Schistosoma mansoni and HIV1 infection Is there any




- Slides: 32
Schistosoma mansoni and HIV-1 infection: Is there any association? Humphrey D. Mazigo, Ph. D
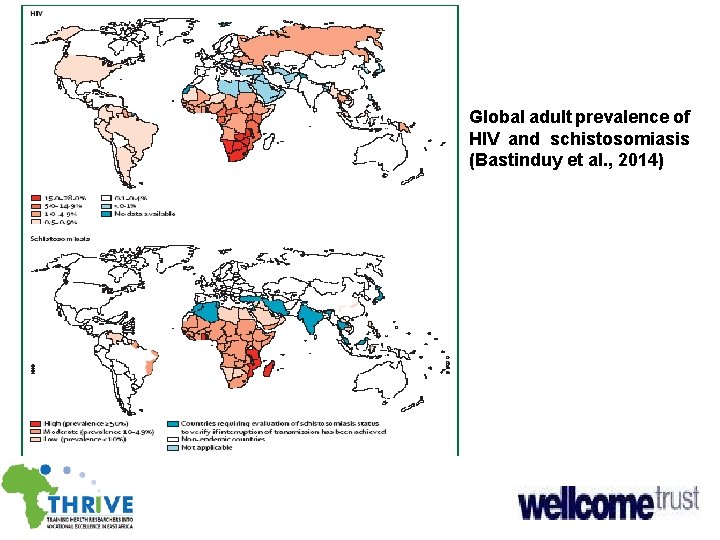
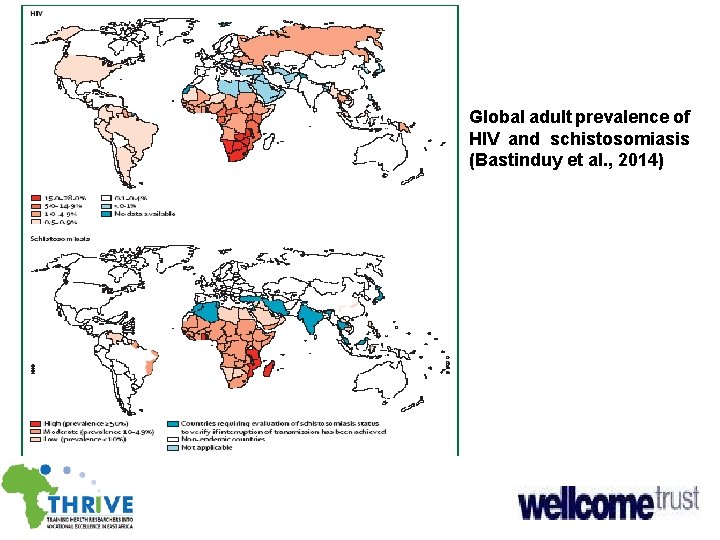
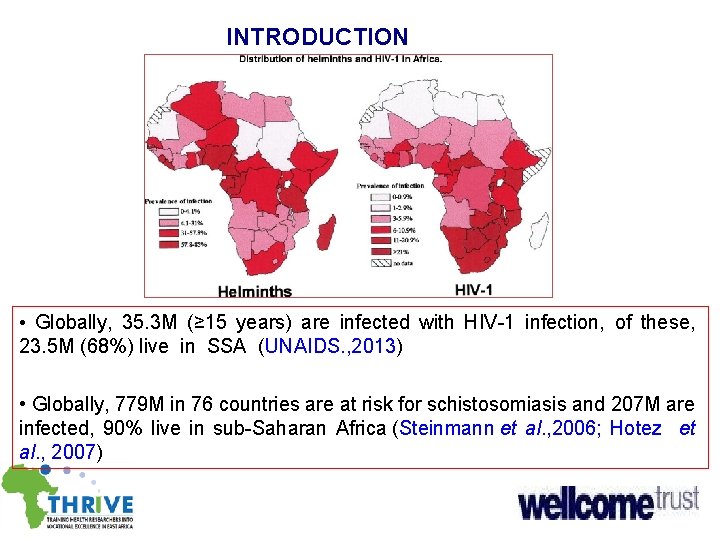
Global adult prevalence of HIV and schistosomiasis (Bastinduy et al. , 2014)
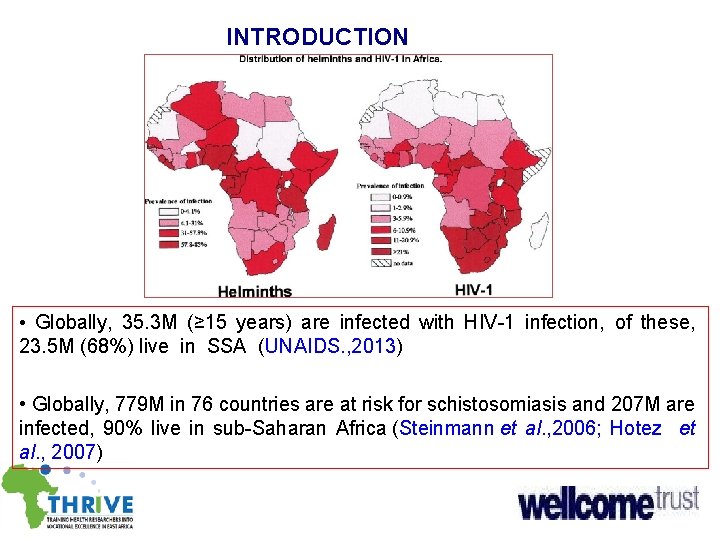
INTRODUCTION • Globally, 35. 3 M (≥ 15 years) are infected with HIV-1 infection, of these, 23. 5 M (68%) live in SSA (UNAIDS. , 2013) • Globally, 779 M in 76 countries are at risk for schistosomiasis and 207 M are infected, 90% live in sub-Saharan Africa (Steinmann et al. , 2006; Hotez et al. , 2007)
Global burden of diseases • The DALYs lost due to schistosomiasis are estimated at 4. 5 M • The DALYs lost due to HIV infection is >80 M • Combined DALYs results into significant morbidities and mortalities Hotez et al. , 2006; 2014

Schistosomiasis in Tanzania • Two spp S. mansoni and S. haematobium are endemic and widely spread in country • S. mansoni is wide spread along the large water bodies • S. haematobium is mainly in small water bodies • National prevalence: 52% but varies between regions • Health effect of S. mansoni infection: Periportal fibrosis, hepatomegaly, splenomegaly and hepatosplenomegaly and death associatted with portal hypertension, oesophageal varices and hemetemesis Mazigo et al. , 2012; Rollinson et al. , 2012
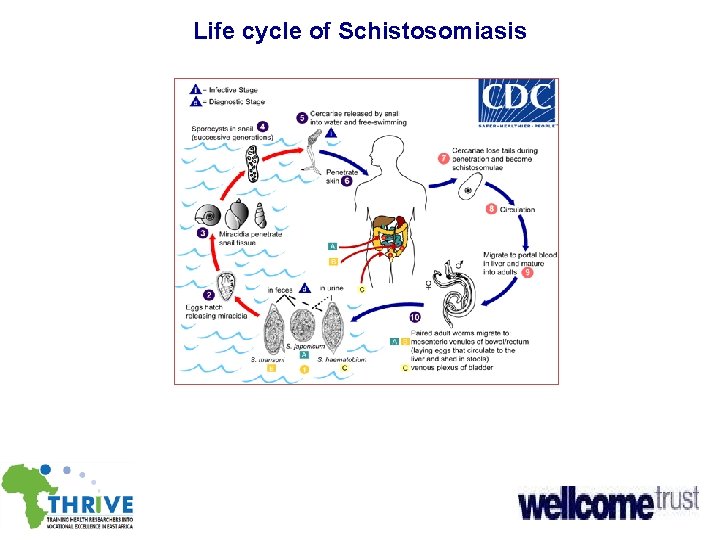
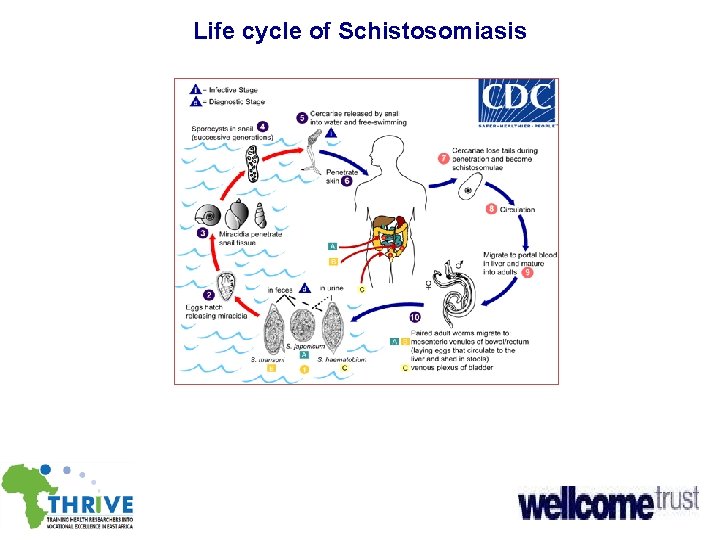
Life cycle of Schistosomiasis
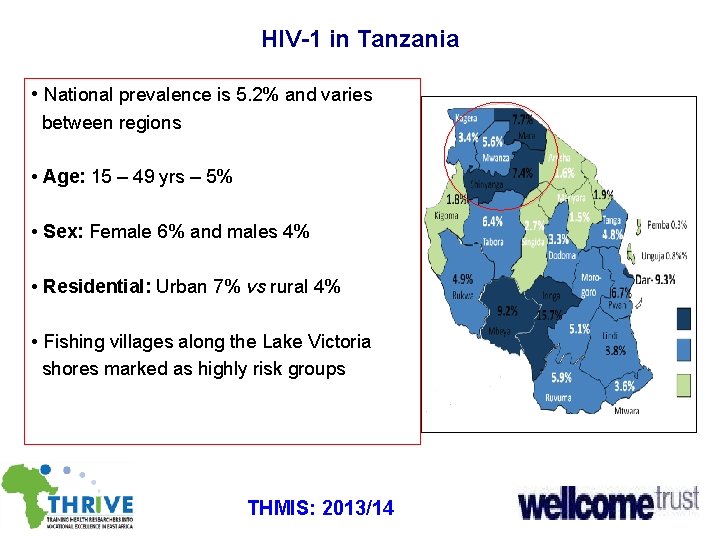
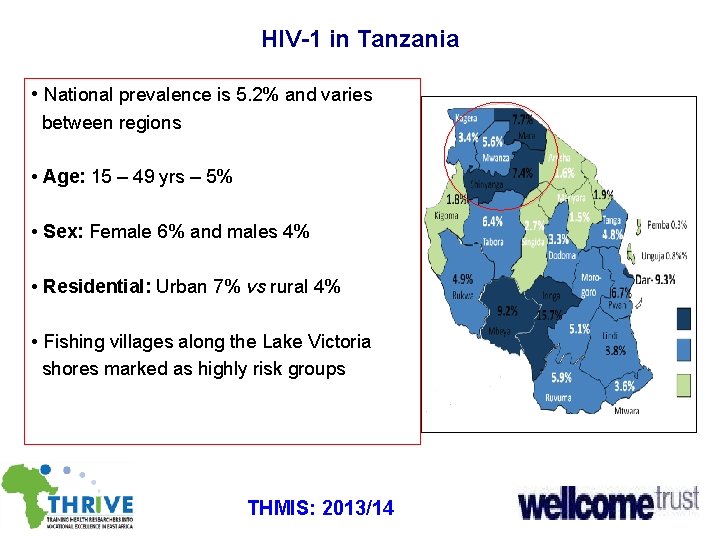
HIV-1 in Tanzania • National prevalence is 5. 2% and varies between regions • Age: 15 – 49 yrs – 5% • Sex: Female 6% and males 4% • Residential: Urban 7% vs rural 4% • Fishing villages along the Lake Victoria shores marked as highly risk groups THMIS: 2013/14
