Texas Medicaid Dental Services Gary Jessee Deputy Executive


- Slides: 16
Texas Medicaid Dental Services Gary Jessee Deputy Executive Commissioner Medical and Social Services Division Health and Human Services Commission November 7, 2016
Overview • Texas Medicaid Dental Benefit • Dental Benefit Quality Drivers u u Managed Care Implementation Establishment of Dental Home • Measuring Success 2
Texas Medicaid Dental Benefit • Primary and preventative dental services available to most children and young adults age birth through 20 • Persons that do not receive services through the Children’s Medicaid managed care dental plans are: u u u Medicaid recipients who are 21 years of age or older Recipients who reside in an institution (e. g. , nursing homes, state supported living centers, ICF-IID) Recipients in the STAR Health Program (dental services subcontracted through health plan) 3
Texas Medicaid Dental Benefit • Following medically necessary services included: u u u u Diagnostic and preventive Therapeutic Restorative Endodontic Periodontal Prosthodontic (removable and fixed) Implant and oral and maxillofacial surgery Orthodontic and adjunctive general 4
Texas Medicaid Dental Benefit • Program Enrollment as of March 2016 u u u Enrolled in Managed Care Dental Plans: 2, 931, 417 Enrolled in Traditional Medicaid (Fee-for-Service): 214, 869 Total Enrolled: 3, 146, 286 Source: HHSC System Forecasting, October 2016 5

Dental Benefit Quality Drivers
Managed Care Implementation • As of March 1, 2012, dental benefits administered under managed care environment by two dental maintenance organizations (DMOs) serving entire state • Members select a dental plan and a main dentist, who serves as the dental home and coordinates care 7
Managed Care Implementation Key Factors • Dental managed care allows a more creative approach to service delivery • Quality initiatives integrated into DMO contracts • DMO contractual requirements regarding network adequacy help ensure a robust network of available dental providers • Medicaid/CHIP Dental Director provides policy guidance and collaborates with stakeholders and agency staff to inform decision-making 8
Dental Home • Based on American Academy of Pediatric Dentistry’s (AAPD) definition: u u u Supports ongoing relationship with client Coordinates all aspects of oral health including referrals to specialists Begins no later than six months of age • Main dental home providers may be: u u Pediatric dentists General dentists Federally qualified health centers (FQHCs) Rural Health Clinics (RHCs) 9
Dental Home • Dental plans develop networks of dentists and specialists • Members choose a dental plan and dental home upon enrollment • Members can change dental home at any time • Dental plans require dental homes to: u Provide diagnostic and preventive care in accordance with AAPD recommendations u Assess the dental needs of members and provide referrals to specialists as needed 10
Dental Home • Dental home model resembles primary care physician (PCP) model • Encourages delivery of oral health care in a comprehensive, continuously accessible, and family-centered way • Dental home model informed by the success of the First Dental Home initiative u u Package of dental services aimed at children ages 6 -35 months Emphasizes early preventive services and simple, consistent oral health information for parents/caregivers 11
Dental Home • Implementation of dental home required informing members of the importance of remaining with one dentist • Members empowered to participate in care decisions with provider • Initial adjustment for providers u u Responsibility to develop dentist/patient relationship Claims paid only to dental home/main dentist or specialist with main dentist’s referral (unless emergency) • HHSC has worked with stakeholders to receive feedback and ensure dental home model operates as intended 12

