PTSD An Update on the Evidence Kathleen M

- Slides: 28
PTSD : An Update on the Evidence Kathleen M. Chard, PHD Associate Chief of Staff/Research Director, Trauma Recovery center Cincinnati VA Medical Center Professor, Psychiatry and Behavioral Neuroscience Director, UC Health Stress Center University of Cincinnati
People can get PTSD from: Combat Violent personal assault: rape, mugging, physical assault Kidnapping POW and Concentration Camp survivors Terrorist Attacks Airplane Crashes Severe Auto Accidents Torture Natural Disaster Fires Hostage situations etc.
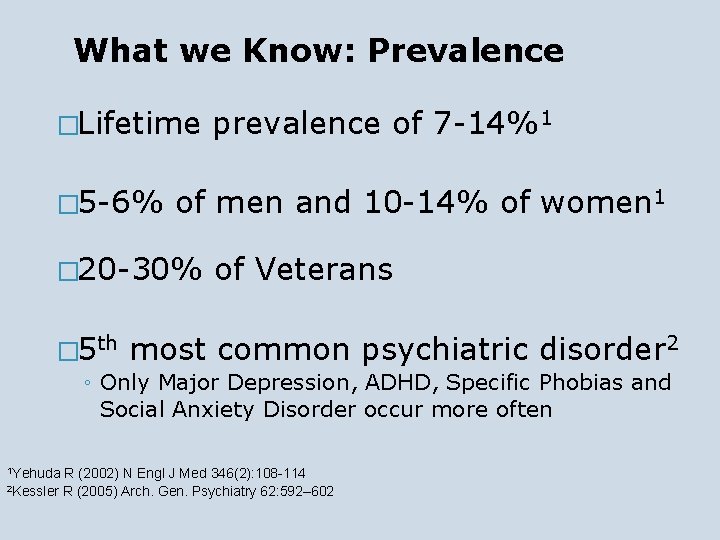
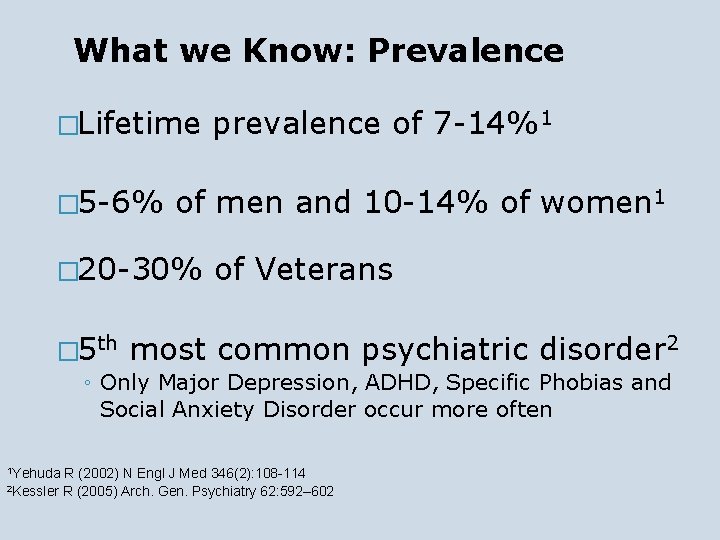
What we Know: Prevalence �Lifetime � 5 -6% of men and 10 -14% of women 1 � 20 -30% � 5 th prevalence of 7 -14%1 of Veterans most common psychiatric disorder 2 ◦ Only Major Depression, ADHD, Specific Phobias and Social Anxiety Disorder occur more often 1 Yehuda R (2002) N Engl J Med 346(2): 108 -114 2 Kessler R (2005) Arch. Gen. Psychiatry 62: 592– 602
Who Develops PTSD? Genes Temperament Family environment Trauma characteristics - age, chronicity, predictability, trust in perpetrator Post-trauma perceived social support PTSD is interrupted recovery
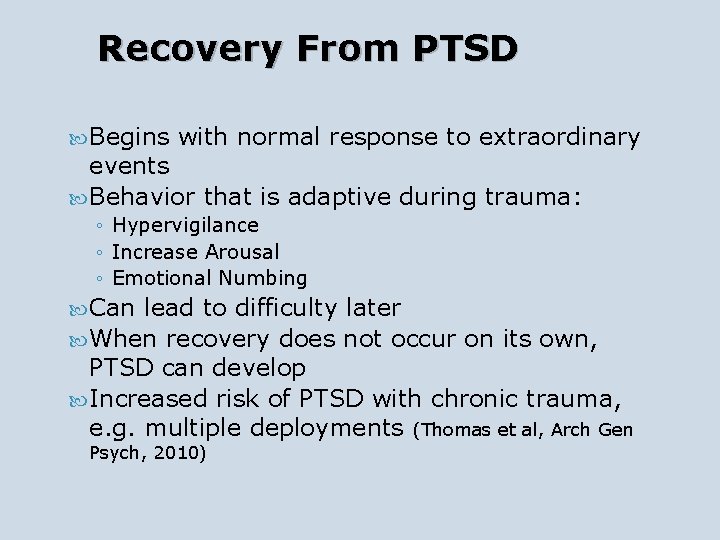
