Spotlight Case Treatment Challenges After Discharge Source and
- Slides: 17
Spotlight Case Treatment Challenges After Discharge
Source and Credits • This presentation is based on the November 2010 AHRQ Web. M&M Spotlight Case – See the full article at http: //webmm. ahrq. gov – CME credit is available • Commentary by: Chase Coffey, MD, Henry Ford Health System, Henry Ford Medical Group – Editor, AHRQ Web. M&M: Robert Wachter, MD – Spotlight Editor: John Q. Young, MD, MPP – Managing Editor: Erin Hartman, MS 2
Objectives • • 3 At the conclusion of this educational activity, participants should be able to: Understand types and frequencies of adverse events occurring between patient discharge from the hospital and first outpatient appointment. Appreciate the unique challenges posed by transition in care from the hospital to outpatient physician. Appreciate the problems related to tests pending at hospital discharge and best practices to address them. Describe current best practices for reducing patient safety risks associated with hospital discharge.
Case: Treatment after Discharge (1) Family members brought a 66 -year-old man with acute-on-chronic altered mental status to the emergency department (ED). Several years earlier, the patient had a craniotomy for a brain tumor, which had resulted in mental retardation. The ED obtained routine laboratory tests (including urinalysis and complete blood count [CBC]) that indicated a urinary tract infection (UTI). 4
Case: Treatment after Discharge (2) After a urine culture was obtained in the ED, the patient was started on vancomycin and admitted to the hospital. By day 3, he showed marked improvement and, according to his family, was returning to his ‘usual self’. He was switched to trimethoprim-sulfamethoxazole, an antibiotic he could take by mouth, and discharged home. The plan was for the patient to follow-up with his primary care physician in 2 weeks. 5
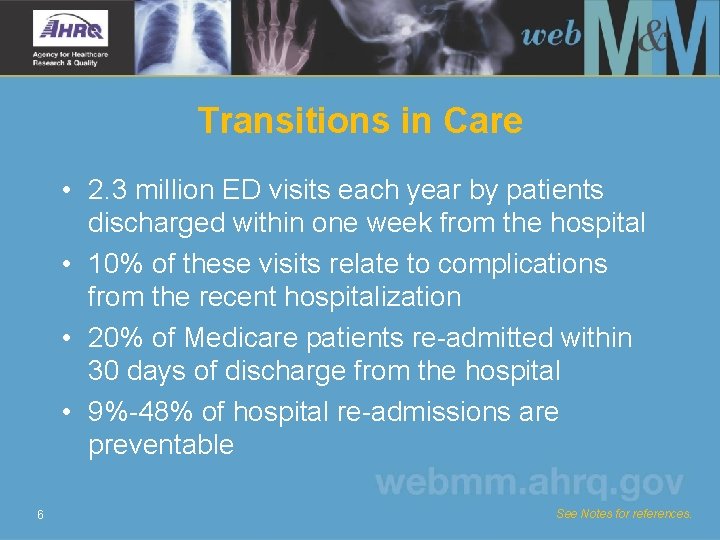
Transitions in Care • 2. 3 million ED visits each year by patients discharged within one week from the hospital • 10% of these visits relate to complications from the recent hospitalization • 20% of Medicare patients re-admitted within 30 days of discharge from the hospital • 9%-48% of hospital re-admissions are preventable 6 See Notes for references.
Problems Surrounding Discharge • • • 7 Adverse drug events Nosocomial infections Procedural complications Diagnostic errors Therapeutic errors See Notes for reference.
Post-Discharge Challenges • Ambiguity over who owns care of patient between discharge and first follow-up appointment • Sending and receiving teams often geographically separated with siloed health information systems • Patients may have poor access to follow-up care after discharge 8
Case: Treatment after Discharge (3) Eleven days later, the patient’s family brought him back to the ED after he had become increasingly disoriented and confused. His white blood cell count, which had been normal previously, was now very high (31, 000), and his blood pressure was lower than usual. 9
Case: Treatment after Discharge (4) The patient was admitted to the hospital with the diagnosis of severe sepsis. The admitting nurse noticed that the urine culture results from his prior hospital admission indicated that the patient’s infection was not sensitive to trimethoprim-sulfamethoxazole. 10
Case: Treatment after Discharge (5) Although these test results became available 2 days after the patient’s discharge, they had not been reviewed by any of the treating hospital clinicians or forwarded to the primary care physician. As a result, the patient had continued to take the trimethoprimsulfamethoxazole. His second hospitalization lasted 7 days. With the correct antibiotic, the patient made a full recovery. 11
More Challenges After Discharge • Patient work-ups often incomplete • Lack of direct or indirect communication between discharging and receiving team • Direct communication occurs 3%-20% of time and discharge summary available only 12%-34% of time at first follow-up visit • Post-discharge, patients often have heightened needs for timely care 12 See Notes for references.
Tests Pending at Discharge (TPAD) • ~40% of patients have TPAD • Nearly 10% of TPADs require physician action • Failure to follow-up on TPADs – Can lead to delays in or missed opportunities for diagnosis and treatment – Account for 25% of diagnosis-related malpractice law suits from one insurer 13 See Notes for references.
Tests Pending at Discharge (cont. ) • Most common – Microbiology (82%, e. g. , blood or sputum cultures) – Toxicology (3. 4%) – Urine studies (3. 0%) • Most academic medical centers do not have formal policies or protocols regarding followup of TPADs 14 See Notes for reference.
Managing Pending Tests • Factors associated with effective management of TPADs: – Physicians and practices with high patient safety awareness in general – Presence of electronic medical record 15 See Notes for references.
Improving the Discharge Process • Patient and family education at point of discharge • Medication reconciliation at discharge • Direct communication between discharging and receiving physician/team • Improved access to health care during the postdischarge period (e. g. , post-discharge telephone calls, scheduling appointments for patients within 1 week of discharge) 16 See Notes for references.
Take-Home Points • Adverse events after discharge are common and include adverse drug events, nosocomial infections, procedural complications, and therapeutic and diagnostic errors. • Patients are particularly vulnerable to adverse events at discharge because the discharge care transition differs significantly from other care transitions. • Tests pending at discharge (TPAD) are common, and can impact patient care. • Successful TPAD management requires physicians to have high safety awareness and to use technology for assistance. 17