SCHIZOPHRENIA 101 Theresa Clemmons DO PGY4 University of


- Slides: 16
SCHIZOPHRENIA 101 Theresa Clemmons, DO – PGY-4 University of Iowa Hospital and Clinics
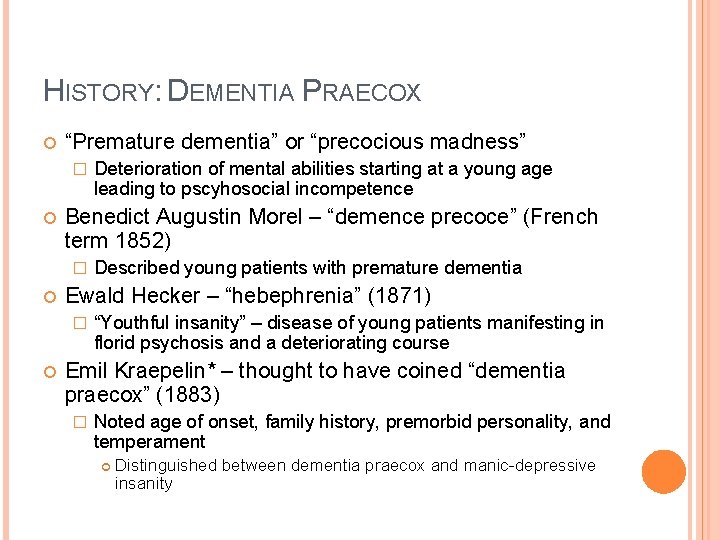
HISTORY: DEMENTIA PRAECOX “Premature dementia” or “precocious madness” � Benedict Augustin Morel – “demence precoce” (French term 1852) � Described young patients with premature dementia Ewald Hecker – “hebephrenia” (1871) � Deterioration of mental abilities starting at a young age leading to pscyhosocial incompetence “Youthful insanity” – disease of young patients manifesting in florid psychosis and a deteriorating course Emil Kraepelin* – thought to have coined “dementia praecox” (1883) � Noted age of onset, family history, premorbid personality, and temperament Distinguished between dementia praecox and manic-depressive insanity

HISTORY: SCHIZOPHRENIA Eugene Bleuler* – introduced “schizophrenia” (1908) � Described primary features of the core illness – the “four As: ” Looseness of associations Affective flattening Autism Considered cardinal component – dropped