Peripheral Vascular System Assessment Overview of Peripheral Vascular





- Slides: 24
Peripheral Vascular System Assessment
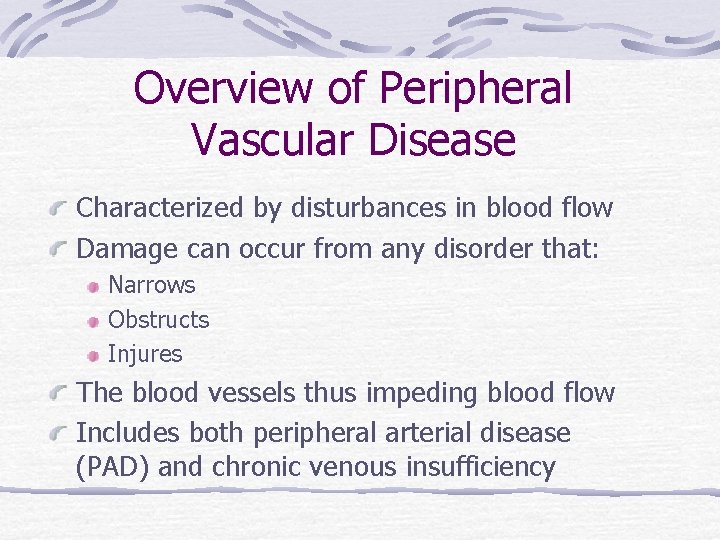
Overview of Peripheral Vascular Disease Characterized by disturbances in blood flow Damage can occur from any disorder that: Narrows Obstructs Injures The blood vessels thus impeding blood flow Includes both peripheral arterial disease (PAD) and chronic venous insufficiency
Peripheral Arterial Disease Can effect any part of vascular system Can manifest as acute or chronic condition Causes of decreased arterial blood flow Atherosclerosis or Spasm Embolism or thrombus Hypotension or Hypercoagulability Trauma Compartment syndrome Risk factors are same as all cardiovascular disease
Peripheral Arterial Disease Also referred to as: PVD 1) Chronic, progressive, arterial narrowing 2) Reduced blood supply resulting in ischemia 02 needs exceed supply, areas of ischemia & ultimately necrosis will develop Symptoms are manifested based on the extent to which tissues are deprived of 02 The ability of the vascular system to develop collateral circulation will have an effect on the development of clinical symptoms
