Pharmacology and the NursePatient Relationship The Nursing Process






- Slides: 29
Pharmacology and the Nurse-Patient Relationship The Nursing Process in Pharmacology Prepared by I Gede Purnawinadi, S. Kep. , M. Kes.
The nursing process is a systematic method of problem solving that forms the foundation of nursing practice. The use of the nursing process is particularly important for patients receiving medications. By using the phases of the nursing process, the nurse can ensure that the interdisciplinary practice of pharmacology results in safe, effective, and individualized medication administration outcomes for patients under their care.
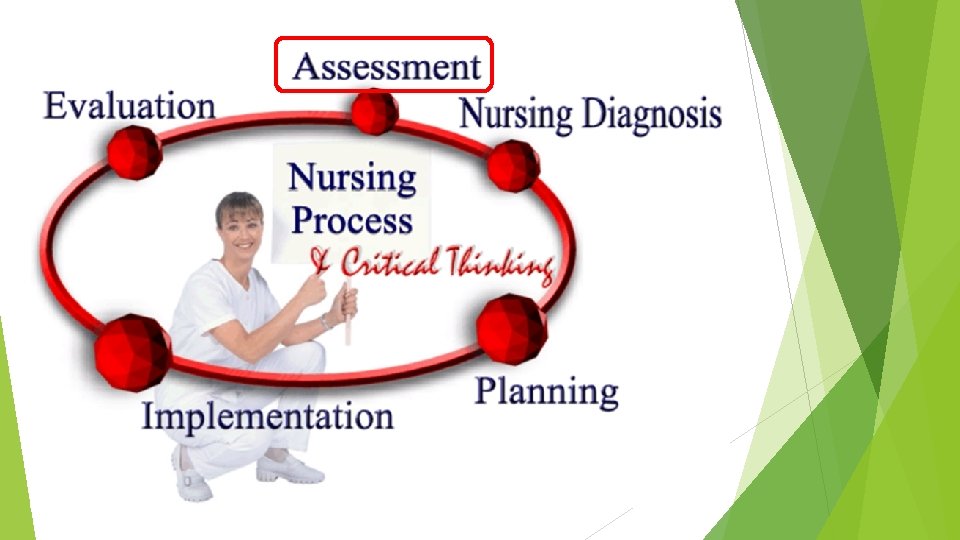
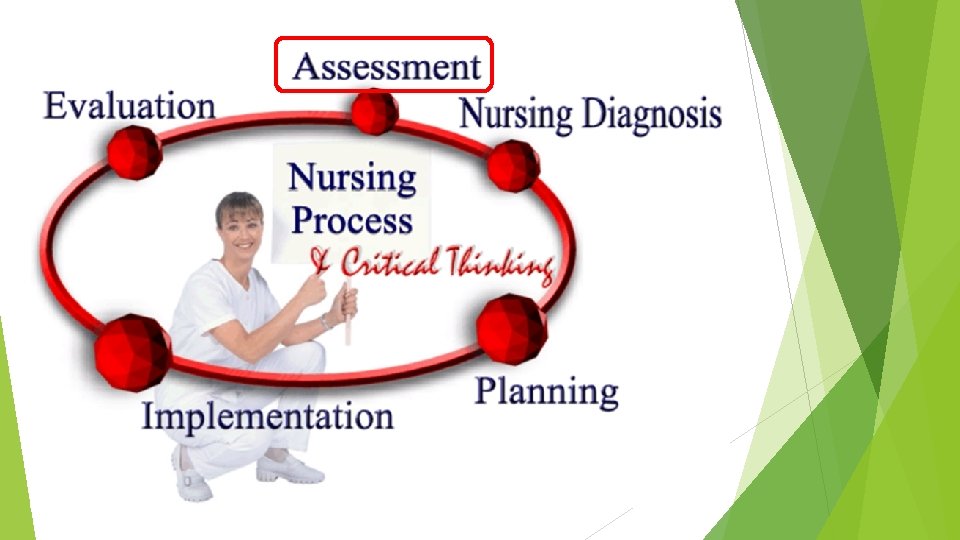
Overview of The Nursing Process The nursing process is a systematic method of problem solving that uses a nurse’s critical thinking skills to care for the patient. It is patient-centered, dynamic, and based on ongoing patient data and needs, and is a collaborative effort between the nurse, patient, and other members of the health care team. The nurse relies on knowledge, technical and critical thinking skills, and even creativity to work through the process of gathering assessment data, establishing nursing diagnoses, planning care with the patient to meet outcomes, implementing, and, finally, evaluating care. The nursing process is cyclical and each phase is related to all the others; they are not separate entities but overlap. For example, when a nurse is evaluating whether the pain medication given to the patient has had therapeutic effects and relieved the pain, the nurse relies on assessment skills to evaluate whether the patient is pain-free or has obtained some relief from the drug.
