PICU Primer II Kevin M Creamer M D

- Slides: 50
PICU Primer II Kevin M. Creamer M. D. Pediatric Critical Care Walter Reed AMC
The Primer Outline ¨ Physiology ¨ ICU Care – Hypoxia / Hypoxemia – Postoperative – ABG’s and Acidosis issues – Sodium and H 2 O – Mechanical metabolism Ventilation – Hemodynamics and ¨ Common Problems Cardiopulmonary – Head trauma interactions – Toxicology
Postoperative Issues ¨ Borrowed in part from Akron syllabus ¨ Know the surgery – what can you expect from a posterior spinal fusion is different than a tracheal reconstruction ¨ Know the patient – Age, PMHx, Syndromes ¨ Be there when they get out of the OR
Postoperative Evaluation ¨ ABC’s ¨ Look at the breathing pattern ¨ Listen to the chest--breath sounds, stridor? ¨ Listen to the heart--gallop, murmur? ¨ Feel the pulses--strong, weak, thready? – Cap refill? , Extremity warmth?
The Anesthesia Report ¨ “History of present illness” for surgical patients – Difficulties with induction or intubation? – Drugs used during case – Regional techniques employed? – Extubation-problems? ¨ Vital signs- BP, HR, RR, Sa. O 2, temp – Patients are frequently cold!
The Anesthesia Report ¨ Ventilation parameters/difficulties ¨ Fluids--ins and outs ¨ Any “events”? ¨ Lines and tubes
Intraoperative Fluids ¨ Pediatrician: “Why do they always get so much fluid? ” ¨ Anesthesiologist: “Because they need it” – maintenance + replacement of “third space” losses • “third space” losses can be 15 cc/kg/hr + replacement of 3 X blood loss
Anesthesia and Fluid Balance ¨ General anesthesia produces vasodilation and some decrease in myocardial contractility. ¨ Increased intrathoracic pressure, and stress response to surgical stimulus, may lead to increased ADH production and decreased urine output
BLOOD loss and replacement ¨Blood loss is estimated ¨ Transfusion Criteria - it depends – Check Hct, HR, UOP, p. H, ongoing loss, Hemodynamics … ¨ When do you need Component Tx? – after a “massive” transfusion or ( 0. 75 -3. 0 blood volumes)
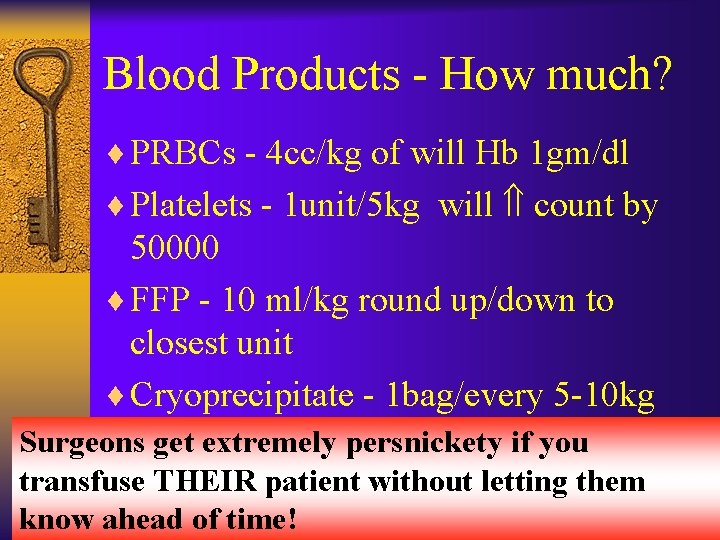
Blood Products - How much? ¨ PRBCs - 4 cc/kg of will Hb 1 gm/dl ¨ Platelets - 1 unit/5 kg will count by 50000 ¨ FFP - 10 ml/kg round up/down to closest unit ¨ Cryoprecipitate - 1 bag/every 5 -10 kg Surgeons get extremely persnickety if you transfuse THEIR patient without letting them know ahead of time!