due to poor definition Ambivalence � Later became positive symptoms � And negative symptoms � Hallucinations, delusions, disorganized/catatonic behavior, disorganized speech Avolition, flat affect, ambivalence, poverty of speech Criticized “dementia praecox” as schizophrenia did not always first appear in adolescence and did not always end in deterioration
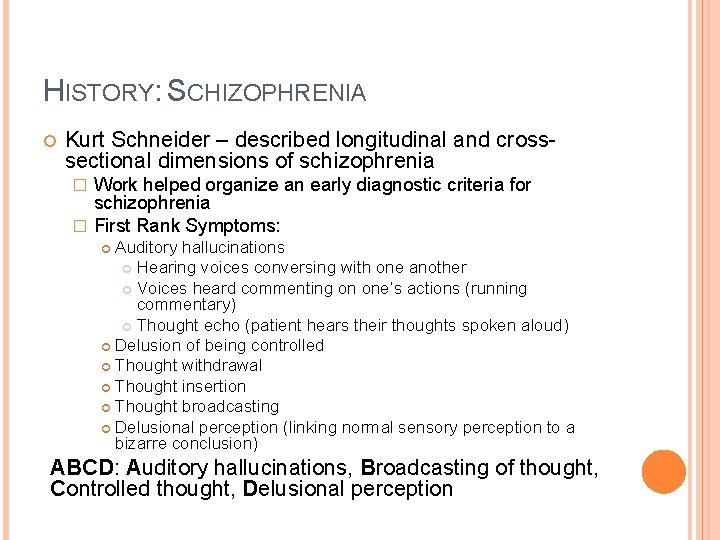
HISTORY: SCHIZOPHRENIA Kurt Schneider – described longitudinal and crosssectional dimensions of schizophrenia Work helped organize an early diagnostic criteria for schizophrenia � First Rank Symptoms: � Auditory hallucinations Hearing voices conversing with one another Voices heard commenting on one’s actions (running commentary) Thought echo (patient hears their thoughts spoken aloud) Delusion of being controlled Thought withdrawal Thought insertion Thought broadcasting Delusional perception (linking normal sensory perception to a bizarre conclusion) ABCD: Auditory hallucinations, Broadcasting of thought, Controlled thought, Delusional perception