Measuring Success
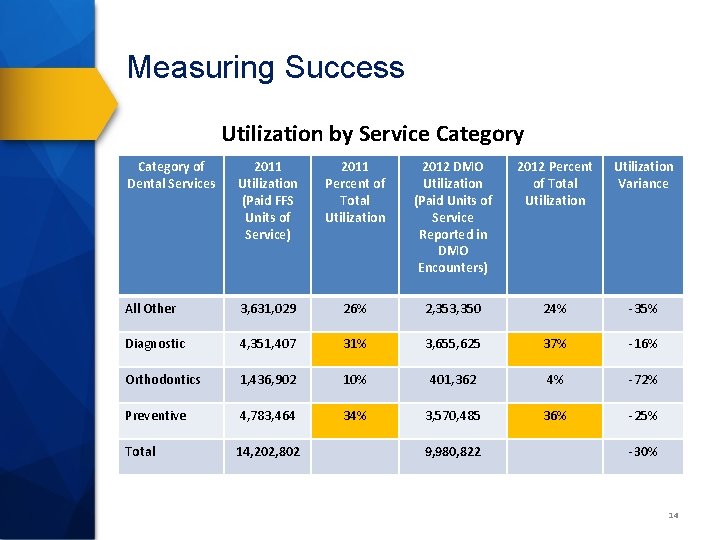
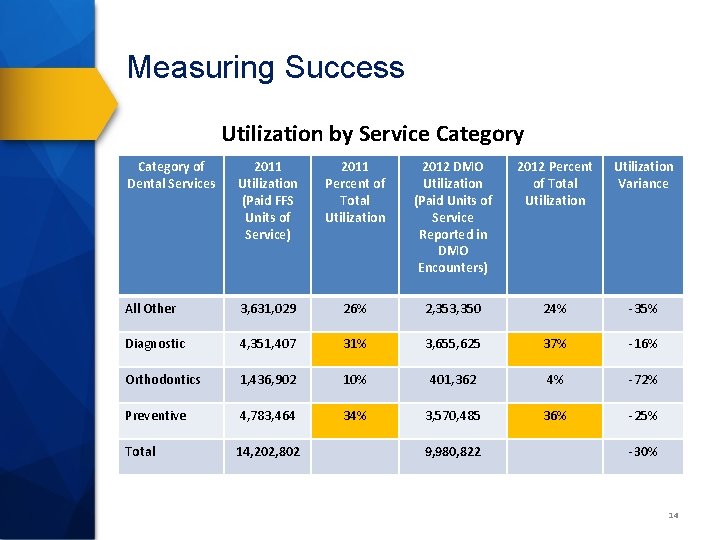
Measuring Success Utilization by Service Category of Dental Services 2011 Utilization (Paid FFS Units of Service) 2011 Percent of Total Utilization 2012 DMO Utilization (Paid Units of Service Reported in DMO Encounters) 2012 Percent of Total Utilization Variance All Other 3, 631, 029 26% 2, 353, 350 24% -35% Diagnostic 4, 351, 407 31% 3, 655, 625 37% -16% Orthodontics 1, 436, 902 10% 401, 362 4% -72% Preventive 4, 783, 464 34% 3, 570, 485 36% -25% Total 14, 202, 802 9, 980, 822 -30% 14
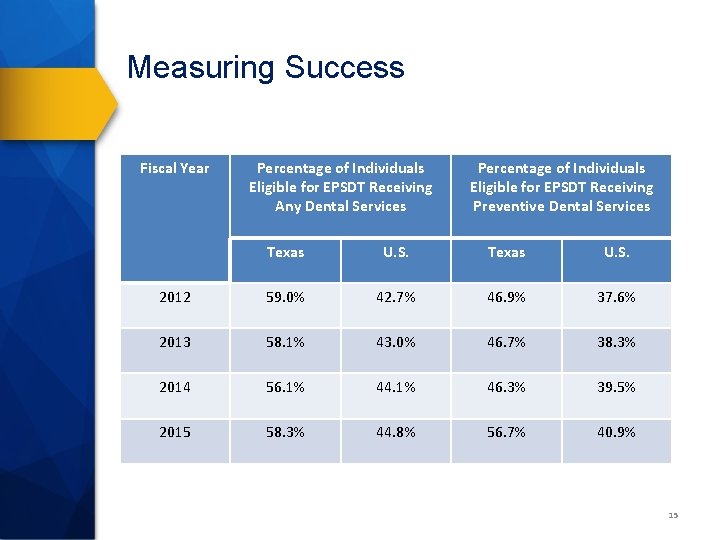
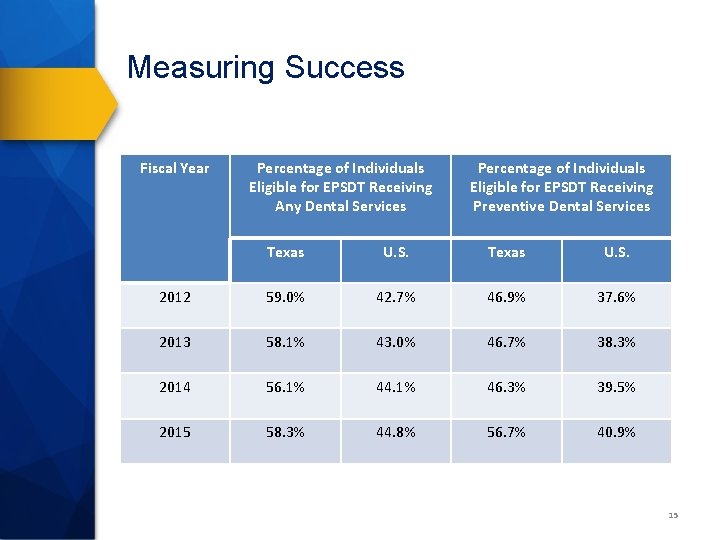
Measuring Success Fiscal Year Percentage of Individuals Eligible for EPSDT Receiving Any Dental Services Percentage of Individuals Eligible for EPSDT Receiving Preventive Dental Services Texas U. S. 2012 59. 0% 42. 7% 46. 9% 37. 6% 2013 58. 1% 43. 0% 46. 7% 38. 3% 2014 56. 1% 44. 1% 46. 3% 39. 5% 2015 58. 3% 44. 8% 56. 7% 40. 9% 15
Questions
 Wyoming medicaid dental coverage
Wyoming medicaid dental coverage Texas nemt
Texas nemt Texas health steps
Texas health steps Deputy stowers
Deputy stowers Head girl manifesto speech
Head girl manifesto speech Onondaga county sheriff civil division
Onondaga county sheriff civil division Confused deputy
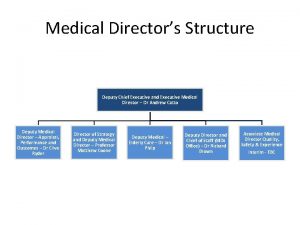
Confused deputy Deputy medical director
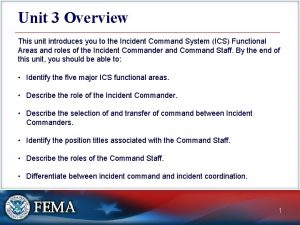
Deputy medical director Which ics functional area arranges for resources
Which ics functional area arranges for resources Deputy jody hull
Deputy jody hull Eft deputy chief
Eft deputy chief Daniel stephens md
Daniel stephens md Deputy head of division
Deputy head of division Brain hemorrhage
Brain hemorrhage Deputy manager wikipedia
Deputy manager wikipedia Who said i have trouble enough without i come five mile
Who said i have trouble enough without i come five mile Hud deputy secretary
Hud deputy secretary