The Two Stage Standard Technique Keeps You Out

- Slides: 25
The Two Stage, Standard Technique Keeps You Out of Trouble & Out of Corners Henry D Clarke MD Professor of Orthopedics Mayo Clinic
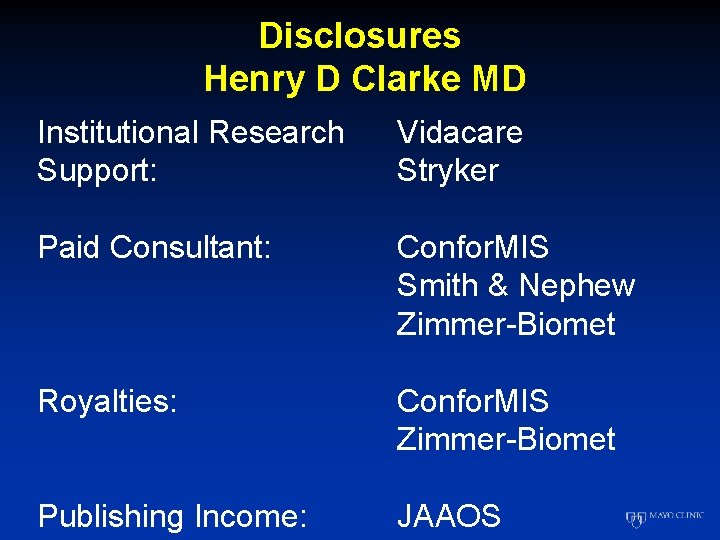
Disclosures Henry D Clarke MD Institutional Research Support: Vidacare Stryker Paid Consultant: Confor. MIS Smith & Nephew Zimmer-Biomet Royalties: Confor. MIS Zimmer-Biomet Publishing Income: JAAOS
Deep Peri-Prosthetic Infection Introduction • Infection #1 Reason for revision TKA - 25. 2% of revisions • Aseptic loosening #2 - 16. 1% of revisions Bozic et al, CORR 2010
Deep Peri-Prosthetic Infection Treatment Options • Antibiotic suppression • Arthroscopic debridement • Open debridement with polyethylene exchange - 1 versus 2 stage with abx cement beads • Prosthesis removal & re-implantation - 1 versus 2 stage • Arthrodesis • Amputation • Resection arthroplasty
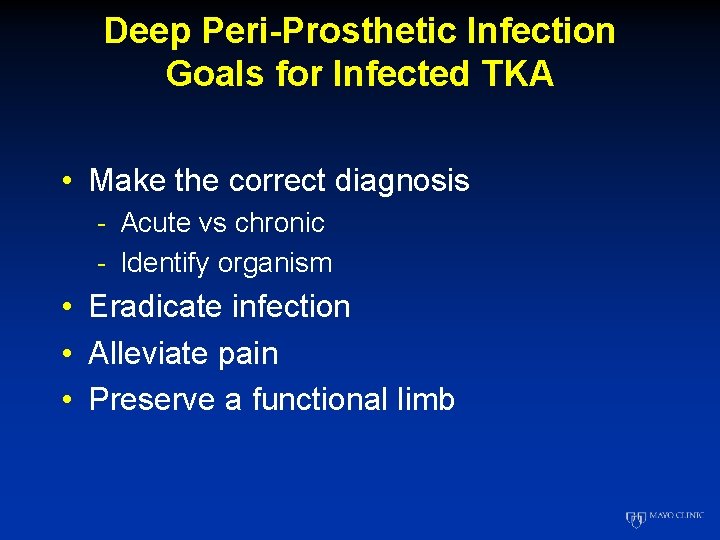
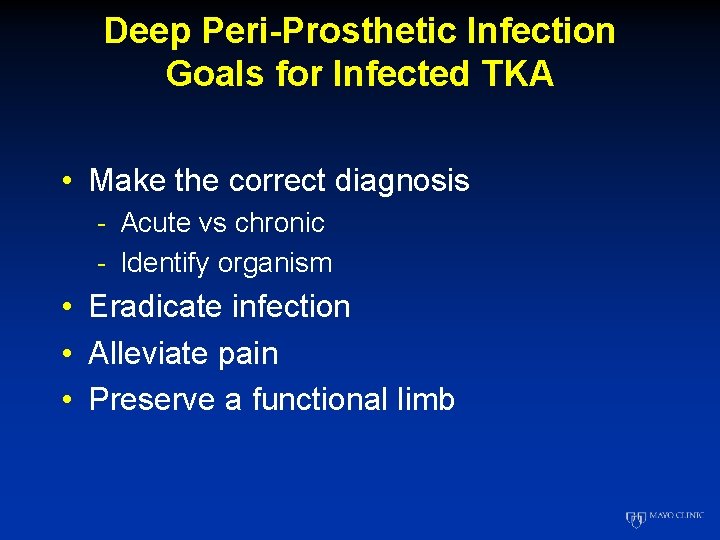