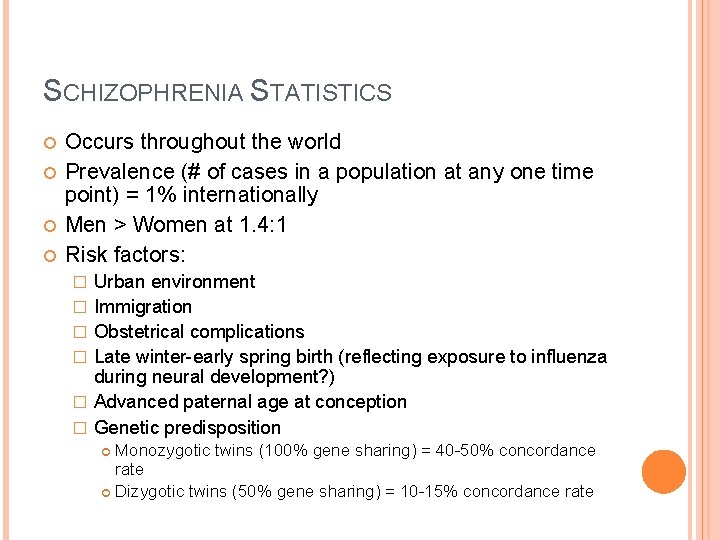
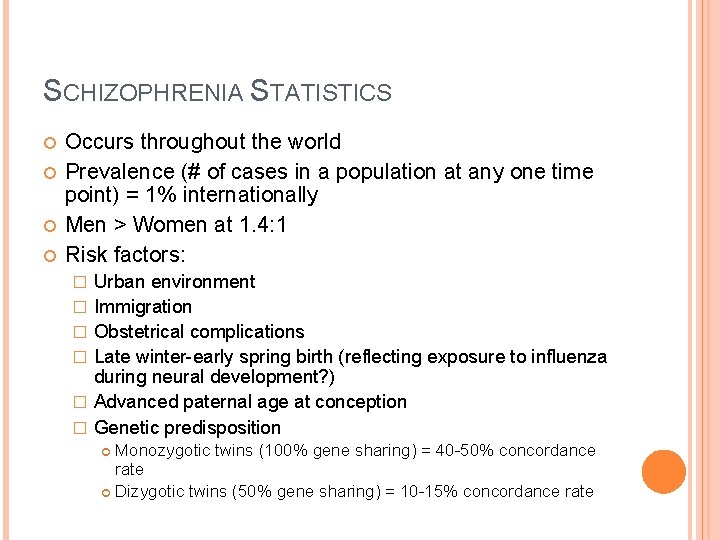
SCHIZOPHRENIA STATISTICS Occurs throughout the world Prevalence (# of cases in a population at any one time point) = 1% internationally Men > Women at 1. 4: 1 Risk factors: � � � Urban environment Immigration Obstetrical complications Late winter-early spring birth (reflecting exposure to influenza during neural development? ) Advanced paternal age at conception Genetic predisposition Monozygotic twins (100% gene sharing) = 40 -50% concordance rate Dizygotic twins (50% gene sharing) = 10 -15% concordance rate
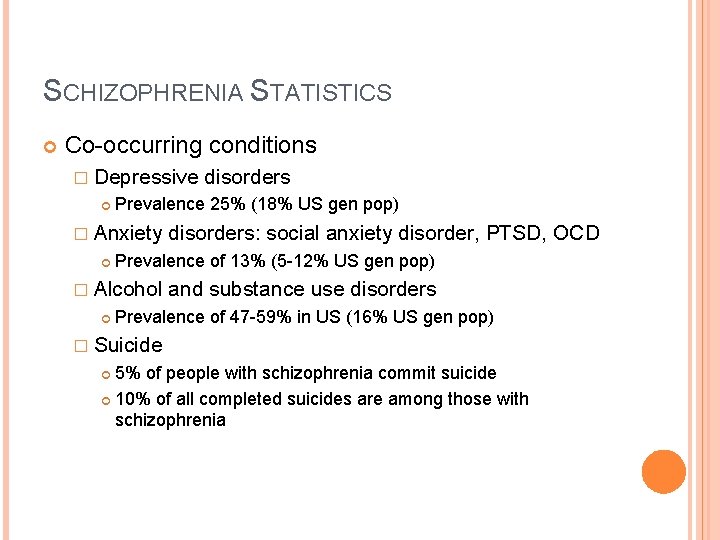
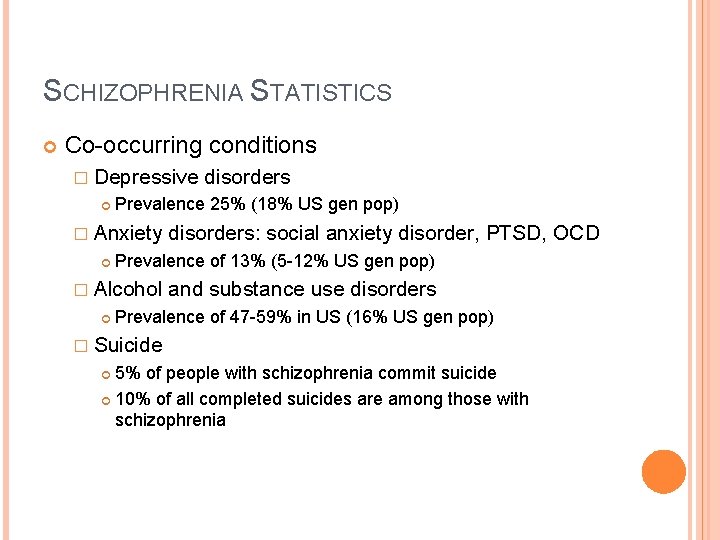
SCHIZOPHRENIA STATISTICS Co-occurring conditions � Depressive Prevalence 25% (18% US gen pop) � Anxiety disorders: social anxiety disorder, PTSD, OCD Prevalence of 13% (5 -12% US gen pop) � Alcohol disorders and substance use disorders Prevalence of 47 -59% in US (16% US gen pop) � Suicide 5% of people with schizophrenia commit suicide 10% of all completed suicides are among those with schizophrenia