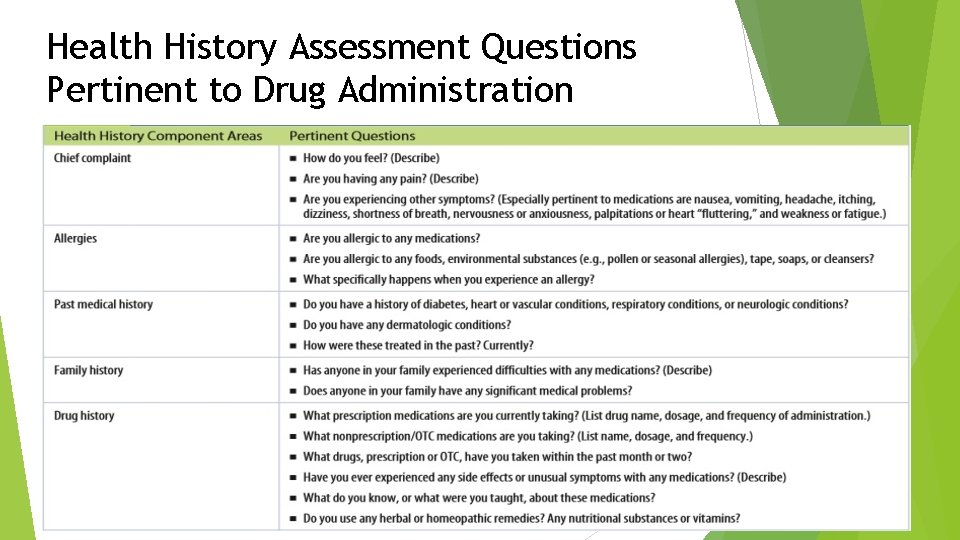
Key Concepts Assessment is the systematic collection of patient data. Assessment of the patient receiving medications includes health history information, physical assessment data, laboratory values and other measurable data, and an assessment of medication effects, including both therapeutic and side effects. Assessment is an ongoing process that begins with the nurse’s initial contact with the patient and continues with every interaction thereafter. Assessment consists of gathering subjective data, which include what the patient says or perceives, and objective data gathered through physical assessment, laboratory tests, and other diagnostic sources.