Recovery From PTSD Begins with normal response to extraordinary events Behavior that is adaptive during trauma: ◦ Hypervigilance ◦ Increase Arousal ◦ Emotional Numbing Can lead to difficulty later When recovery does not occur on its own, PTSD can develop Increased risk of PTSD with chronic trauma, e. g. multiple deployments (Thomas et al, Arch Gen Psych, 2010)
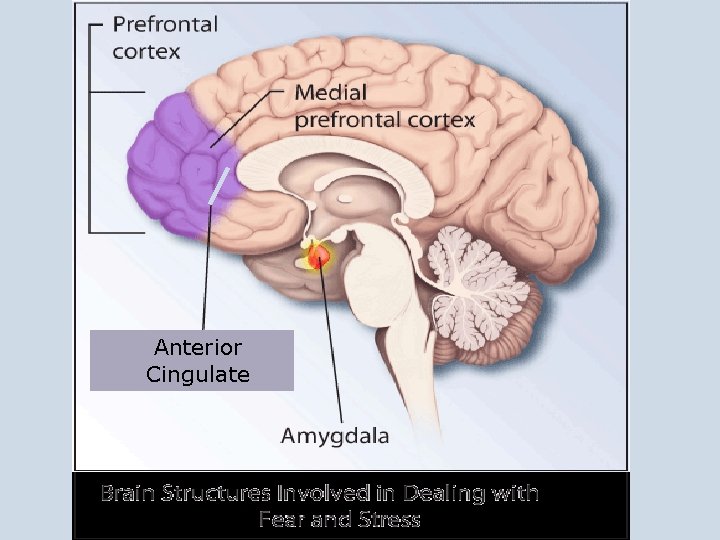
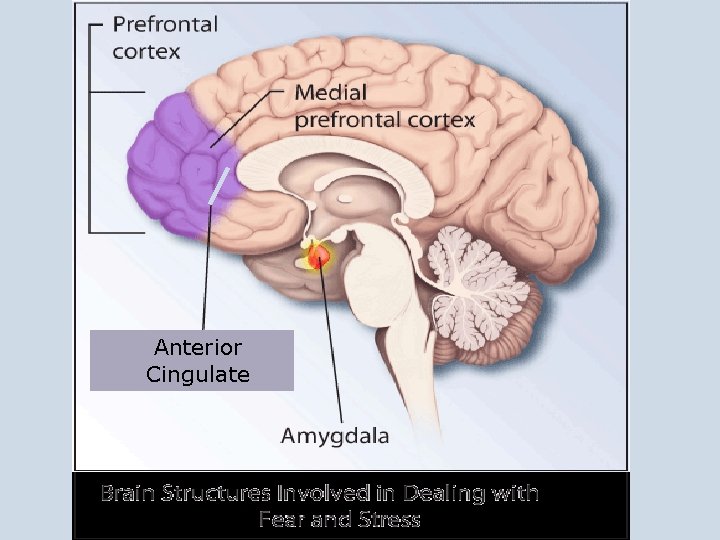
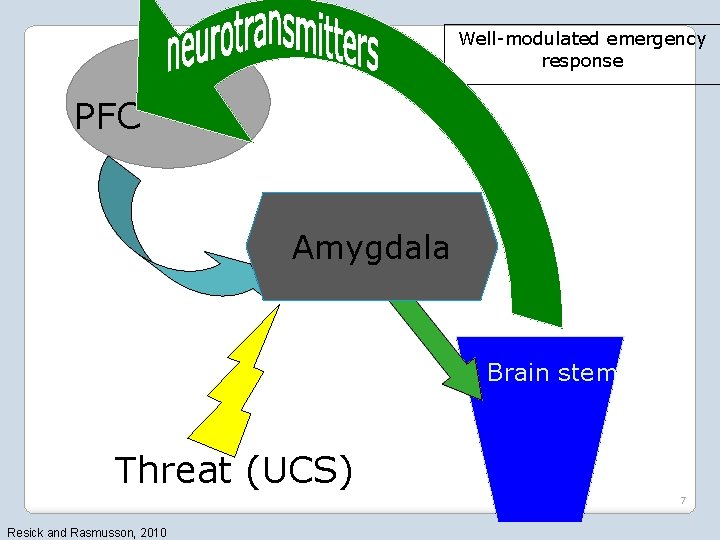
Anterior Cingulate
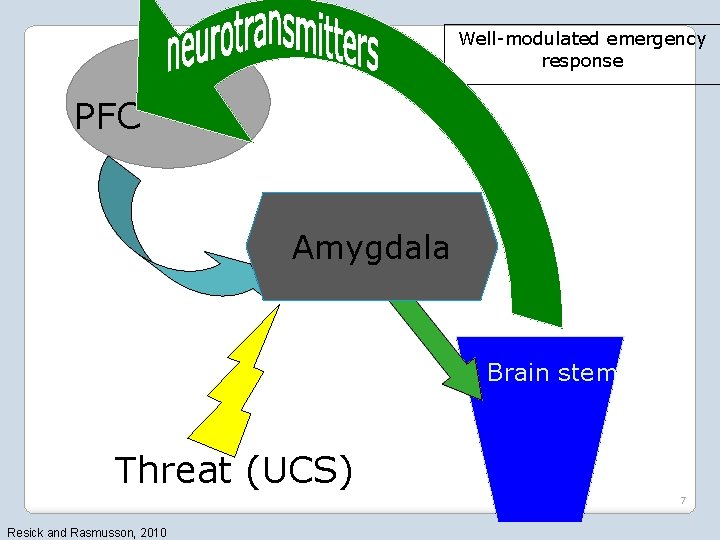
Well-modulated emergency response PFC Amygdala Brain stem Threat (UCS) 7 Resick and Rasmusson, 2010
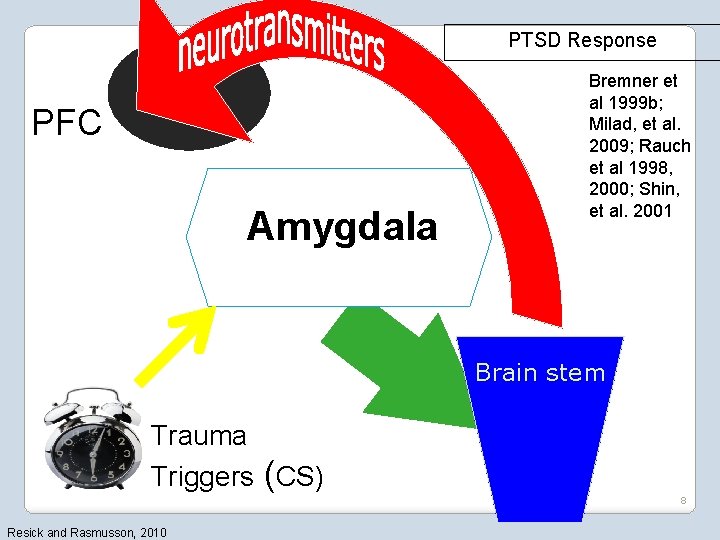
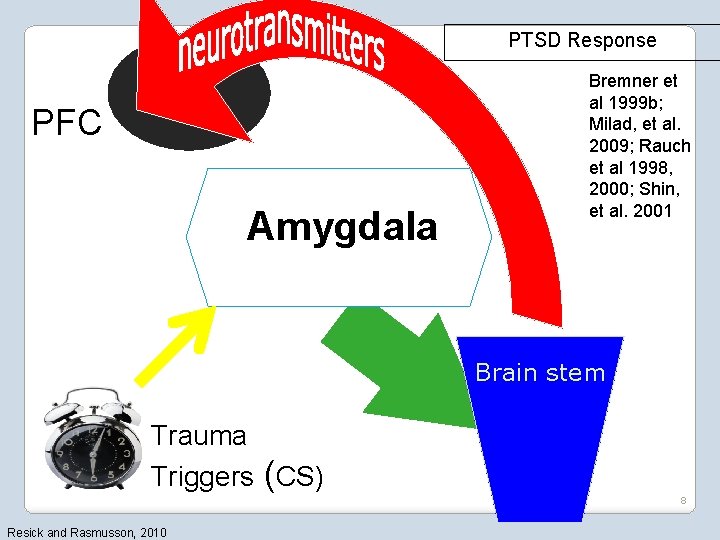
PTSD Response PFC Amygdala Bremner et al 1999 b; Milad, et al. 2009; Rauch et al 1998, 2000; Shin, et al. 2001 Brain stem Trauma Triggers (CS) 8 Resick and Rasmusson, 2010
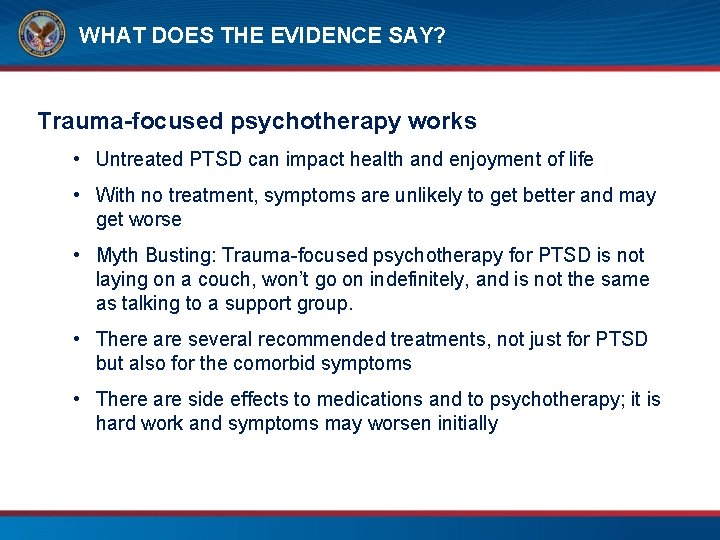
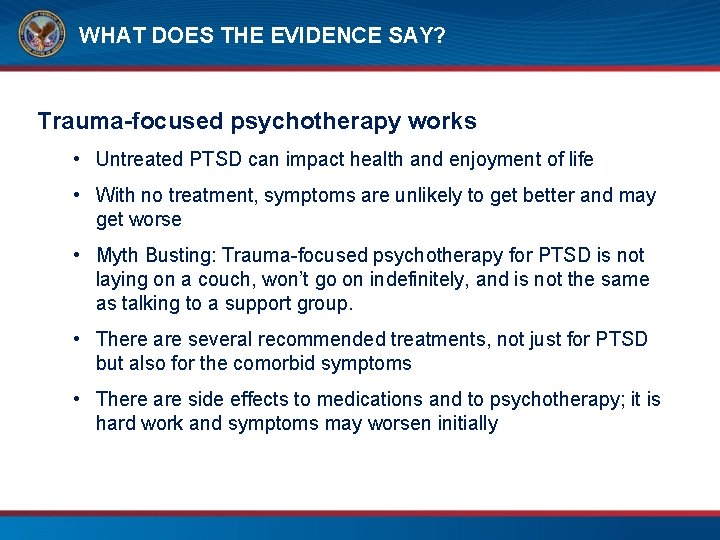
WHAT DOES THE EVIDENCE SAY? Trauma-focused psychotherapy works • Untreated PTSD can impact health and enjoyment of life • With no treatment, symptoms are unlikely to get better and may get worse • Myth Busting: Trauma-focused psychotherapy for PTSD is not laying on a couch, won’t go on indefinitely, and is not the same as talking to a support group. • There are several recommended treatments, not just for PTSD but also for the comorbid symptoms • There are side effects to medications and to psychotherapy; it is hard work and symptoms may worsen initially
