ReninAngiotensin System Afferent Macula Densa JG Apparatus Efferent

- Slides: 27
Renin-Angiotensin System
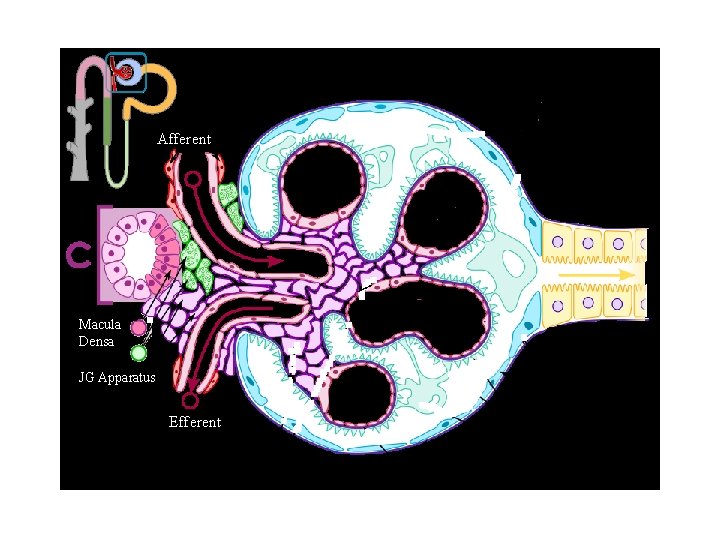
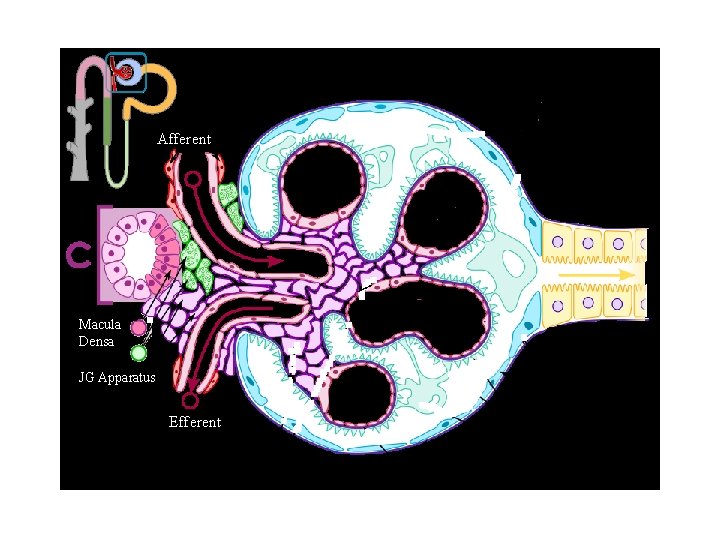
Afferent Macula Densa JG Apparatus Efferent
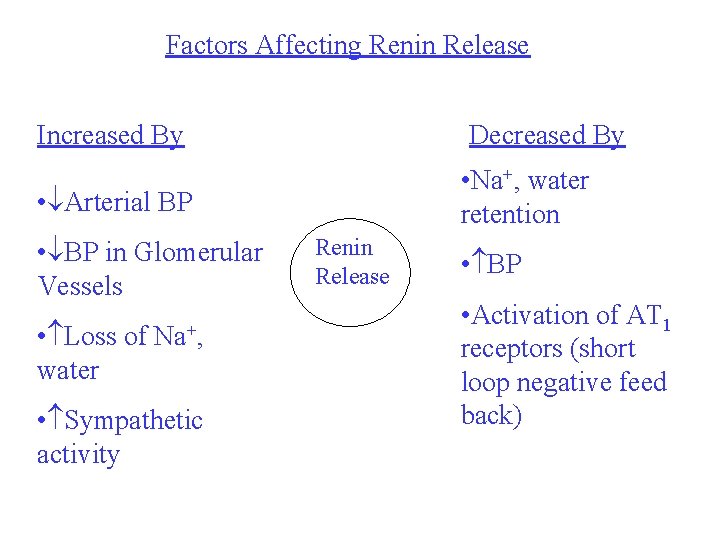
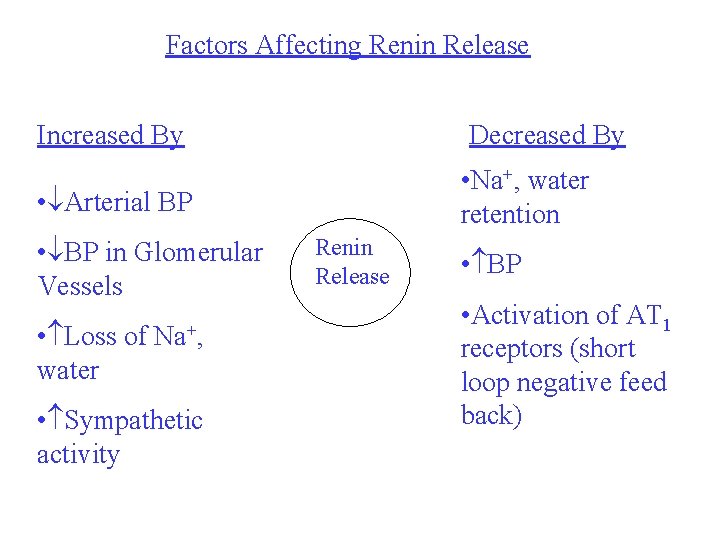
Factors Affecting Renin Release Increased By Decreased By • Na+, water retention • Arterial BP • BP in Glomerular Vessels • Loss of Na+, water • Sympathetic activity Renin Release • BP • Activation of AT 1 receptors (short loop negative feed back)
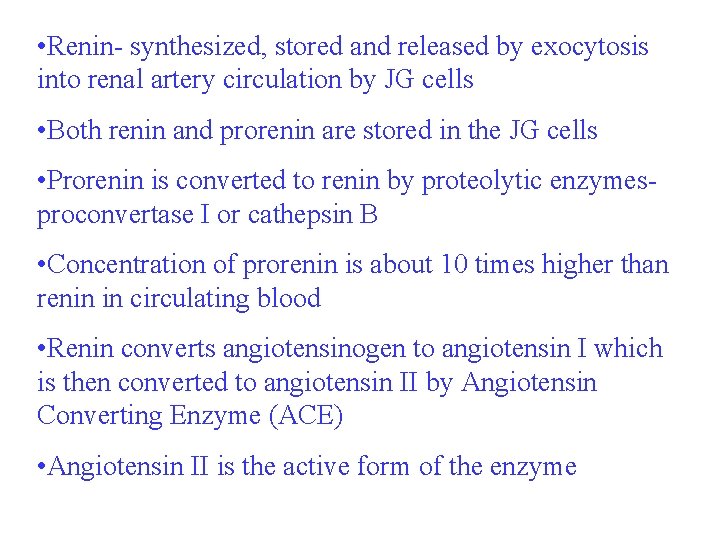
• Renin- synthesized, stored and released by exocytosis into renal artery circulation by JG cells • Both renin and prorenin are stored in the JG cells • Prorenin is converted to renin by proteolytic enzymesproconvertase I or cathepsin B • Concentration of prorenin is about 10 times higher than renin in circulating blood • Renin converts angiotensinogen to angiotensin I which is then converted to angiotensin II by Angiotensin Converting Enzyme (ACE) • Angiotensin II is the active form of the enzyme
Control of Renin Secretion • Macula densa pathway • Intrarenal baroreceptor pathway • -receptor pathway
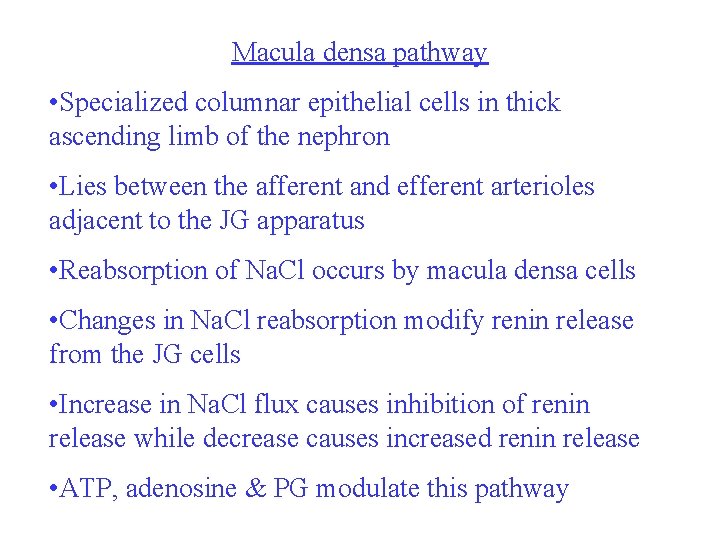
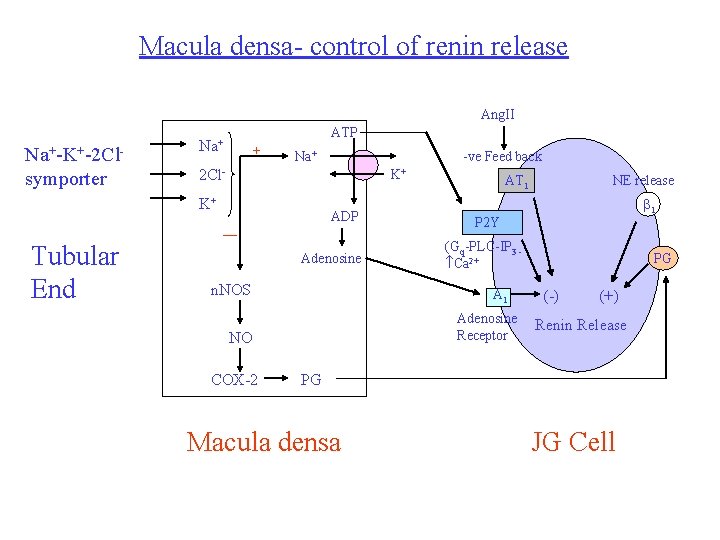
Macula densa pathway • Specialized columnar epithelial cells in thick ascending limb of the nephron • Lies between the afferent and efferent arterioles adjacent to the JG apparatus • Reabsorption of Na. Cl occurs by macula densa cells • Changes in Na. Cl reabsorption modify renin release from the JG cells • Increase in Na. Cl flux causes inhibition of renin release while decrease causes increased renin release • ATP, adenosine & PG modulate this pathway
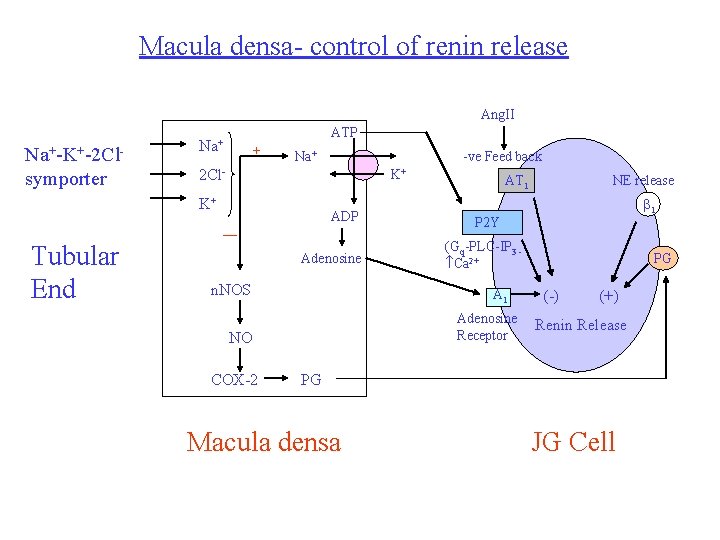
Macula densa- control of renin release Ang. II Na+-K+-2 Clsymporter ATP Na+ + Na+ K+ K+ Tubular End -ve Feed back 2 Cl. ADP — Adenosine n. NOS NE release 1 P 2 Y (Gq-PLC-IP 3 Ca 2+ A 1 Adenosine Receptor NO COX-2 AT 1 PG (-) (+) Renin Release PG Macula densa JG Cell
