PTSD Treatment The State of the Evidence Paula







![Pharmacotherapy Choices • As monotherapy, strongly recommend [A]: - SSRIs (fluoxetine, paroxetine, and sertraline Pharmacotherapy Choices • As monotherapy, strongly recommend [A]: - SSRIs (fluoxetine, paroxetine, and sertraline](https://slidetodoc.com/presentation_image/76303698b4e13c8546b0fb2d849c9df0/image-21.jpg)


- Slides: 29
PTSD Treatment: The State of the Evidence Paula P. Schnurr, Ph. D VA National Center for PTSD, Executive Division Dartmouth Medical School

Overview • Review evidence on the treatment of PTSD • Describe the new VA/Do. D Practice Guideline for PTSD • Discuss implications for treating women veterans

Effectiveness of Treatments for PTSD Medication. 36 Somatic 1. 15 Psychotherapy 1. 13 N = 51 N=4 N = 67 Antidepressant. 40 Atyp. Antipsychotic. 39 N = 30 N=8 Acupuncture 1. 28 N=1 CBT 1. 26 N = 47 EMDR 1. 04 N = 10 Group. 46 N=6 Other -. 53 -. 78 N=4 (some ns) Only significant 1 st and 2 nd level categories are shown. – Watts, Schnurr et al. , under review. Effect sizes are represented as a modified Hedges g, indicating benefit relative to a control group. N = number of comparisons.

Meta-Regression of Psychotherapy and Medication Effects Psychotherapy Medication Effect size 1. 13 . 36** Adjusted effect sizea . 91 . 41* a. Adjusted for type of comparison group, missing data procedure, blinding, % of veteran subjects, and % of women. *p<. 05, **p<. 001 – Watts, Schnurr et al. , under review. Effect sizes are represented as a modified Hedges g, indicating benefit relative to a control group.
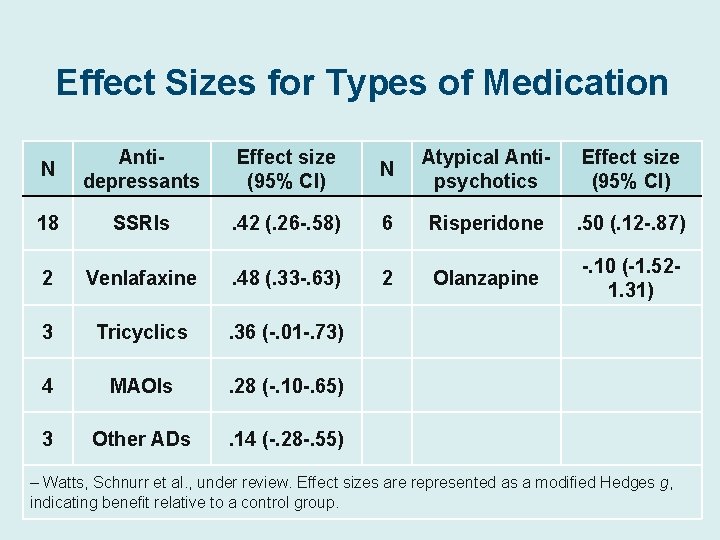
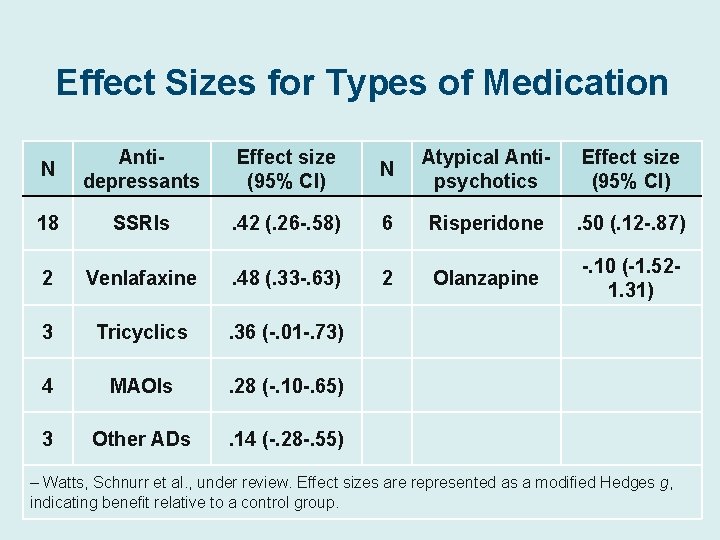
Effect Sizes for Types of Medication N Antidepressants Effect size (95% CI) N Atypical Antipsychotics Effect size (95% CI) 18 SSRIs . 42 (. 26 -. 58) 6 Risperidone . 50 (. 12 -. 87) 2 Venlafaxine . 48 (. 33 -. 63) 2 Olanzapine -. 10 (-1. 521. 31) 3 Tricyclics . 36 (-. 01 -. 73) 4 MAOIs . 28 (-. 10 -. 65) 3 Other ADs . 14 (-. 28 -. 55) – Watts, Schnurr et al. , under review. Effect sizes are represented as a modified Hedges g, indicating benefit relative to a control group.