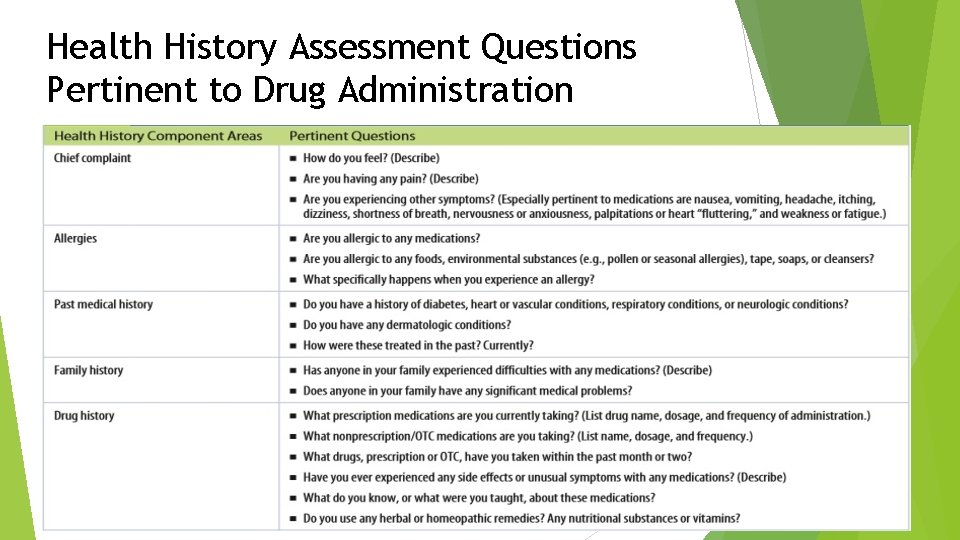
Health History Assessment Questions Pertinent to Drug Administration
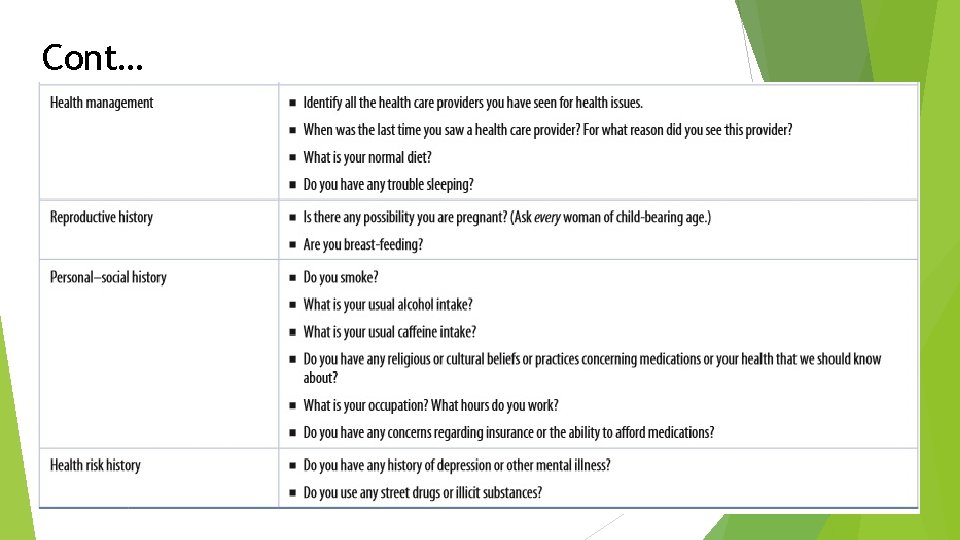
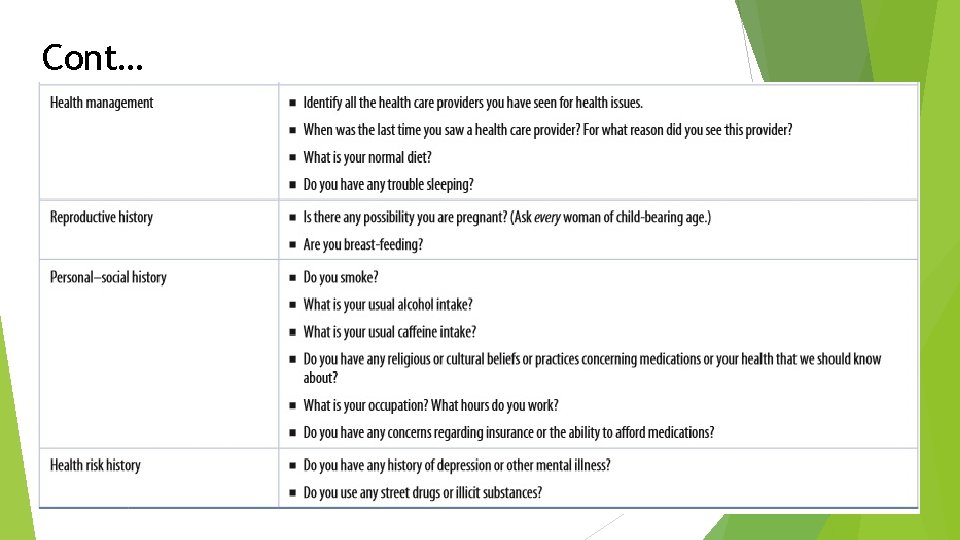
Cont…

Key Concepts Nursing diagnoses are written to address the patient’s responses related to drug administration. Nursing diagnoses are clinical judgments of a patient’s actual or potential health problem that is within the nurse’s scope of practice to address. They are developed after an analysis of the assessment data, are focused on the patient’s problems, and are verified with the patient or caregiver. Unlike medical diagnoses that focus on a disease or condition, nursing diagnoses focus on a patient’s response to actual or potential health and life processes.