The Surgical Report ¨ Since we are not surgeons we need to know what they anticipate and worry about – Amount of pain – Third spacing – Possible complications ¨ Their wish list: – Extubate tomorrow, MRI at midnight – Special meds: antibiotic and stress ulcer prophylaxis
The Surgical Report ¨ What to touch and not to touch? – NG, foley, chest tube, rectum, etc. ¨ Check all their orders for appropriate dosing and fluids – mg/kg/dose is not in surgical vocabulary ¨ Who is in Charge? (Us vs. Them) ¨ Surgical POC? – Interface with surgeons before they return to the OR in AM regarding the plan
Assessment of Fluid Balance: ¨ Vital signs (HR/BP) ¨ Urine output ¨ Extremity warmth, CRT ¨ Acid-base status ¨ Occasionally invasive monitoring – Remember the Liver!
Extubation Time? ¨ Adequate airway (edema? , Leak? ) ¨ Maintain oxygenation and ventilation ¨ Neurologically able to protect the airway and maintain adequate drive. ¨ Small/young infants are at increased risk of apnea – Especially if post-conceptual age < 50 weeks
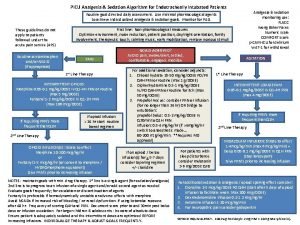
Sedation and Analgesia ¨ Analgesia for painful diseases and procedures ¨ Compliance with controlled ventilation and routine intensive care ¨ Sedation for amnesia for the periods of noxious stimuli ¨ Reduce the physiologic responses to stress