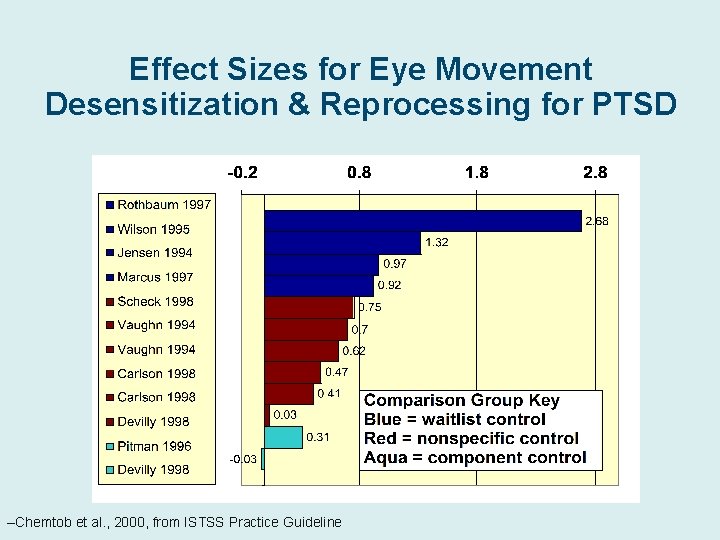
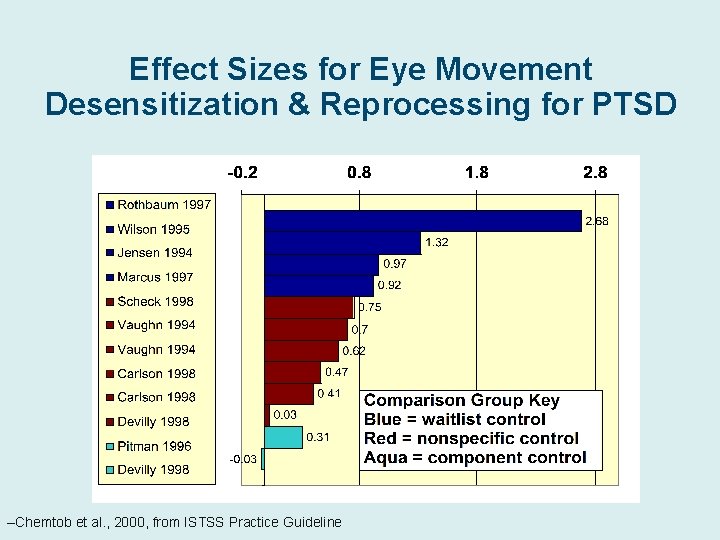
Effect Sizes for Eye Movement Desensitization & Reprocessing for PTSD –Chemtob et al. , 2000, from ISTSS Practice Guideline

Effect Sizes for Types of Cognitive -Behavioral Therapy Primarily Cognitive Effect size 95% CI % waitlist control 1. 71 Primarily Cognitive & Stress Exposure Inoculation 1. 09 1. 2. 12. 86 -1. 33 71% 48% 1. 31 1. 37 . 93 -1. 69 . 80 -1. 94 72% 100% All comparisons between treatments are not statistically significant – Watts, Schnurr et al. , under review. Effect sizes are represented as a modified Hedges g, indicating benefit relative to a control group.
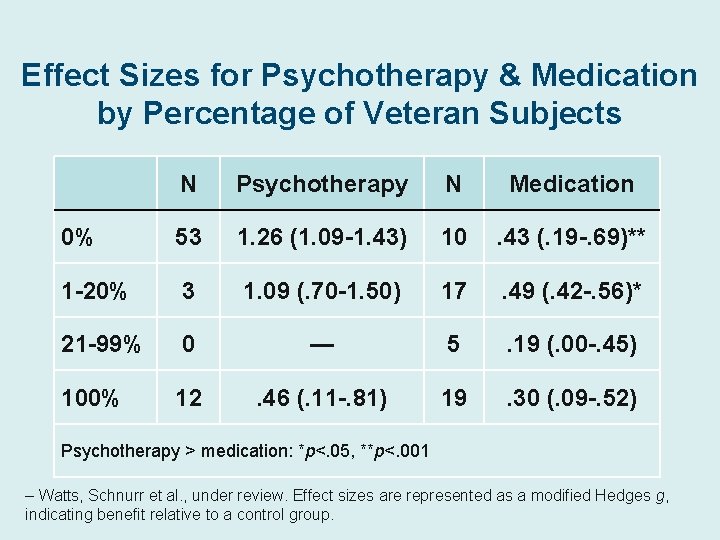
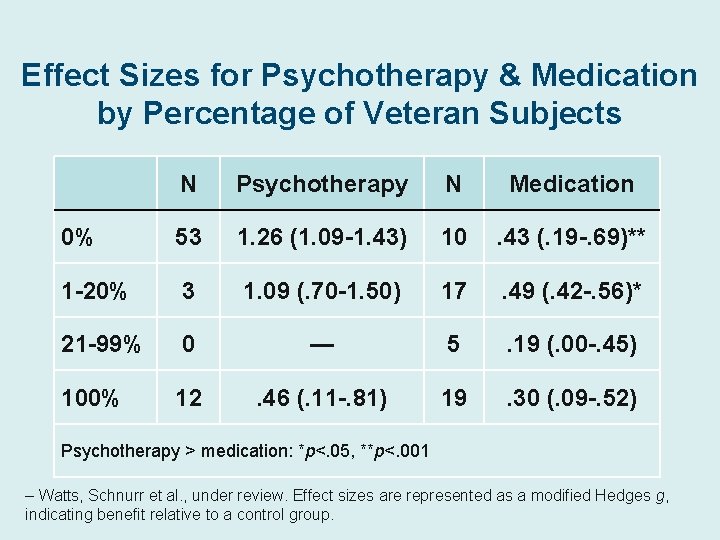
Effect Sizes for Psychotherapy & Medication by Percentage of Veteran Subjects N Psychotherapy N Medication 0% 53 1. 26 (1. 09 -1. 43) 10 . 43 (. 19 -. 69)** 1 -20% 3 1. 09 (. 70 -1. 50) 17 . 49 (. 42 -. 56)* 21 -99% 0 — 5 . 19 (. 00 -. 45) 100% 12 . 46 (. 11 -. 81) 19 . 30 (. 09 -. 52) Psychotherapy > medication: *p<. 05, **p<. 001 – Watts, Schnurr et al. , under review. Effect sizes are represented as a modified Hedges g, indicating benefit relative to a control group.