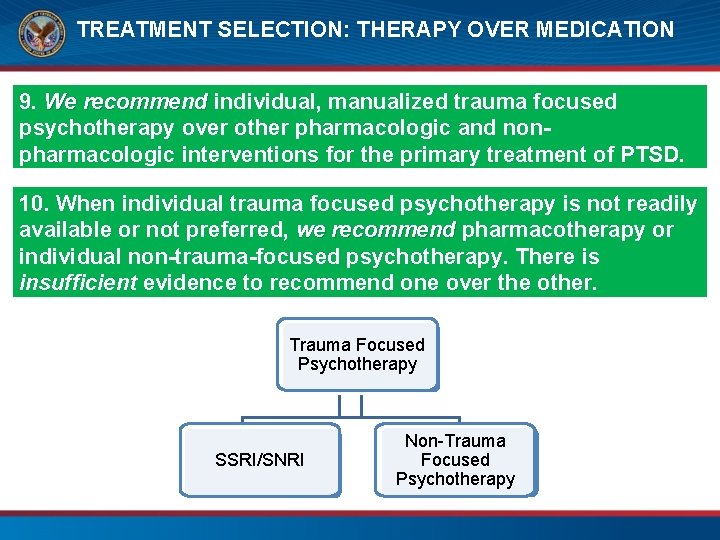
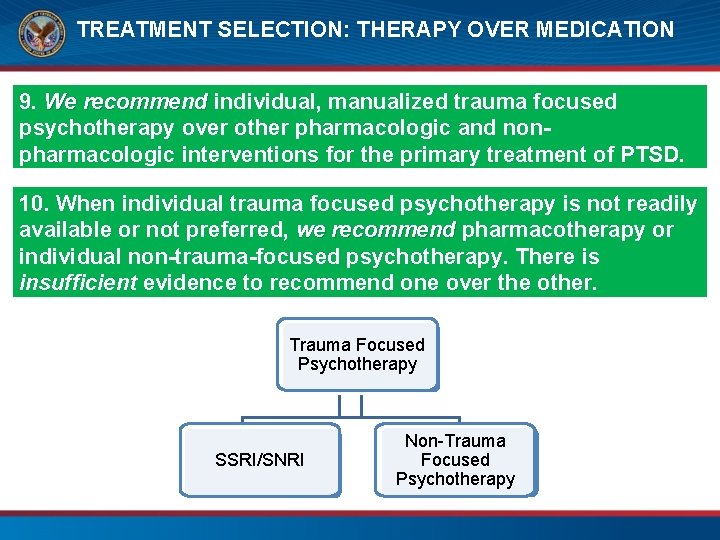
TREATMENT SELECTION: THERAPY OVER MEDICATION 9. We recommend individual, manualized trauma focused psychotherapy over other pharmacologic and nonpharmacologic interventions for the primary treatment of PTSD. 10. When individual trauma focused psychotherapy is not readily available or not preferred, we recommend pharmacotherapy or individual non-trauma-focused psychotherapy. There is insufficient evidence to recommend one over the other. Trauma Focused Psychotherapy SSRI/SNRI Non-Trauma Focused Psychotherapy
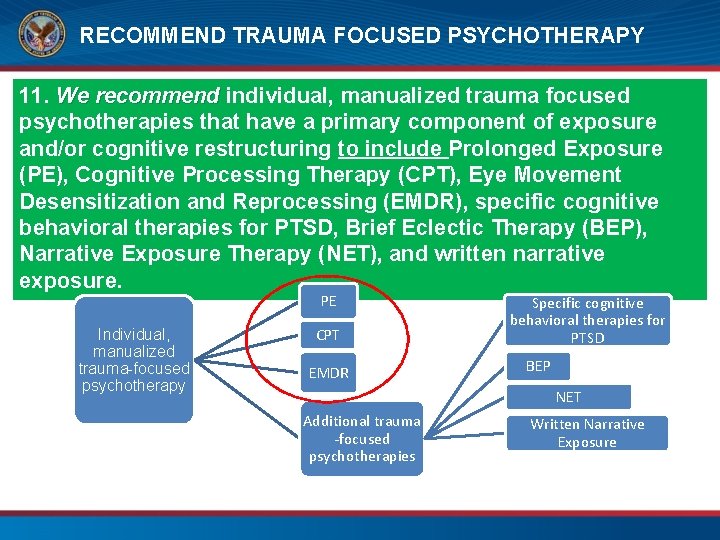
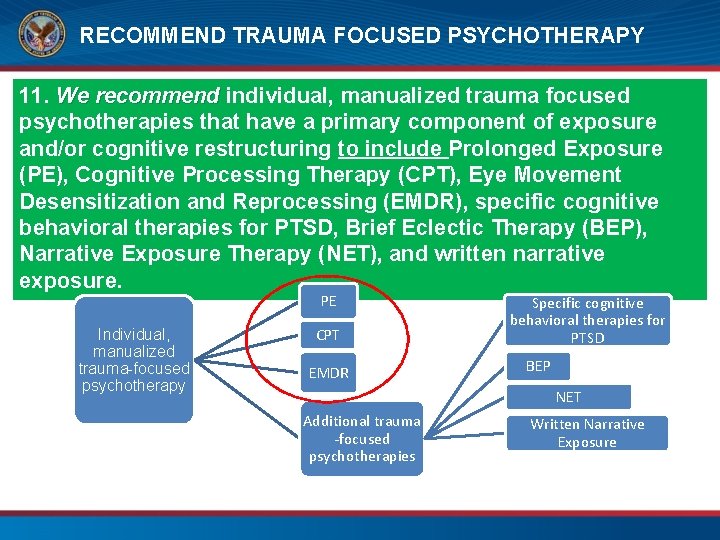
RECOMMEND TRAUMA FOCUSED PSYCHOTHERAPY 11. We recommend individual, manualized trauma focused psychotherapies that have a primary component of exposure and/or cognitive restructuring to include Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), Eye Movement Desensitization and Reprocessing (EMDR), specific cognitive behavioral therapies for PTSD, Brief Eclectic Therapy (BEP), Narrative Exposure Therapy (NET), and written narrative exposure. PE Individual, manualized trauma-focused psychotherapy CPT EMDR Specific cognitive behavioral therapies for PTSD BEP NET Additional trauma -focused psychotherapies Written Narrative Exposure