HIV-1 and S. mansoni co-infections • Because of the overlap of HIV-1 and S. mansoni in SSA, half of 25 M HIV infected individuals may be co-infected (Secor 2000: Bentwich et al. , 2000) • Hypothesis: - co-infection of HIV-1 and S. mansoni may enhance virulence of each other within a co-infected host (Lawn 2001; Wolday 2002) • But, the role played by concurrent HIV-1 infection as accelerating factor for S. mansoni infection, related morbidities and PZQ treatment outcome remain a topic of further studies
HIV-1 and S. mansoni co-infections u The effects of HIV-1 on schistosomiasis u CD 4+ T cell reductions by HIV-1: - Alters eggs excretion efficiency (Karanja et al. , 1997) - Decrease fibrogenesis, hence, severe hepatic morbidities (Mwinzi et al. , 2001) - Increases susceptible to re-infection with Schistosomes (Karanja et al. , 2002) - Low CD 4+ T cell counts are associated with reduced levels of eosinophils which are necessary for resistance to repeated schistosomal infections (Ganley et al. , 2006)
HIV-1 and S. mansoni co-infections The effects of schistosomiasis in HIV-1 • Infections with schistosomes cause chronic stimulation of the immune system with a strong bias towards Th 2 CD 4+ response (Pearce et al. , 1991). • Th 2 response to Schistosomes Ag down-regulates Th 1 -type responses which are necessary for efficient antiviral CD 8+ CTL prod. (Mc. Elroy et al. , 2005). • HIV replicates more rapidly in activated T cells with Schistosomes Ag and CD 4+ T cells lines are more easily affected than Th 1 (Lawn et al. , 1991). • In Ethiopia, a study of HIV-1 infected and uninfected, helminth infection was associated with increased T- cell activation (Kassu, 2003). • In HIV-uninfected indiv. increased T-cell activation make them more susceptible to HIV infection (Kassu, 2003).
