Our Children Their Future Our Vision Worster Drought




- Slides: 21

Our Children, Their Future, Our Vision
Worster Drought Syndrome Case Studies Hannah Essex and Debra Collins Speech and Language Therapists
What is Worster Drought Syndrome? • Worster-Drought syndrome (WDS) is a type of cerebral palsy (movement disorder) that affects the muscles around the mouth and throat. It is also known as Congenital Suprabulbar paresis, This is a permanent movement disorder of the bulbar muscles causing persistent difficulties with swallowing, feeding, talking, saliva management. As well as other actions controlled by these muscles, such as coughing, nose-blowing, kissing and crying. • Children with WDS often have additional difficulties with co-ordination, learning, behaviour and epilepsy. 3
Neurology: What are the causes? • Worster-Drought syndrome is caused by damage to the perisylvian area of the brain, which controls the mouth and throat muscles, this abnormality occurs around weeks 12 to 16 of gestation. • The cause is thought to be connected to the blood supply to the perisylvian area, or due to genetic vulnerability. 4
Prognosis • As Worster drought syndrome affects the control of muscles, which are responsible for the movement of the lips, jaw, tongue, soft palate, and upper gullet. • Typical speech therapy is likely to only have a limited impact on speech clarity so alternative methods of communication should be considered. • Clarke et al (2000) reported that; • Children with Worster drought had significant bulbar difficulties of these 80% of children needed a modified diet and augmentative communication methods • 86% had dribbling, 60% had glue ear, gastro-oesophageal reflux in 40%, history of poor nutrition in 40% and aspiration in 40% 5 • The mean age of diagnosis was 6 years.
• Case study of 2 children and comparing differences in presentation and progress. • First child is age 4 y 4 m and the second child is 10 y 2 m 6
Case Study 1 Case History • Attended a Speech and language drop in session aged 2. • Concerns with lots of dribbling, repeatedly needing to change bibs. • Difficulties latching on the bottle (anterior loss) and difficulties with weaning. • Difficulties with chewing. • Parents had requested investigations into tongue-tie, no indication of this so discharged from ENT team. • Reduced clarity of speech, mainly using vowel sounds. • No history of chest infections, some ear infections noted. 7
• The child was sent directly to the dysphagia team for an assessment of his eating and drinking skills and placed on the waiting list for direct therapy. • At initial assessment of feeding • Due to age/shyness unable to copy any oral movements or open mouth for full assessment of structures. • Observations were: • -Drooling noticed at rest, wetting a bib and toys. • -Unable to blow through his mouth, nasal omission occurred when he attempted this. • • • Eating (sandwich, banana and yoghurt) Using his fingers to place food onto the back of tongue or side of mouth. Sucking to retrieve food from spoon Using lip smacking, sucking movements and some munching to prepare bolus. Lack of awareness of anterior loss. 8

