SameDay Discharge PostPCI Arnold Seto MD MPA Long







- Slides: 16
Same-Day Discharge Post-PCI Arnold Seto, MD, MPA Long Beach VA Medical Center University of California, Irvine

Disclosures Research Grants: Philips Acist Corp Speaker Honoraria: Janssen Getinge Terumo GE Opsens Boston Scientific
Why expedite discharge • Reduced resource utilization • Patients prefer it • It is safe

Evidence for SDD • MA of 13 studies involving 111, 830 pts • MACE for SDD had OR=1. 2 in RCT and 0. 67 in observational trials. • Low event rate, an adequately powered trial would require >17, 000 pts Abdelaal JACC Interv 2013; 6(2): 99 -112

SDD costs less • Premier Database of 437 Hospitals • 672, 470 patients with elective PCI • Overall 3. 5% SDD, increased to 6. 3% in 2015 • No increase in MACE • Savings of $5128 per procedure mainly from room/board Amin, JAMA Cardiology, 2018; 3: 1041 -9
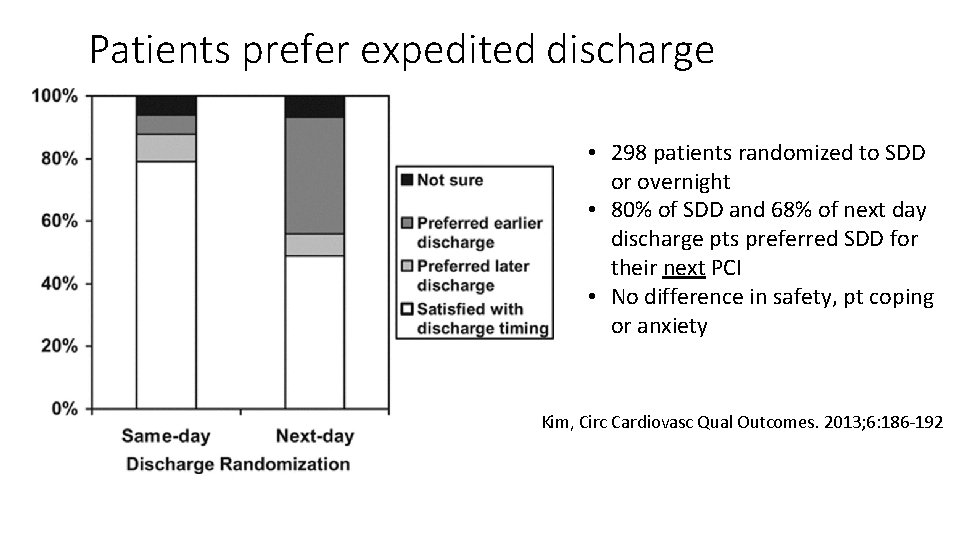
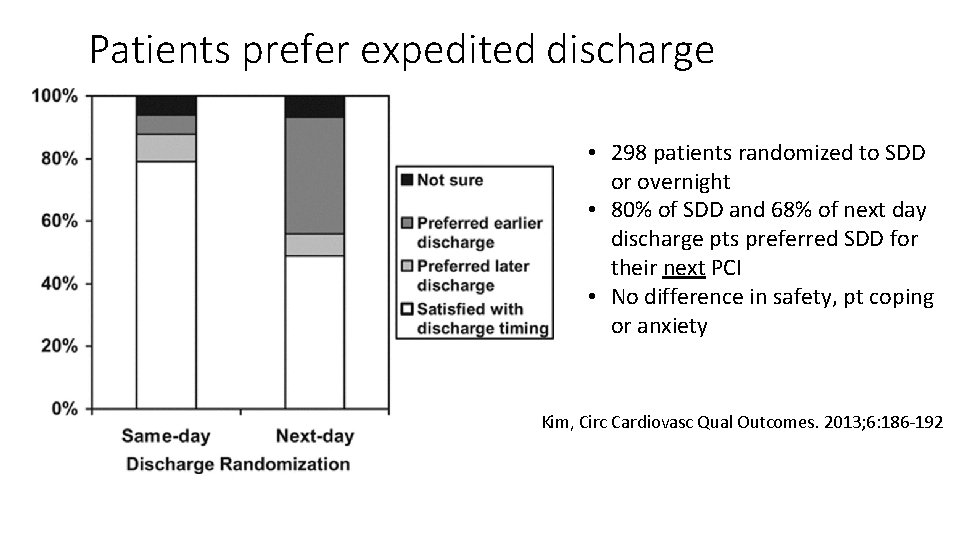
Patients prefer expedited discharge • 298 patients randomized to SDD or overnight • 80% of SDD and 68% of next day discharge pts preferred SDD for their next PCI • No difference in safety, pt coping or anxiety Kim, Circ Cardiovasc Qual Outcomes. 2013; 6: 186 -192
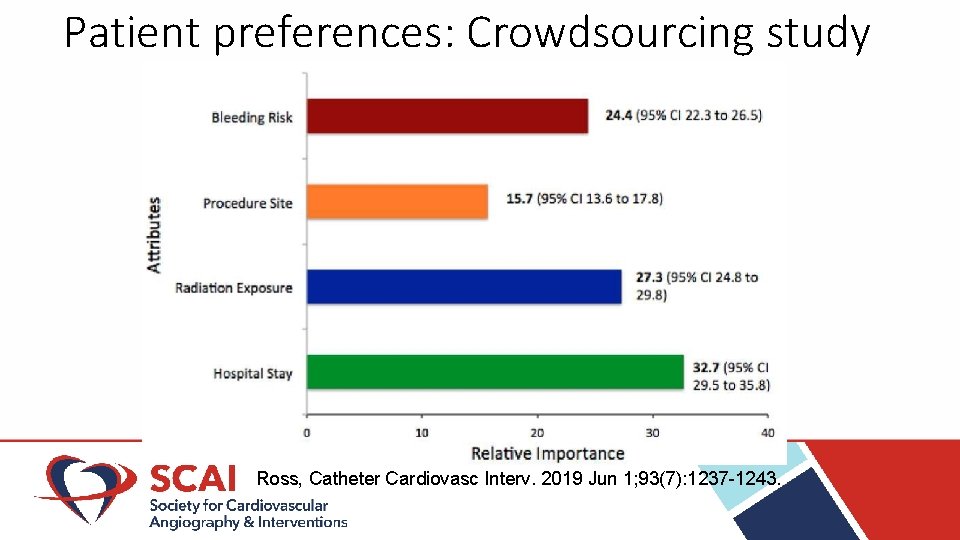
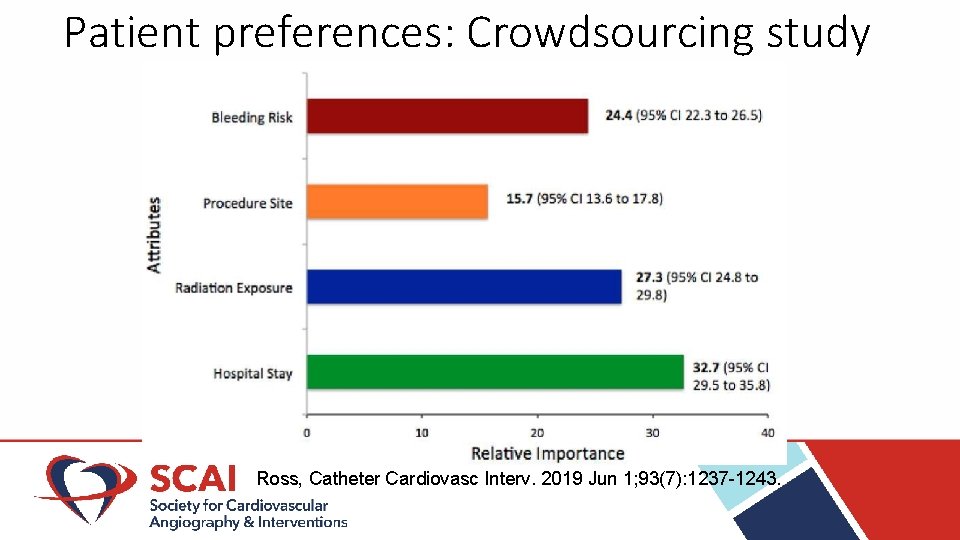
Patient preferences: Crowdsourcing study Ross, Catheter Cardiovasc Interv. 2019 Jun 1; 93(7): 1237 -1243.