Sedation and Analgesia ¨ The idea of titrating drugs to effect-- there is no “dose”. – Keep in mind what the “target” response is. ¨ Consider Round-the-clock Tylenol for 24 -48 hours as adjunct – First PR dose may be 30 -40 mg/kg ¨ Anesthesia service manages Epidurals ¨ Consider a continuous drip
BP: hypotension, H: Histamine, A: Apnea, CWR: chest wall rigidity
Muscle Relaxants ¨ They provide ZERO sedation/analgesia. ¨ Indications (always relative) – Mechanical ventilation where risk of extubation is great, or risk of baro/volutrauma is high – Procedures such as central line placement or biopsy in the intubated patient – Intractable intracranial hypertension (IF ICP being monitored)
Problems with Blockade ¨ Fluid retention ¨ Long term weakness – continuous infusions – most commonly the steroid based NMBs – myopathy associated with Atracurium – consider using cis-Atracurium ¨ Consider Train of Four testing ¨ FREQUNTLY OVERUSED
¨ NEXT UP – Mechanical ventilation This is not the NICU!
Lesson Learned: VALI –Predisposing Factors ¨ High lung Volumes – With high peak pressure and alveolar overdistension ¨ Repeated alveolar collapse and reopening ¨ High inspired oxygen Concentrations ¨ Preexisting lung injury Slutsky Am J Resp CCM, 1999, Dreyfuss Am J Resp CCM 1998
Mechanical Ventilation ¨ Do’s and Don’ts – Avoid Overdistension and High Pressure by limiting Tv – Avoid Hyperoxic Lung damage by turning FIO 2 down (Sat 90% okay) – Avoid cyclic collapse by using PEEP to recruit FRC and keep it above Closing volume ¨ Infant high risk 2° high elastic recoil and complaint chest wall