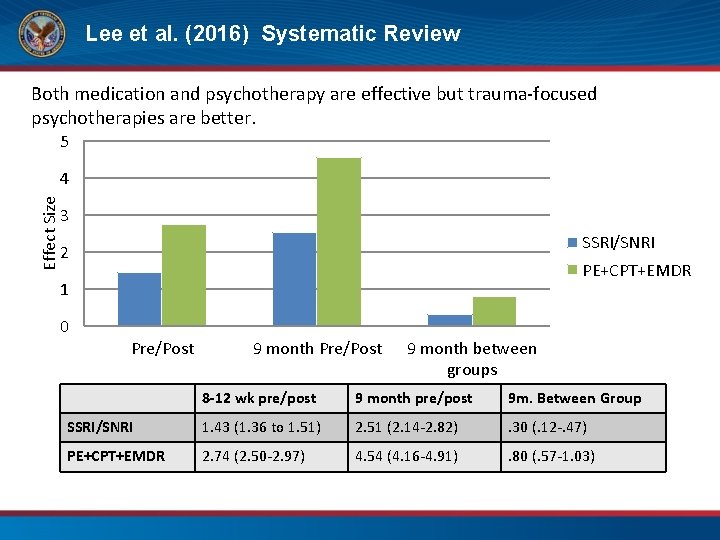
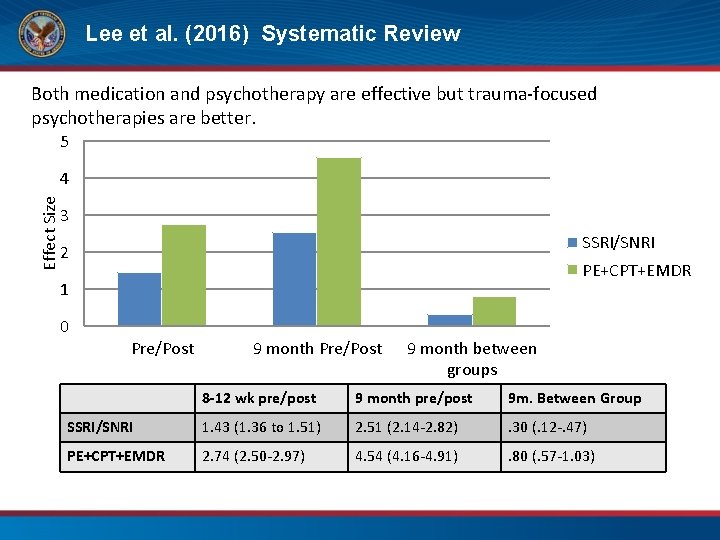
Lee et al. (2016) Systematic Review Both medication and psychotherapy are effective but trauma-focused psychotherapies are better. 5 Effect Size 4 3 SSRI/SNRI 2 PE+CPT+EMDR 1 0 Pre/Post 9 month between groups 8 -12 wk pre/post 9 month pre/post 9 m. Between Group SSRI/SNRI 1. 43 (1. 36 to 1. 51) 2. 51 (2. 14 -2. 82) . 30 (. 12 -. 47) PE+CPT+EMDR 2. 74 (2. 50 -2. 97) 4. 54 (4. 16 -4. 91) . 80 (. 57 -1. 03)
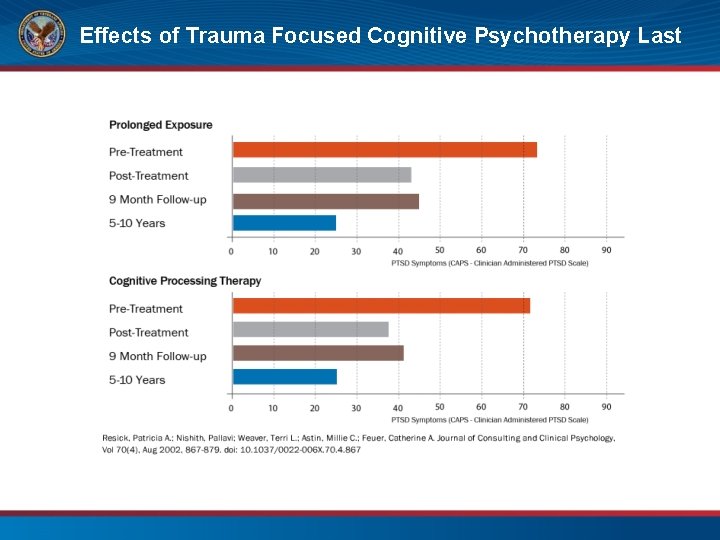
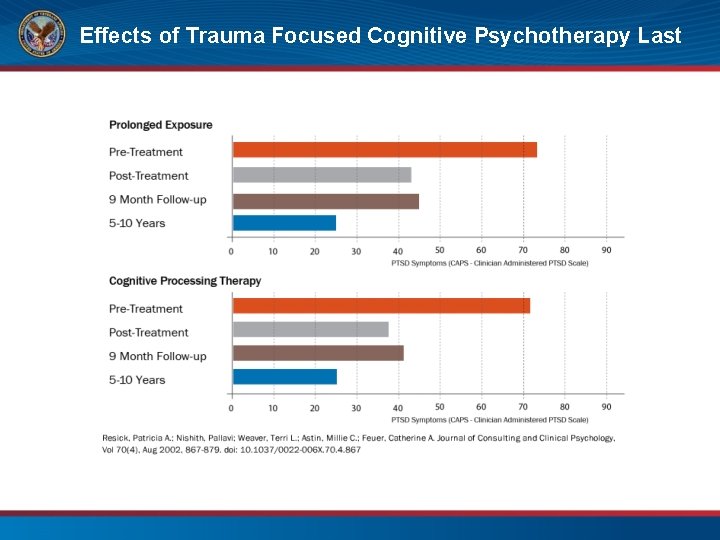
Effects of Trauma Focused Cognitive Psychotherapy Last
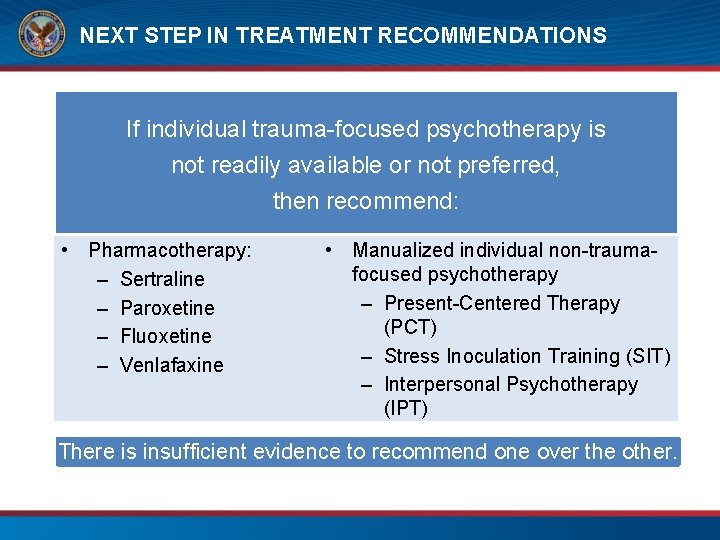
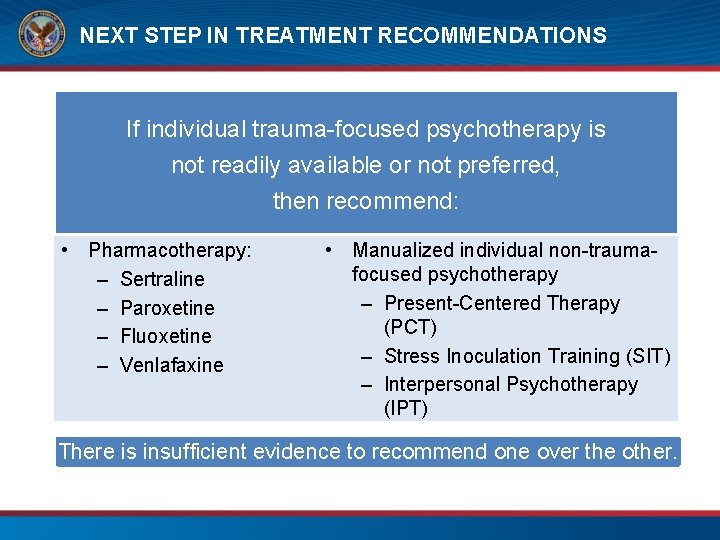
NEXT STEP IN TREATMENT RECOMMENDATIONS If individual trauma-focused psychotherapy is not readily available or not preferred, then recommend: • Pharmacotherapy: – Sertraline – Paroxetine – Fluoxetine – Venlafaxine • Manualized individual non-traumafocused psychotherapy – Present-Centered Therapy (PCT) – Stress Inoculation Training (SIT) – Interpersonal Psychotherapy (IPT) There is insufficient evidence to recommend one over the other.
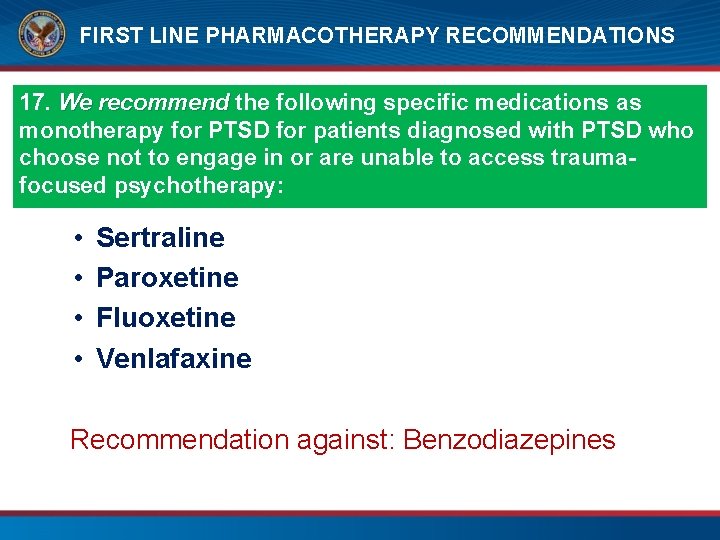