Deep Peri-Prosthetic Infection Goals for Infected TKA • Make the correct diagnosis - Acute vs chronic - Identify organism • Eradicate infection • Alleviate pain • Preserve a functional limb
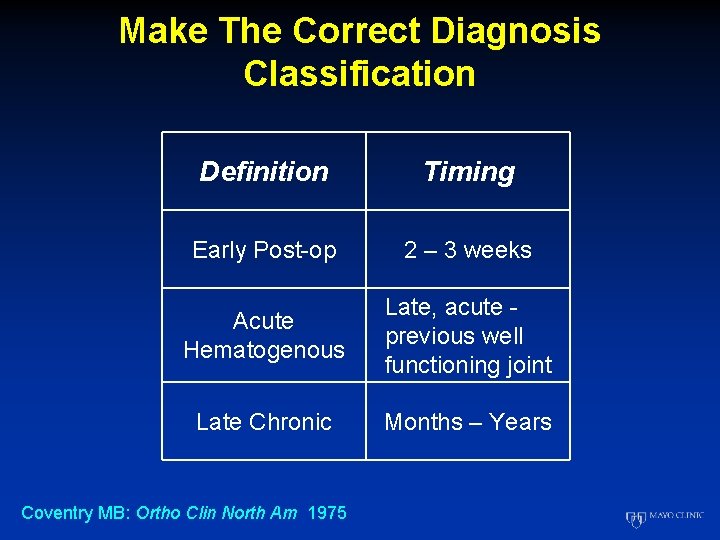
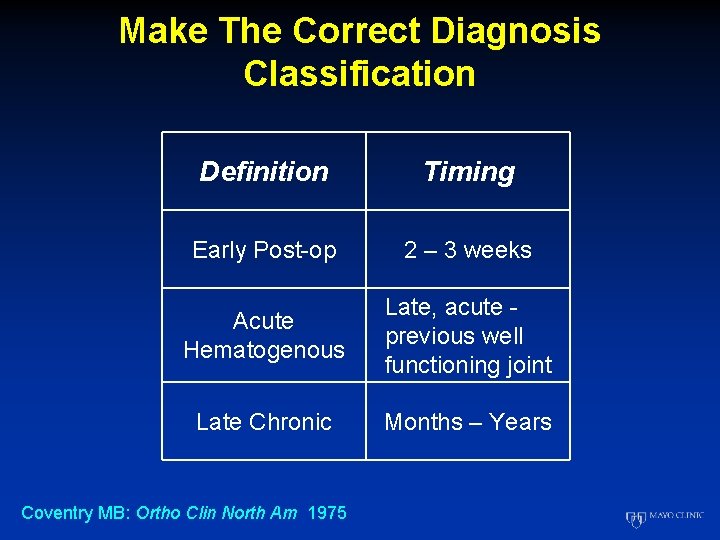
Make The Correct Diagnosis Classification Definition Timing Early Post-op 2 – 3 weeks Acute Hematogenous Late, acute previous well functioning joint Late Chronic Months – Years Coventry MB: Ortho Clin North Am 1975
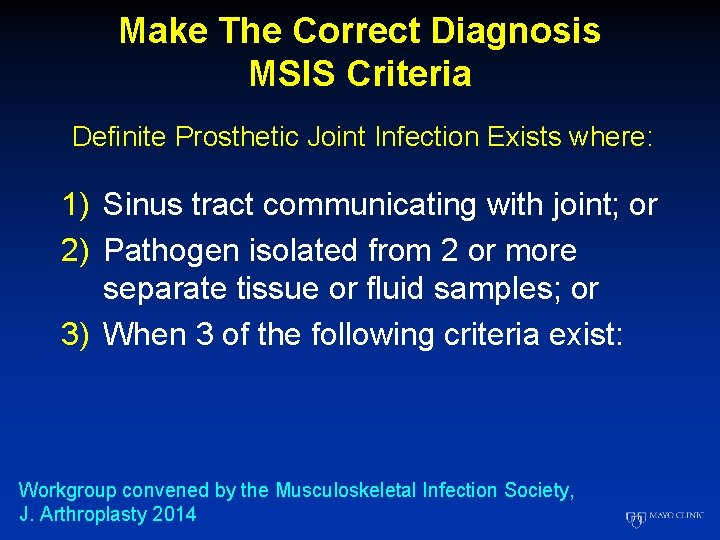
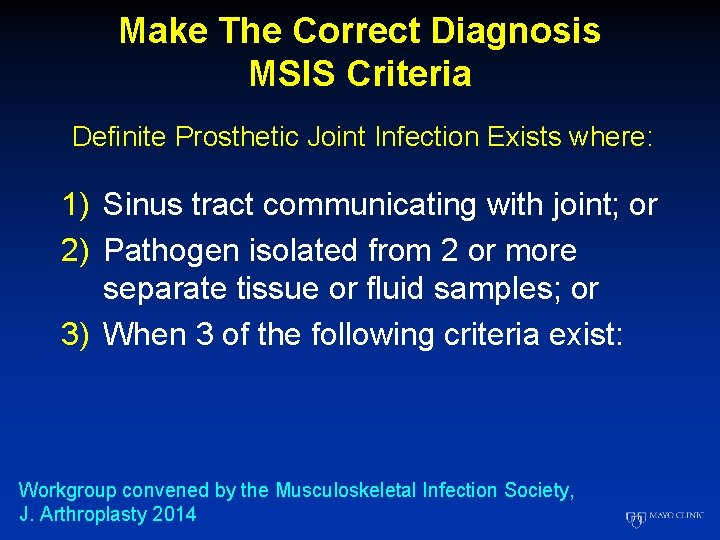
Make The Correct Diagnosis MSIS Criteria Definite Prosthetic Joint Infection Exists where: 1) Sinus tract communicating with joint; or 2) Pathogen isolated from 2 or more separate tissue or fluid samples; or 3) When 3 of the following criteria exist: Workgroup convened by the Musculoskeletal Infection Society, J. Arthroplasty 2014
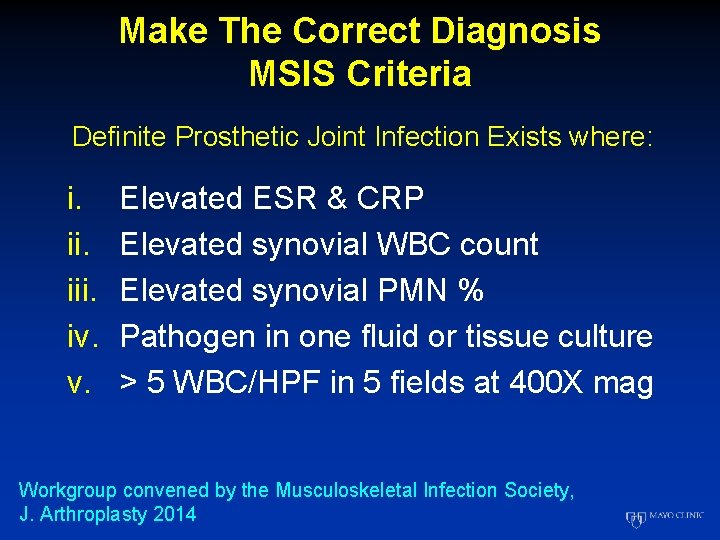
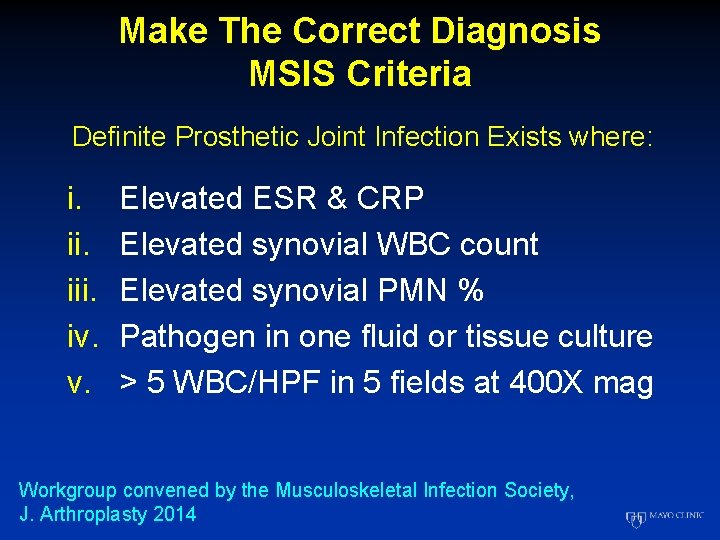