Open Lung Strategy

Getting Started (Parameters)
Getting Started (Mode)
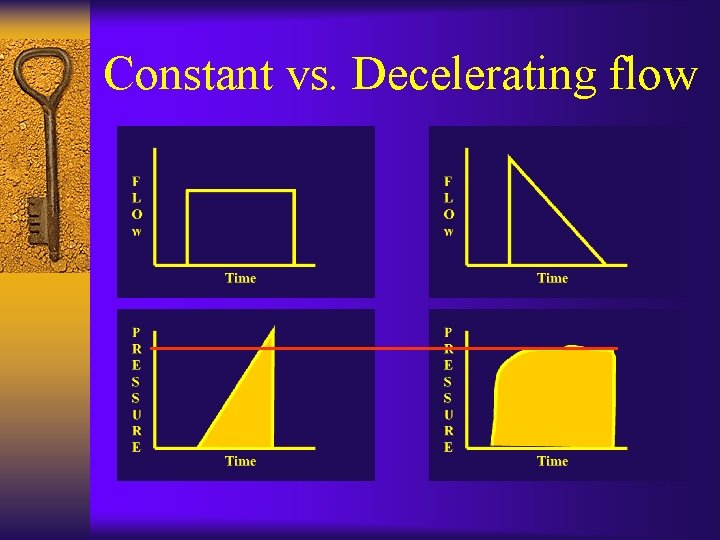
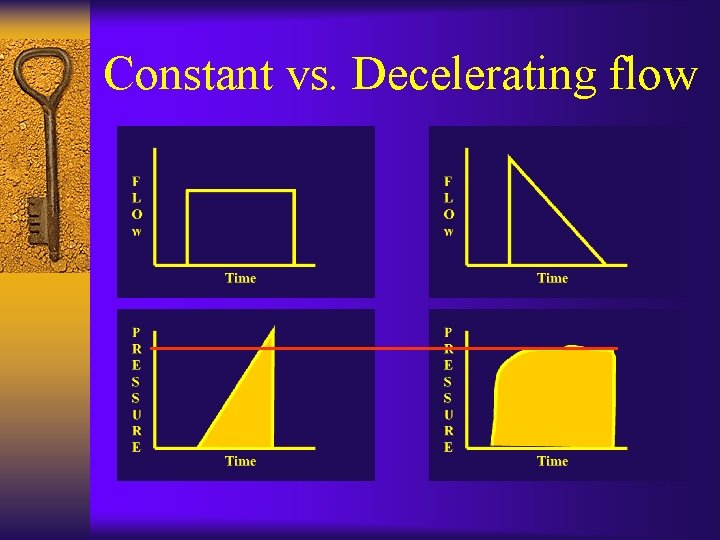
Constant vs. Decelerating flow
Getting Started (Settings) ¨ FIO 2 - 50%, if sick 100% ¨ It - minimum. 5 sec, older kids 1 sec ¨ Rate - age appropriate 15 -30 to start ¨ Tv - 10 ml/kg to start ¨ Look / Listen / Ask ¨ PEEP - 4 cm, higher if FRC compromised
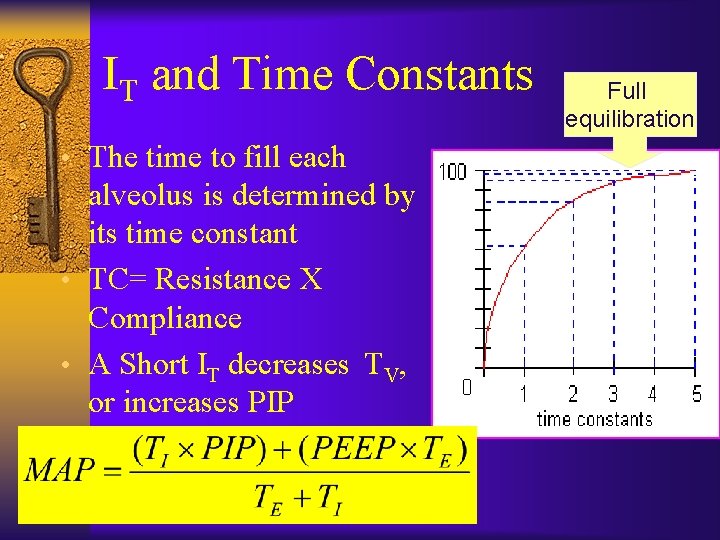
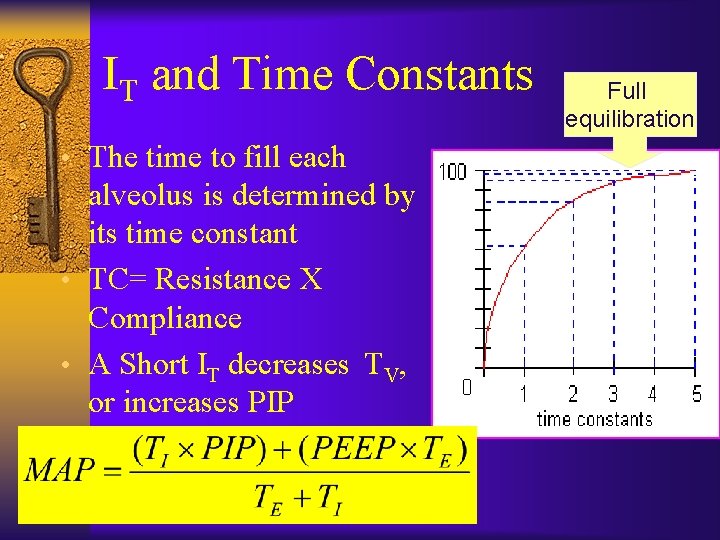
IT and Time Constants • The time to fill each alveolus is determined by its time constant • TC= Resistance X Compliance • A Short IT decreases TV, or increases PIP Full equilibration
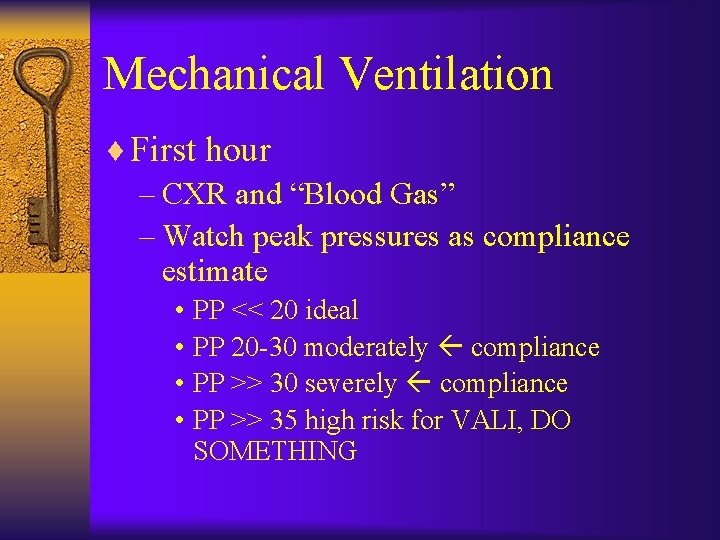
Mechanical Ventilation ¨ First hour – CXR and “Blood Gas” – Watch peak pressures as compliance estimate • PP << 20 ideal • PP 20 -30 moderately compliance • PP >> 30 severely compliance • PP >> 35 high risk for VALI, DO SOMETHING
Mechanical Ventilation ¨ Change Tv only for inappropriate chest rise or for elevated inspiratory pressures (Don’t WEAN Tv) ¨ Sedation to allow patient - ventilator synchrony (Paralytics aren’t required)
Monitoring adjuncts ¨ Pulse oximeter ¨ End tidal CO 2 - can use for Dead space estimate ¨ ABG’s and CBG’s ¨ Calculate Compliance, A-a gradient, Oxygenation Index (OI), check for Autopeep ¨ Graphics - PV and flow-volume loops