VA/Do. D Clinical Practice Guideline for Management of Post-Traumatic Stress Update– 2010 www. healthquality. va. gov www. qmo. amedd. army. mil
Why Have Clinical Practice Guidelines? • To inform practice • To enhance patient outcomes • To reduce unnecessary variation • To promote efficient and effective use of resources
Methods of Guideline Development • Based on systematic reviews and metaanalyses of evidence • Guidelines vary in what is considered and how evidence is weighted - Well-done randomized controlled trials carry the highest weight - Other studies may be considered - Quality and amount of evidence is considered
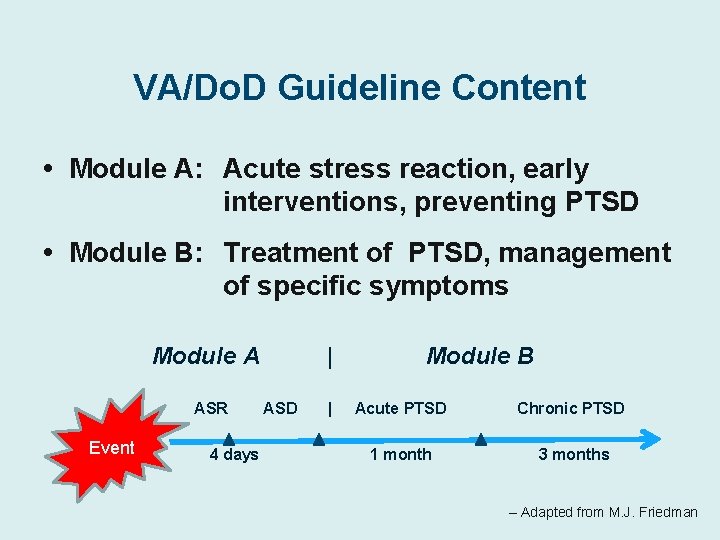
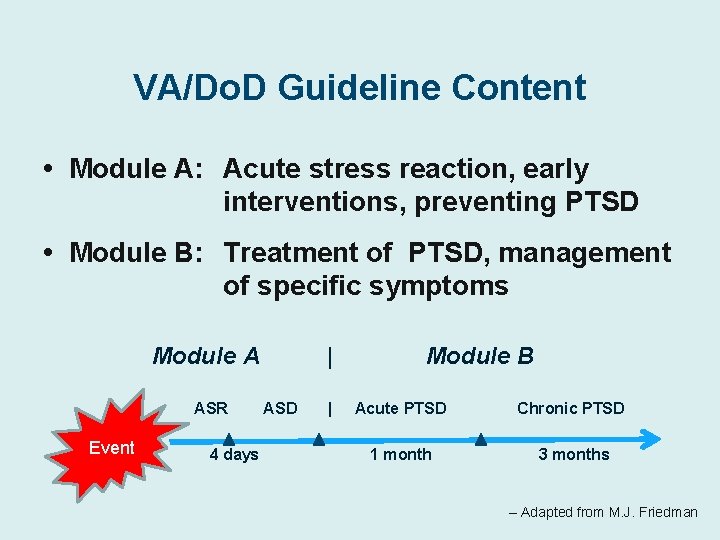
VA/Do. D Guideline Content • Module A: Acute stress reaction, early interventions, preventing PTSD • Module B: Treatment of PTSD, management of specific symptoms Module A ASR Event 4 days | ASD | Module B Acute PTSD Chronic PTSD 1 month 3 months – Adapted from M. J. Friedman
Differences From the 2004 VA/Do. D Guideline • Original 5 modules have been consolidated into 2 modules: 1. Acute Stress Response and early prevention of PTSD 2. Treatment of PTSD • Guideline recommendations are patientcentered, regardless of setting of care • Psychological First Aid – Key concept as initial response – Adapted from M. J. Friedman
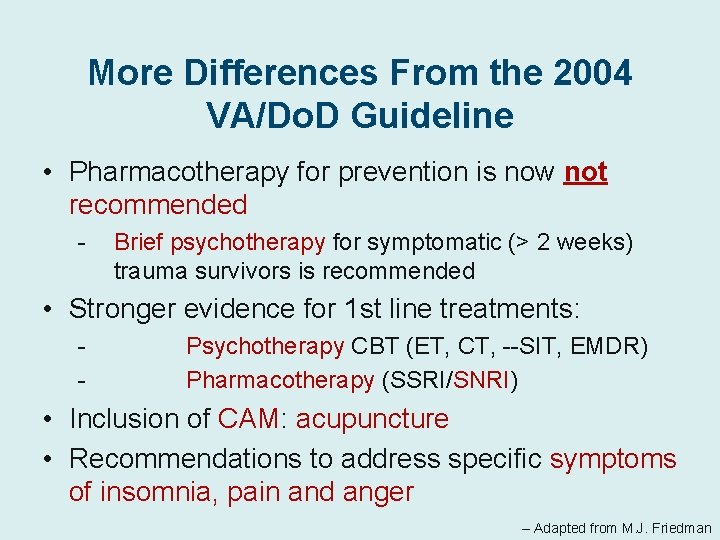
More Differences From the 2004 VA/Do. D Guideline • Pharmacotherapy for prevention is now not recommended - Brief psychotherapy for symptomatic (> 2 weeks) trauma survivors is recommended • Stronger evidence for 1 st line treatments: - Psychotherapy CBT (ET, CT, --SIT, EMDR) Pharmacotherapy (SSRI/SNRI) • Inclusion of CAM: acupuncture • Recommendations to address specific symptoms of insomnia, pain and anger – Adapted from M. J. Friedman