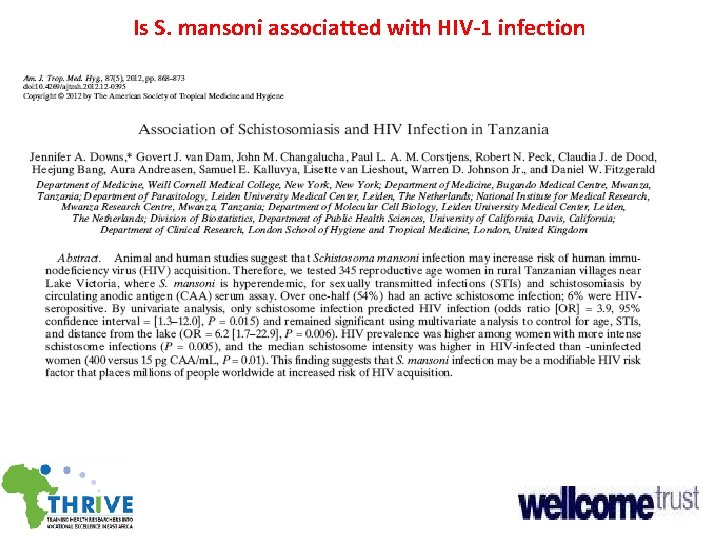
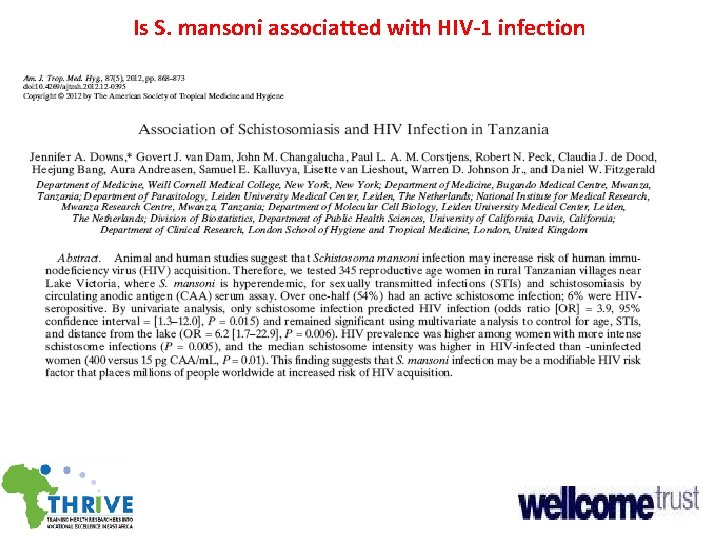
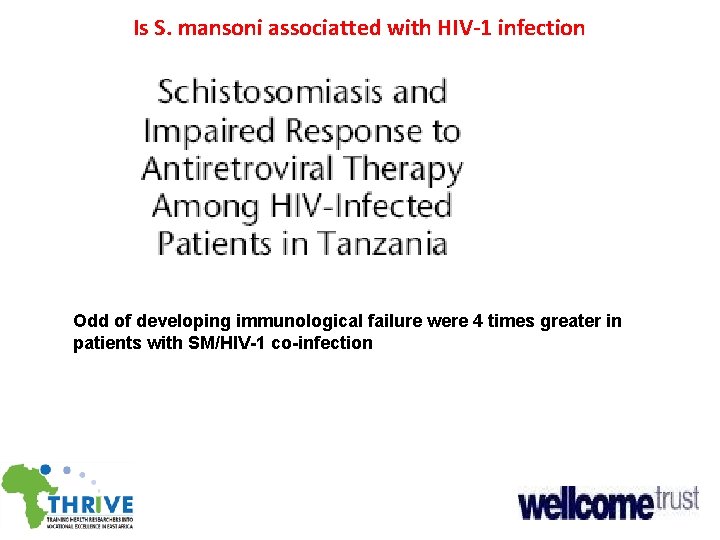
Is S. mansoni associatted with HIV-1 infection
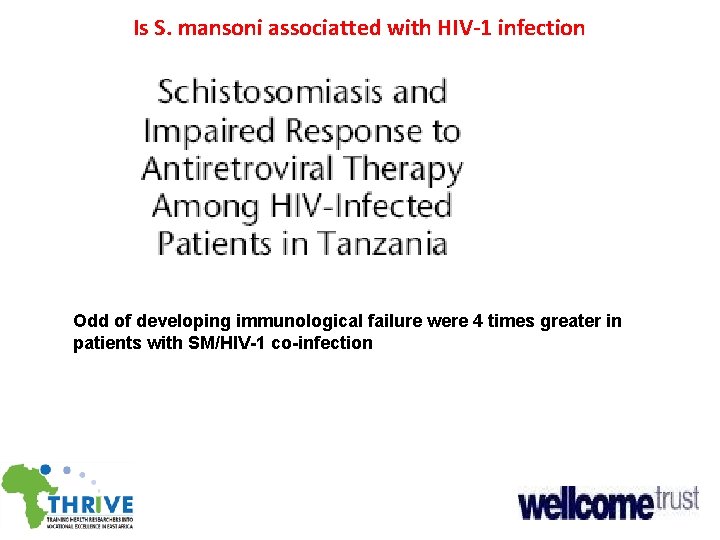
Is S. mansoni associatted with HIV-1 infection Odd of developing immunological failure were 4 times greater in patients with SM/HIV-1 co-infection
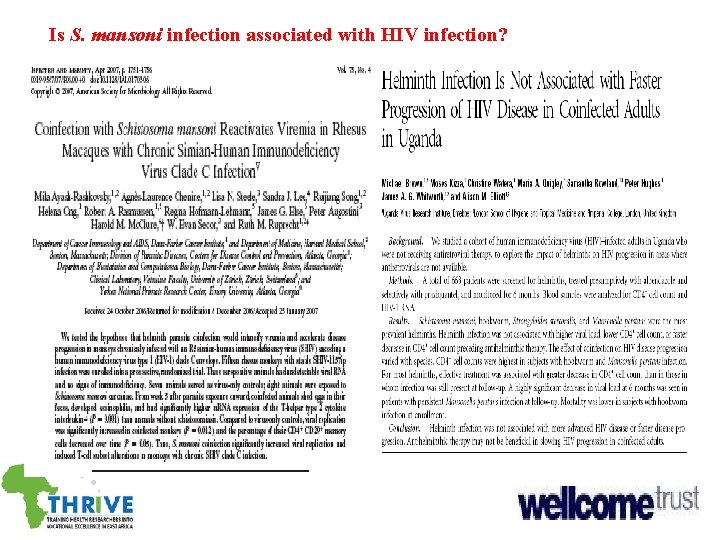
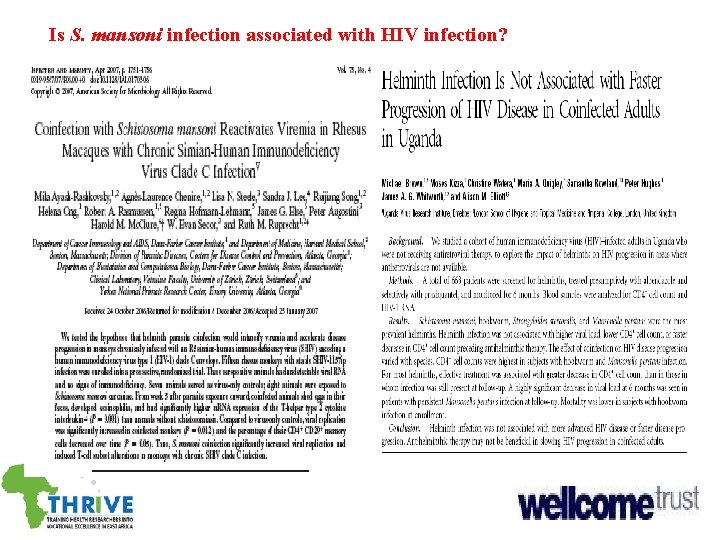
Is S. mansoni infection associated with HIV infection?