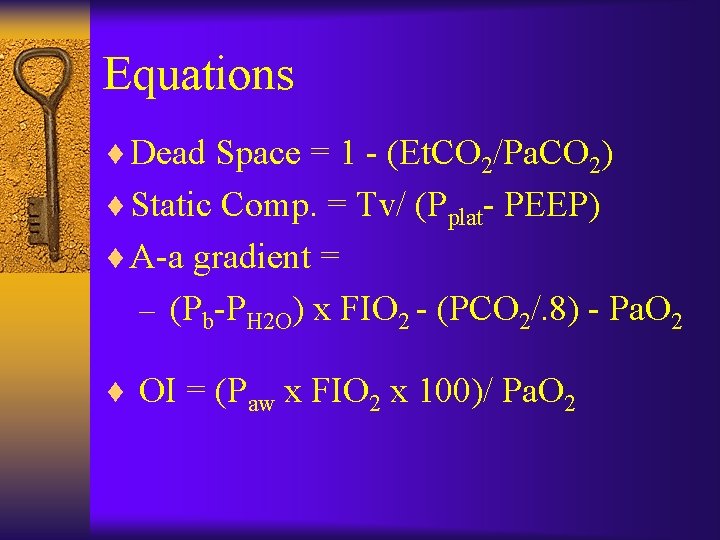
Equations ¨ Dead Space = 1 - (Et. CO 2/Pa. CO 2) ¨ Static Comp. = Tv/ (Pplat- PEEP) ¨ A-a gradient = – (Pb-PH 2 O) x FIO 2 - (PCO 2/. 8) - Pa. O 2 ¨ OI = (Paw x FIO 2 x 100)/ Pa. O 2
When things go wrong ¨ Don’t be a DOPE ¨ Hypoxemia - PEEP to FRC, to allow FIO 2 wean to < 50% ¨ Elevated peak pressures - suction, adopt Permissive hypercapnia, consider changing to pressure mode ¨ Check circuit size – an inappropriately large circuit can gobble up lots of tidal volume
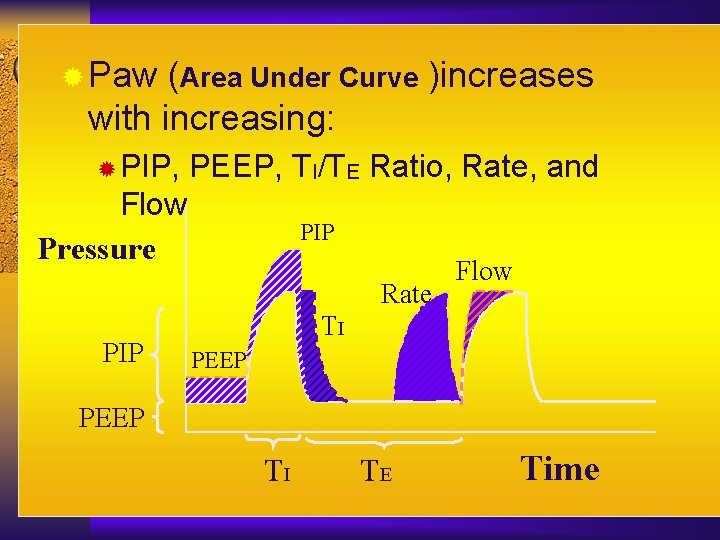
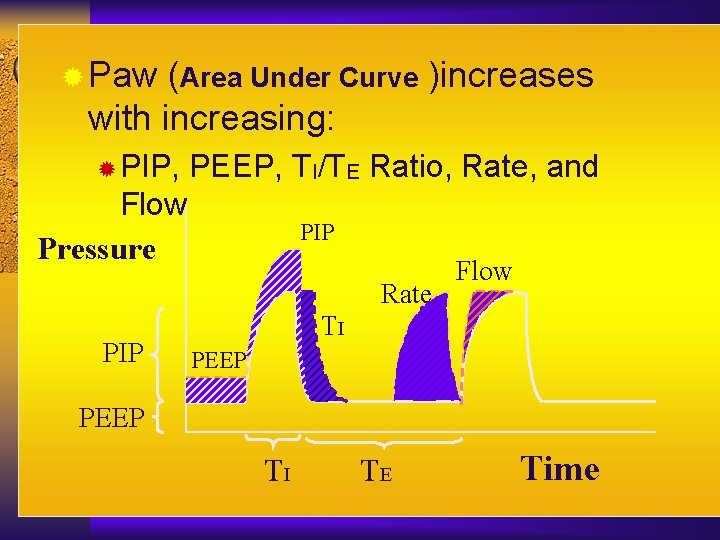
® Paw (Area Under Curve )increases with increasing: ® PIP, PEEP, TI/TE Ratio, Rate, and Flow Pressure PIP Rate PIP Flow TI PEEP TI TE Time
Circuit compliance ¨ When using volume ventilation the ventilator circuit or tubing will stretch – Neonatal 0. 35 ml / cm H 2 O – Pediatric 1. 4 ml / cm H 2 O – Adult 2. 8 ml / cm H 2 O ¨ This means the stiffer the lung the more volume is lost in the circuit
Mechanical Ventilation ¨ First day and beyond – Watch for fluid overload • all patients on positive pressure ventilation retain lung water – Assist patient efforts • Pressure support or volume support • Trigger sensitivity (age and disease appropriate) – Treat underlying condition – Feed patient