FIRST LINE PHARMACOTHERAPY RECOMMENDATIONS 17. We recommend the following specific medications as monotherapy for PTSD for patients diagnosed with PTSD who choose not to engage in or are unable to access traumafocused psychotherapy: • • Sertraline Paroxetine Fluoxetine Venlafaxine Recommendation against: Benzodiazepines
WHAT DOES THIS ALL MEAN? • For a majority of people treatment will help • There a number of treatment options and it is not a one size fits all model • Some people will need to try several different treatments to obtain the recovery level they desire
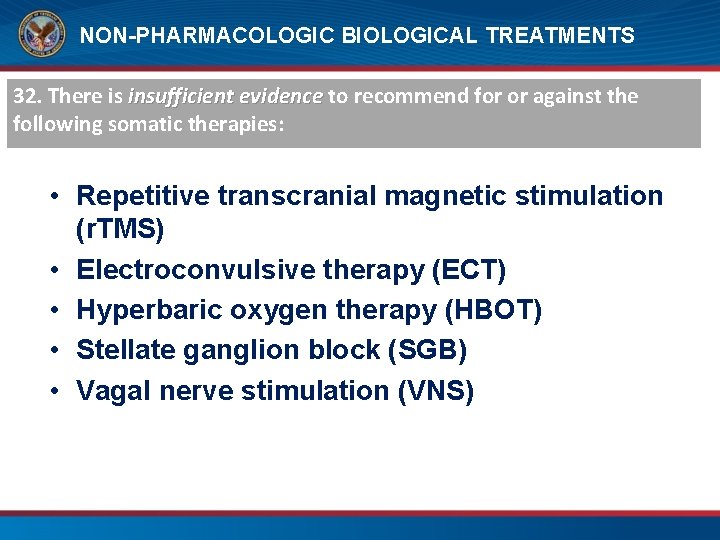
NON-PHARMACOLOGIC BIOLOGICAL TREATMENTS 32. There is insufficient evidence to recommend for or against the following somatic therapies: • Repetitive transcranial magnetic stimulation (r. TMS) • Electroconvulsive therapy (ECT) • Hyperbaric oxygen therapy (HBOT) • Stellate ganglion block (SGB) • Vagal nerve stimulation (VNS)
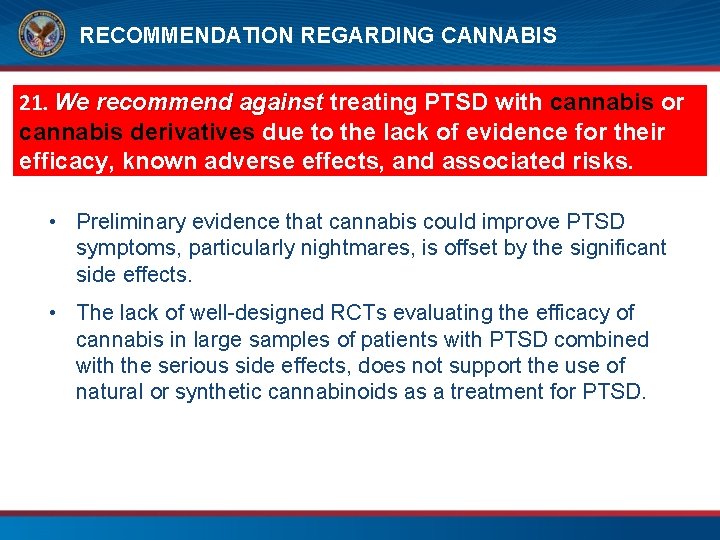
RECOMMENDATION REGARDING CANNABIS 21. We recommend against treating PTSD with cannabis or cannabis derivatives due to the lack of evidence for their efficacy, known adverse effects, and associated risks. • Preliminary evidence that cannabis could improve PTSD symptoms, particularly nightmares, is offset by the significant side effects. • The lack of