• In macula densa, regulation is mainly by concentration of Cl- concentration rather than Na+ concentration • Concentration of Na+ in tubular lumen is usually higher than required for saturating the symporter due to which changes in levels of Na+ do not have much effect on macula densa • Cl- concentrations required for saturation of the symporter are high due to which changes in its concentration mainly effect macula densa mediated renin release
• Renin release control: mechanism II- intrarenal baroreceptor pathway • in BP or renal perfusion pressure in preglomerular vessels inhibits renin release and vice versa • May be mediated by stretch receptors in arterial walls or/and by PG synthesis • Mechanism III: via 1 receptors on JG cells
• Increased renin secretion enhances formation of angiotensin II which is responsible for short loop negative feed back • Other factors in negative feed back: üActivating high pressure baroreceptors and thereby reducing renal sympathetic tone- k/a long loop negative feed back üIncreasing pressure in the preglomerular vessels üReducing Na. Cl reabsorption from the proximal tubule (pressure natriuresis) thereby reducing delivery of Na. Cl to macula densa which reduces renin release
Physiological factors modifying renin release: • Systemic blood pressure • Dietary salt intake • Pharmacological agentsüNSAIDs- inhibit PG synthesis renin release üLoop diuretics decrease BP and increase Na. Cl reabsorption causing increased renin release üACE inhibitors, ARBs, renin inhibitors üCentrally acting sympatholytic agents and -blockers decrease renin secretion by reducing -receptor activation
ACE • It is a glycoprotein • It is nonspecific enzyme that catalyzes diverse amino acids • It is identical to Kinase II that inactivates bradykinin and other potent vasodilator peptides • ACE is present in the vascular endothelium which is responsible for rapid conversion of Ang I to Ang II • ACE 2: present in human body- carboxypeptidase • It cleaves one amino acid residue from Ang I to convert it to Ang (1 -9) and Ang II to Ang (1 -7) • Ang (1 -7) binds to Mas receptors and elicits vasodilator and non-proliferative responses
