments Treatments for AD can be theoretically classified according to whether they affect: 1 • the symptoms of the disease (‘symptomatic treatments’) • the underlying pathology of the disease (‘disease-modifying treatments’). The current treatments for AD are symptomatic; disease-modifying treatments are not yet available. 2 A symptomatic treatment can provide an initial benefit, but the patient will continue to decline. 1 The disease pathology will not be affected, and, if the treatment is withdrawn, the patient will return to the untreated trajectory. 1 1. Kennedy. Primary Psychiatry. 2013; 2. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 3. Adapted from: Van Dam & De Deyn. Nat Rev Drug Discov 2006; 5(11): 956– 970
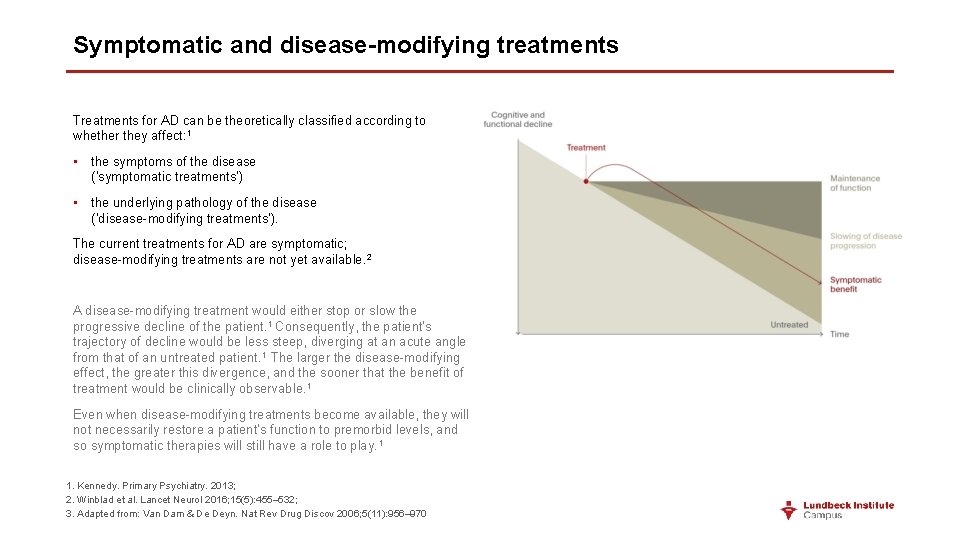
Symptomatic and disease-modifying treatments Treatments for AD can be theoretically classified according to whether they affect: 1 • the symptoms of the disease (‘symptomatic treatments’) • the underlying pathology of the disease (‘disease-modifying treatments’). The current treatments for AD are symptomatic; disease-modifying treatments are not yet available. 2 A disease-modifying treatment would either stop or slow the progressive decline of the patient. 1 Consequently, the patient’s trajectory of decline would be less steep, diverging at an acute angle from that of an untreated patient. 1 The larger the disease-modifying effect, the greater this divergence, and the sooner that the benefit of treatment would be clinically observable. 1 Even when disease-modifying treatments become available, they will not necessarily restore a patient’s function to premorbid levels, and so symptomatic therapies will still have a role to play. 1 1. Kennedy. Primary Psychiatry. 2013; 2. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 3. Adapted from: Van Dam & De Deyn. Nat Rev Drug Discov 2006; 5(11): 956– 970
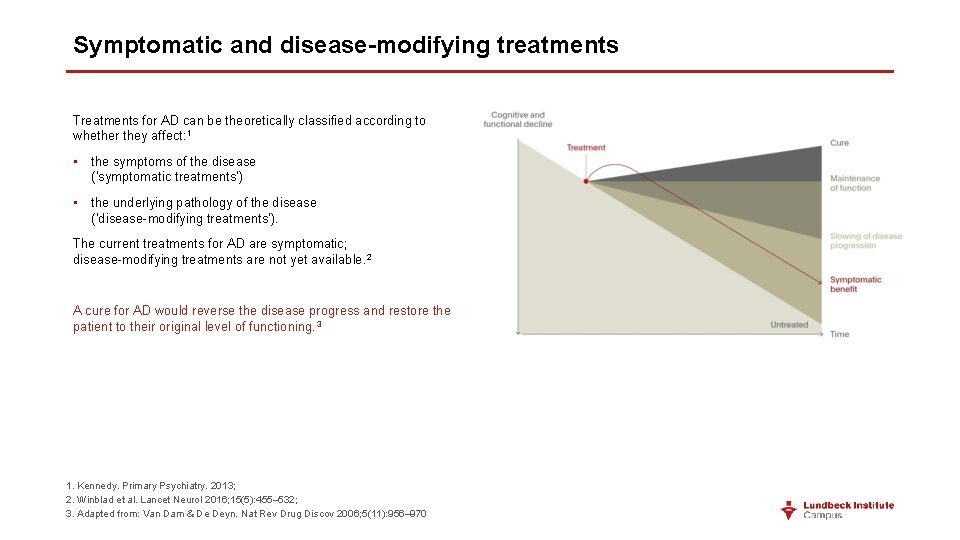
Symptomatic and disease-modifying treatments Treatments for AD can be theoretically classified according to whether they affect: 1 • the symptoms of the disease (‘symptomatic treatments’) • the underlying pathology of the disease (‘disease-modifying treatments’). The current treatments for AD are symptomatic; disease-modifying treatments are not yet available. 2 A cure for AD would reverse the disease progress and restore the patient to their original level of functioning. 3 1. Kennedy. Primary Psychiatry. 2013; 2. Winblad et al. Lancet Neurol 2016; 15(5): 455– 532; 3. Adapted from: Van Dam & De Deyn. Nat Rev Drug Discov 2006; 5(11): 956– 970