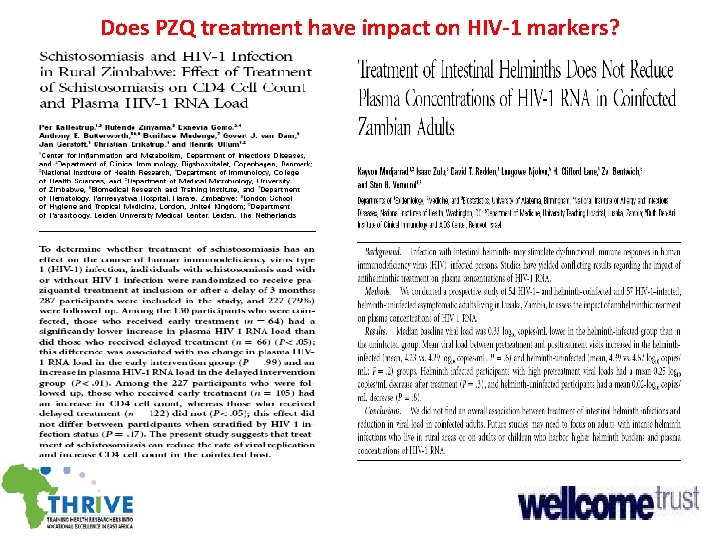
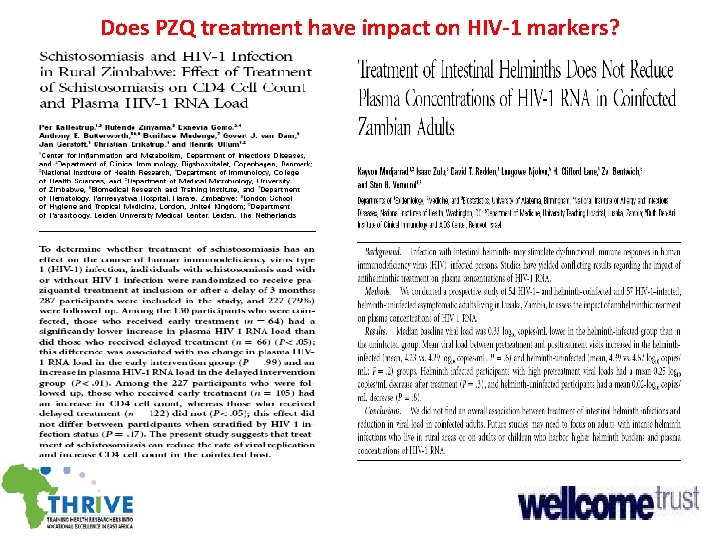
Does PZQ treatment have impact on HIV-1 markers?

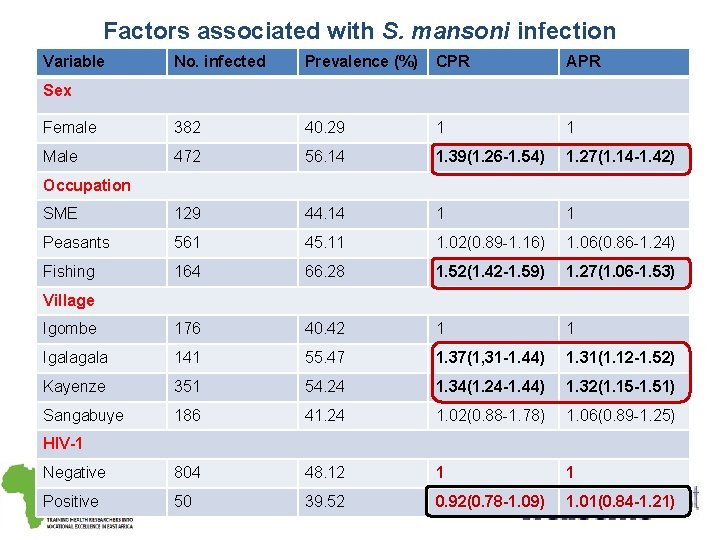
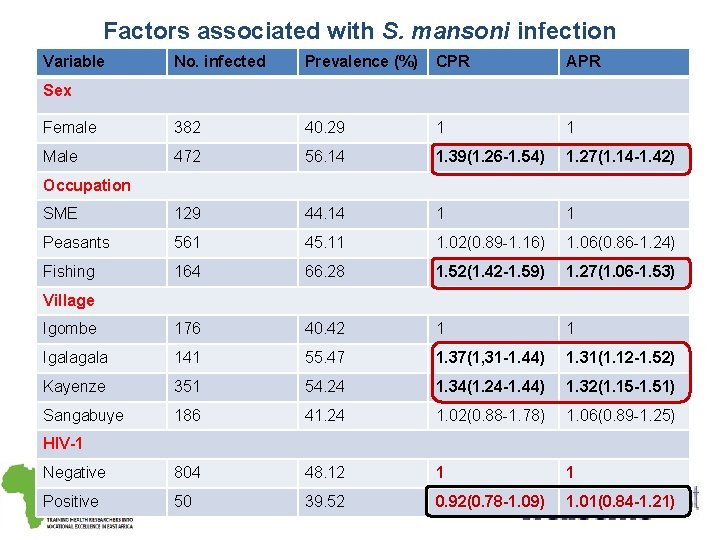
Factors associated with S. mansoni infection Variable No. infected Prevalence (%) CPR APR Female 382 40. 29 1 1 Male 472 56. 14 1. 39(1. 26 -1. 54) 1. 27(1. 14 -1. 42) SME 129 44. 14 1 1 Peasants 561 45. 11 1. 02(0. 89 -1. 16) 1. 06(0. 86 -1. 24) Fishing 164 66. 28 1. 52(1. 42 -1. 59) 1. 27(1. 06 -1. 53) Igombe 176 40. 42 1 1 Igala 141 55. 47 1. 37(1, 31 -1. 44) 1. 31(1. 12 -1. 52) Kayenze 351 54. 24 1. 34(1. 24 -1. 44) 1. 32(1. 15 -1. 51) Sangabuye 186 41. 24 1. 02(0. 88 -1. 78) 1. 06(0. 89 -1. 25) Negative 804 48. 12 1 1 Positive 50 39. 52 0. 92(0. 78 -1. 09) 1. 01(0. 84 -1. 21) Sex Occupation Village HIV-1
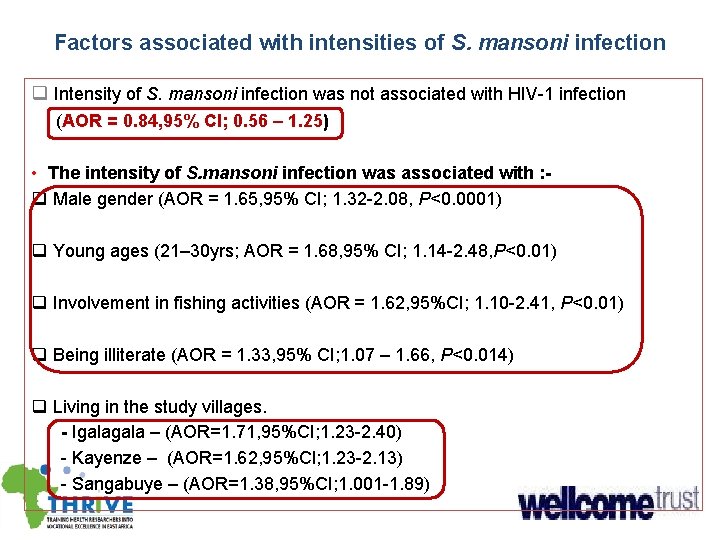
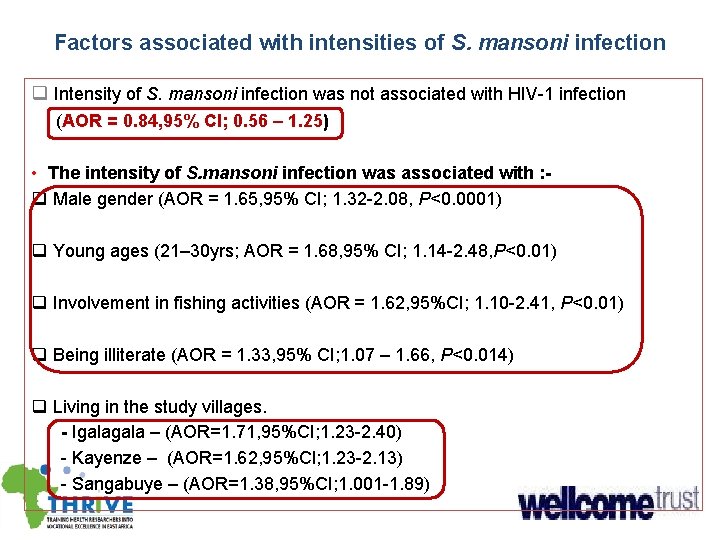
Factors associated with intensities of S. mansoni infection q Intensity of S. mansoni infection was not associated with HIV-1 infection (AOR = 0. 84, 95% CI; 0. 56 – 1. 25) • The intensity of S. mansoni infection was associated with : q Male gender (AOR = 1. 65, 95% CI; 1. 32 -2. 08, P<0. 0001) q Young ages (21– 30 yrs; AOR = 1. 