Intermittent Claudication Aching pain or cramping sensation that occurs in the muscle distal to the occlusion that occurs with activity and disappears with rest Due to inadequate oxygenation. Similar to angina, predictable and reproducible. May escalate into rest ischemia or pain (urgent attention needed)
Intermittent Claudication Rest ischemia May be accompanied by coldness and/or paresthesias May be aggravated by elevation of extremities Gravity improves perfusion and decreases symptoms
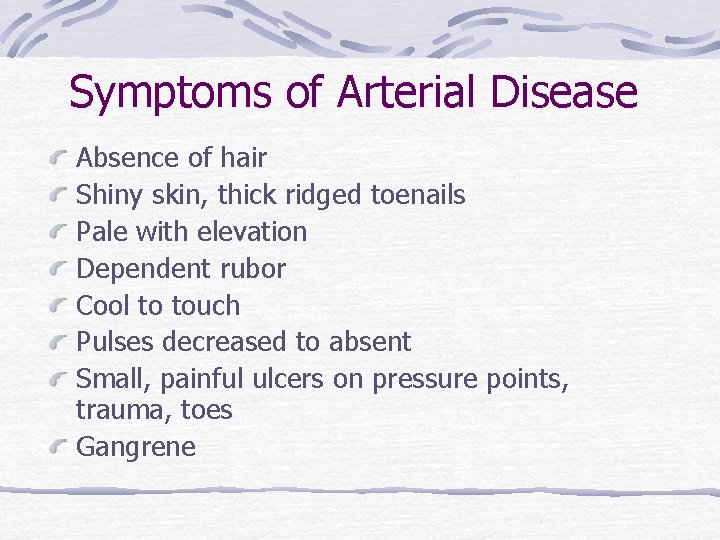
Symptoms of Arterial Disease Absence of hair Shiny skin, thick ridged toenails Pale with elevation Dependent rubor Cool to touch Pulses decreased to absent Small, painful ulcers on pressure points, trauma, toes Gangrene


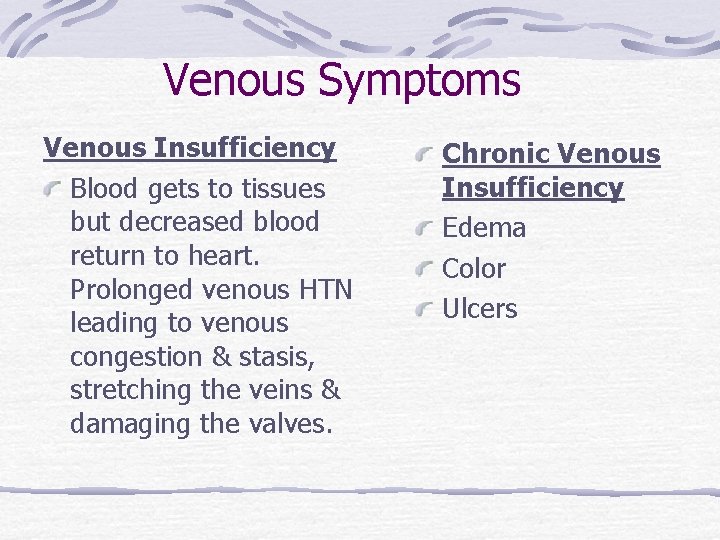
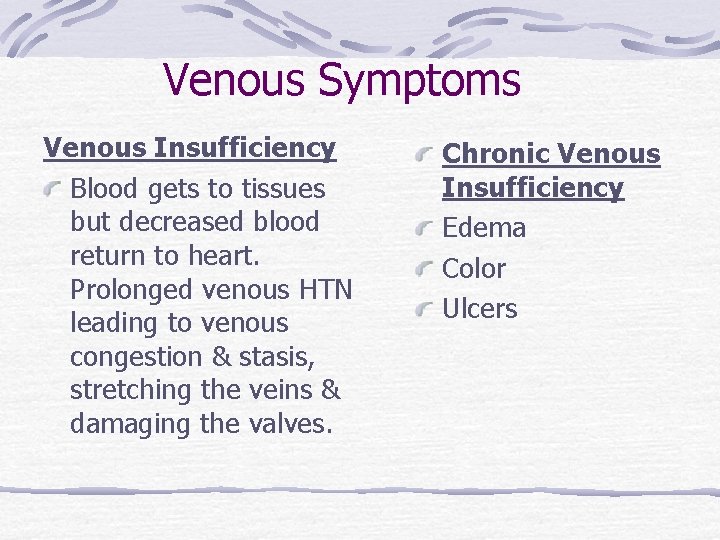