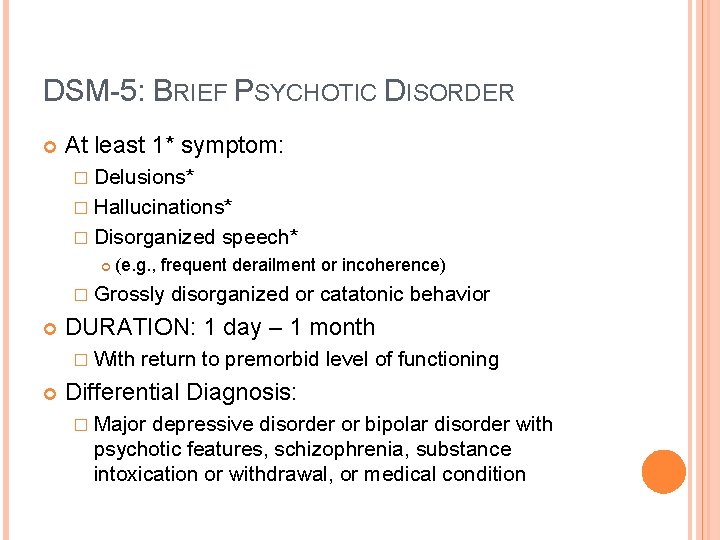
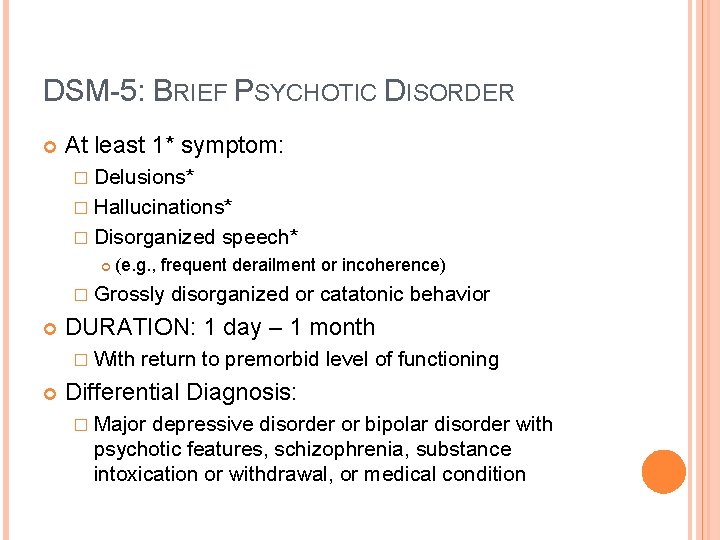
DSM-5: BRIEF PSYCHOTIC DISORDER At least 1* symptom: � Delusions* � Hallucinations* � Disorganized (e. g. , frequent derailment or incoherence) � Grossly disorganized or catatonic behavior DURATION: 1 day – 1 month � With speech* return to premorbid level of functioning Differential Diagnosis: � Major depressive disorder or bipolar disorder with psychotic features, schizophrenia, substance intoxication or withdrawal, or medical condition

DSM-5: SCHIZOPHRENIFORM DISORDER At least 2 symptoms (1* symptom): � Delusions* � Hallucinations* � Disorganized speech (e. g. , frequent derailment of incoherence) � Grossly disorganized or catatonic behavior � Negative symptoms (i. e. , diminished emotional expression or avolition) DURATION: 1 month – 6 months Differential Diagnosis: � Schizoaffective disorder, depressive disorder or bipolar disorder with psychotic features, substance intoxication/withdrawal, and medical condition
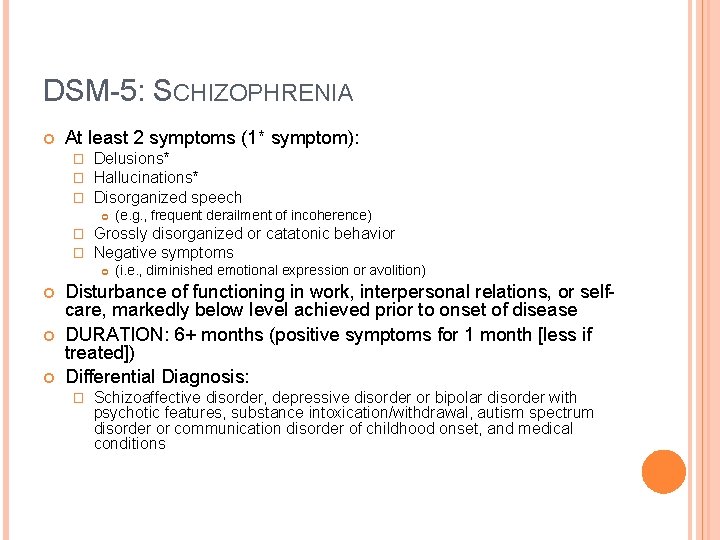
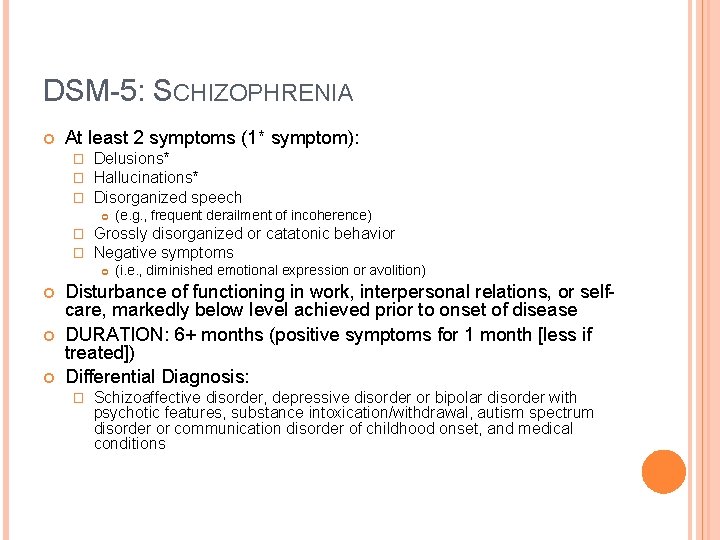