• ACE 2 has 400 fold greater affinity for Ang. II than Ang. I • ACE 2 is not inhibited by standard ACE inhibitors used • It has no effect on bradykinin • Physiological significance uncertain • May act a a counter-regulatory mechanism to oppose effects of ACE • It regulates effects of Ang II by converting it to Ang (2 -8) also called Ang III • Ang IV (3 -8) is formed from Ang III • Ang I has is less than 1% potent than Ang II
• Angiotensinogen is formed in the liver • Major site for conversion of Ang I to Ang II is the lung • Reason: because it has a large number of capillaries and ACE is present in the endothelial cells of the capillaries • Other sites: other blood vessels specially of kidney • Angiotensinages are diverse group of enzymes like aminopeptidases, endopeptidases, carboxypeptidases and other peptidases that degrade and inactivate angiotensin • They are non-specific enzymes
Local (Tissue) Renin-Angiotensin System • Important for its role in hypertrophy, inflammation, remodelling and apoptosis • Binding of renin or pro-renin to pro-renin receptors located on cell surface • Present in many tissues like brain, pituitary blood vessels, heart, kidney, adrenal glands • Extrinsic local RAS: in vascular endothelium of these tissues • Intrinsic local RAS: tissues having m. RNA expression
• Number of enzymes that act as alternative pathway for conversion of angiotensinogen to Ang. I or directly to Ang. II • Enzymes are: cathepsin, tonin, cathepsin G, chymostatin sensitive. Ang. II generating enzyme and heart chymase • Angiotensin receptors: two typesüAT 1 and AT 2 üMost effects of Ang. II are mediated by AT 1 receptors üRole of AT 22 receptors not well defined üMay counterbalance many effects of AT 1 activation
Functions of RAS • Effects of Ang. II on CVS include: üRapid pressor respone- peripheral resistance üSlow pressor response- via decrease in renal excretion and production of endothelin-1 üVascular and cardiac hypertrophy and remodeling
Rapid pressor response: • AT 1 receptors are located in the vascular smooth muscle cells • Ang II activates these receptors and constricts the precapillary arterioles and to a lesser extent the postcapillary venules • It stimulates the Gq-PLC-IP 3 -Ca 2+ pathway • Vasoconstriction is maximum in kidneys, lesser in splanchnic. • Weak vasoconstrictor action in brain, lung and skeletal muscles