• Drinking (thin fluid through a straw) • Using rhythmic sucking (with lip smacking motion) and breaks in between • Unable to maintain low pressure to keep fluid going up the straw or keep fluid in his mouth, anterior loss noticed. • *Audible gulping swallows heard during eating and drinking, however, no overt signs of aspiration. • Summary and Next Steps • Child presented with oral phase difficulties due to reduced oral motor function. However he had developed his own strategies to compensate for very limited / absence tongue movements. • -Child was referred to the paediatrician for a neurodevelopmental assessment. Then to tertiary consultant neurologist to confirm diagnosis. • Diagnosis • -Worster drought syndrome with bulbar dysfunction and recent imaging demonstrating bilateral perisylvian polymicrogyria. • As bilateral perisylvian polymicrogyria was noted on MRI imaging, this increased his risk of developing epilepsy. 9
Video of current feeding skills. Area’s of difficulty reported and observed: Ø Increase in number of choking incidences at home and in school Ø food becoming compacted on hard palate ØPoor co-ordination of movements ØInconsistent jaw excursion ØSeverely reduced clarity of speech. ØFollowing this assessment, a referral is being made for a videofluoroscopy for further assessment to establishing safe & manageable consistencies. 10
Progress: • Communication: Now attends a resource unit. Using a communication book effectively, linking 3 plus words to request and inform. Also using signing to support communication. Family are very proactive in working on alternative communication. There has been limited progress with his speech sound production. • Feeding -Child is now on Trihexyphendyl medication due to his excess saliva. This had a small impact so far and the amount is slowly being increased. -chewing skills have shown some improvements, more jaw movement and rotary chew observed than on previous assessment. Hard chew consistencies remain more challenging. -Focus has also been on developing his lip seal when drinking as previously a lot of anterior loss occurred. 11
Case Study 2 • Referred to Speech and language therapy on going therapy for speech sound difficulties from age 3. Oral dyspraxia considered. Parents did not report chest infections or respiratory difficulties. • Raised to feeding team at age 8. Long history of multiple allergies and frequent chest infections requiring antibiotics and hospital admission. His respiratory consultant referred to tertiary Speech and language services for a videofluoroscopy. Case History • Maternal history of swallowing difficulties and speech sound production, which she grew out of. Lots of familial history of speech sound difficulties. • 25 admissions to hospital for respiratory illnesses • Persistent bacterial bronchitis • Lower respiratory tract infections associated with hypoxia. • Suspected Reflux after transitioning to bottle feeding at 3 months, however, this turned out to be an egg allergy. • Weaned well initially on to a chopped adult diet, however, continued to gag and vomit until age 5 years. • Dribbling, however, this had improved with age. • Attention and listening difficulties and speech sound difficulties despite a high level of input. 12
Initial assessment Oral motor assessment revealed: • Limited tongue movements; difficulty moving laterally, protruding and elevating. • Difficulty co-ordinating tongue movements. • Open mouth posture when eating. Some anterior loss of food little awareness observed. Feeding assessment • Wet voice and cough immediately following suck, swallow bursts of milk (thin fluid). Swallow delayed so custard thick fluids suggested. • Throat clearing noticed when he was drinking. 13
Videofluoroscopy findings • Oral stage • Poor bolus control and formation of all consistencies. Bolus passively spilling over tongue base and entering the pharynx prior to swallow trigger. • Pharyngeal stage • Thin fluids and Syrup thick fluids; swallow triggered at pyriform sinuses and penetration occurred. Mild residue post swallow. • Custard thick fluids; swallows triggered as material entering the pyriform sinuses, swallow delayed, mild residue observed but not consistently cleared. • Recommendations • -Child should have custard thick fluids. Is at risk of aspiration due to delayed swallow and mild residue. 14
Progress at 10 years • Child is now managing better with bolus control and chewing, he remains at risk with bite and splinter/bite and crumble foods. • Due to numerous allergies is only able to tolerate one thickener brand, which he dislikes in water. • He is currently having naturally thickened drinks where possible and on occasion thin fluids. • Recommendations are unlikely to change so he is being managed closely by respiratory. 15
Diagnosis outcome • Both children present with very similar oral stage feeding difficulties. • Worster drought was confirmed in child one following neurological assessment by a specialist team; MRI scan revealed; clear bulbar dysfunction and bilteral perisylvian polymicrogyria. • Worster drought was very recently ruled out for child 2. No abnormalities revealed on MRI scan and no neurological indicators of WD. • -He has now been given a diagnosis of Developmental Coordination disorder (Dyspraxia) and Dysphagia by his paediatrician. 16
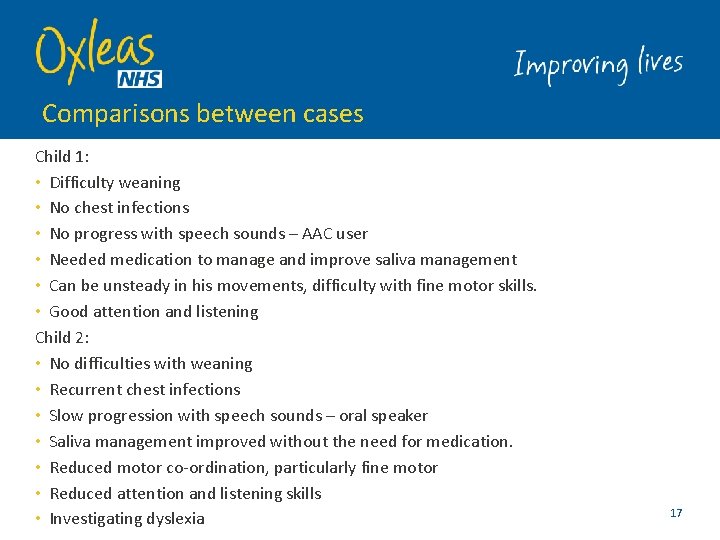
Comparisons between cases Child 1: • Difficulty weaning • No chest infections • No progress with speech sounds – AAC user • Needed medication to manage and improve saliva management • Can be unsteady in his movements, difficulty with fine motor skills. • Good attention and listening Child 2: • No difficulties with weaning • Recurrent chest infections • Slow progression with speech sounds – oral speaker • Saliva management improved without the need for medication. • Reduced motor co-ordination, particularly fine motor • Reduced attention and listening skills • Investigating dyslexia 17
• Both children are expected to have on going feeding difficulties 18
References • Worster-Drought syndrome, a mild tetraplegic perisylvian cerebral palsy. Review of 47 cases. Maria Clark, Lucinda Carr, Sheena Reilly*, Brian G. R. Neville. Brain (2000) 123, 2160 -2170 19

Any questions?

Thank you
 See future perfect
See future perfect Future continuous and future perfect
Future continuous and future perfect Our census our future
Our census our future Our census our future
Our census our future Our future is in our hands quotes
Our future is in our hands quotes Drought sentence for class 1
Drought sentence for class 1 Hong kong drought
Hong kong drought Concept of sustainable development
Concept of sustainable development Drought usaco
Drought usaco Drought presentation
Drought presentation Anasazi drought
Anasazi drought Conclusion on drought
Conclusion on drought Vermont drought monitor
Vermont drought monitor Utah drought map
Utah drought map Drought stopper system
Drought stopper system World, drought monitor
World, drought monitor Jordan drought
Jordan drought Drought present tense
Drought present tense Drought and desertification
Drought and desertification What are solutions of drought
What are solutions of drought Children are made readers on the laps of their parents
Children are made readers on the laps of their parents In go kiss the world the author s mother died in
In go kiss the world the author s mother died in