Make The Correct Diagnosis MSIS Criteria Definite Prosthetic Joint Infection Exists where: i. iii. iv. v. Elevated ESR & CRP Elevated synovial WBC count Elevated synovial PMN % Pathogen in one fluid or tissue culture > 5 WBC/HPF in 5 fields at 400 X mag Workgroup convened by the Musculoskeletal Infection Society, J. Arthroplasty 2014
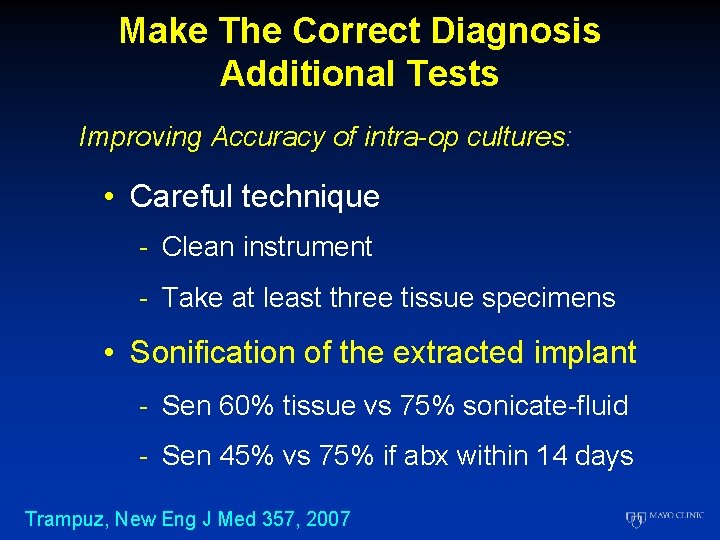
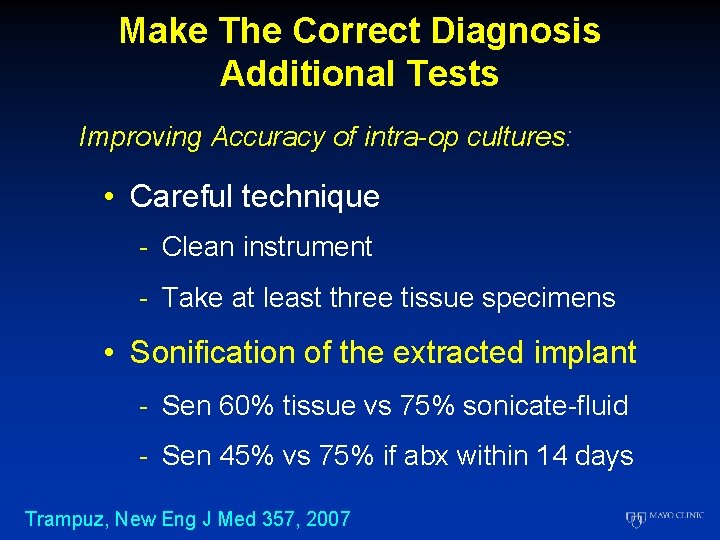
Make The Correct Diagnosis Additional Tests Improving Accuracy of intra-op cultures: • Careful technique - Clean instrument - Take at least three tissue specimens • Sonification of the extracted implant - Sen 60% tissue vs 75% sonicate-fluid - Sen 45% vs 75% if abx within 14 days Trampuz, New Eng J Med 357, 2007
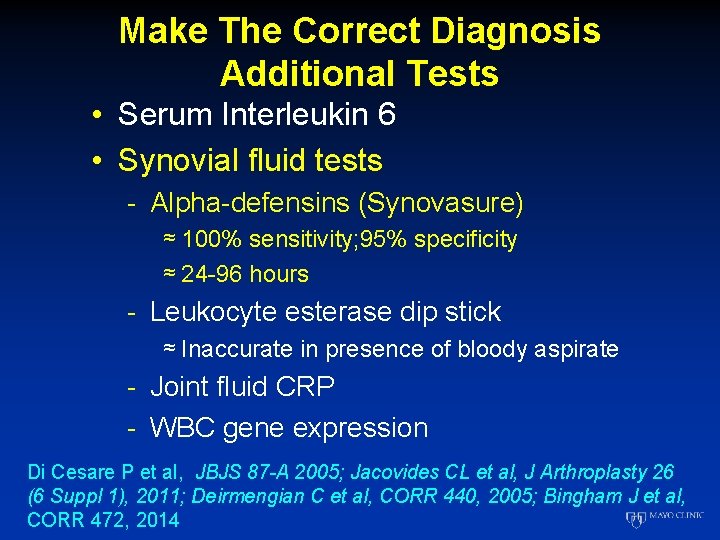
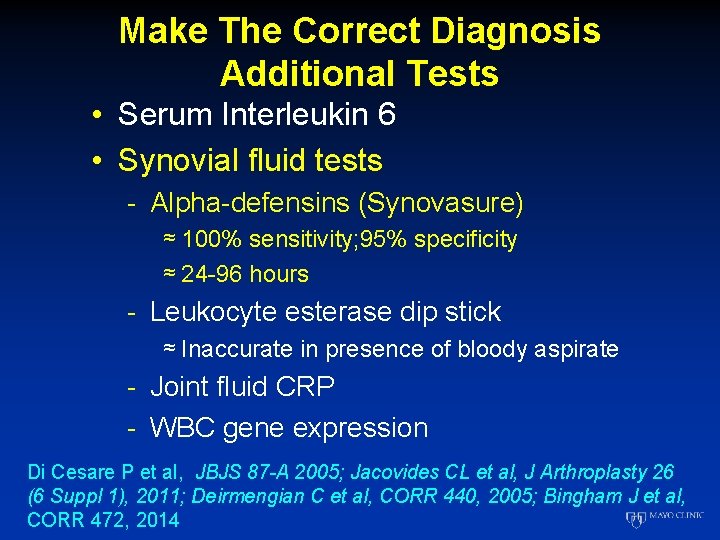
Make The Correct Diagnosis Additional Tests • Serum Interleukin 6 • Synovial fluid tests - Alpha-defensins (Synovasure) ≈ 100% sensitivity; 95% specificity ≈ 24 -96 hours - Leukocyte esterase dip stick ≈ Inaccurate in presence of bloody aspirate - Joint fluid CRP - WBC gene expression Di Cesare P et al, JBJS 87 -A 2005; Jacovides CL et al, J Arthroplasty 26 (6 Suppl 1), 2011; Deirmengian C et al, CORR 440, 2005; Bingham J et al, CORR 472, 2014
Deep Peri-Prosthetic Infection Chronic PJI • What are the options? - One stage revision - Two stage revision with antibiotic spacer ≈ Static ≈ Articulating
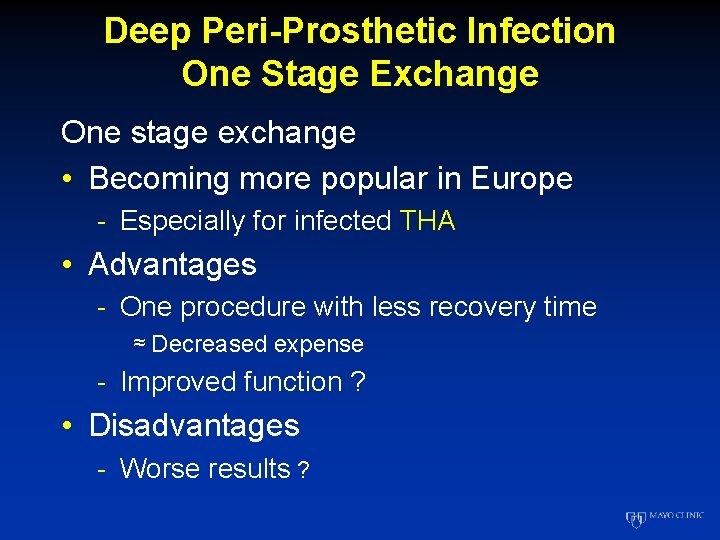
Deep Peri-Prosthetic Infection One Stage Exchange One stage exchange • Becoming more popular in Europe - Especially for infected THA • Advantages - One procedure with less recovery time ≈ Decreased expense - Improved function ? • Disadvantages - Worse results ?
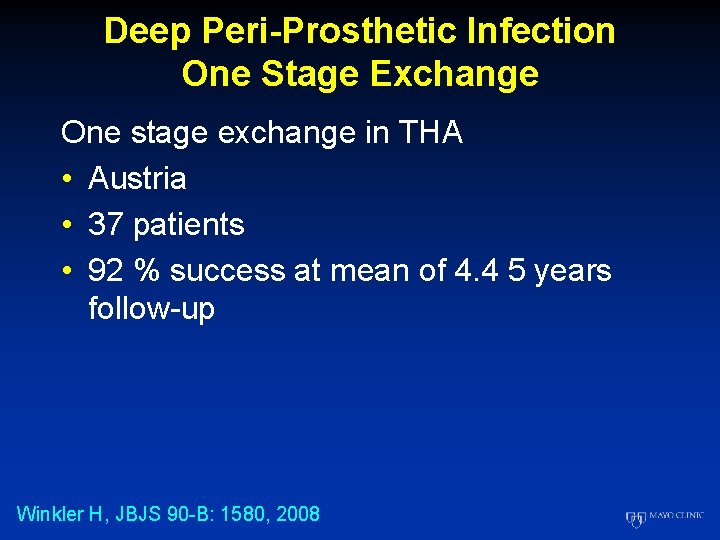
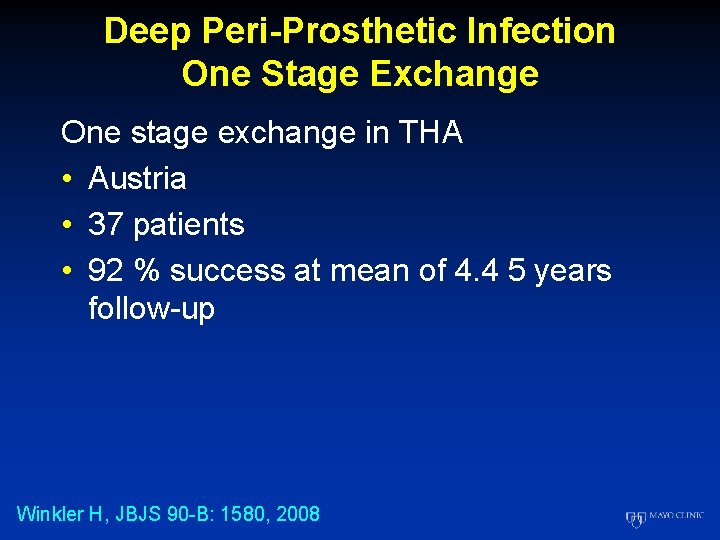
Deep Peri-Prosthetic Infection One Stage Exchange One stage exchange in THA • Austria • 37 patients • 92 % success at mean of 4. 4 5 years follow-up Winkler H, JBJS 90 -B: 1580, 2008