Key points • Current treatments for AD are symptomatic; there is no cure, or disease-modifying treatment, that can affect the underlying pathology of the disease. • Alleviating the symptoms of AD, and delaying symptom progression, are meaningful therapeutic goals. • Even when disease-modifying treatments become available, they will not necessarily restore a patient’s function to premorbid levels – symptomatic therapies will still have a role to play.
Current approaches to AD management
Current approaches to AD management • The management of AD can be categorized into pharmacological, psychosocial, and caregiving aspects. Pharmacological Psychosocial Caregiving • Dementia is a progressive disorder, and a patient’s treatment must evolve with time to address newly emerging issues. 1 • Furthermore, as the manifestation of dementia varies considerably from patient to patient, treatment plans should be individualized. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014
Current approaches to AD management • The management of AD can be categorized into pharmacological, psychosocial, and caregiving aspects. Pharmacological Psychosocial Caregiving Pharmacological therapies indicated for the treatment of AD are: 1, 2 • acetylcholinesterase inhibitors (ACh. EIs) • NMDA receptor antagonist. Other pharmacological therapies used in AD include: 1, 2 • antipsychotics for psychosis and agitation • antidepressants for depression • sedatives for sleep disturbance. • Dementia is a progressive disorder, and a patient’s treatment must evolve with time to address newly emerging issues. 1 • Furthermore, as the manifestation of dementia varies considerably from patient to patient, treatment plans should be individualized. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014
Current approaches to AD management • The management of AD can be categorized into pharmacological, psychosocial, and caregiving aspects. Pharmacological Psychosocial Caregiving • Dementia is a progressive disorder, and a patient’s treatment must evolve with time to address newly emerging issues. 1 • Furthermore, as the manifestation of dementia varies considerably from patient to patient, treatment plans should be individualized. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014 Psychosocial therapies include: 1, 2 • behavior-oriented approaches • stimulation-oriented approaches • emotion-oriented approaches • cognition-oriented approaches • sleep hygiene.
Current approaches to AD management • The management of AD can be categorized into pharmacological, psychosocial, and caregiving aspects. Pharmacological Psychosocial Caregiving • Dementia is a progressive disorder, and a patient’s treatment must evolve with time to address newly emerging issues. 1 • Furthermore, as the manifestation of dementia varies considerably from patient to patient, treatment plans should be individualized. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014 Family/caregiver support is a key part of the management of patients with AD.