68, 95% CI; 1. 14 -2. 48, P<0. 01) q Involvement in fishing activities (AOR = 1. 62, 95%CI; 1. 10 -2. 41, P<0. 01) q Being illiterate (AOR = 1. 33, 95% CI; 1. 07 – 1. 66, P<0. 014) q Living in the study villages. - Igala – (AOR=1. 71, 95%CI; 1. 23 -2. 40) - Kayenze – (AOR=1. 62, 95%CI; 1. 23 -2. 13) - Sangabuye – (AOR=1. 38, 95%CI; 1. 001 -1. 89)
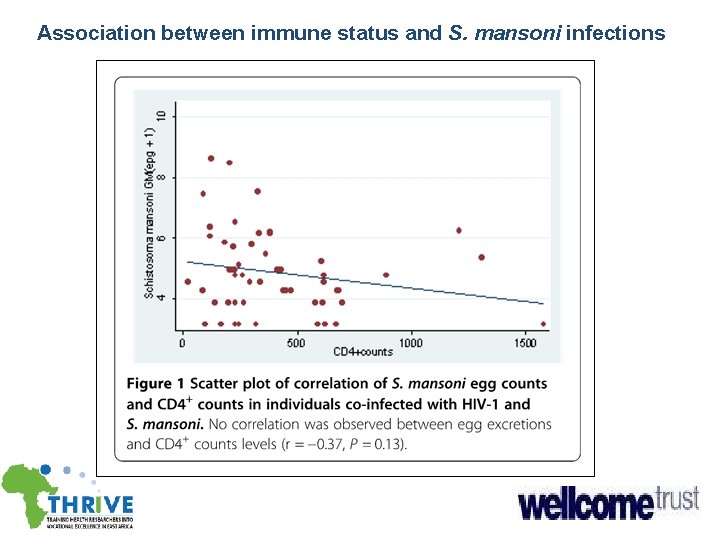
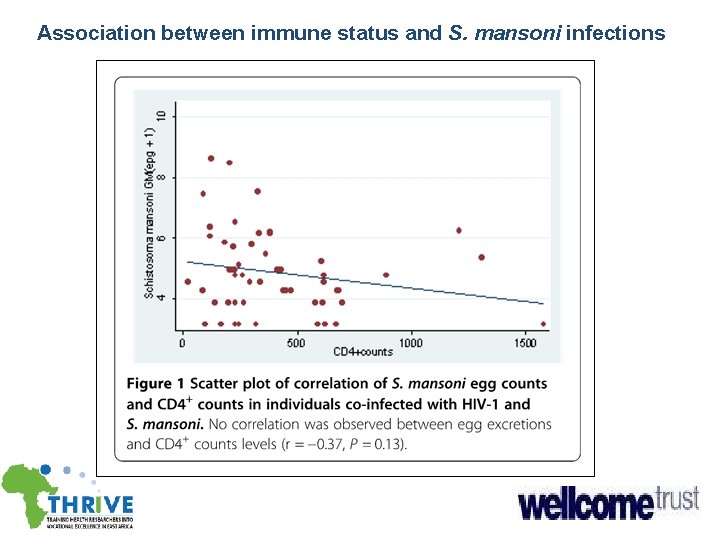
Association between immune status and S. mansoni infections

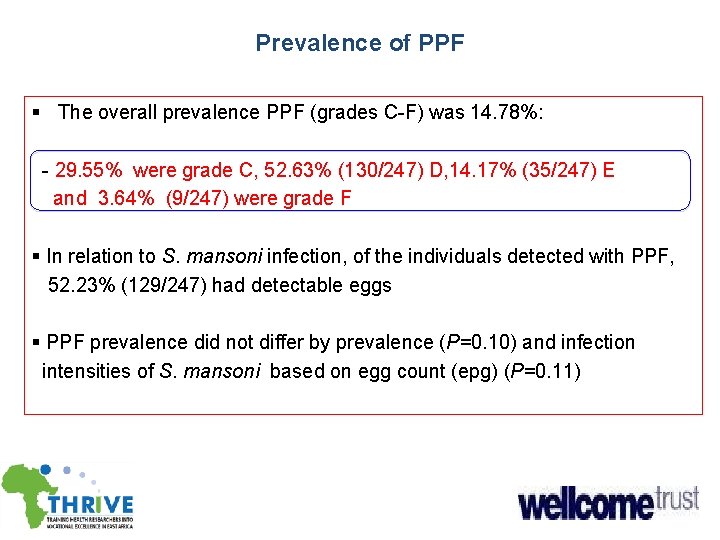
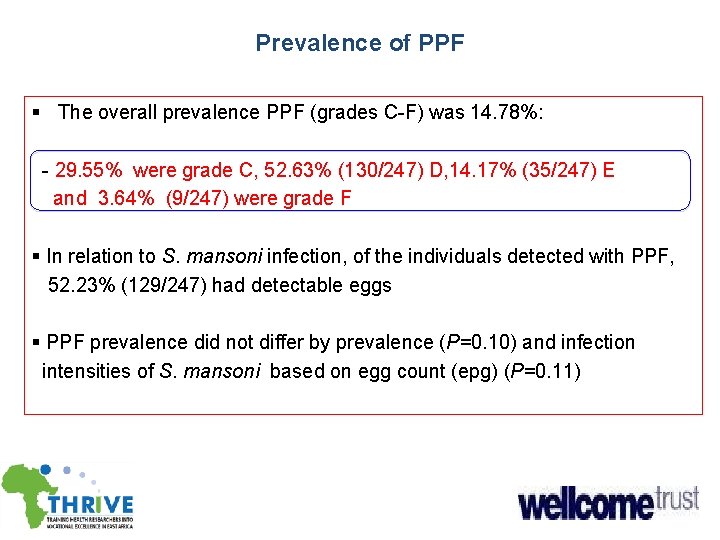
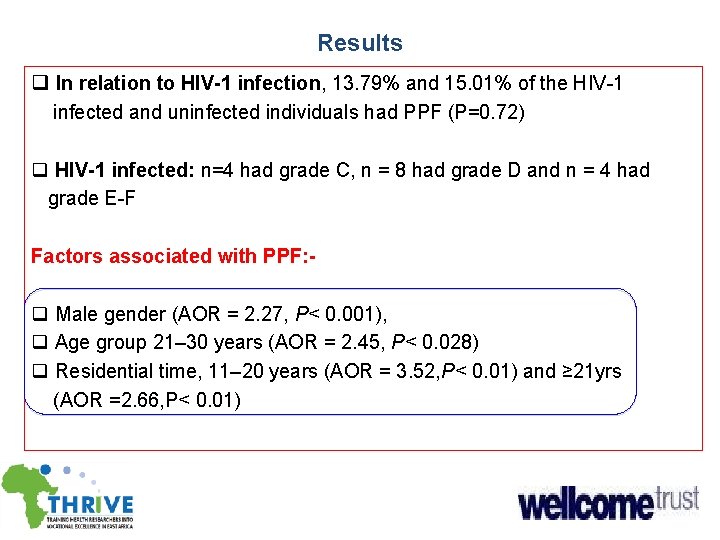
Prevalence of PPF § The overall prevalence PPF (grades C-F) was 14. 78%: - 29. 55% were grade C, 52. 63% (130/247) D, 14. 17% (35/247) E and 3. 64% (9/247) were grade F § In relation to S. mansoni infection, of the individuals detected with PPF, 52. 23% (129/247) had detectable eggs § PPF prevalence did not differ by prevalence (P=0. 10) and infection intensities of S. mansoni based on egg count (epg) (P=0. 11)
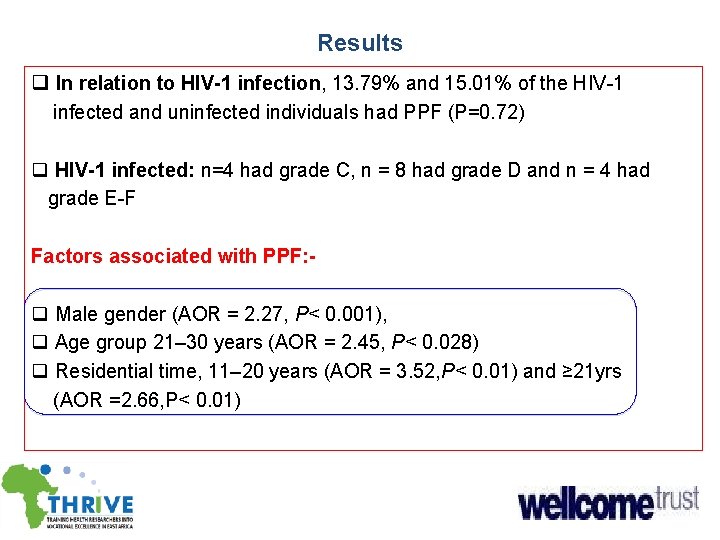