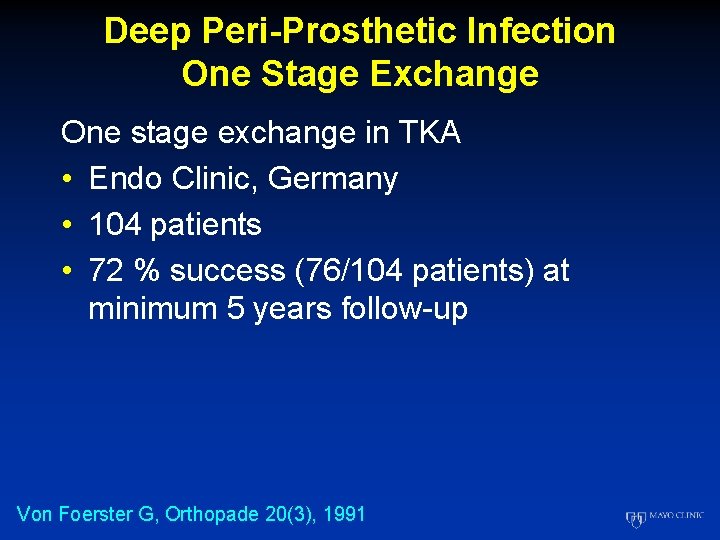
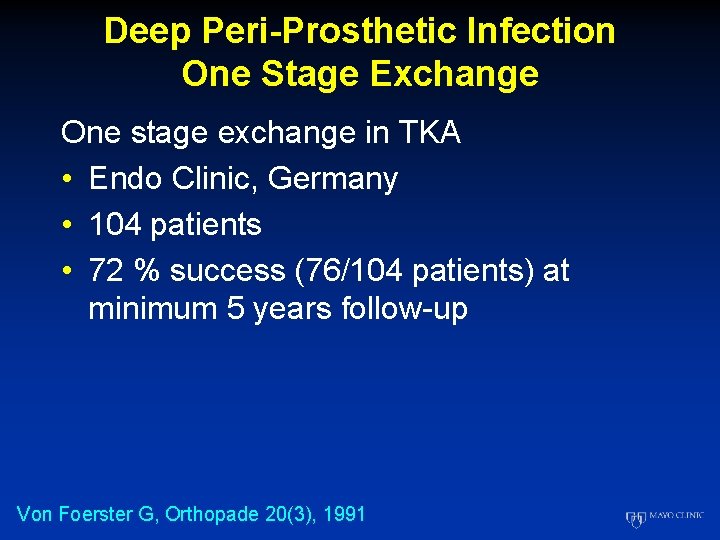
Deep Peri-Prosthetic Infection One Stage Exchange One stage exchange in TKA • Endo Clinic, Germany • 104 patients • 72 % success (76/104 patients) at minimum 5 years follow-up Von Foerster G, Orthopade 20(3), 1991
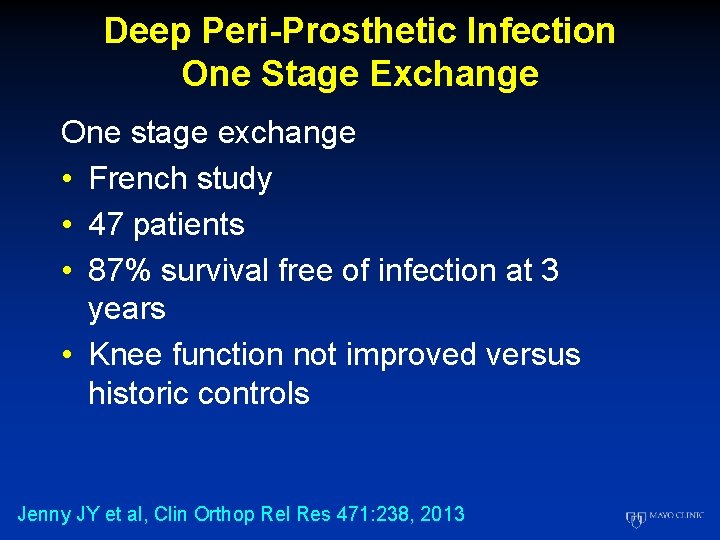
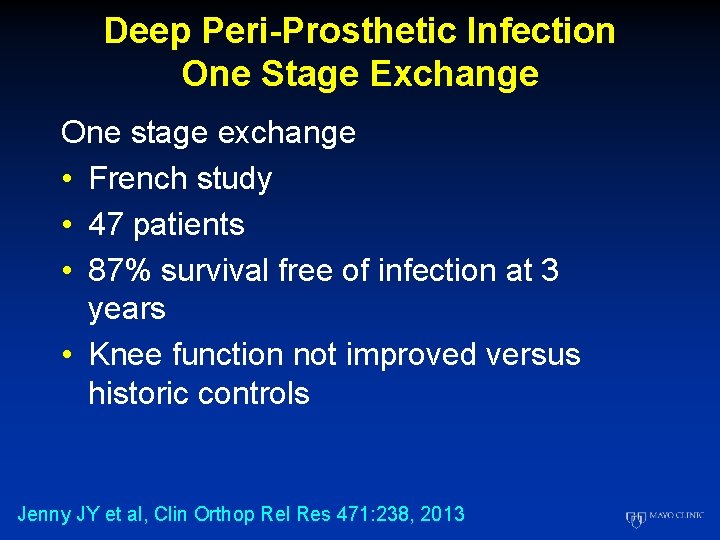
Deep Peri-Prosthetic Infection One Stage Exchange One stage exchange • French study • 47 patients • 87% survival free of infection at 3 years • Knee function not improved versus historic controls Jenny JY et al, Clin Orthop Rel Res 471: 238, 2013
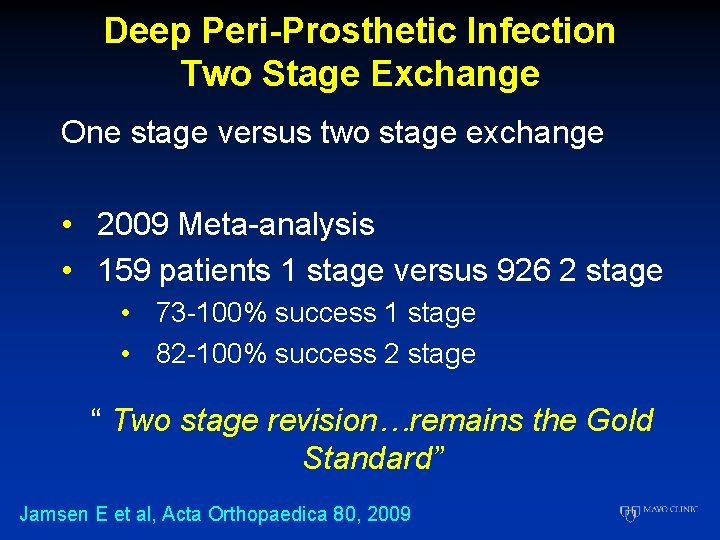
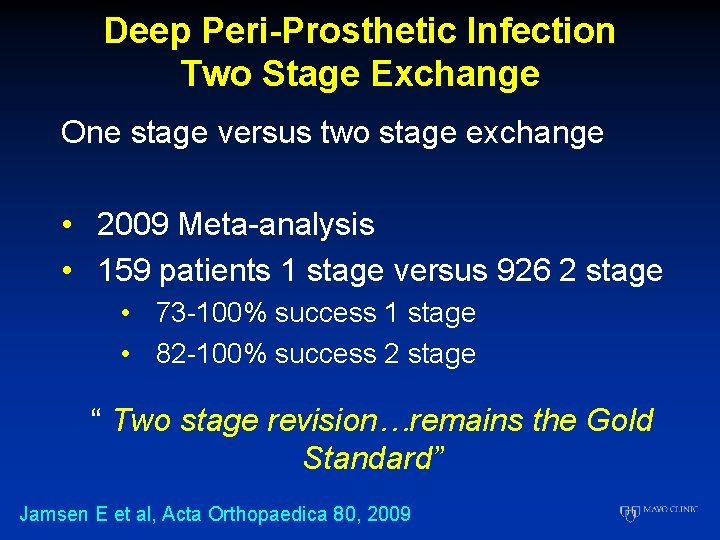
Deep Peri-Prosthetic Infection Two Stage Exchange One stage versus two stage exchange • 2009 Meta-analysis • 159 patients 1 stage versus 926 2 stage • 73 -100% success 1 stage • 82 -100% success 2 stage “ Two stage revision…remains the Gold Standard” Jamsen E et al, Acta Orthopaedica 80, 2009