Other contributing factors are: • Enhancement of peripheral NE neurotransmission by: üInhibiting reuptake of NE into nerve terminals üEnhancing vascular response to NE üHigh concentrations of Ang II stimulate ganglion cells directly • CNS Effects: üIncrease in central sympathetic outflow üAttenuation of baroreceptor mediated reductions in sympathetic discharge from brain
• Brain contains all components of RAS • Brain is affected by both circulating Ang. II and Ang. II formed within the brain • Action of Ang. II on brain causes: üIncreased central sympathetic tone üDipsogenic effect (thirst) • Release of catecholamines from adrenal medulla: Ang. II depolarises the chromaffin cells of adrenal medulla and causes release of adrenaline
Slow Pressor Response: • Produced by effect on the kidneys • Ang. II: üReduces urinary excretion of Na+ and water üIncreases excretion of K+ üStimulates Na+/H+ exchange in proximal tubule due to which Na+, Cl- and bicarbonate reabsorption increases üIncreases expression of Na+-glucose symporter in proximal tubule üDirectly stimulates Na+-K+-2 Cl- symporter in thick ascending limb
• Proximal tubule secretes angiotensinogen and the connecting tubule secretes renin • Paracrine tubular RAS? Functions? • Ang. II stimulates zona glomerulosa of adrenal cortex to increase the synthesis and secretion of aldosterone • Also auguments its response to other stimuli like ACTH, K+ • Aldosterone acts on distal and collecting tubules to cause retention of Na+ and excretion of K+ and H+ • Stimulatory effect of Ang. II on aldosterone secretion depends on plasma concentrations of Na+ and K+
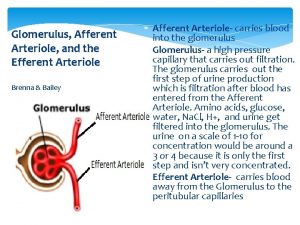
• Release of aldosterone is enhanced in cases of hyponatremia or hyperkalemia and vice versa • Effect on glomerular filtrate: üConstriction of afferent arterioles reduces intraglomerular pressor and tends to reduce GFR üContraction of mesangial cells decreases the capillary surface area within the glomerulous and tends to decrease GFR üConstriction of efferent arterioles increases the intraglomerular pressor and tends to increase GFR üNormally, GFR is slightly reduced by Ang. II