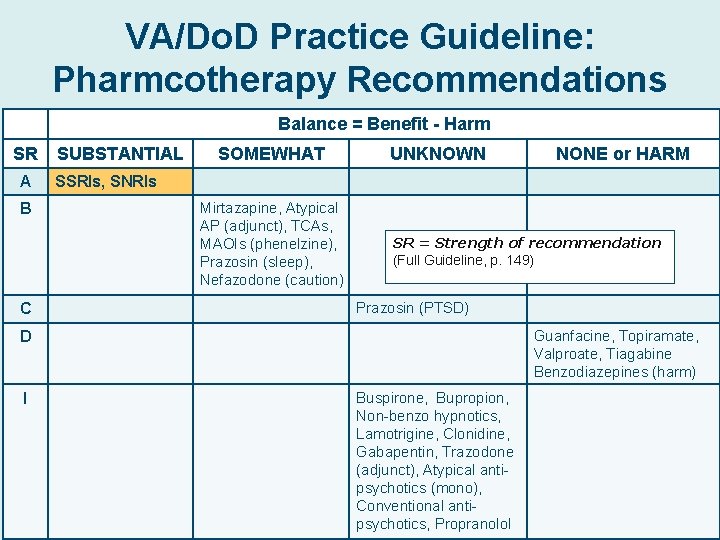
Strength of Recommendations A • A strong recommendation that clinicians provide the intervention to eligible patients. Good evidence … that the intervention improves important health outcomes and … benefits substantially outweigh harm. B • A recommendation that clinicians provide (the service) to eligible patients. At least fair evidence … that the intervention improves health outcomes and … benefits outweigh harm. C • No recommendation for or against the routine provision of the intervention is made. At least fair evidence … that the intervention can improve health outcomes but … the balance of benefits and harms is too close to justify a general recommendation. I • …evidence is insufficient to recommend for or against routinely providing the intervention. Evidence that the intervention is effective is lacking, of poor quality, or conflicting, and the balance of benefits and harms can not be determined.

VA/Do. D Practice Guideline: Psychotherapy Recommendations Balance = Benefit - Harm SR A SUBSTANTIAL • Trauma-focused psychotherapy that includes components of exposure and/or cognitive restructuring; OR • Stress inoculation training SOMEWHAT UNKNOWN SR = Strength of recommendation (Full Guideline, p. 115). C Patient Education, Imagery Rehearsal Therapy, Psychodynamic Therapy, Hypnosis, Relaxation Techniques, Group Therapy I Family therapy Web-Based CBT, Dialectical Behavior Therapy, Acceptance & Commitment Therapy
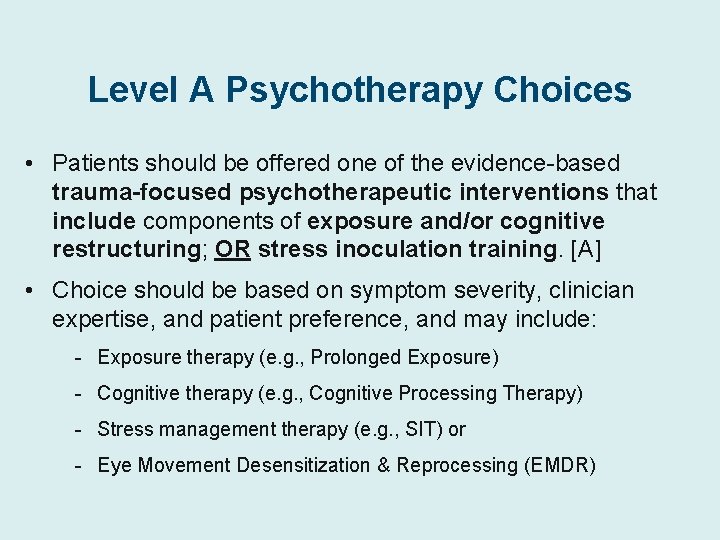