Results q In relation to HIV-1 infection, 13. 79% and 15. 01% of the HIV-1 infected and uninfected individuals had PPF (P=0. 72) q HIV-1 infected: n=4 had grade C, n = 8 had grade D and n = 4 had grade E-F Factors associated with PPF: - q Male gender (AOR = 2. 27, P< 0. 001), q Age group 21– 30 years (AOR = 2. 45, P< 0. 028) q Residential time, 11– 20 years (AOR = 3. 52, P< 0. 01) and ≥ 21 yrs (AOR =2. 66, P< 0. 01)
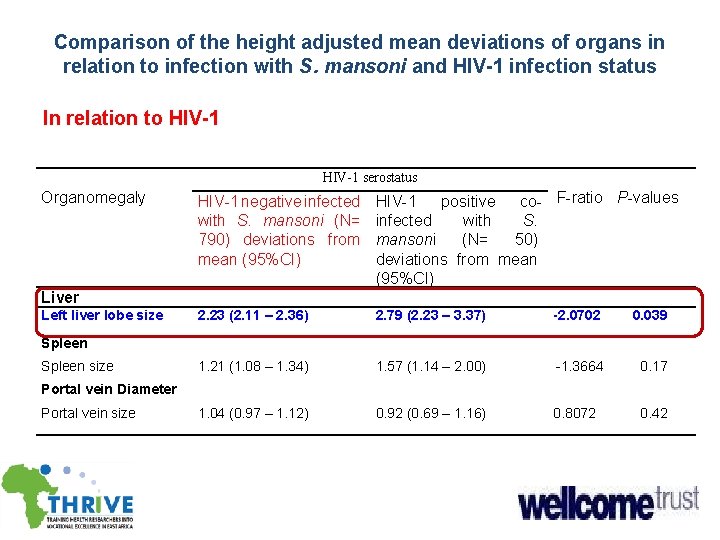
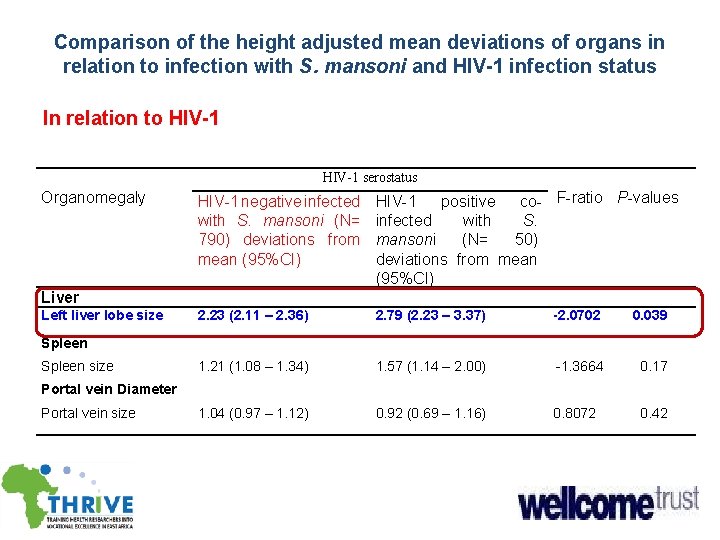
Comparison of the height adjusted mean deviations of organs in relation to infection with S. mansoni and HIV-1 infection status In relation to HIV-1 serostatus Organomegaly HIV-1 negative infected with S. mansoni (N= 790) deviations from mean (95%CI) HIV-1 positive co- F-ratio P-values infected with S. mansoni (N= 50) deviations from mean (95%CI) 2. 23 (2. 11 – 2. 36) 2. 79 (2. 23 – 3. 37) -2. 0702 0. 039 1. 21 (1. 08 – 1. 34) 1. 57 (1. 14 – 2. 00) -1. 3664 0. 17 1. 04 (0. 97 – 1. 12) 0. 92 (0. 69 – 1. 16) 0. 8072 0. 42 Liver Left liver lobe size Spleen size Portal vein Diameter Portal vein size
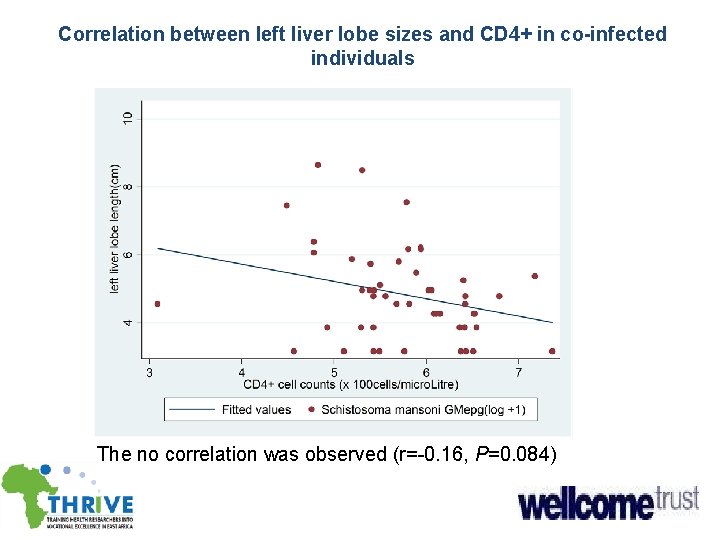
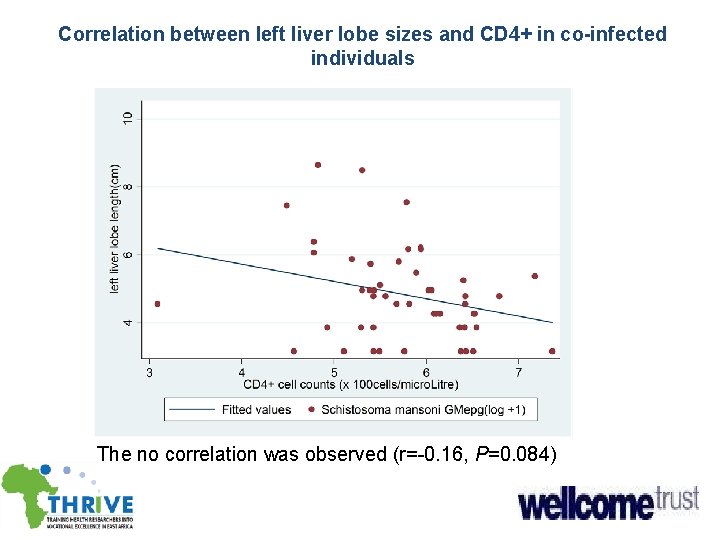
Correlation between left liver lobe sizes and CD 4+ in co-infected individuals The no correlation was observed (r=-0. 16, P=0. 084)
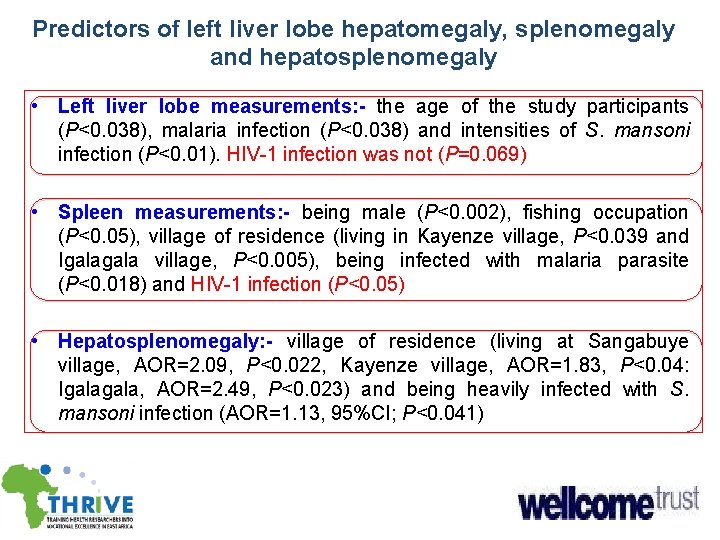
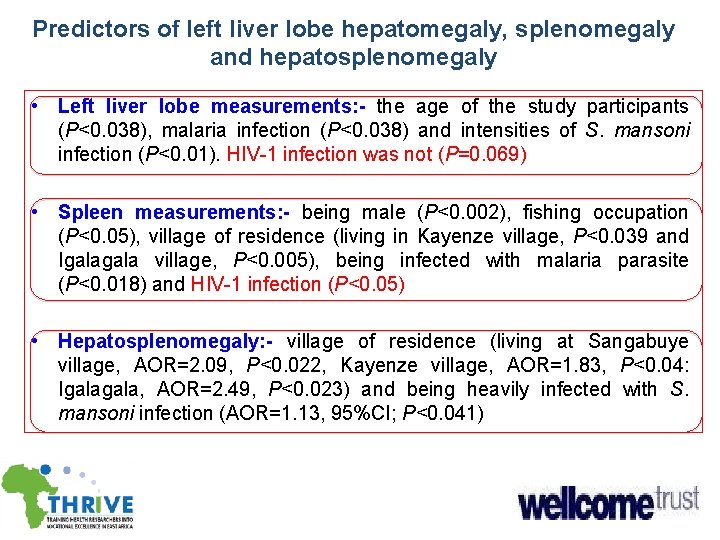