Deep Peri-Prosthetic Infection Two Stage Exchange When to consider one stage exchange? • THA>TKA • Known organism • No antibiotic resistance • No sinus tract • No massive bone loss • Adequate soft tissue coverage Gerke T et al, The Infected Hip, JBJS 95 -B: 77, 2013
Deep Peri-Prosthetic Infection Two Stage Exchange Treatment principles • Accurate diagnosis • Identification of organism • Removal of prosthesis, infected tissue, & ALL foreign material • HIGH dose antibiotic cement spacer • 6 weeks appropriate IV antibiotics • Delayed re-implantation with LOW dose antibiotic cement
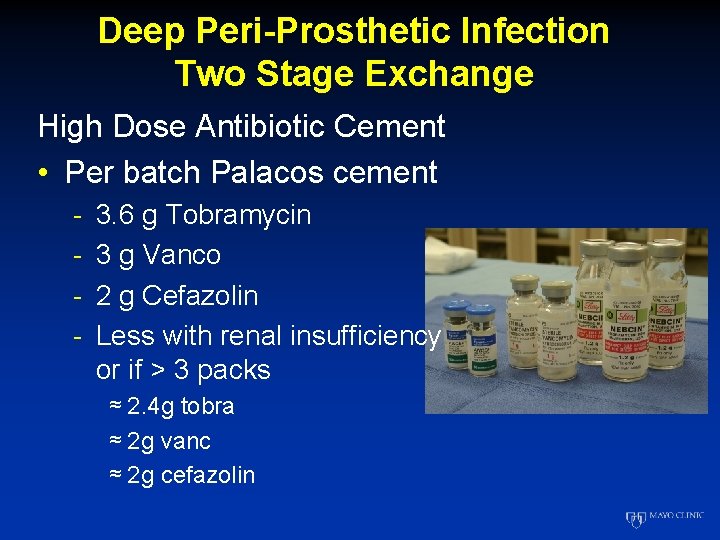
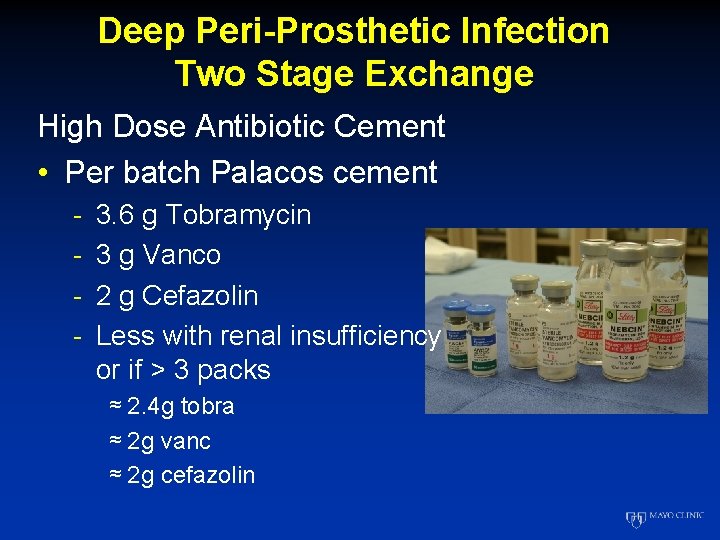
Deep Peri-Prosthetic Infection Two Stage Exchange High Dose Antibiotic Cement • Per batch Palacos cement - 3. 6 g Tobramycin 3 g Vanco 2 g Cefazolin Less with renal insufficiency or if > 3 packs ≈ 2. 4 g tobra ≈ 2 g vanc ≈ 2 g cefazolin
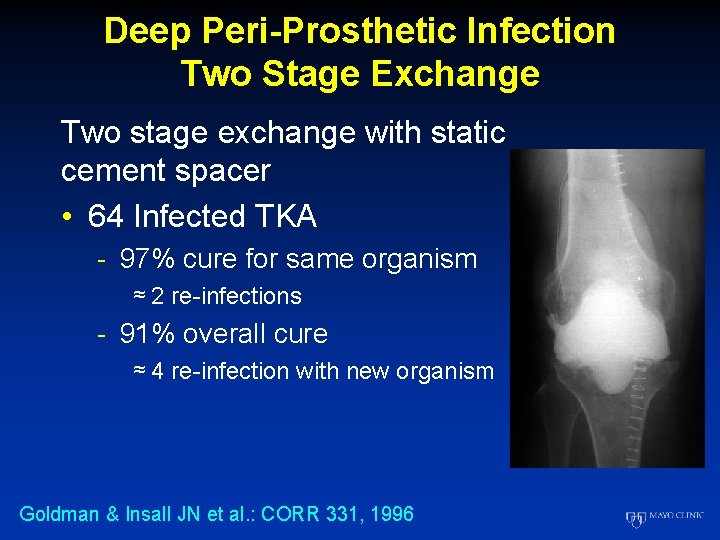