Weaning ¨ Get condition under control ¨ Stop paralytics (PEEP < 8) ¨ Encourage patient’s efforts – Rate (slow then fast) – add Pressure support (2/3 P) ¨ Wean PEEP and PS slowly in 1 -2 cm H 2 O increments ¨ Wean FIO 2 to 30% if possible
Signs of weaning failure ¨ Increased Work of breathing – fast spontaneous RR – small spontaneous Tv ¨ Increased FIO 2 requirement ¨ Hemodynamic compromise
Time for Extubation? ¨ Think SOAP – Secretions / Sedation / Spontaneous Tv (>5 ml/kg) – Oxygenation <35% – Airway - Maintainable? , Leak? , Steroids? – Pressures - PP <25, PEEP < 5
Extubation success predictors Khan, CCM 1996
Special situations I ¨ Obstructive Diseases – Asthma and RSV Bronchiolitis – Watch for air trapping / breath stacking • Low rate, larger Tidal volume, long Expiratory time • check Autopeep • preserve I-time • Consider Heliox, Ketamine, Halothane
Special situations II ¨ ARDS – Limit Tv accept hypercapnia – Increase PEEP for FRC – Prone positioning – Ca. O 2 and tolerate lower Sat % – consider High Frequency Oscillatory Ventilation>>> Surfactant>>> Nitric Oxide
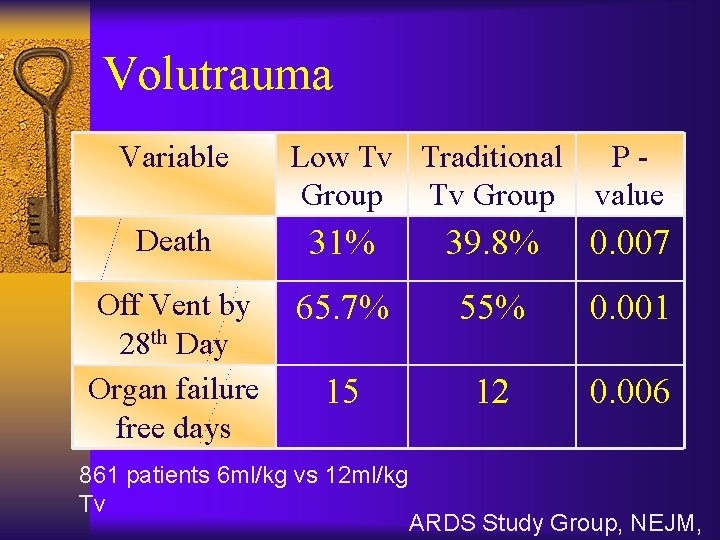
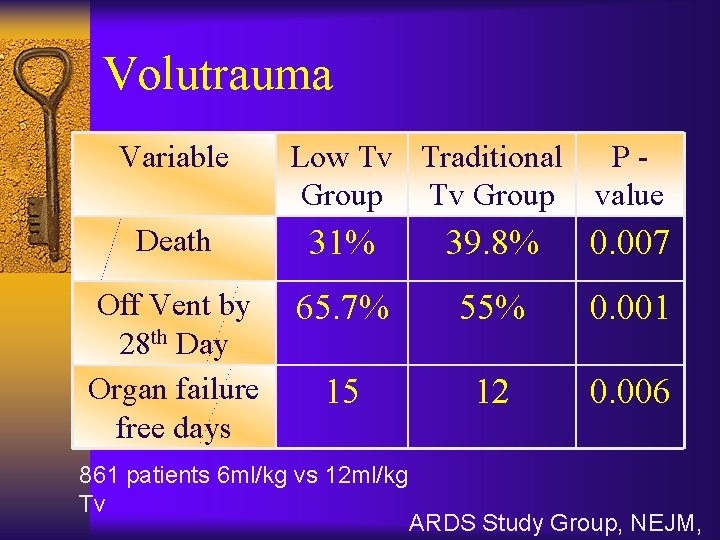
Volutrauma Variable Low Tv Traditional Group Tv Group Pvalue Death 31% 39. 8% 0. 007 Off Vent by 28 th Day Organ failure free days 65. 7% 55% 0. 001 15 12 0. 006 861 patients 6 ml/kg vs 12 ml/kg Tv ARDS Study Group, NEJM,
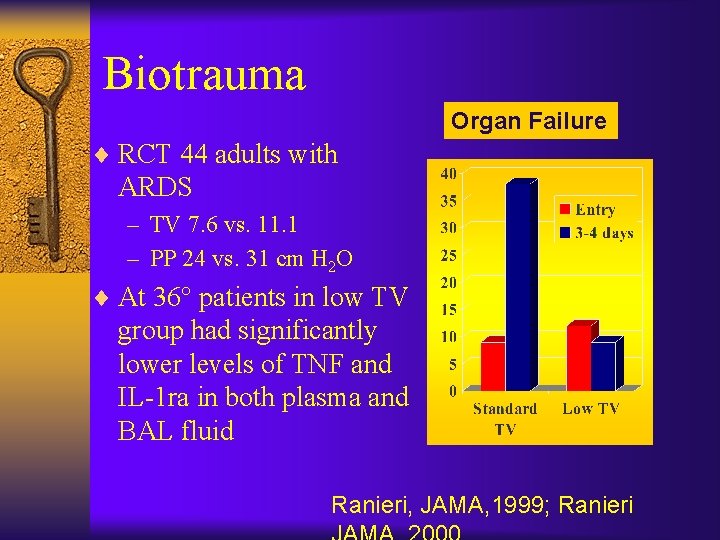
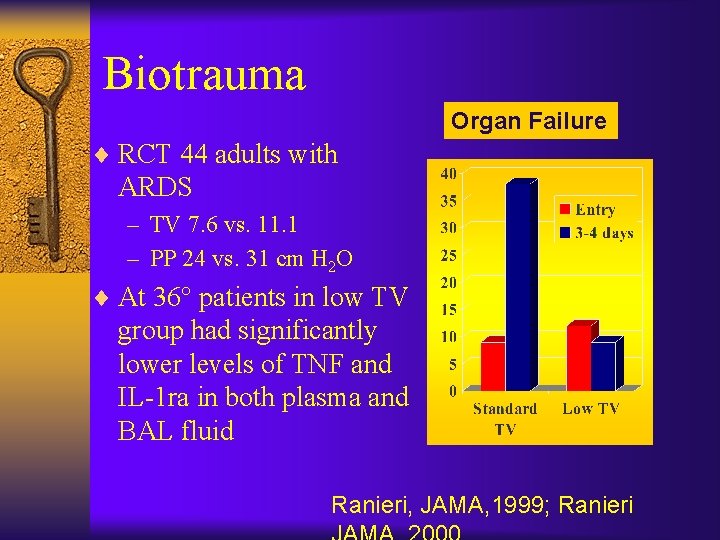