DSM-5: SCHIZOPHRENIA At least 2 symptoms (1* symptom): � � � Delusions* Hallucinations* Disorganized speech � � Grossly disorganized or catatonic behavior Negative symptoms (e. g. , frequent derailment of incoherence) (i. e. , diminished emotional expression or avolition) Disturbance of functioning in work, interpersonal relations, or selfcare, markedly below level achieved prior to onset of disease DURATION: 6+ months (positive symptoms for 1 month [less if treated]) Differential Diagnosis: � Schizoaffective disorder, depressive disorder or bipolar disorder with psychotic features, substance intoxication/withdrawal, autism spectrum disorder or communication disorder of childhood onset, and medical conditions
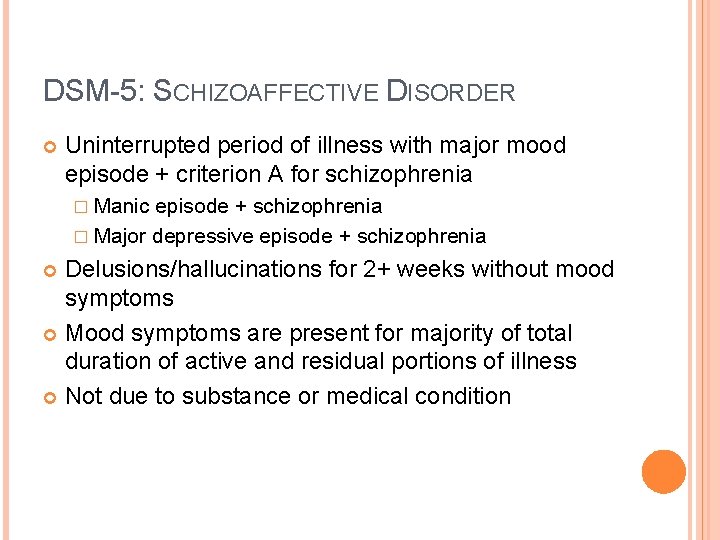
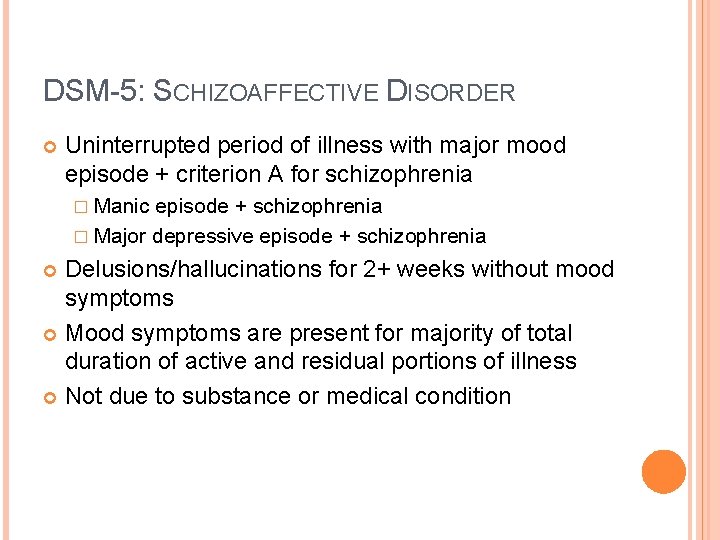
DSM-5: SCHIZOAFFECTIVE DISORDER Uninterrupted period of illness with major mood episode + criterion A for schizophrenia � Manic episode + schizophrenia � Major depressive episode + schizophrenia Delusions/hallucinations for 2+ weeks without mood symptoms Mood symptoms are present for majority of total duration of active and residual portions of illness Not due to substance or medical condition