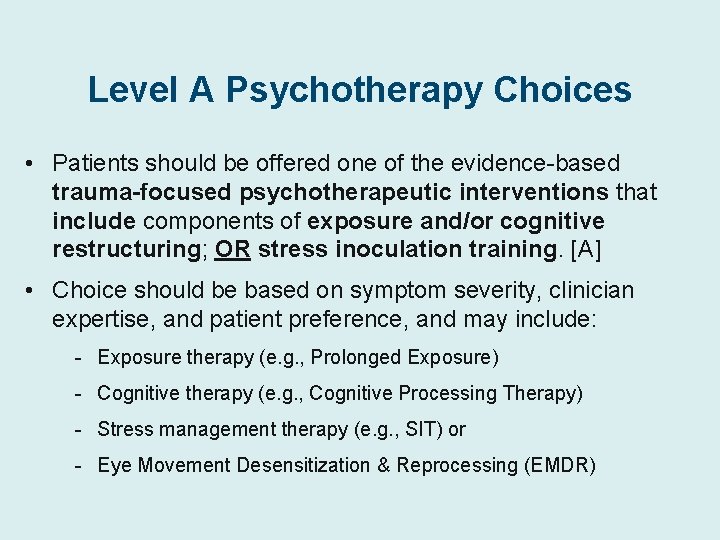
Level A Psychotherapy Choices • Patients should be offered one of the evidence-based trauma-focused psychotherapeutic interventions that include components of exposure and/or cognitive restructuring; OR stress inoculation training. [A] • Choice should be based on symptom severity, clinician expertise, and patient preference, and may include: - Exposure therapy (e. g. , Prolonged Exposure) - Cognitive therapy (e. g. , Cognitive Processing Therapy) - Stress management therapy (e. g. , SIT) or - Eye Movement Desensitization & Reprocessing (EMDR)
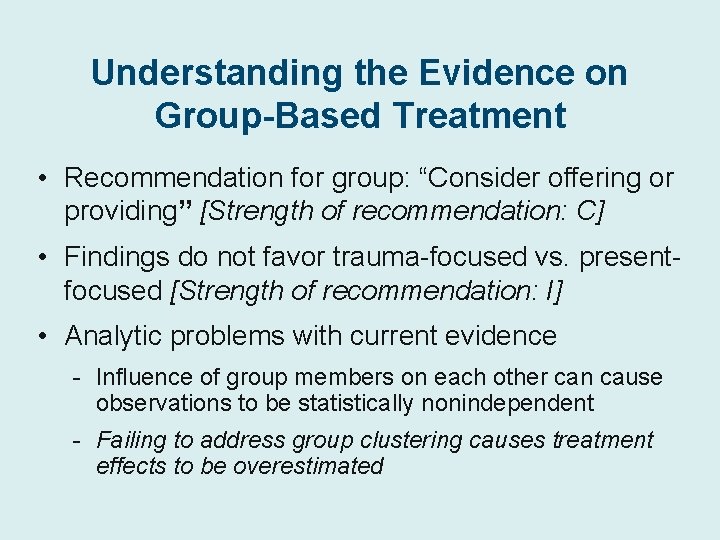
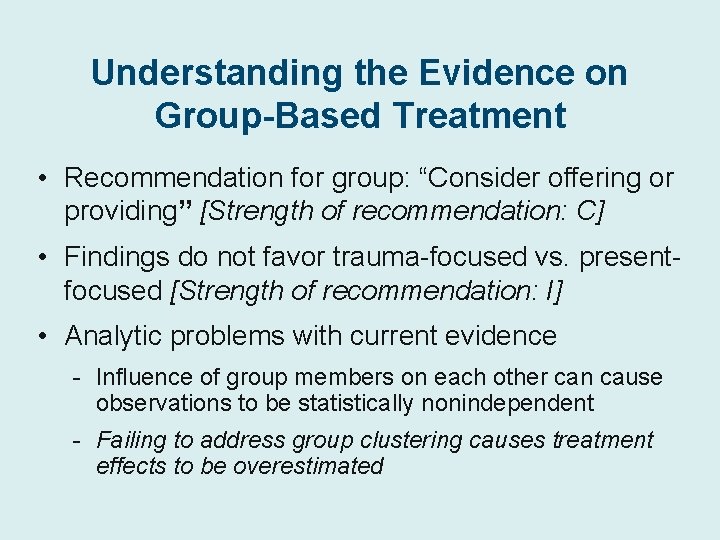
Understanding the Evidence on Group-Based Treatment • Recommendation for group: “Consider offering or providing” [Strength of recommendation: C] • Findings do not favor trauma-focused vs. presentfocused [Strength of recommendation: I] • Analytic problems with current evidence - Influence of group members on each other can cause observations to be statistically nonindependent - Failing to address group clustering causes treatment effects to be overestimated

Effects of Corrected Analysis on Results of Group Treatment Baldwin et al. (2006) reanalysis of significant tests for evidence-based group treatments - Corrected dfs - Varied ICC assumptions Implications: evidence is optimistically biased
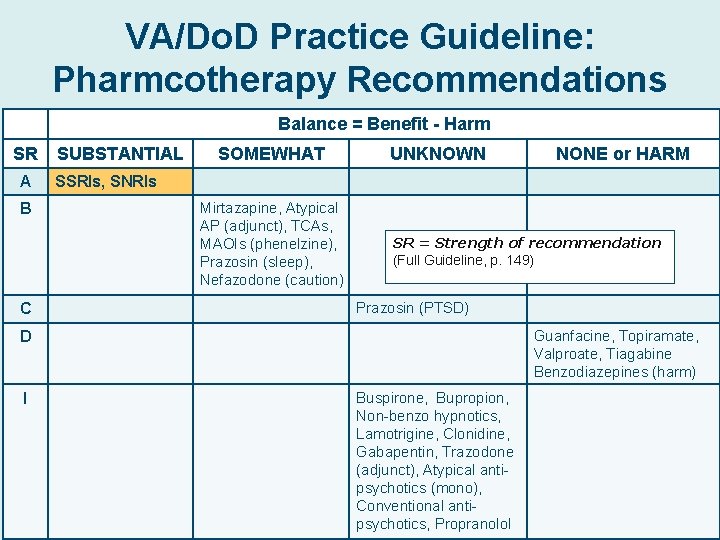