Current approaches to AD management • The management of AD can be categorized into pharmacological, psychosocial, and caregiving aspects. Pharmacological Psychosocial Caregiving • Dementia is a progressive disorder, and a patient’s treatment must evolve with time to address newly emerging issues. 1 • Furthermore, as the manifestation of dementia varies considerably from patient to patient, treatment plans should be individualized. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014 • In addition to the emergence of new symptoms of AD with time, patients may require treatment for co-occurring psychiatric and medical conditions. 1, 2
Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Behavior-oriented approaches Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014 Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1

Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Behavior-oriented approaches Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1 • The aim of behavior-oriented treatments is to identify problem behaviors and to reduce their frequency, by making changes to the patient’s environment. 1 • Examples of behavioral interventions are scheduled toileting (to reduce urinary incontinence), and aggressive-behavior management training for caregivers. 1 • Behavioral interventions are supported by small trials and case studies, and are in widespread clinical use. 1, 2 Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014
Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1 • The aim of stimulation-oriented treatments is to activate the patient’s available cognitive resources. 1 • Examples of stimulation interventions are recreational activities or therapies (e. g. , crafts, games, pets), art therapies (e. g. , music, dance, art), and exercise. 1 • Stimulation interventions have limited data to support their efficacy, but should be considered part of the humane care of patients with dementia. 1, 2 Behavior-oriented approaches Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014
Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1 • The aims of emotion-oriented treatments are to address issues of loss, and to improve mood and behavior. 1 • Examples of emotion interventions are reminiscence therapy (in the context of the patient’s life history), validation therapy, and supportive psychotherapy. 1 • Emotion interventions have limited data to support their efficacy. 1, 2 Behavior-oriented approaches Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014
Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1 • The aim of cognition-oriented treatments is to restore cognitive deficits, often in a classroom setting. 1 • Examples of cognition interventions are reality orientation, cognitive retraining, and skills training (focused on specific cognitive deficits). 1 • Cognition interventions may provide modest and transient improvements; however, they are associated with adverse emotional consequences (such as frustration). 1, 2 Behavior-oriented approaches Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014
Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Behavior-oriented approaches Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014 Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1 • Many patients with AD suffer from sleep disturbances, which may be minimized by their participation in daytime activities, and by improving sleep hygiene (e. g. , consistent rising times, minimizing daytime napping, and daily exercise). 1
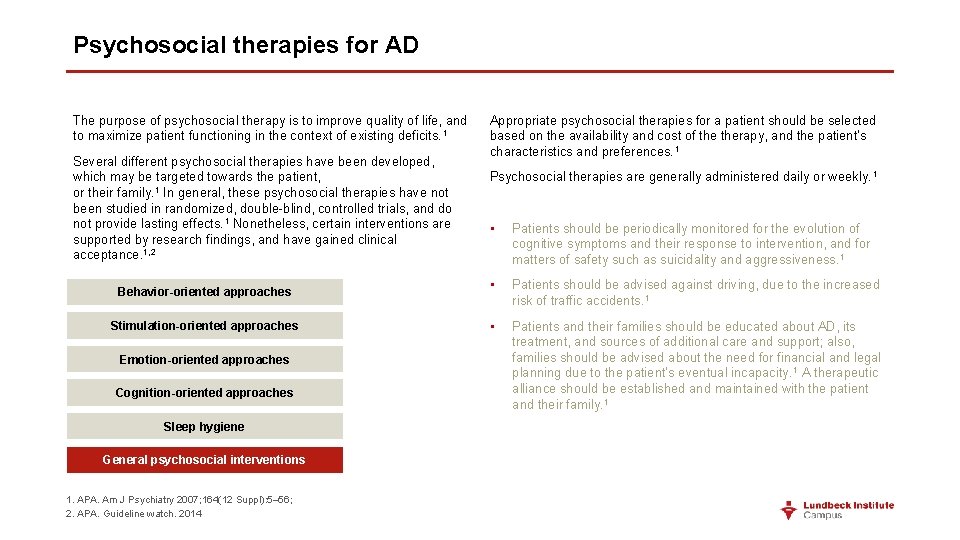
Psychosocial therapies for AD The purpose of psychosocial therapy is to improve quality of life, and to maximize patient functioning in the context of existing deficits. 1 Several different psychosocial therapies have been developed, which may be targeted towards the patient, or their family. 1 In general, these psychosocial therapies have not been studied in randomized, double-blind, controlled trials, and do not provide lasting effects. 1 Nonetheless, certain interventions are supported by research findings, and have gained clinical acceptance. 1, 2 Behavior-oriented approaches Stimulation-oriented approaches Emotion-oriented approaches Cognition-oriented approaches Sleep hygiene General psychosocial interventions 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. APA. Guideline watch. 2014 Appropriate psychosocial therapies for a patient should be selected based on the availability and cost of therapy, and the patient’s characteristics and preferences. 1 Psychosocial therapies are generally administered daily or weekly. 1 • Patients should be periodically monitored for the evolution of cognitive symptoms and their response to intervention, and for matters of safety such as suicidality and aggressiveness. 1 • Patients should be advised against driving, due to the increased risk of traffic accidents. 1 • Patients and their families should be educated about AD, its treatment, and sources of additional care and support; also, families should be advised about the need for financial and legal planning due to the patient’s eventual incapacity. 1 A therapeutic alliance should be established and maintained with the patient and their family. 1