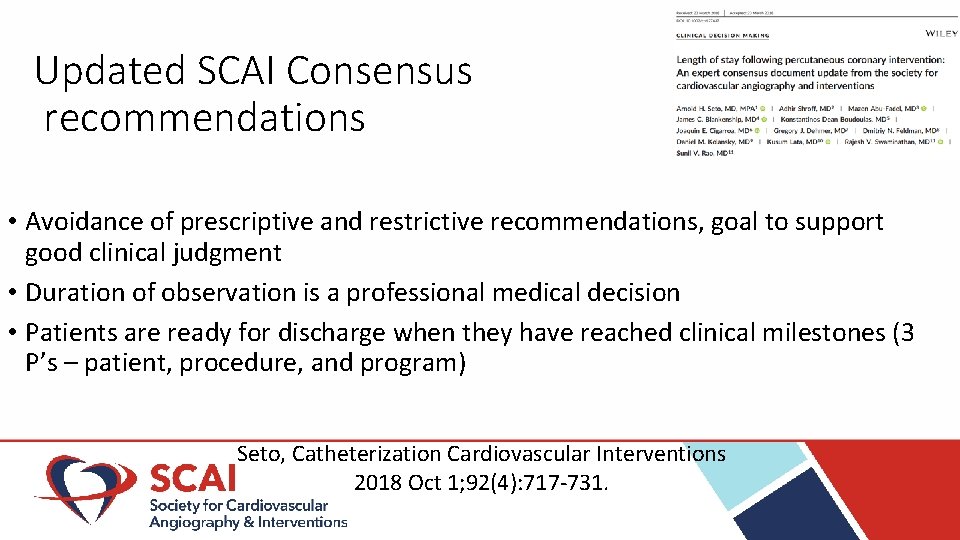
Updated SCAI Consensus recommendations • Avoidance of prescriptive and restrictive recommendations, goal to support good clinical judgment • Duration of observation is a professional medical decision • Patients are ready for discharge when they have reached clinical milestones (3 P’s – patient, procedure, and program) Seto, Catheterization Cardiovascular Interventions 2018 Oct 1; 92(4): 717 -731.