well-designed RCTs evaluating the efficacy of cannabis in large samples of patients with PTSD combined with the serious side effects, does not support the use of natural or synthetic cannabinoids as a treatment for PTSD.
WHAT ABOUT COMORBIDITIES, TECHNOLOGY, AND COMPLIMENTARY AND INTEGRATIVE HEALTH?
COMPLIMENTARY AND INTEGRATIVE HEALTH RECOMMENDATIONS 32. There is insufficient evidence to recommend any complementary and integrative health (CIH) practice, such as meditation (including mindfulness), yoga, acupuncture, and mantram meditation, as a primary treatment for PTSD. • Important to clarify that we are not recommending against these treatments but are saying that at this time, the research does not support the use of any CIH practice for the primary treatment of PTSD. Recognize their value to improve wellness and promote recovery. • No studies evaluating the use of animal-assisted therapy met the threshold for inclusion.
What Does Treatment Look Like? 7 -15 sessions Sessions can be weekly or “massed” Individual, Group or Combined Focus on traumatic retelling can vary from none to prolonged • Adherence is Key • Homework is important • •
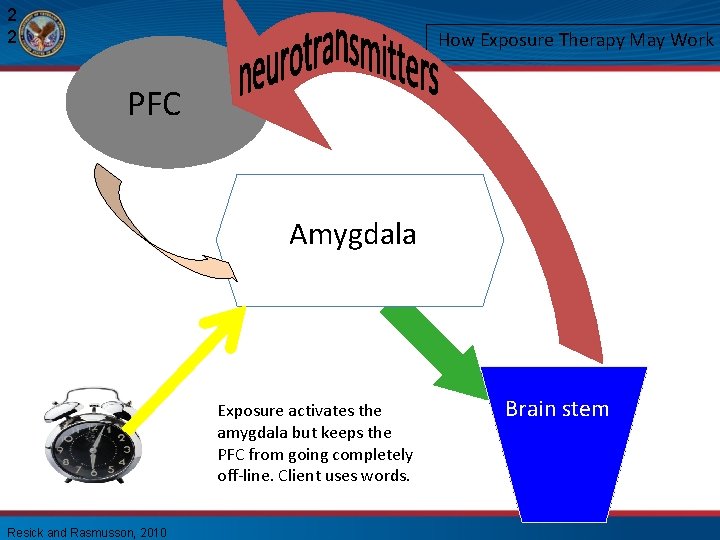
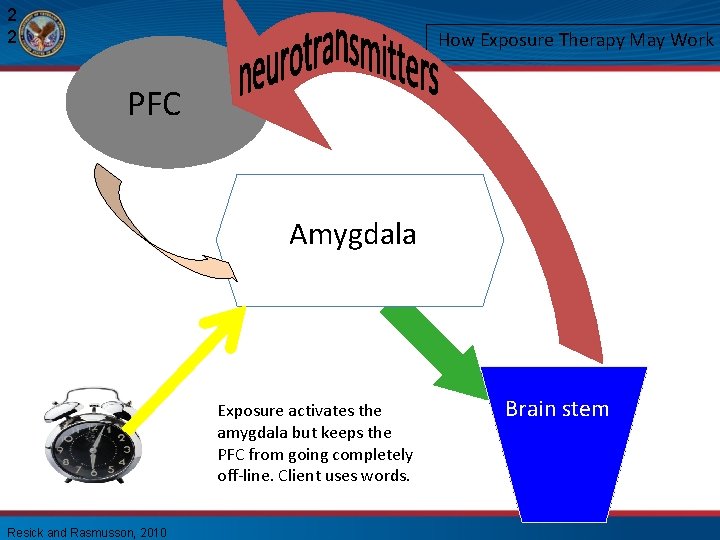