VA/Do. D Practice Guideline: Pharmcotherapy Recommendations Balance = Benefit - Harm SR A B C SUBSTANTIAL SOMEWHAT UNKNOWN SSRIs, SNRIs Mirtazapine, Atypical AP (adjunct), TCAs, MAOIs (phenelzine), Prazosin (sleep), Nefazodone (caution) SR = Strength of recommendation (Full Guideline, p. 149). Prazosin (PTSD) Guanfacine, Topiramate, Valproate, Tiagabine Benzodiazepines (harm) D I NONE or HARM Buspirone, Bupropion, Non-benzo hypnotics, Lamotrigine, Clonidine, Gabapentin, Trazodone (adjunct), Atypical antipsychotics (mono), Conventional antipsychotics, Propranolol
![Pharmacotherapy Choices As monotherapy strongly recommend A SSRIs fluoxetine paroxetine and sertraline Pharmacotherapy Choices • As monotherapy, strongly recommend [A]: - SSRIs (fluoxetine, paroxetine, and sertraline](https://slidetodoc.com/presentation_image/76303698b4e13c8546b0fb2d849c9df0/image-21.jpg)
Pharmacotherapy Choices • As monotherapy, strongly recommend [A]: - SSRIs (fluoxetine, paroxetine, and sertraline have strongest support) - SNRIs (venlafaxine has the strongest support for treatment of PTSD) • As adjunctive therapy, recommend [B]: - Atypical antipsychotics (risperidone and olanzapine) – Adapted from M. J. Friedman
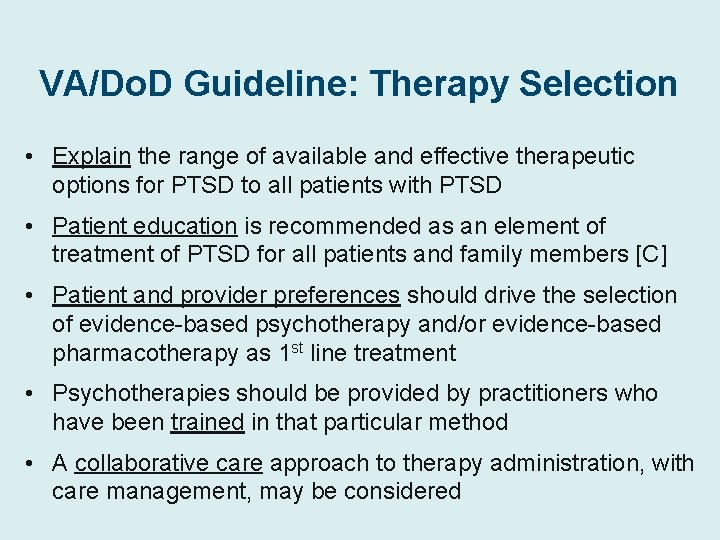
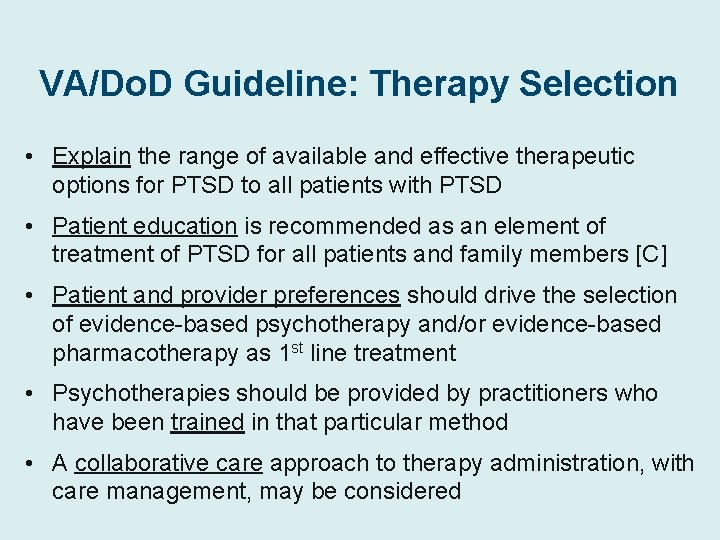
VA/Do. D Guideline: Therapy Selection • Explain the range of available and effective therapeutic options for PTSD to all patients with PTSD • Patient education is recommended as an element of treatment of PTSD for all patients and family members [C] • Patient and provider preferences should drive the selection of evidence-based psychotherapy and/or evidence-based pharmacotherapy as 1 st line treatment • Psychotherapies should be provided by practitioners who have been trained in that particular method • A collaborative care approach to therapy administration, with care management, may be considered