Predictors of left liver lobe hepatomegaly, splenomegaly and hepatosplenomegaly • Left liver lobe measurements: - the age of the study participants (P<0. 038), malaria infection (P<0. 038) and intensities of S. mansoni infection (P<0. 01). HIV-1 infection was not (P=0. 069) • Spleen measurements: - being male (P<0. 002), fishing occupation (P<0. 05), village of residence (living in Kayenze village, P<0. 039 and Igala village, P<0. 005), being infected with malaria parasite (P<0. 018) and HIV-1 infection (P<0. 05) • Hepatosplenomegaly: - village of residence (living at Sangabuye village, AOR=2. 09, P<0. 022, Kayenze village, AOR=1. 83, P<0. 04: Igala, AOR=2. 49, P<0. 023) and being heavily infected with S. mansoni infection (AOR=1. 13, 95%CI; P<0. 041)
Objective 3 a
Parasitological cure rates in relation to HIV-1 serostatus • Overall parasitological cure rate: 61. 80% (n=343/555) • HIV-1 negative: 526 infected with S. mansoni at baseline, cure rate: 62. 19% (329/555) • HIV-1 + S. mansoni: - cure rate: 48. 28% (14/29) • No significance difference (P= 0. 12)
Parasitological cure rates in relation to CD 4+ cells counts • Co-infected with CD 4+ cell counts <350 cells/µL: cure rate 43. 75%(7/16) • Co-infected with CD 4+ cells counts ≥ 350 cells/µL: cure rate: 66. 67%(8/12).