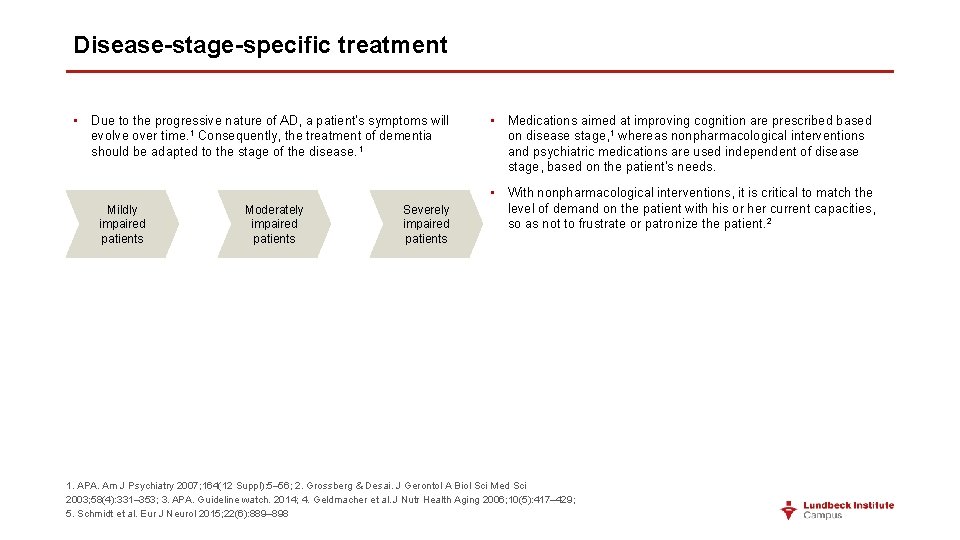
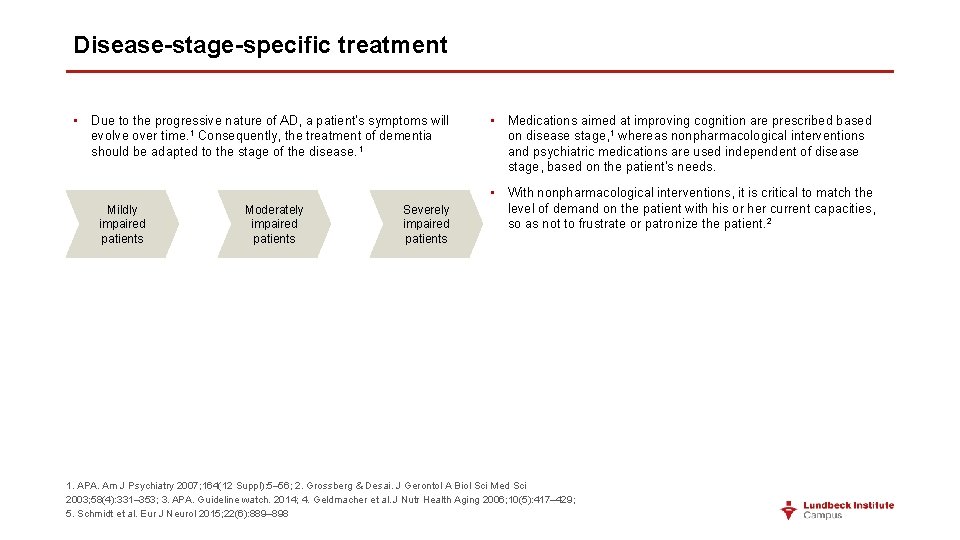
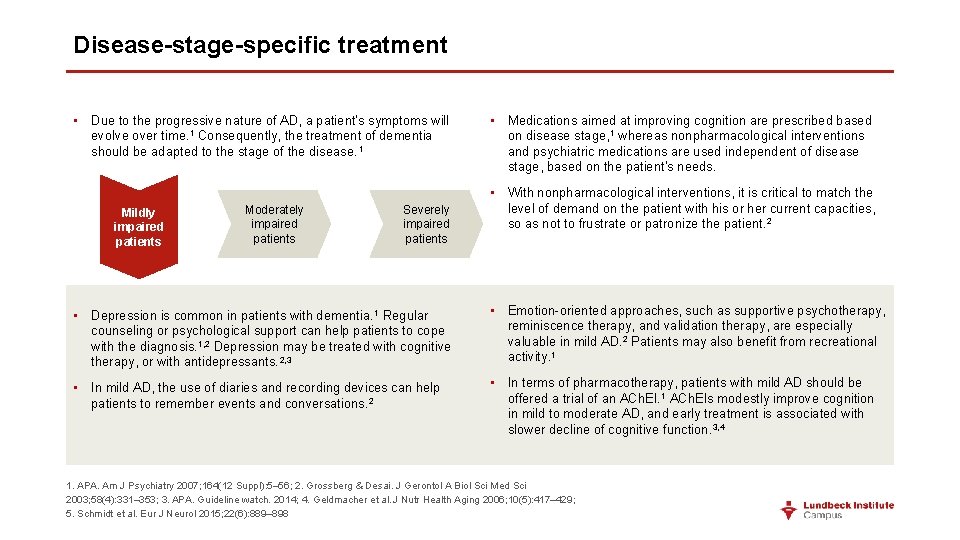
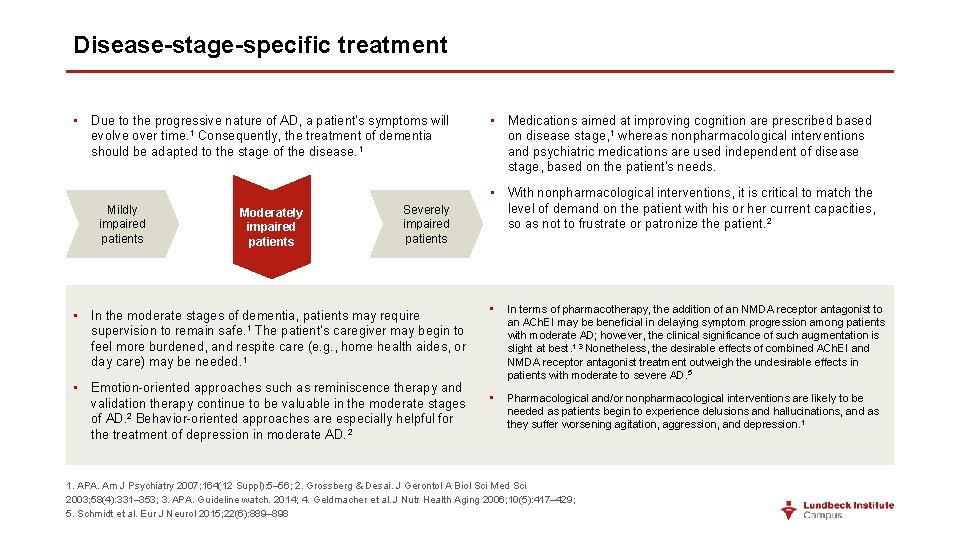
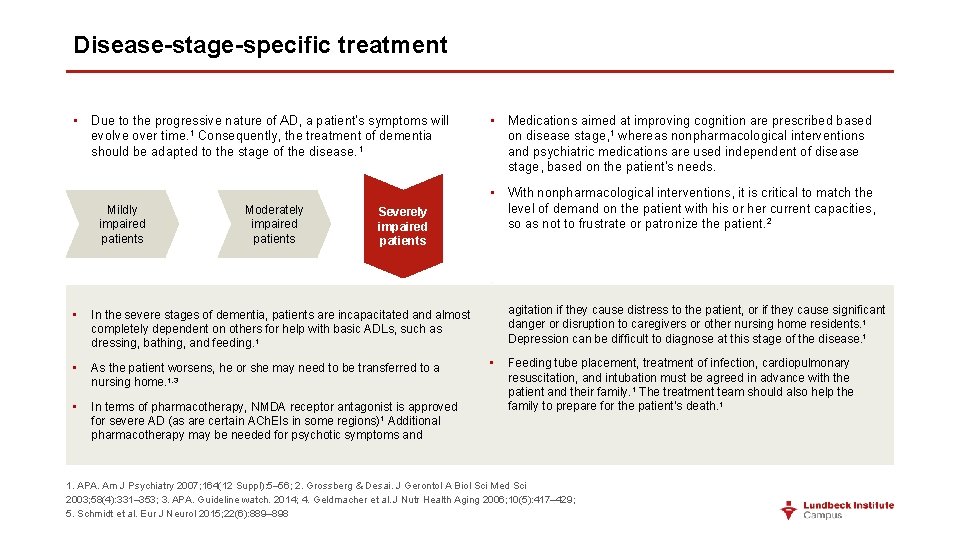
Disease-stage-specific treatment • Due to the progressive nature of AD, a patient’s symptoms will evolve over time. 1 Consequently, the treatment of dementia should be adapted to the stage of the disease. 1 Mildly impaired patients Moderately impaired patients Severely impaired patients • Medications aimed at improving cognition are prescribed based on disease stage, 1 whereas nonpharmacological interventions and psychiatric medications are used independent of disease stage, based on the patient’s needs. • With nonpharmacological interventions, it is critical to match the level of demand on the patient with his or her current capacities, so as not to frustrate or patronize the patient. 2 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. Grossberg & Desai. J Gerontol A Biol Sci Med Sci 2003; 58(4): 331– 353; 3. APA. Guideline watch. 2014; 4. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429; 5. Schmidt et al. Eur J Neurol 2015; 22(6): 889– 898
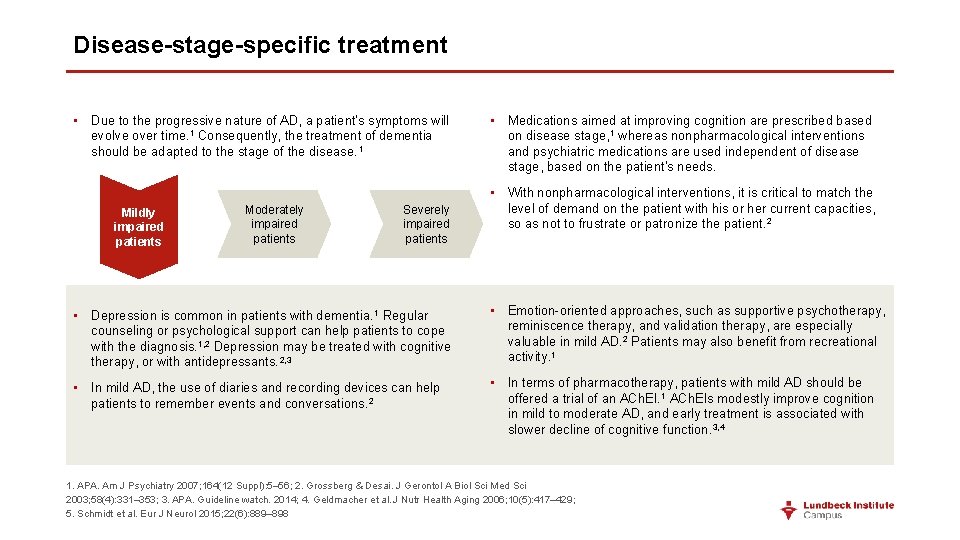
Disease-stage-specific treatment • Due to the progressive nature of AD, a patient’s symptoms will evolve over time. 1 Consequently, the treatment of dementia should be adapted to the stage of the disease. 1 Mildly impaired patients Moderately impaired patients Severely impaired patients • Medications aimed at improving cognition are prescribed based on disease stage, 1 whereas nonpharmacological interventions and psychiatric medications are used independent of disease stage, based on the patient’s needs. • With nonpharmacological interventions, it is critical to match the level of demand on the patient with his or her current capacities, so as not to frustrate or patronize the patient. 2 • Depression is common in patients with dementia. 1 Regular counseling or psychological support can help patients to cope with the diagnosis. 1, 2 Depression may be treated with cognitive therapy, or with antidepressants. 