Biotrauma Organ Failure ¨ RCT 44 adults with ARDS – TV 7. 6 vs. 11. 1 – PP 24 vs. 31 cm H 2 O ¨ At 36° patients in low TV group had significantly lower levels of TNF and IL-1 ra in both plasma and BAL fluid Ranieri, JAMA, 1999; Ranieri
Special situations III ¨ Head Trauma – Avoid Hypercarbia (PCO 2 < 35) – Avoid Hypoxemia – PEEP may adversely effect venous return and ICP – Coughing/gagging extremely bad (Use paralytics)
Special situations IV ¨ HFOV Indications – ARHF with OI > 13 for 6 hours – Contraindicated in High airway resistance, ICP, unstable hemodynamics ¨ Part of an Open lung strategy with Mean airway pressure and Tv < dead space
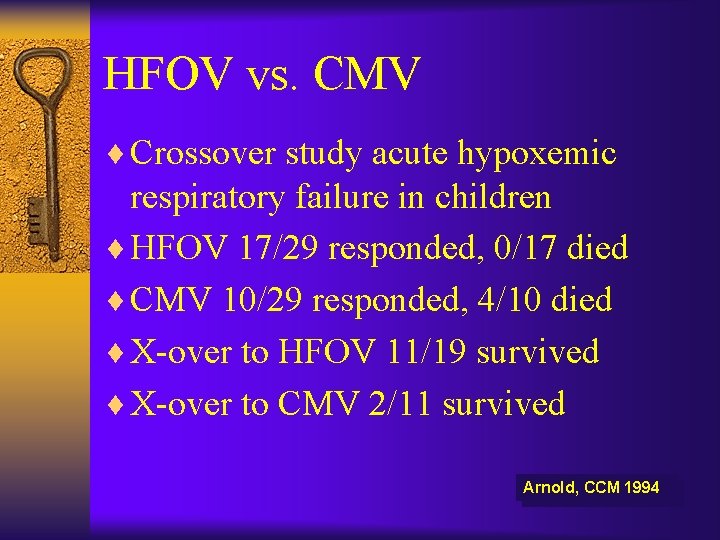
HFOV vs. CMV ¨ Crossover study acute hypoxemic respiratory failure in children ¨ HFOV 17/29 responded, 0/17 died ¨ CMV 10/29 responded, 4/10 died ¨ X-over to HFOV 11/19 survived ¨ X-over to CMV 2/11 survived Arnold, CCM 1994
Ventilation Simulator ¨ Not for the weak of heart
The End Mind what you have learned. Save you it can.
Questions?
 Kevin creamer
Kevin creamer Night float survival guide
Night float survival guide Plan prodaje primer
Plan prodaje primer Cs6410
Cs6410 Kevin gensler
Kevin gensler Kevin mayo
Kevin mayo Zita wallace letter to kevin rudd
Zita wallace letter to kevin rudd Kevin lui
Kevin lui National robotics initiative
National robotics initiative Adcb cash deposit machine in alain