In FY 2010, 5. 9% of VA users were women • Overall, 10. 9% of women had PTSD vs. 8. 2% of men • Among OEF/OIF Veterans, 17. 3% of women had PTSD vs. 23. 6% of men

The Percentage of Veterans Who are Women is Growing – National Center for Veterans Analysis and Statistics, 2010
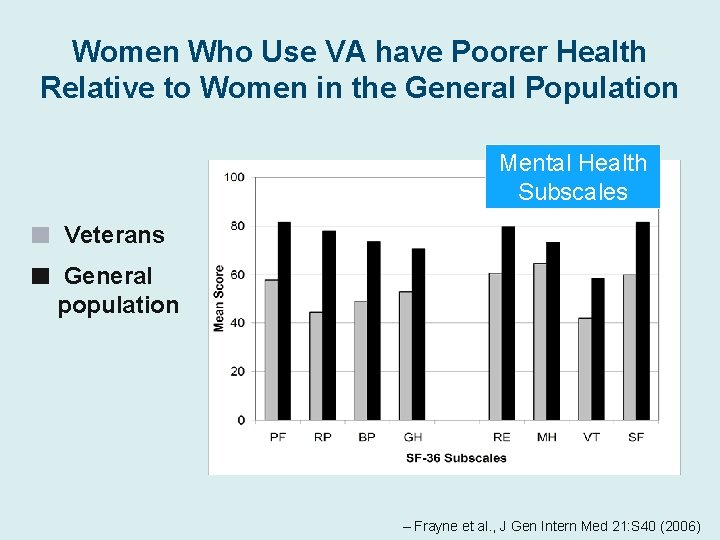
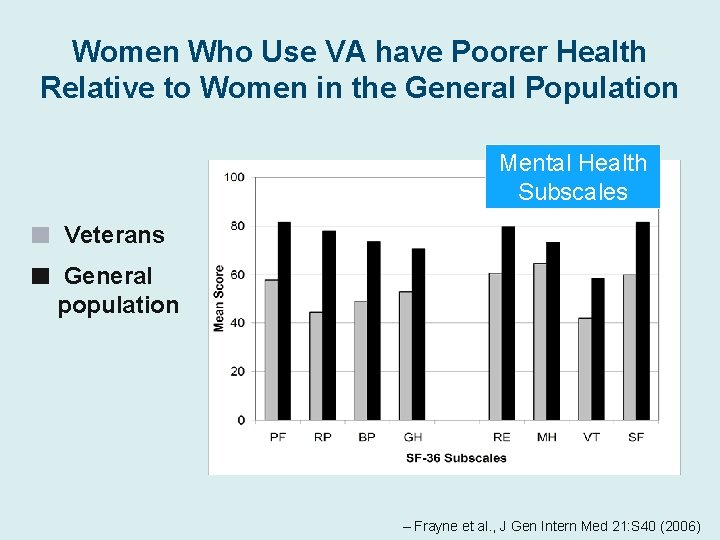
Women Who Use VA have Poorer Health Relative to Women in the General Population Mental Health Subscales ■ ■ Veterans General population – Frayne et al. , J Gen Intern Med 21: S 40 (2006)

Among VA Users, Women are More Likely Than Men to have Mental Health Problems 31% of women vs. 20% of men have a diagnosed mental health condition From Frayne, VA Women’s Health Evaluation Initiative. Percents are based on presence of at least 2 instances of mental health condition ICD-9 codes in VA outpatient administrative data 26 in FY 08; includes veteran patients only.
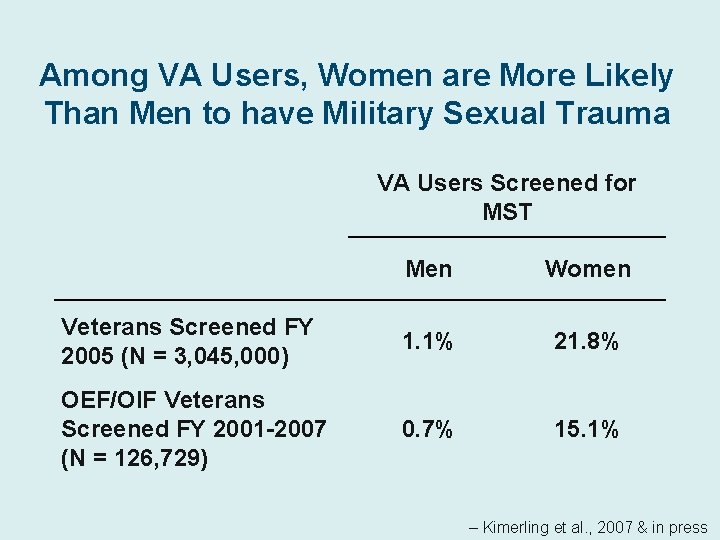
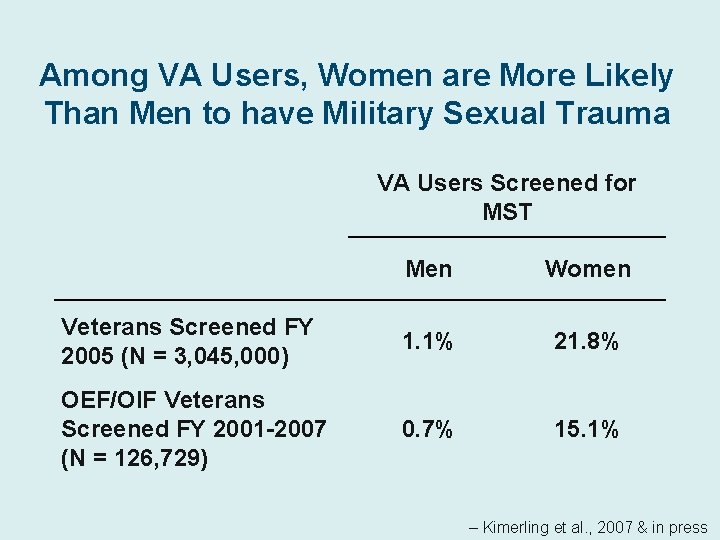
Among VA Users, Women are More Likely Than Men to have Military Sexual Trauma VA Users Screened for MST Men Women Veterans Screened FY 2005 (N = 3, 045, 000) 1. 1% 21. 8% OEF/OIF Veterans Screened FY 2001 -2007 (N = 126, 729) 0. 7% 15. 1% – Kimerling et al. , 2007 & in press
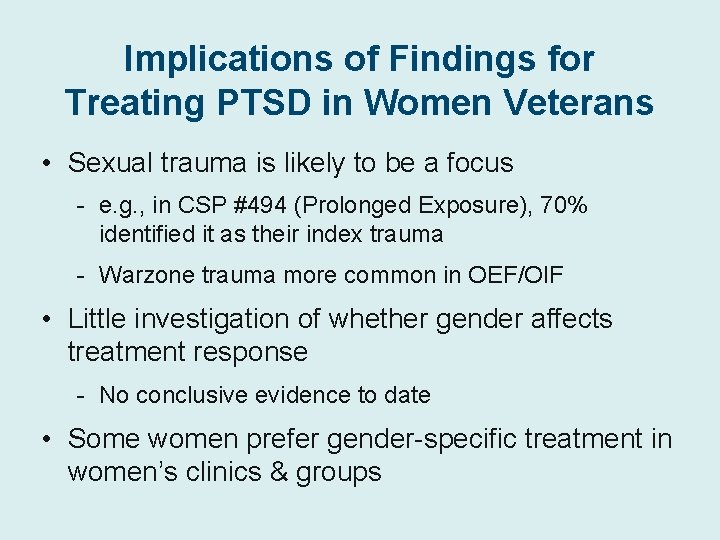
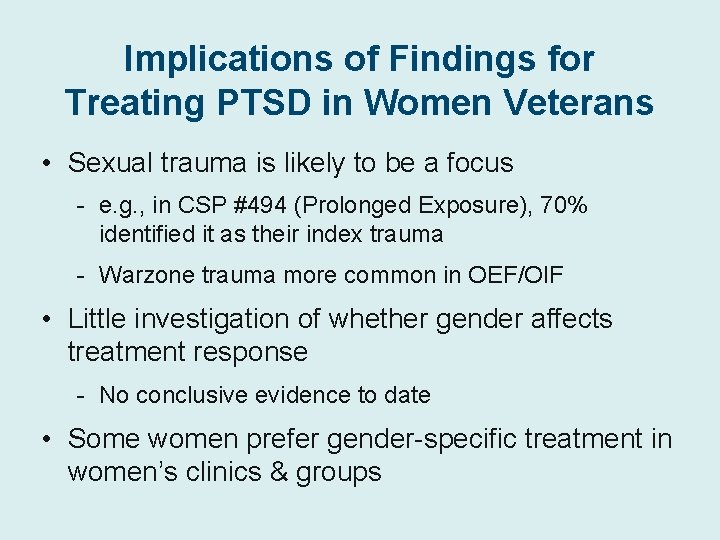
Implications of Findings for Treating PTSD in Women Veterans • Sexual trauma is likely to be a focus - e. g. , in CSP #494 (Prolonged Exposure), 70% identified it as their index trauma - Warzone trauma more common in OEF/OIF • Little investigation of whether gender affects treatment response - No conclusive evidence to date • Some women prefer gender-specific treatment in women’s clinics & groups