2, 3 • Emotion-oriented approaches, such as supportive psychotherapy, reminiscence therapy, and validation therapy, are especially valuable in mild AD. 2 Patients may also benefit from recreational activity. 1 • In mild AD, the use of diaries and recording devices can help patients to remember events and conversations. 2 • In terms of pharmacotherapy, patients with mild AD should be offered a trial of an ACh. EI. 1 ACh. EIs modestly improve cognition in mild to moderate AD, and early treatment is associated with slower decline of cognitive function. 3, 4 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. Grossberg & Desai. J Gerontol A Biol Sci Med Sci 2003; 58(4): 331– 353; 3. APA. Guideline watch. 2014; 4. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429; 5. Schmidt et al. Eur J Neurol 2015; 22(6): 889– 898
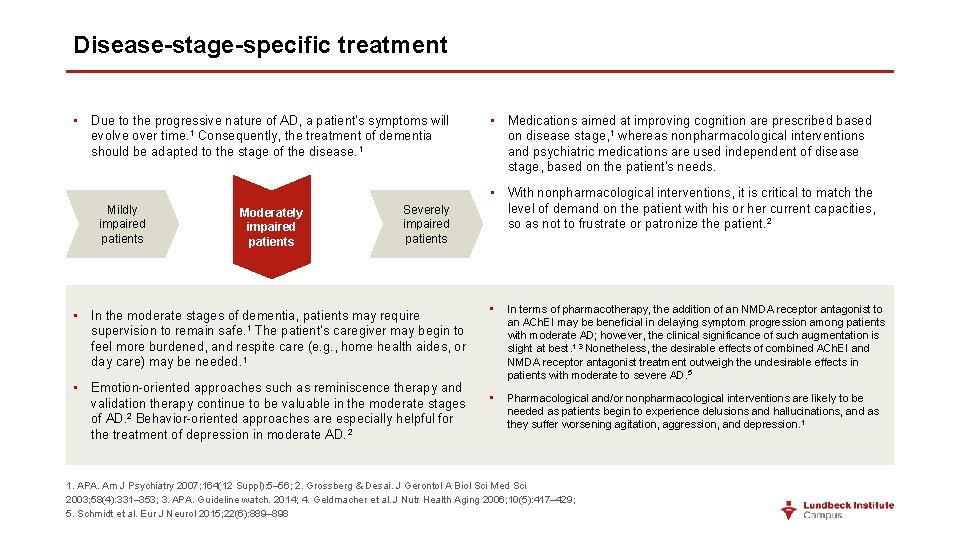
Disease-stage-specific treatment • Due to the progressive nature of AD, a patient’s symptoms will evolve over time. 1 Consequently, the treatment of dementia should be adapted to the stage of the disease. 1 Mildly impaired patients Moderately impaired patients Severely impaired patients • In the moderate stages of dementia, patients may require supervision to remain safe. 1 The patient’s caregiver may begin to feel more burdened, and respite care (e. g. , home health aides, or day care) may be needed. 1 • Emotion-oriented approaches such as reminiscence therapy and validation therapy continue to be valuable in the moderate stages of AD. 2 Behavior-oriented approaches are especially helpful for the treatment of depression in moderate AD. 2 • Medications aimed at improving cognition are prescribed based on disease stage, 1 whereas nonpharmacological interventions and psychiatric medications are used independent of disease stage, based on the patient’s needs. • With nonpharmacological interventions, it is critical to match the level of demand on the patient with his or her current capacities, so as not to frustrate or patronize the patient. 2 • In terms of pharmacotherapy, the addition of an NMDA receptor antagonist to an ACh. EI may be beneficial in delaying symptom progression among patients with moderate AD; however, the clinical significance of such augmentation is slight at best. 1, 3 Nonetheless, the desirable effects of combined ACh. EI and NMDA receptor antagonist treatment outweigh the undesirable effects in patients with moderate to severe AD. 5 • Pharmacological and/or nonpharmacological interventions are likely to be needed as patients begin to experience delusions and hallucinations, and as they suffer worsening agitation, aggression, and depression. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. Grossberg & Desai. J Gerontol A Biol Sci Med Sci 2003; 58(4): 331– 353; 3. APA. Guideline watch. 2014; 4. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429; 5. Schmidt et al. Eur J Neurol 2015; 22(6): 889– 898
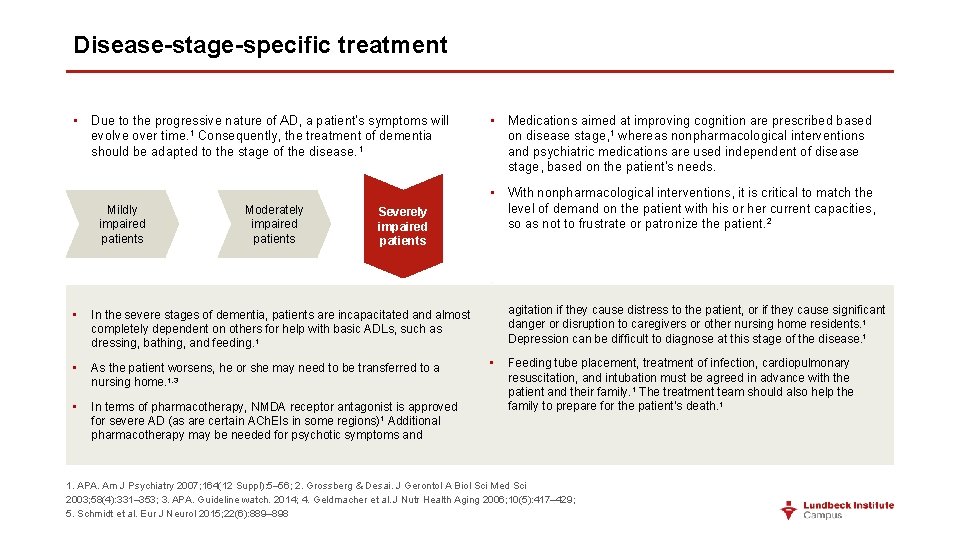
Disease-stage-specific treatment • Due to the progressive nature of AD, a patient’s symptoms will evolve over time. 1 Consequently, the treatment of dementia should be adapted to the stage of the disease. 1 Mildly impaired patients Moderately impaired patients Severely impaired patients • Medications aimed at improving cognition are prescribed based on disease stage, 1 whereas nonpharmacological interventions and psychiatric medications are used independent of disease stage, based on the patient’s needs. • With nonpharmacological interventions, it is critical to match the level of demand on the patient with his or her current capacities, so as not to frustrate or patronize the patient. 2 • • In the severe stages of dementia, patients are incapacitated and almost completely dependent on others for help with basic ADLs, such as dressing, bathing, and feeding. 1 • As the patient worsens, he or she may need to be transferred to a nursing home. 1, 3 • In terms of pharmacotherapy, NMDA receptor antagonist is approved for severe AD (as are certain ACh. EIs in some regions)1 Additional pharmacotherapy may be needed for psychotic symptoms and agitation if they cause distress to the patient, or if they cause significant danger or disruption to caregivers or other nursing home residents. 1 Depression can be difficult to diagnose at this stage of the disease. 1 • Feeding tube placement, treatment of infection, cardiopulmonary resuscitation, and intubation must be agreed in advance with the patient and their family. 1 The treatment team should also help the family to prepare for the patient’s death. 1 1. APA. Am J Psychiatry 2007; 164(12 Suppl): 5– 56; 2. Grossberg & Desai. J Gerontol A Biol Sci Med Sci 2003; 58(4): 331– 353; 3. APA. Guideline watch. 2014; 4. Geldmacher et al. J Nutr Health Aging 2006; 10(5): 417– 429; 5. Schmidt et al. Eur J Neurol 2015; 22(6): 889– 898