2017 Consensus: Patient Criteria Seto, Catheterization Cardiovascular Interventions 2018 Oct 1; 92(4): 717 -731.
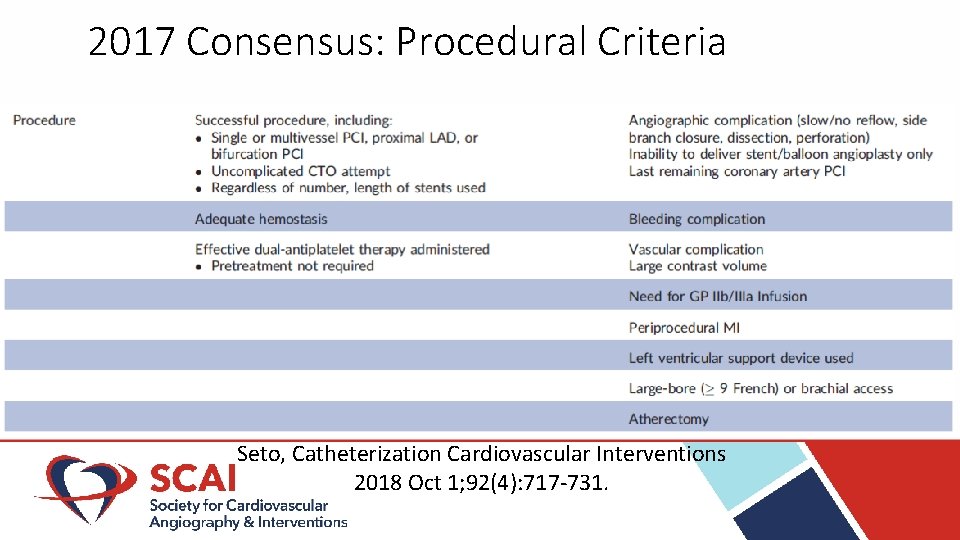
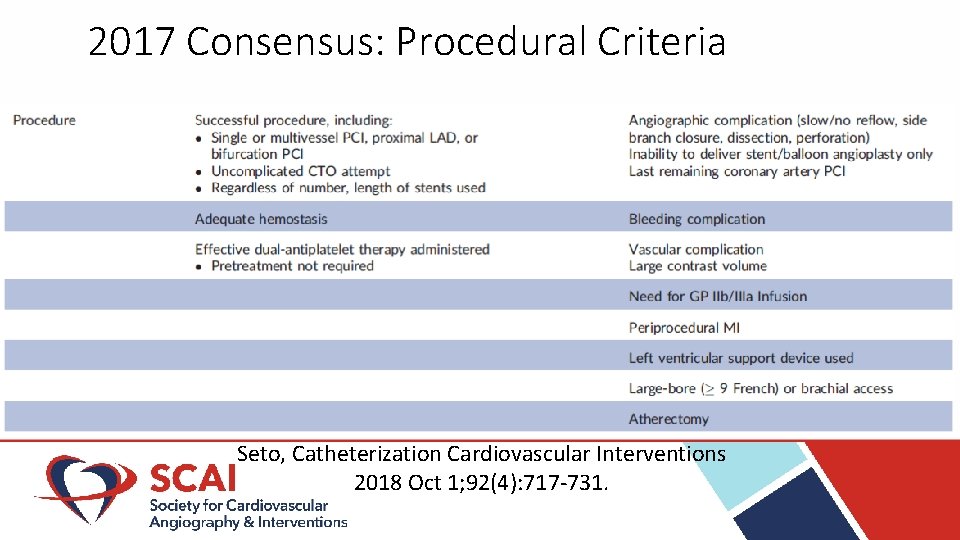
2017 Consensus: Procedural Criteria Seto, Catheterization Cardiovascular Interventions 2018 Oct 1; 92(4): 717 -731.
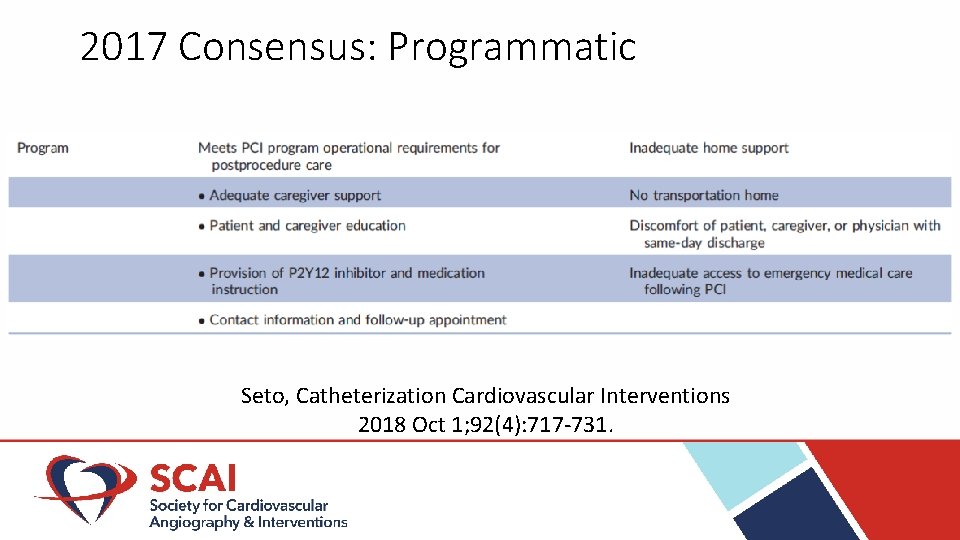
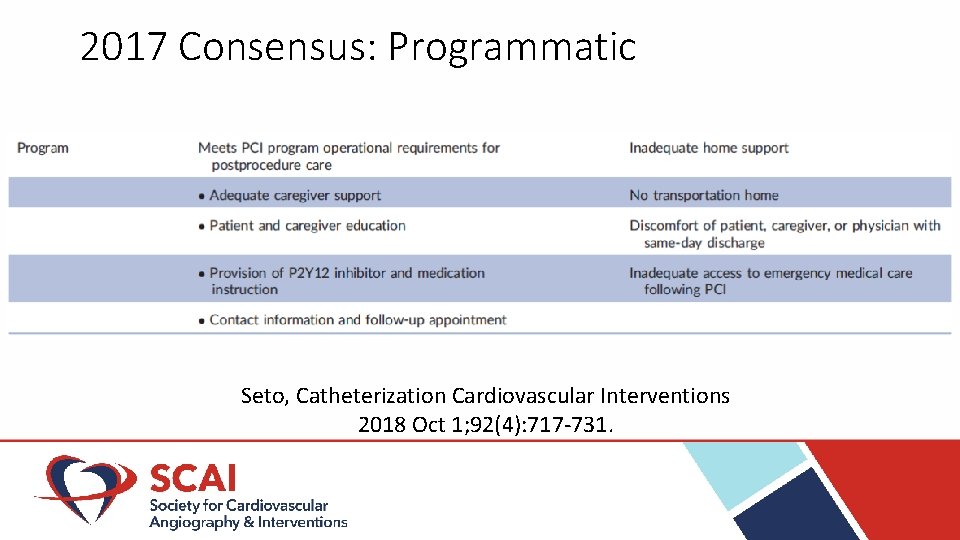
2017 Consensus: Programmatic Seto, Catheterization Cardiovascular Interventions 2018 Oct 1; 92(4): 717 -731.
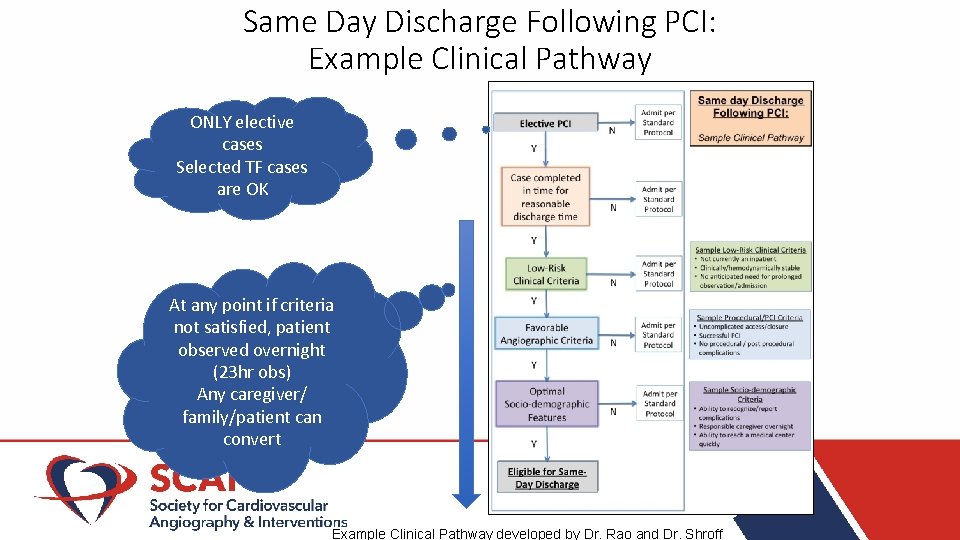
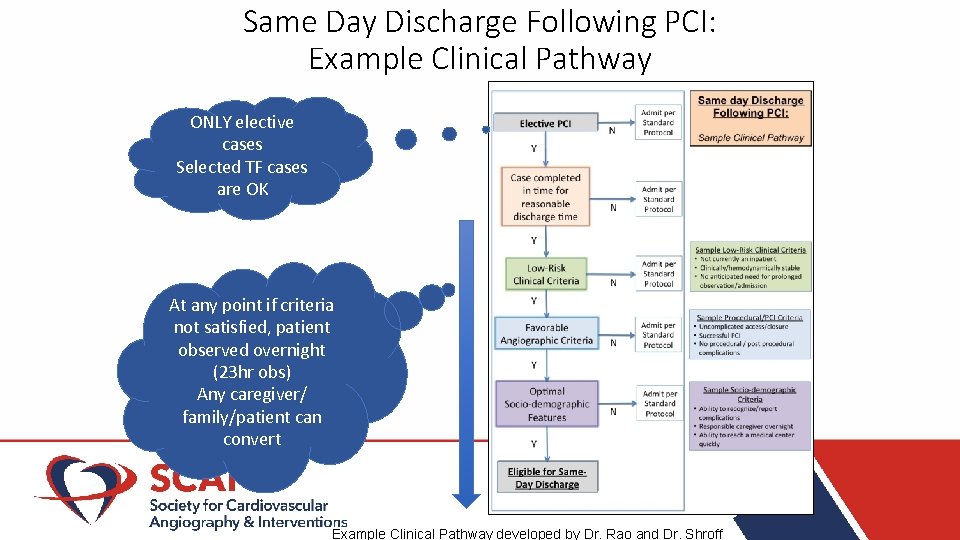