Comparison of HIV-1 viral loads, CD 4 -Th 2 lymphocytes and effects of praziquantel treatment among adults infected or not with S. mansoni in fishing villages of North-Western Tanzania. Infectious Diseases of Poverty
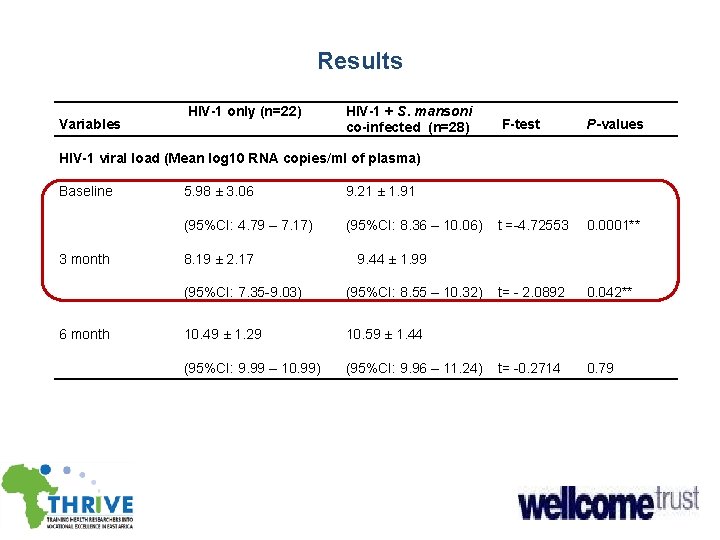
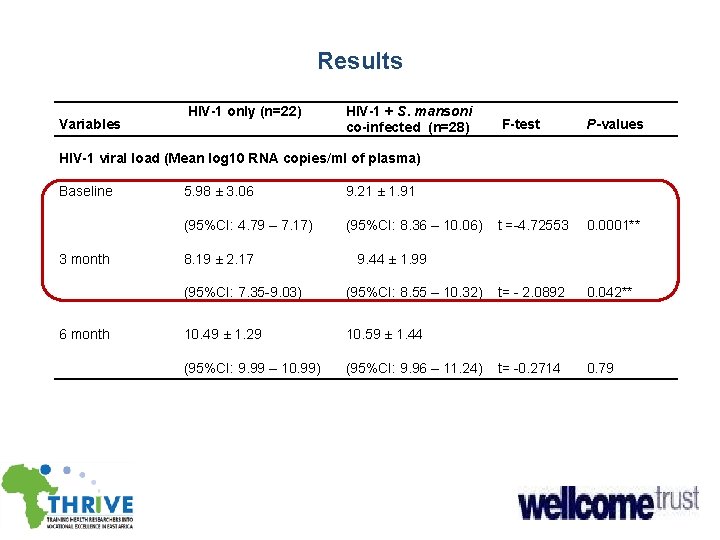
Results Variables HIV-1 only (n=22) HIV-1 + S. mansoni co-infected (n=28) F-test P-values t =-4. 72553 0. 0001** t= - 2. 0892 0. 042** t= -0. 2714 0. 79 HIV-1 viral load (Mean log 10 RNA copies/ml of plasma) Baseline 3 month 6 month 5. 98 ± 3. 06 9. 21 ± 1. 91 (95%CI: 4. 79 – 7. 17) (95%CI: 8. 36 – 10. 06) 8. 19 ± 2. 17 9. 44 ± 1. 99 (95%CI: 7. 35 -9. 03) (95%CI: 8. 55 – 10. 32) 10. 49 ± 1. 29 10. 59 ± 1. 44 (95%CI: 9. 99 – 10. 99) (95%CI: 9. 96 – 11. 24)
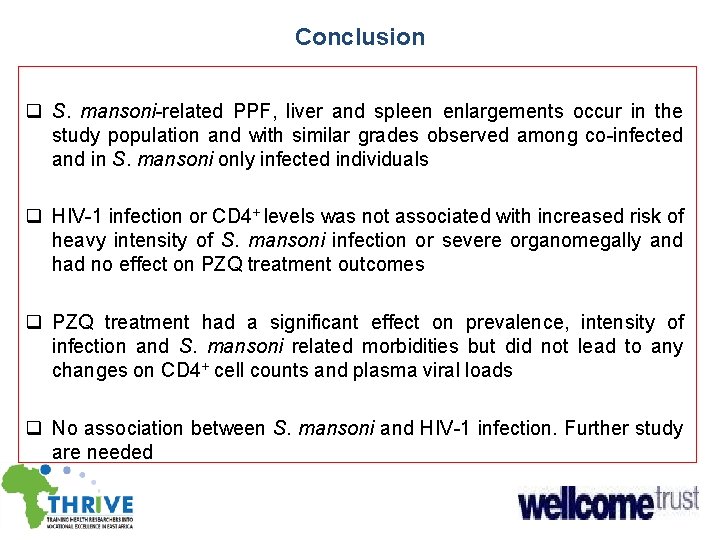
Conclusion q S. mansoni-related PPF, liver and spleen enlargements occur in the study population and with similar grades observed among co-infected and in S. mansoni only infected individuals q HIV-1 infection or CD 4+ levels was not associated with increased risk of heavy intensity of S. mansoni infection or severe organomegally and had no effect on PZQ treatment outcomes q PZQ treatment had a significant effect on prevalence, intensity of infection and S. mansoni related morbidities but did not lead to any changes on CD 4+ cell counts and plasma viral loads q No association between S. mansoni and HIV-1 infection. Further study are needed

Asanteni
 Daur hidup cacing darah
Daur hidup cacing darah Schistosoma mansoni
Schistosoma mansoni Ovo schistosoma mansoni morfologia
Ovo schistosoma mansoni morfologia There any any
There any any Some ve any kullanımı
Some ve any kullanımı Spirometra mansoni
Spirometra mansoni Piperazina dosis
Piperazina dosis Berapa ukuran telur diphyllobothrium latum
Berapa ukuran telur diphyllobothrium latum Life cycle of fasciola hepatica
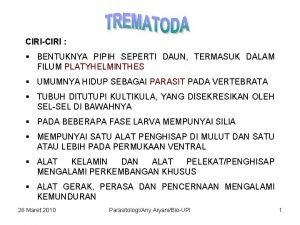
Life cycle of fasciola hepatica Trematoda
Trematoda Fasciolopsis buski
Fasciolopsis buski Schistosoma life cycle stages
Schistosoma life cycle stages Siklus hidup metagonimus yokogawai
Siklus hidup metagonimus yokogawai Schistosoma
Schistosoma S
S Schistosomiasis
Schistosomiasis Schistosoma haematobium life cycle
Schistosoma haematobium life cycle Epidermis
Epidermis Strepsiptera in humans
Strepsiptera in humans Endoparazité
Endoparazité Any to any connectivity
Any to any connectivity Any question atau any questions
Any question atau any questions Usp solubility
Usp solubility There won't be any schools in the future
There won't be any schools in the future Is there any bias in gender roles based on the excerpt
Is there any bias in gender roles based on the excerpt Question tags definition
Question tags definition Uncountable noun singular or plural
Uncountable noun singular or plural Irregular uncountable nouns
Irregular uncountable nouns Kleene plus
Kleene plus Short workings are recouped when there is *
Short workings are recouped when there is * There are books in chair
There are books in chair 51 prime or composite
51 prime or composite There is and there
There is and there