Key points • AD is managed through a combination of pharmacological, psychosocial, and caregiving approaches. • Pharmacological therapies indicated for the treatment of AD are the ACh. EIs and NMDA receptor antagonist. • Psychosocial therapies include those targeted at behavior, stimulation, emotions, cognition, and sleep hygiene. In general, evidence to support these therapies is limited. • As the disease advances, patients with AD become increasingly dependent on caregivers. Consequently, the pressure on caregivers increases. • Treatment plans should be individualized, and should evolve as the disease progresses.
 Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Georgia alzheimers planning
Georgia alzheimers planning Fast scale for dementia
Fast scale for dementia Alzheimers sjukdom
Alzheimers sjukdom Alzheimers nz conference 2020
Alzheimers nz conference 2020 Historical research
Historical research Alzheimers society contented dementia
Alzheimers society contented dementia Alzheimers eye test joke
Alzheimers eye test joke Communicable disease and non communicable disease
Communicable disease and non communicable disease General goals and specific goals
General goals and specific goals Examples of generic goals and product-specific goals
Examples of generic goals and product-specific goals Treatment for prion disease
Treatment for prion disease Minimal change disease treatment
Minimal change disease treatment Maple syrup urine disease treatment
Maple syrup urine disease treatment Modern treatment of heart disease
Modern treatment of heart disease The disease-control phase of treatment includes
The disease-control phase of treatment includes Adhd goals and objectives examples
Adhd goals and objectives examples What are protection goals and principles
What are protection goals and principles Audio lingual method conclusion
Audio lingual method conclusion Goals and principles of protection in os
Goals and principles of protection in os Principles of drug addiction treatment
Principles of drug addiction treatment Disease-specific workflows
Disease-specific workflows Lhon
Lhon Decompensated liver disease
Decompensated liver disease Disease betekenis
Disease betekenis Infectivity definition
Infectivity definition Type of disease
Type of disease Thousand cankers disease map
Thousand cankers disease map Frog leg
Frog leg Chemistry of life summary
Chemistry of life summary Raynaud's disease lupus
Raynaud's disease lupus Disease specific mortality rate formula
Disease specific mortality rate formula