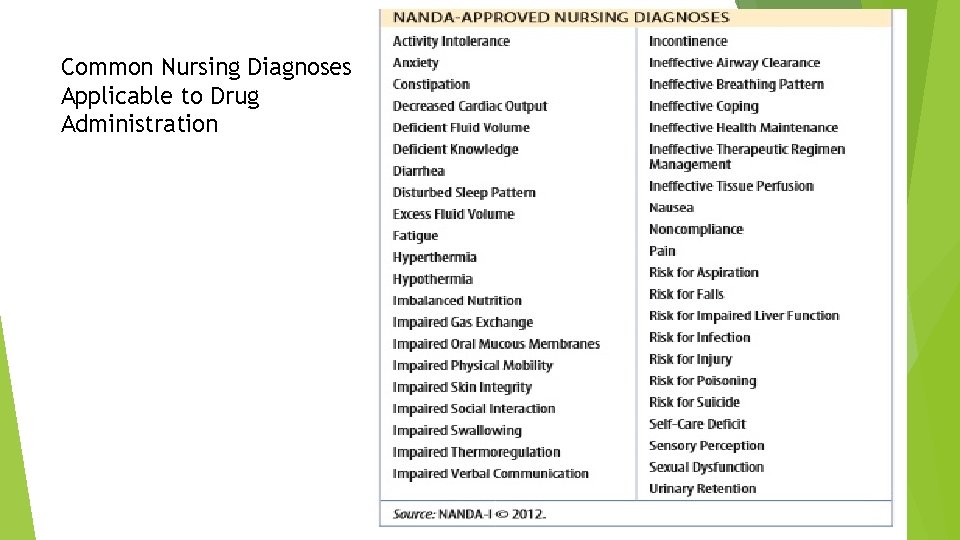
The North American Nursing Diagnosis Association (NANDA) defines nursing diagnoses as: A clinical judgment about individual, family, or community responses to actual or potential health/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable (NANDA-I © 2012). When applied to pharmacotherapy, the diagnosis phase of the nursing process addresses three main areas of concern: 1. Promoting therapeutic drug effects. 2. Minimizing adverse drug effects and toxicity. 3. Maximizing the ability of the patient for self-care, including the knowledge, skills, and resources necessary for safe and effective drug administration.