Venous Symptoms Venous Insufficiency Blood gets to tissues but decreased blood return to heart. Prolonged venous HTN leading to venous congestion & stasis, stretching the veins & damaging the valves. Chronic Venous Insufficiency Edema Color Ulcers
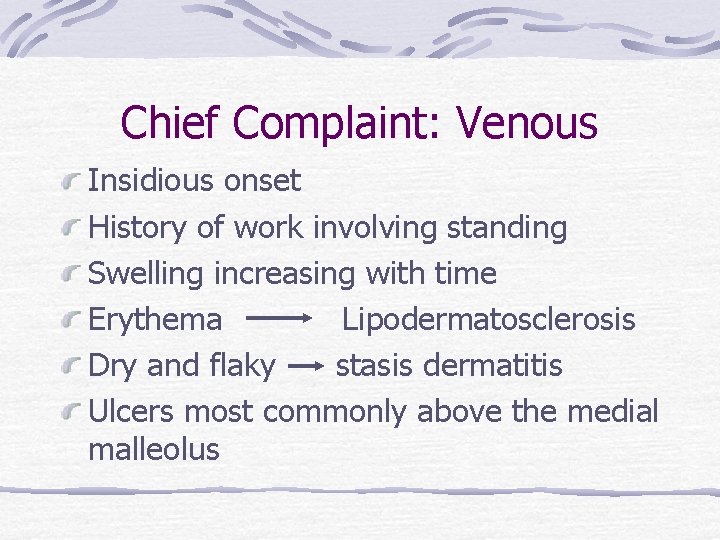
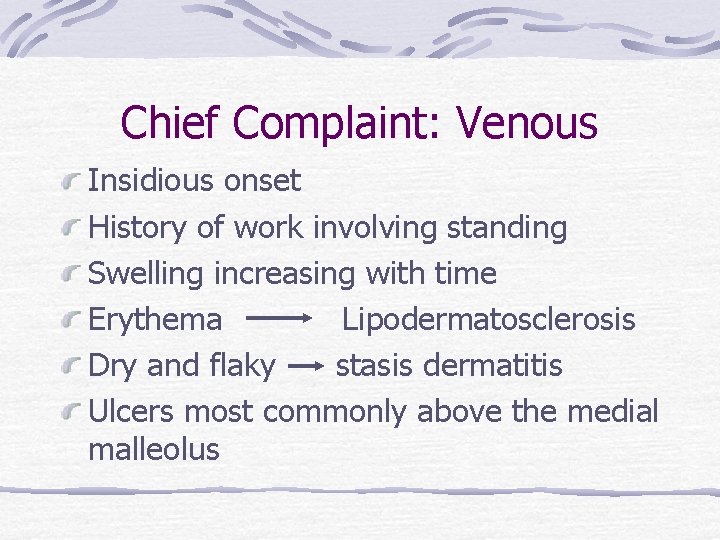
Chief Complaint: Venous Insidious onset History of work involving standing Swelling increasing with time Erythema Lipodermatosclerosis Dry and flaky stasis dermatitis Ulcers most commonly above the medial malleolus

Examples of Venous Disease
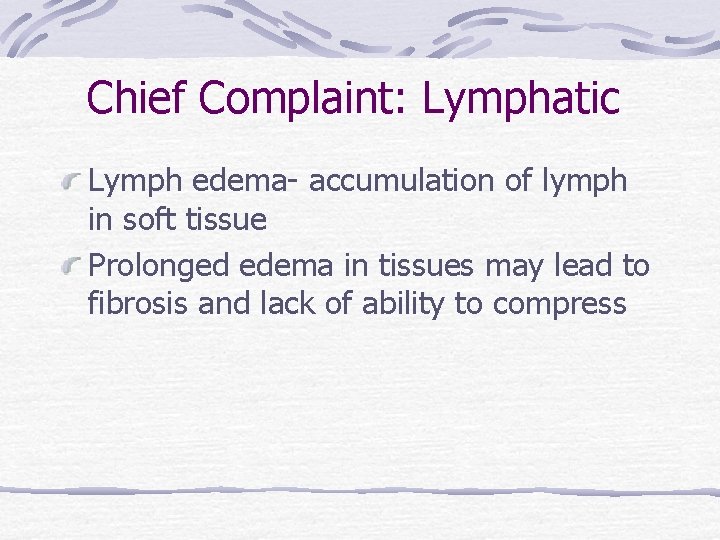
Chief Complaint: Lymphatic Lymph edema- accumulation of lymph in soft tissue Prolonged edema in tissues may lead to fibrosis and lack of ability to compress

Massive Lymphedema
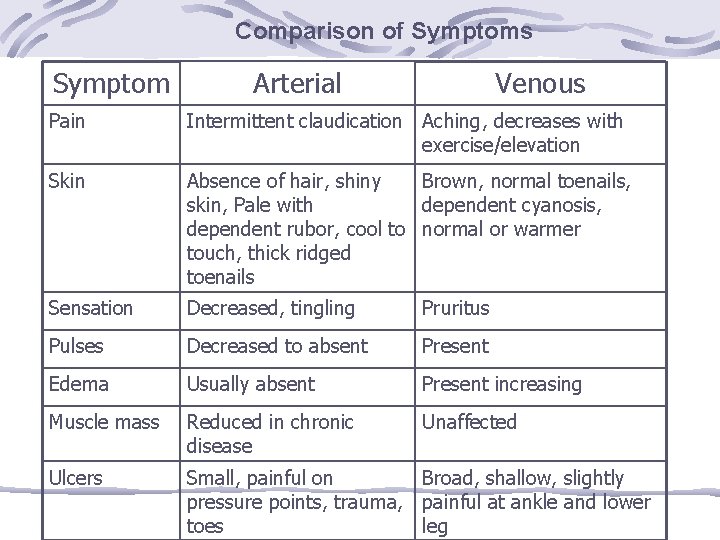
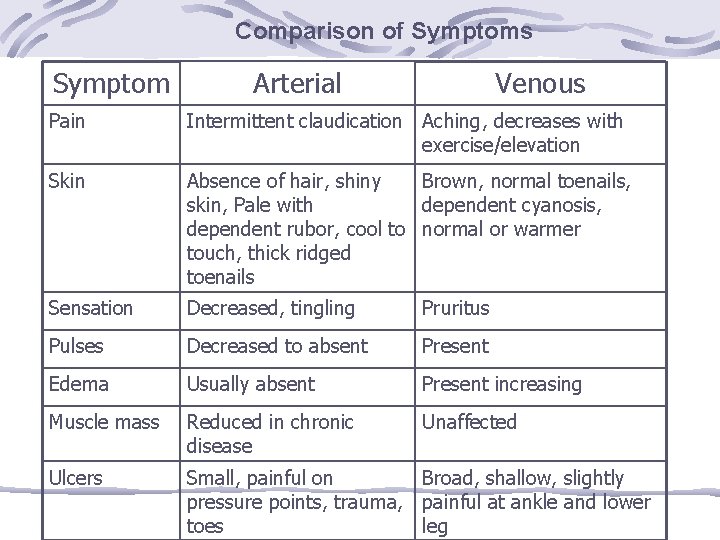
Comparison of Symptoms Symptom Arterial Venous Pain Intermittent claudication Aching, decreases with exercise/elevation Skin Absence of hair, shiny Brown, normal toenails, skin, Pale with dependent cyanosis, dependent rubor, cool to normal or warmer touch, thick ridged toenails Sensation Decreased, tingling Pruritus