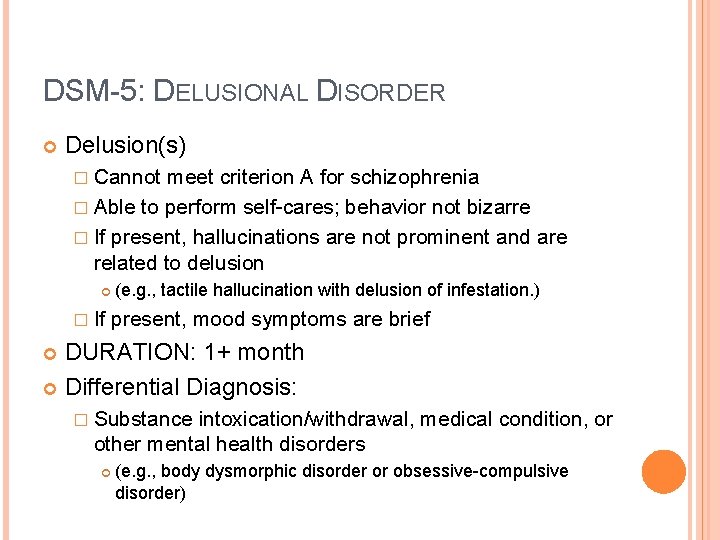
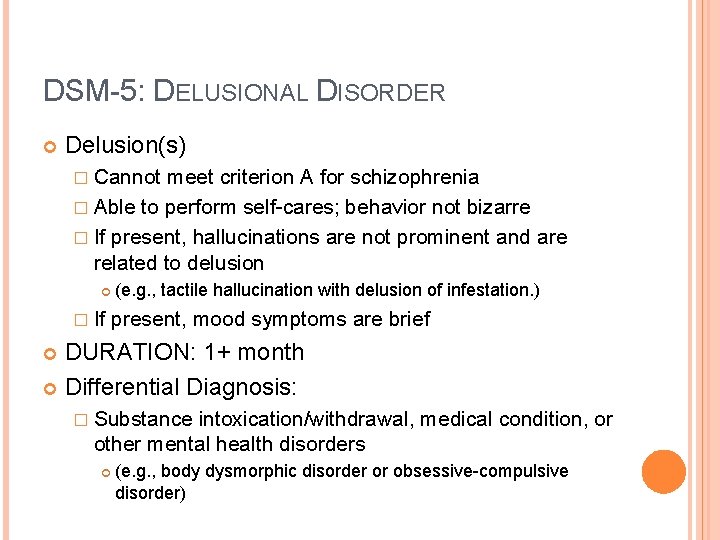
DSM-5: DELUSIONAL DISORDER Delusion(s) � Cannot meet criterion A for schizophrenia � Able to perform self-cares; behavior not bizarre � If present, hallucinations are not prominent and are related to delusion � If (e. g. , tactile hallucination with delusion of infestation. ) present, mood symptoms are brief DURATION: 1+ month Differential Diagnosis: � Substance intoxication/withdrawal, medical condition, or other mental health disorders (e. g. , body dysmorphic disorder or obsessive-compulsive disorder)
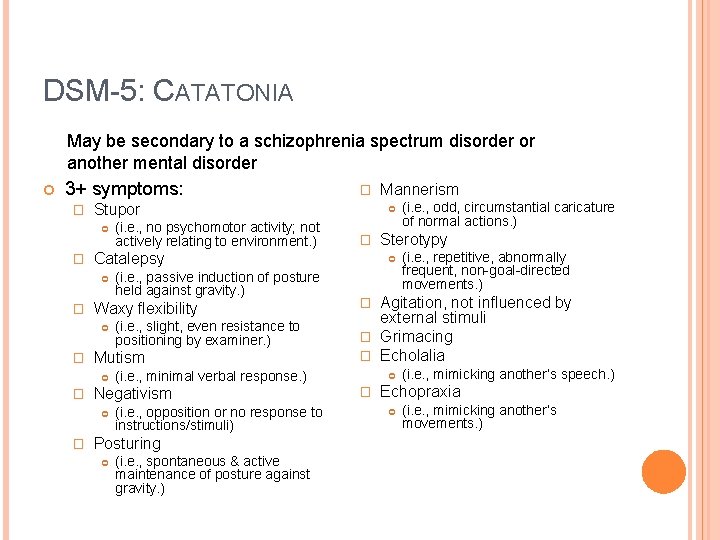
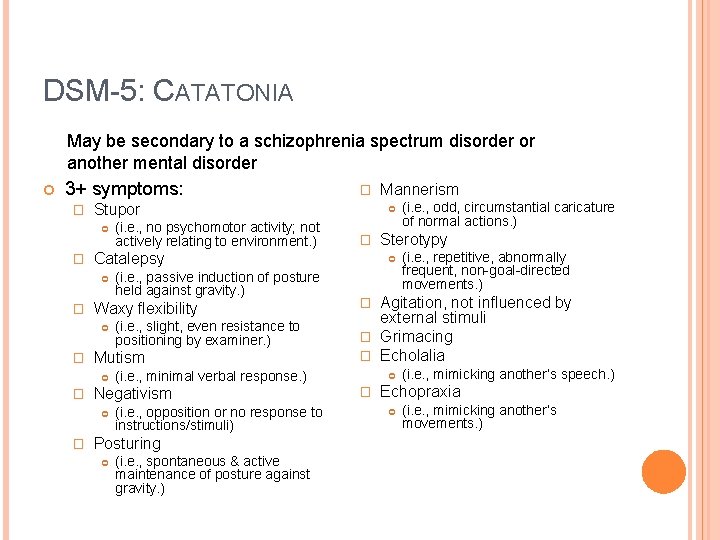
DSM-5: CATATONIA May be secondary to a schizophrenia spectrum disorder or another mental disorder 3+ symptoms: � Stupor � � (i. e. , opposition or no response to instructions/stimuli) Posturing (i. e. , spontaneous & active maintenance of posture against