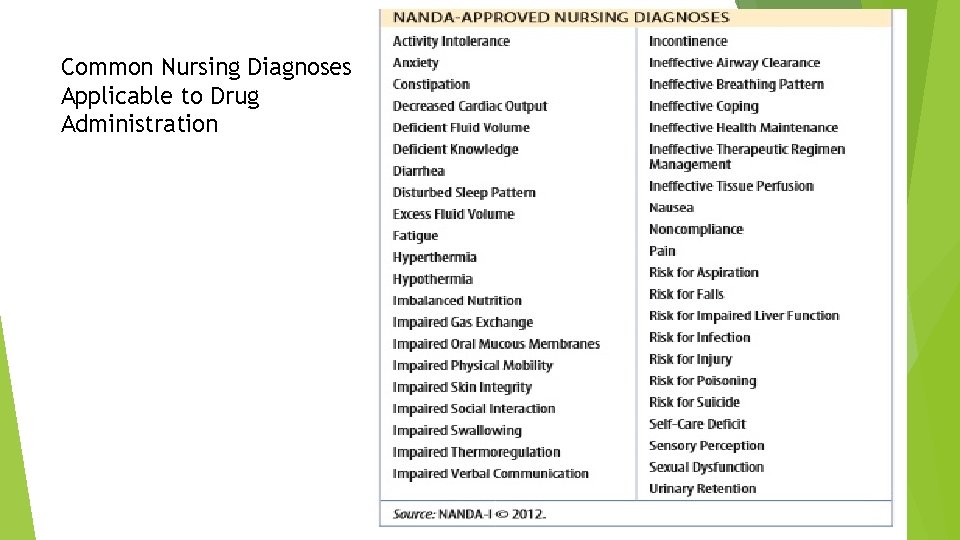
Common Nursing Diagnoses Applicable to Drug Administration

Key Concepts Goals and outcomes, which are developed from the nursing diagnoses, direct the interventions required by the plan of care. Goals focus on what the patient should be able to achieve, and outcomes provide the specific, measurable criteria that will be used to measure goal attainment. Short- or long-term goals are established that focus on what the patient will be able to do or achieve, not what the nurse will do.
Outcomes are the specific criteria used to measure attainment of the selected goals. They are written to include the subject (usually the patient), the actions required by that subject, under what circumstances, the expected performance, and the specific time frame in which the subject will accomplish that performance. In the example of the patient who will be taught to self-administer anticoagulant therapy at home, an outcome may be written as: “Patient will demonstrate the injection of enoxaparin (Lovenox) using the preloaded syringe provided, given subcutaneously into the anterior abdominal areas, in 2 days (1 day prior to discharge). ” This outcome includes the subject (patient), actions (demonstrate injection), circumstances (using a preloaded syringe), performance (SC injection into the abdomen), and time frame (2 days from now— 1 day before discharge home). Writing specific outcomes also gives the nurse a concrete time frame to work toward assisting the patient to meet the goals.
Before administering medications, the nurse should establish clear, realistic goals and outcomes so that planned interventions ensure safe and effective use of these drugs. The nurse establishes priorities based on the assessment data and nursing diagnoses, with high-priority needs addressed before low-priority needs. The goals and outcomes identified in the plan of care will assist the nurse, and other health care providers, in implementing interventions and evaluating the effectiveness of that care.

Key Concepts The implementation phase involves administering the drug and carrying out interventions to promote a therapeutic response and minimize adverse effects of the drug. The implementation phase is when the nurse applies the knowledge, skills, and principles of nursing care to help move the patient toward the desired goal and optimal wellness. Implementation involves action on the part of the nurse or patient: administering a drug, monitoring drug effects, providing patient teaching, and initiating other specific actions identified by the plan of care. Key interventions required of the nurse in the implementation phase include, documenting medications.
Patient Education Patient teaching is a vital component of the nurse’s interventions for a patient receiving medications. Knowledge deficit are directly related to the type and quality of medication education that a patient receives. Every nurse–patient interaction can present an opportunity for teaching. Discussing medications each time they are administered is an effective way to increase the amount of education accomplished.


Key Concepts The evaluation phase of the nursing process compares the patient’s current health status with the desired outcome. This step is important to determine if the plan of care is appropriate, if it was met, or if it needs revision. Nursing diagnoses are reviewed or rewritten, goals and outcomes are refined, and new interventions are carried out. If it was met, the plan of care was appropriate, and the problem or risk was resolved. The nurse and patients can then address the next highest priority health need. If the goal was partially met, the patient is moving toward the goal, but the nurse may need to continue interventions for a longer time, or somehow modify interventions to completely resolve the problem.

Medication Errors and Risk Reduction In clinical practice, the nurse maximizes patient safety by striving to be 100% accurate when administering medications. Drug administration, however, requires multiple complex steps by health care providers, pharmacists, nurses, and patients and can never be 100% error-free. Occasionally medication errors are made that can significantly affect treatment outcomes. The purpose of this chapter is to examine the reasons for medication errors and explore strategies the nurse may use to prevent them.