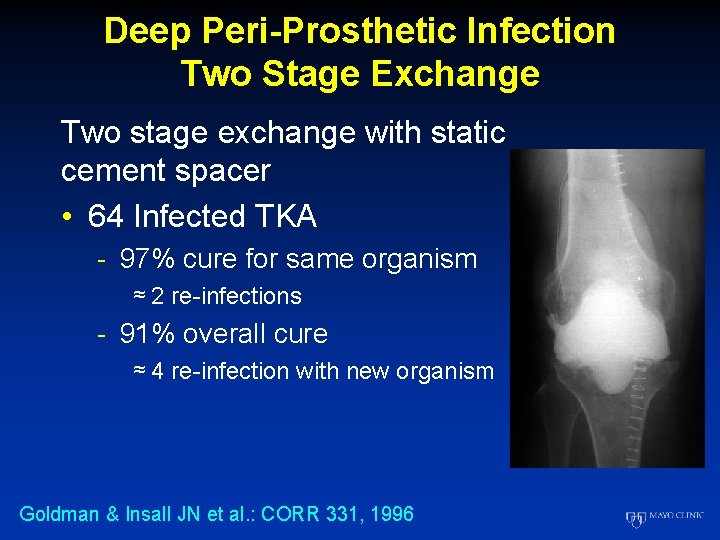
Deep Peri-Prosthetic Infection Two Stage Exchange Two stage exchange with static cement spacer • 64 Infected TKA - 97% cure for same organism ≈ 2 re-infections - 91% overall cure ≈ 4 re-infection with new organism Goldman & Insall JN et al. : CORR 331, 1996
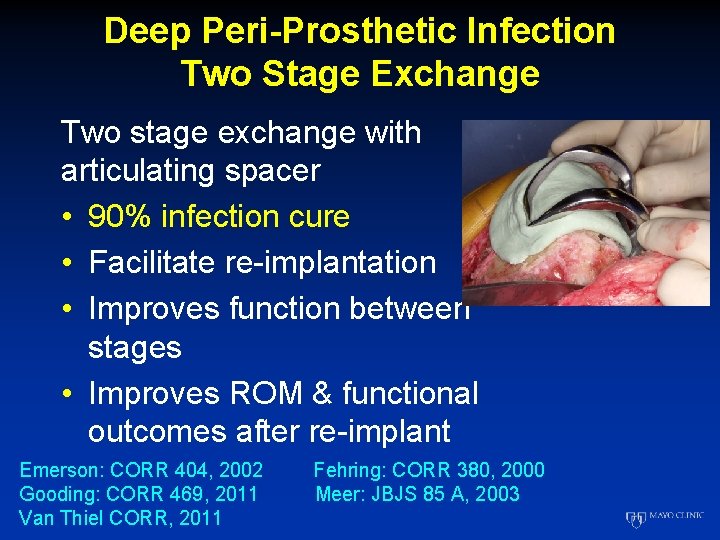
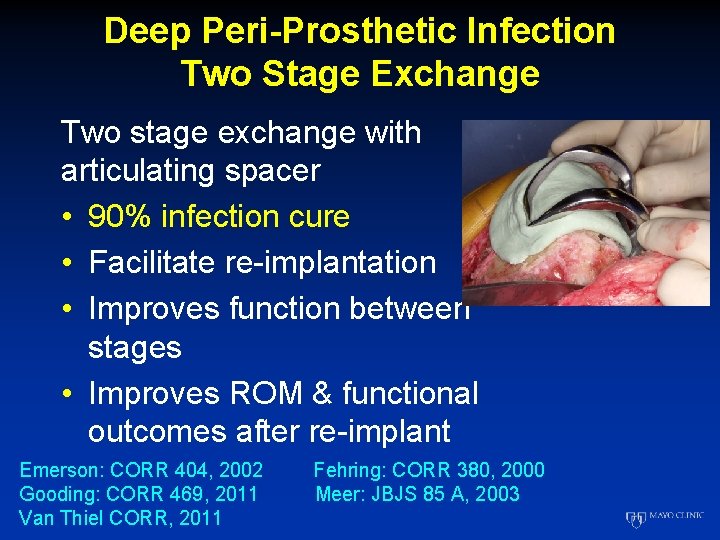
Deep Peri-Prosthetic Infection Two Stage Exchange Two stage exchange with articulating spacer • 90% infection cure • Facilitate re-implantation • Improves function between stages • Improves ROM & functional outcomes after re-implant Emerson: CORR 404, 2002 Gooding: CORR 469, 2011 Van Thiel CORR, 2011 Fehring: CORR 380, 2000 Meer: JBJS 85 A, 2003
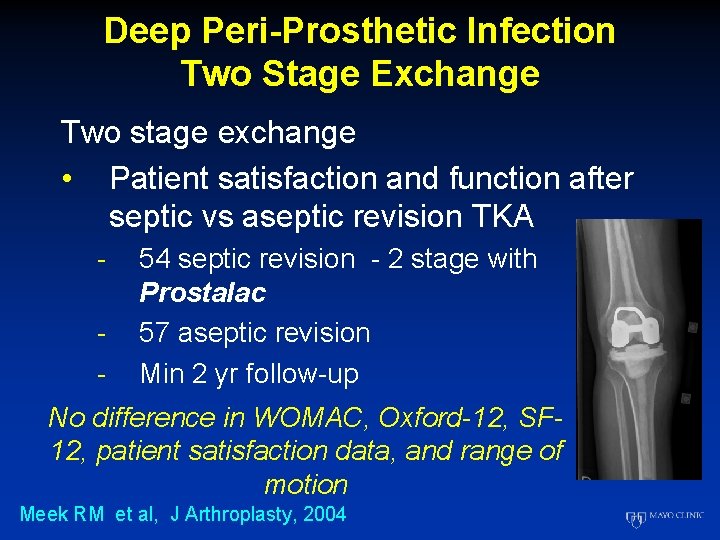
Deep Peri-Prosthetic Infection Two Stage Exchange Two stage exchange • Patient satisfaction and function after septic vs aseptic revision TKA - 54 septic revision - 2 stage with Prostalac 57 aseptic revision Min 2 yr follow-up No difference in WOMAC, Oxford-12, SF 12, patient satisfaction data, and range of motion Meek RM et al, J Arthroplasty, 2004