Same Day Discharge Following PCI: Example Clinical Pathway ONLY elective cases Selected TF cases are OK At any point if criteria not satisfied, patient observed overnight (23 hr obs) Any caregiver/ family/patient can convert Example Clinical Pathway developed by Dr. Rao and Dr. Shroff

Same Day Discharge Following PCI: Example Sample Workflow Order set Have discharge criteria Follow-up is essential Example Clinical Pathway developed by Dr. Rao and Dr. Shroff

Current State of the Art SDD process 2 hours 4 -6 hours Procedure • Radial access • 5000 U UFH • P 2 Y 12 load • Disposition (SDD vs ON) Recovery Moderate sedation: 30 min TR Band release: 90 min Hydration: 4 -6 hours Post-procedure check 1 hour Discharge Process: • Discharge Order • Rx • Patient education • Transportation • Appointment • Waiting room

Expediting Discharges beyond SDD • Protocol/Pathway • Order sets, criteria for discharge • Education material, pharmacy/nurse/logistic support • Faster Hemostasis • • ? Shorter compression times ? Lower heparin doses ? Hemostatic patches ? Manual compression • Minimize contrast volume to reduce duration of post-procedural hydration • ? Need for safety data for SDD < 4 -6 hrs
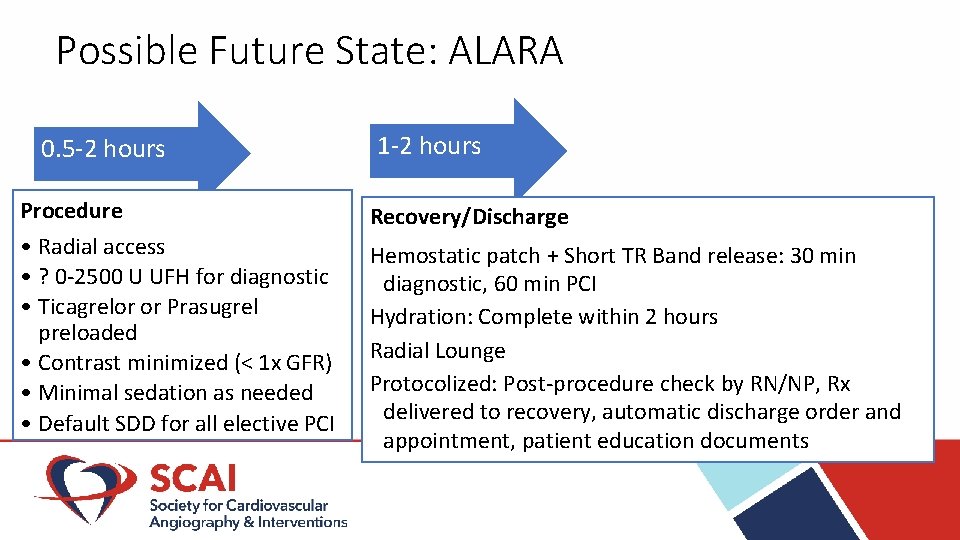
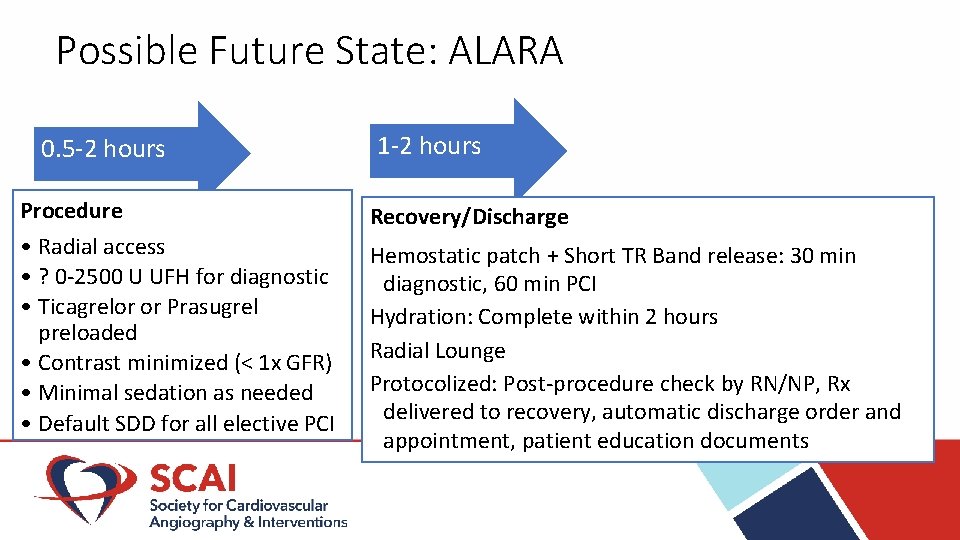
Possible Future State: ALARA 0. 5 -2 hours Procedure • Radial access • ? 0 -2500 U UFH for diagnostic • Ticagrelor or Prasugrel preloaded • Contrast minimized (< 1 x GFR) • Minimal sedation as needed • Default SDD for all elective PCI 1 -2 hours Recovery/Discharge Hemostatic patch + Short TR Band release: 30 min diagnostic, 60 min PCI Hydration: Complete within 2 hours Radial Lounge Protocolized: Post-procedure check by RN/NP, Rx delivered to recovery, automatic discharge order and appointment, patient education documents