gravity. ) (i. e. , odd, circumstantial caricature of normal actions. ) Sterotypy (i. e. , repetitive, abnormally frequent, non-goal-directed movements. ) Agitation, not influenced by external stimuli � Grimacing � Echolalia � (i. e. , minimal verbal response. ) Negativism � (i. e. , slight, even resistance to positioning by examiner. ) Mutism � (i. e. , passive induction of posture held against gravity. ) Waxy flexibility � (i. e. , no psychomotor activity; not actively relating to environment. ) Mannerism Catalepsy � � � (i. e. , mimicking another’s speech. ) Echopraxia (i. e. , mimicking another’s movements. )
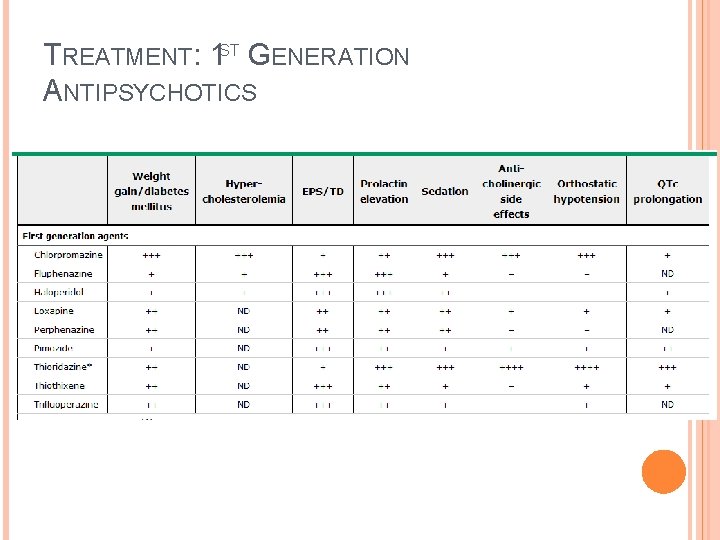
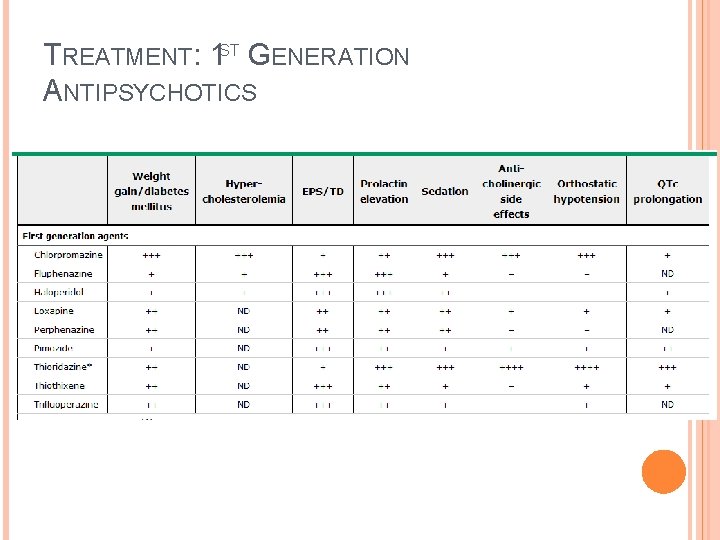
TREATMENT: 1 ST GENERATION ANTIPSYCHOTICS
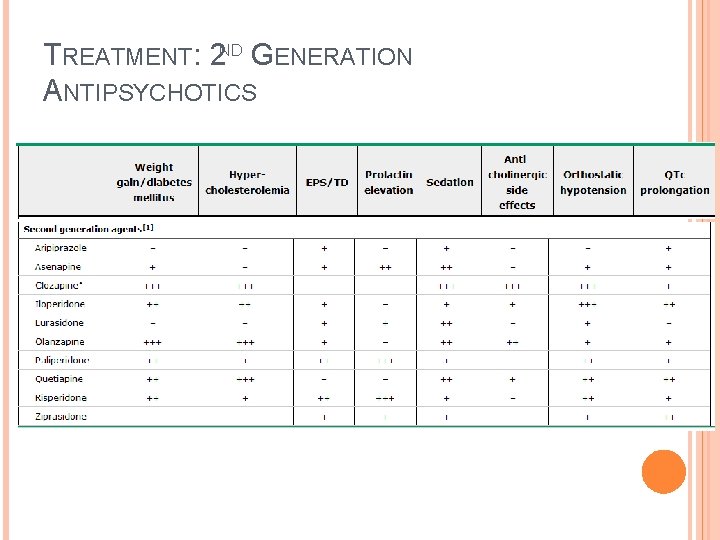
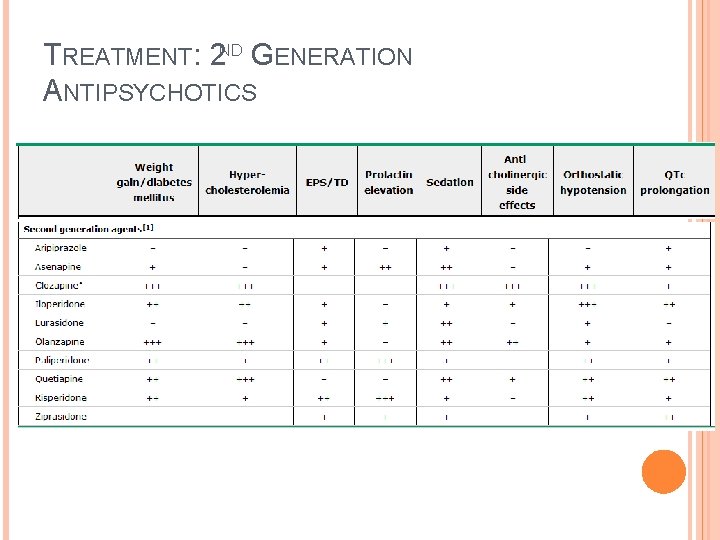
TREATMENT: 2 ND GENERATION ANTIPSYCHOTICS
TREATMENT: ELECTROCONVULSIVE THERAPY FOR SCHIZOPHRENIA Used today as an adjunct with antipsychotics for treatment-resistant schizophrenia � Randomized trial of 40 patients with schizophrenia found that combination of ECT and antipsychotic medications resulted in greater improvement of +/symptoms than antipsychotic medications alone � Meta-analysis found ECT to be superior to sham ECT, but inferior to antipsychotic medications As a rule, ECT is used for treatment-resistant schizophrenia as the results are short-lasting (requiring maintenance ECT) and due to side effects and cost of the procedure. Medications are thought to be superior in treatment of symptoms.
REFERENCES Adityanjee et al. Dementia praecox to schizophrenia: the first 100 years. Psychiatry Clin Neurosci. 1999 Aug; 53(4): 437 -48 Fischer et al. Schizophrenia: Epidemiology and pathogenesis. Up. To. Date. 2014 Aug 19. Diagnostic and Statistical Manual – 5. American Psychiatric Association. Jibson MD. First-Generation Antipsychotic Medications: Pharmacology, administration, and comparative side effects. Up. To. Date. 2014 Mar 3. Kane et al. Treatment-resistant schizophrenia. Up. To. Date. 2014 Jan 9. You. Tube: Four Patients with Schizophrenia video: https: //www. youtube. com/watch? v=b. Wa. Fqw 8 Xnp. A