Pulses Decreased to absent Present Edema Usually absent Present increasing Muscle mass Reduced in chronic disease Unaffected Ulcers Small, painful on Broad, shallow, slightly pressure points, trauma, painful at ankle and lower toes leg
Physical Assessment: Inspection Skin color – pallor, rubor, cyanosis Hair distribution Nail beds Capillary refill Muscle atrophy Edema Ulcers
Physical Assessment: Palpation Temperature Pulses Allen’s test Homan’s sign - unreliable
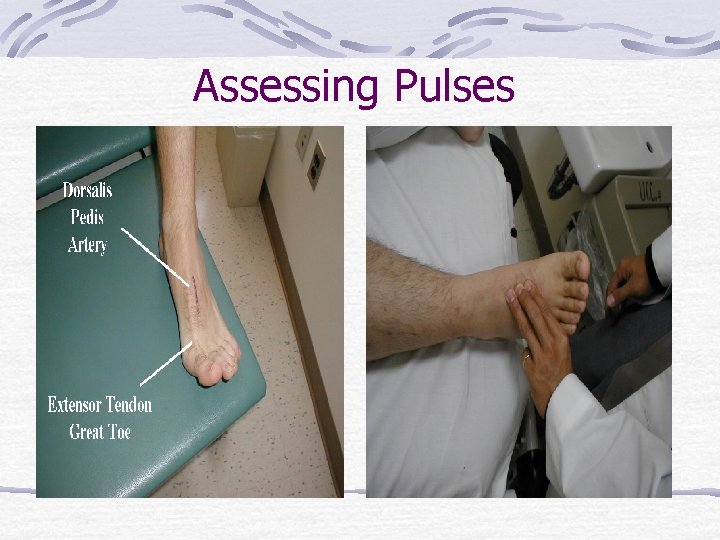
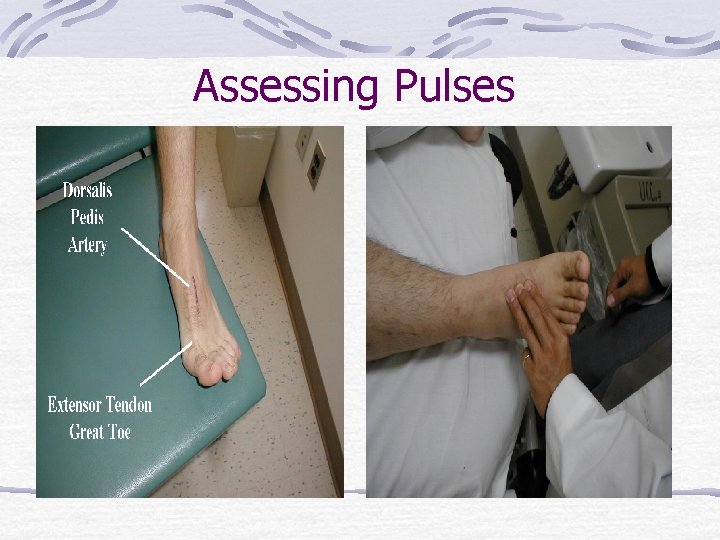
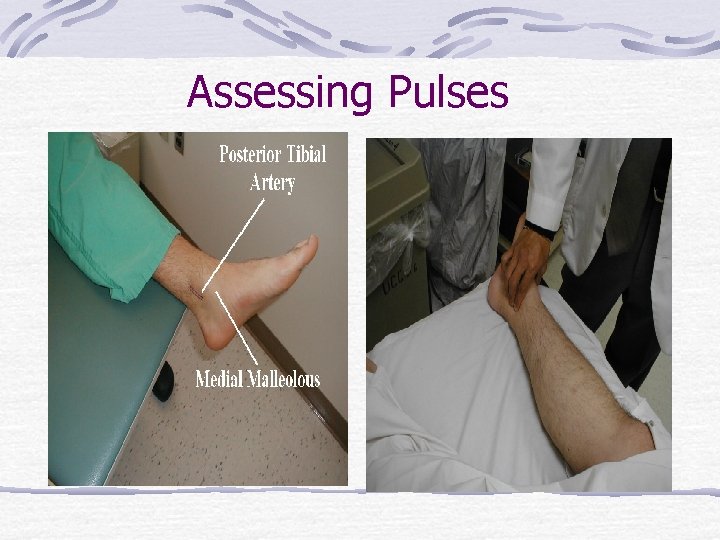
Assessing Pulses
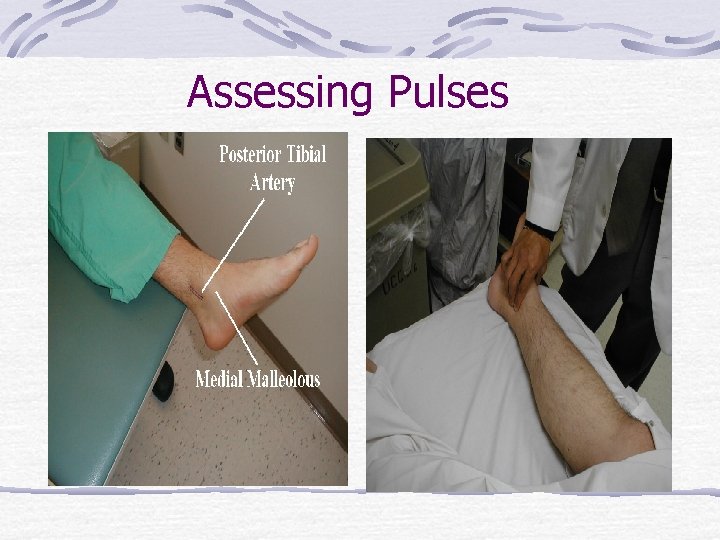
Assessing Pulses
Physical Assessment: Ausculation Limb blood pressure Single best indicator of arterial perfusion Bruits – whooshing sound from turbulent blood flow from vessel wall abnormalities Carotid, aorta, renal, femoral, popliteal
Diagnostic Tests: Non-Invasive Doppler ultrasound – audible arterial signals and measurement of limb pressures B Mode (Brightness Mode)Ultrasound – 2 dimensional image: size, compressibility, thrombus and valve functions Ankle-Brachial index – Equation using pressures obtained from cuffs Image exams – CT scan, MRI