• Vascular and cardiac hypertrophy and remodeling: üCells involved- vascular smooth muscle cells, cardiac myocytes and fibroblasts üStimulates migration, proliferation and hypertrophy of vascular smooth muscle cells üIncreases extracellular matrix production by vascular smooth muscle cells üCauses hypertrophy of cardiac myocytes üIncreases extracellular matrix production by cardiac fibroblasts
Effect on heart: • Increases cardiac contractility directly by opening of voltage gated Ca 2+ channels in cardiac myocyte • Increases cardiac rate indirectly by increasing central sympathetic tone • Increases adrenal release of catecholamines • Facilitates adrenergic neurotransmission • Rapid rise in BP causes baroreceptor stimulationdecrease in central sympathetic tone and increased vagal tone • Net effect-uncertain

Inhibitors of RAS • ACE inhibitors (ACEIs) • Angiotensin receptor blockers (ARBs) • Direct renin inhibitors (DRIs)
 Juxtaglomerular apparatus and macula densa
Juxtaglomerular apparatus and macula densa Convoluted tubule
Convoluted tubule Mesangial
Mesangial Pelve renal
Pelve renal Function of macula densa
Function of macula densa Macula densa
Macula densa Macula densa
Macula densa Tütün növləri
Tütün növləri Mioepiteliales
Mioepiteliales Anatomie microscopique du rein
Anatomie microscopique du rein Nephron
Nephron Intralobular artery
Intralobular artery Sodium reabsorption
Sodium reabsorption Nephron osmolarity diagram
Nephron osmolarity diagram Macula densa adenosina
Macula densa adenosina Akomodasyon refleksi sinirleri
Akomodasyon refleksi sinirleri Visceral afferent vs efferent
Visceral afferent vs efferent Cremasteric reflex
Cremasteric reflex Cremasteric reflex afferent and efferent
Cremasteric reflex afferent and efferent Oncotic pressure vs hydrostatic
Oncotic pressure vs hydrostatic Système parasympathique et sympathique
Système parasympathique et sympathique Gl lacrimalis innervasyonu
Gl lacrimalis innervasyonu The urinary system consists of
The urinary system consists of Efferent arteriole
Efferent arteriole Renal column
Renal column In neurons, efferent is to ______ as afferent is to ______.
In neurons, efferent is to ______ as afferent is to ______. Efferent division of nervous system
Efferent division of nervous system Densa
Densa