2 2 How Exposure Therapy May Work PFC Amygdala Exposure activates the amygdala but keeps the PFC from going completely off-line. Client uses words. Resick and Rasmusson, 2010 Brain stem
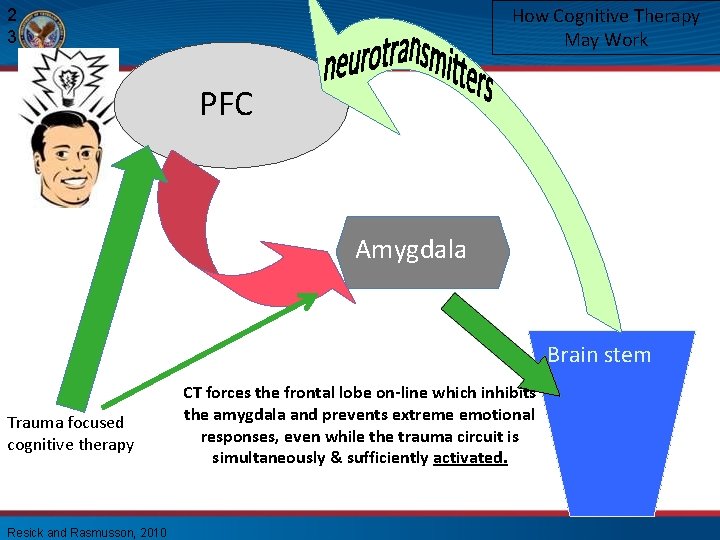
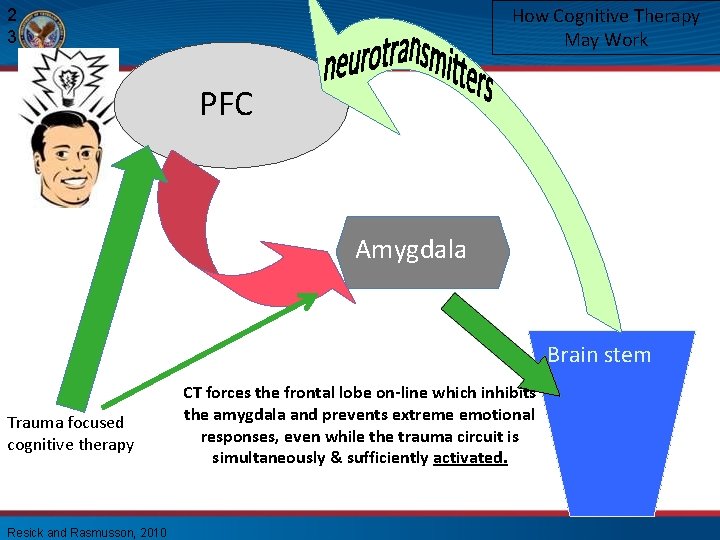
How Cognitive Therapy May Work 2 3 PFC BL Amygdala CE Brain stem Trauma focused cognitive therapy Resick and Rasmusson, 2010 CT forces the frontal lobe on-line which inhibits the amygdala and prevents extreme emotional responses, even while the trauma circuit is simultaneously & sufficiently activated.
Where Are We Going? • • Improved assessment – biological Change in Delivery – Massed Couples Based Treatments Medication facilitated therapy – CBD, MDMA Prevention- medication in ED 2 nd Wave interventions
RESOURCES
A new online tool to help patients learn about and compare evidence-based PTSD treatments www. ptsd. va. gov/decisionaid

MOBILE APPS • NCPTSD has partnered with a number of organizations to develop a variety of mobile apps. • Apps are focused on PTSD, related health problems (e. g. , insomnia, alcohol use, etc. ), or general well-being. • There apps for patients, providers, and for use with patient-provider dyads. www. ptsd. va. gov/public/materials/apps/index. asp
Cincinnati VA Medical Center Trauma Recovery Center 859 -572 -6208 Stress Center 513 -558 -5872
 Kathleen peterson forensic evidence