Medication Errors According to the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP), a medication error is “any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. ”
Medication Errors A medication error may be related to misinterpretations, miscalculations, misadministrations, handwriting misinterpretation, and misunderstanding of verbal or phone orders. Whether the patient is injured or not, it is still a medication error. The nurse is legally and ethically responsible for reporting medication errors—whether or not they cause harm to a patient—in the patient’s medical record and on an incident report. Nurse practice acts define professional nursing, including safe medication delivery. Standards of care defined by nurse practice acts and the rule of reasonable and prudent action.
Medication Errors The most frequent types of drug errors vary depending on the specific population (e. g. , pediatrics versus geriatrics) or health care unit (e. g. , intensive care versus long-term care). The most common types of errors usually involve administering an improper dose, giving the wrong drug, and using the wrong route of administration.
Reducing Medication Errors Practice the rights of medication administration: right patient, right time and frequency of administration, right dose, right route of administration, right drug, and right documentation. Keep the following steps in mind as well: 1. Positively verify the identity of each patient using two means (e. g. , name and birth date) before administering the medication according to facility policy and procedures. 2. Use the correct procedures and techniques for all routes of administration. Use sterile materials and aseptic techniques when administering parenteral or eye medication. 3. Calculate medication doses correctly and measure liquid drugs carefully. 4. Always confirm that the patient has swallowed the medication. Never leave the medication at the bedside unless there is a specific order that medications may be left there. 5. Record the medication on the MAR immediately after administration.
To minimize the potential for medication errors, the nurse should teach the patients or home caregivers the following: 1. Know the names of all medications they are taking, the uses, the doses, and when and how they should be taken. 2. Know what side effects need to be reported immediately. 3. Read the label prior to each drug administration and use the medication device that comes with liquid medications rather than household measuring spoons. 4. Carry a list of all medications, including drugs, as well as herbal and dietary supplements that are being taken. If possible, use one pharmacy for all prescriptions. 5. Ask questions. Health care providers want to be partners in maintaining safe medication principles.
Chapter Test
 Nursing process introduction
Nursing process introduction Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Venipuncture for radiologic technologists
Venipuncture for radiologic technologists Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Toxicology and applied pharmacology
Toxicology and applied pharmacology Annual review of pharmacology and toxicology
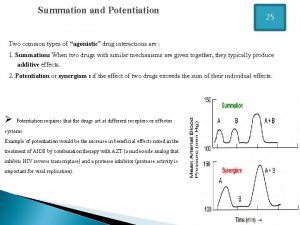
Annual review of pharmacology and toxicology Potentiation example
Potentiation example Rate of elimination of drug
Rate of elimination of drug What is ion trapping in pharmacology
What is ion trapping in pharmacology Factors affecting drug metabolism
Factors affecting drug metabolism Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology Ion trapping
Ion trapping Alia drug testing
Alia drug testing Drug excretion
Drug excretion First pass effect in pharmacology
First pass effect in pharmacology Mechanism of drug action
Mechanism of drug action First pass effect in pharmacology
First pass effect in pharmacology Alpha 1 vs alpha 2 receptors
Alpha 1 vs alpha 2 receptors What is pharmacology
What is pharmacology Pharmacology introduction
Pharmacology introduction Competitive antagonist
Competitive antagonist What is ion trapping in pharmacology
What is ion trapping in pharmacology What is pharmacology
What is pharmacology Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Respiratory pharmacology quiz
Respiratory pharmacology quiz Pharmacology module
Pharmacology module Hepatic extraction ratio
Hepatic extraction ratio Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Pharmacology of drugs acting on respiratory system
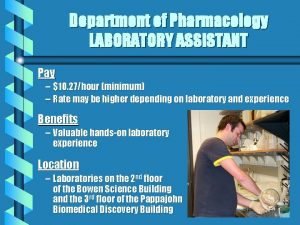
Pharmacology of drugs acting on respiratory system Pharmacology pay
Pharmacology pay