Diagnostic Tests: Invasive Angiography – most invasive and highest risk to client. Usually done prior to surgical intervention Involves injecting contrast agent into an arterial system and obtaining radiological pictures

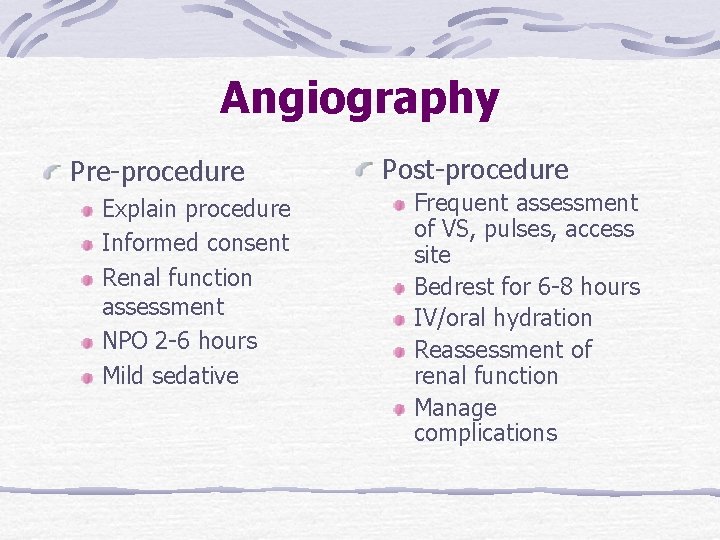
Angiography Pre-procedure Explain procedure Informed consent Renal function assessment NPO 2 -6 hours Mild sedative Post-procedure Frequent assessment of VS, pulses, access site Bedrest for 6 -8 hours IV/oral hydration Reassessment of renal function Manage complications
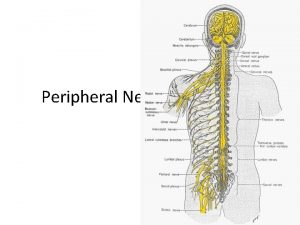
 Peripheral vascular system
Peripheral vascular system Non vascular plants
Non vascular plants Non vascular vs vascular plants
Non vascular vs vascular plants Vascular and non vascular difference
Vascular and non vascular difference Peripheral vascular disease slideshare
Peripheral vascular disease slideshare Vascular system
Vascular system Where is a starfish mouth located
Where is a starfish mouth located Erp 2 systems
Erp 2 systems Content management system introduction
Content management system introduction What are the advantages of computerized accounting
What are the advantages of computerized accounting Ductus parotideus
Ductus parotideus Crtd sap
Crtd sap Operating systems overview
Operating systems overview Fitness center management system
Fitness center management system Anatomy of the digestive system exercise 38
Anatomy of the digestive system exercise 38 Computer memory system overview
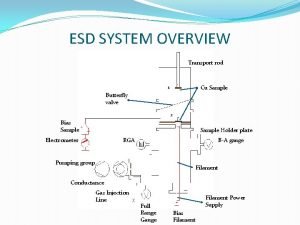
Computer memory system overview Computer memory system overview
Computer memory system overview British school system
British school system Chapter 2 an overview of the financial system
Chapter 2 an overview of the financial system British school system overview
British school system overview System analysis
System analysis System design overview
System design overview System overview sample
System overview sample Solar system overview
Solar system overview 3 lobes lung
3 lobes lung