Kathleen peterson forensic evidence ........ is an alternative of log based recovery.
........ is an alternative of log based recovery. Va ptsd rating scale pdf
Va ptsd rating scale pdf Causes of ptsd
Causes of ptsd Cognitive processing therapy worksheets
Cognitive processing therapy worksheets Ptsd norsk
Ptsd norsk Ptsd circumcision
Ptsd circumcision Ptsd
Ptsd Evolution of ptsd
Evolution of ptsd Lorna myers pnes
Lorna myers pnes Ptsd stages
Ptsd stages Remains by simon armitage poem
Remains by simon armitage poem She should have died hereafter analysis
She should have died hereafter analysis Jamal and deborah therapy
Jamal and deborah therapy Dual representation theory ptsd
Dual representation theory ptsd Ptsd model ehlers and clark
Ptsd model ehlers and clark Ptsd violent behavior
Ptsd violent behavior Psykoedukation ptsd
Psykoedukation ptsd C ptsd
C ptsd Ptsd spiritual warfare
Ptsd spiritual warfare Kompleks ptsd trigger
Kompleks ptsd trigger Psychosis and ptsd
Psychosis and ptsd Frelsning
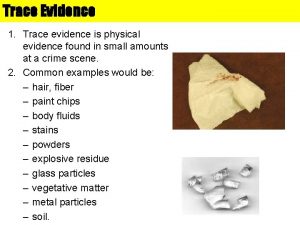
Frelsning Secondary sources
Secondary sources Example of fallacy
Example of fallacy Class vs individual evidence
Class vs individual evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Secondary sources
Secondary sources Primary evidence vs secondary evidence
Primary evidence vs secondary evidence