Adcb cash deposit machine in alain Kevin tunstall
Kevin tunstall Kevin o'malley illustrator
Kevin o'malley illustrator Kevin lawler
Kevin lawler Kevin schwendemann
Kevin schwendemann Kevin salcido asu
Kevin salcido asu Kevin fadum
Kevin fadum Kevin forsythe
Kevin forsythe Kevin bekkers
Kevin bekkers Gcu chancellor scholarship
Gcu chancellor scholarship Photojournalism code of ethics
Photojournalism code of ethics Kevin buckman
Kevin buckman Kevin bao
Kevin bao Kevin liu attorney
Kevin liu attorney Kevin svetlitski
Kevin svetlitski Kevin uart
Kevin uart Kevin choi md
Kevin choi md Kevin ferland
Kevin ferland Kevin lusk
Kevin lusk Kevin horn medical examiner
Kevin horn medical examiner Kevin seqniqi
Kevin seqniqi Ear specially designed
Ear specially designed Recfe
Recfe Andrew pryfogle
Andrew pryfogle Kevin parker drum kit
Kevin parker drum kit Gloucestershire mash
Gloucestershire mash Paul shumate
Paul shumate Kevin powderly
Kevin powderly Cos423
Cos423 Kevin maruno
Kevin maruno Kevin lee yates coos bay oregon
Kevin lee yates coos bay oregon Kevin suitor
Kevin suitor Hanti lin
Hanti lin Kevin buchin
Kevin buchin Kevin cowtan
Kevin cowtan Kevin zbuk
Kevin zbuk Kevin baity
Kevin baity Dr kevin mulcahy
Dr kevin mulcahy The cockroach by kevin halligan
The cockroach by kevin halligan Kevin grittner
Kevin grittner The sound of silence alfredo jaar
The sound of silence alfredo jaar Agilent erp
Agilent erp