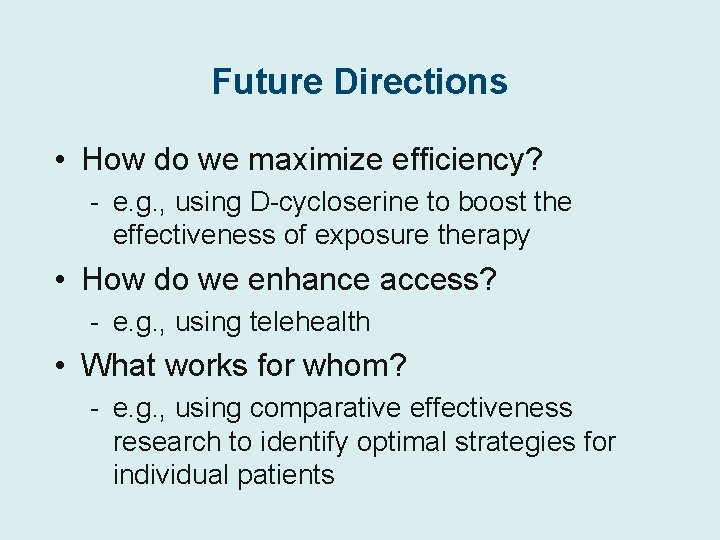
Future Directions • How do we maximize efficiency? - e. g. , using D-cycloserine to boost the effectiveness of exposure therapy • How do we enhance access? - e. g. , using telehealth • What works for whom? - e. g. , using comparative effectiveness research to identify optimal strategies for individual patients
 Psychosis and ptsd
Psychosis and ptsd Ptsd symptomer
Ptsd symptomer Macbeth nihilism quote
Macbeth nihilism quote Psykoedukation ptsd
Psykoedukation ptsd Va ptsd rating scale pdf
Va ptsd rating scale pdf Lorna myers pnes
Lorna myers pnes Dual representation theory ptsd
Dual representation theory ptsd Ptsd spiritual warfare
Ptsd spiritual warfare Cpt impact statement example
Cpt impact statement example Remains simon armitage
Remains simon armitage Ptsd violent behavior
Ptsd violent behavior Strukturell dissociation
Strukturell dissociation Evolution of ptsd
Evolution of ptsd Ptsd
Ptsd Ptsd
Ptsd C ptsd
C ptsd Causes of ptsd
Causes of ptsd Ptsd stages
Ptsd stages Ptsd model ehlers and clark
Ptsd model ehlers and clark Toleransevinduet
Toleransevinduet Ptsd circumcision
Ptsd circumcision Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Secondary sources
Secondary sources Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Are fibers class evidence
Are fibers class evidence Class evidence vs individual evidence
Class evidence vs individual evidence Explain how class evidence may be useful
Explain how class evidence may be useful Individual vs class evidence
Individual vs class evidence