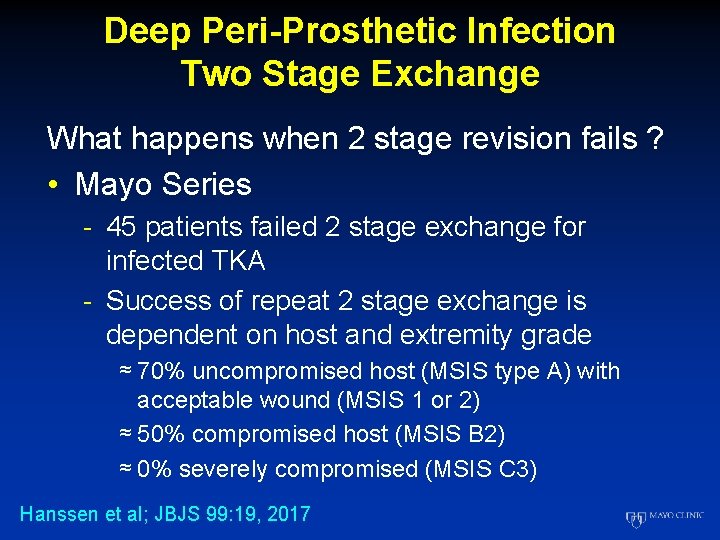
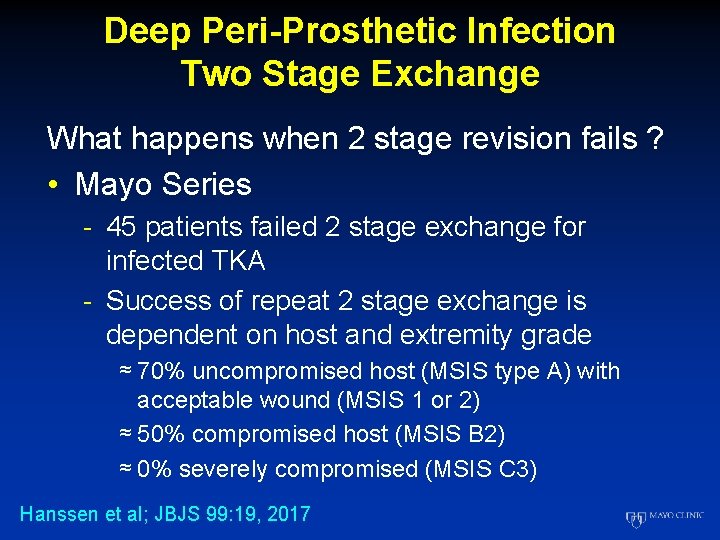
Deep Peri-Prosthetic Infection Two Stage Exchange What happens when 2 stage revision fails ? • Mayo Series - 45 patients failed 2 stage exchange for infected TKA - Success of repeat 2 stage exchange is dependent on host and extremity grade ≈ 70% uncompromised host (MSIS type A) with acceptable wound (MSIS 1 or 2) ≈ 50% compromised host (MSIS B 2) ≈ 0% severely compromised (MSIS C 3) Hanssen et al; JBJS 99: 19, 2017
How I Manage an Infected TKA Take Home Message • 2 stage revision with high dose antibiotic articulating cement spacer - Gold standard - Chronic infection, especially in TKA • Let Dr Mc. Pherson and others at high volume centers experiment • Do the right thing for your patients, get on base…don’t swing big and miss!

Thank You for Your Attention