Optimizing Outcomes Digging Deeper into the Basic Tenets
Optimizing Outcomes Digging Deeper into the Basic Tenets
The Basic Tenets ü 1. Understanding the science behind the FOTO system 2. Standardizing Patient Instructions ü 3. Serial Status’ ü 4. High completion rates 5. Cognitive Behavioral Treatments
Validity – who’s job is it? The Researchers’ Job Our Job • • ü Participation Rates ü Completion Rates • Minimize Risk of Bias Content Validity Face Validity Structural Validity Construct Validity Measurement error Scaling Scoring Etc…etc. . . etc…. – What we say and do – What we don’t say and do
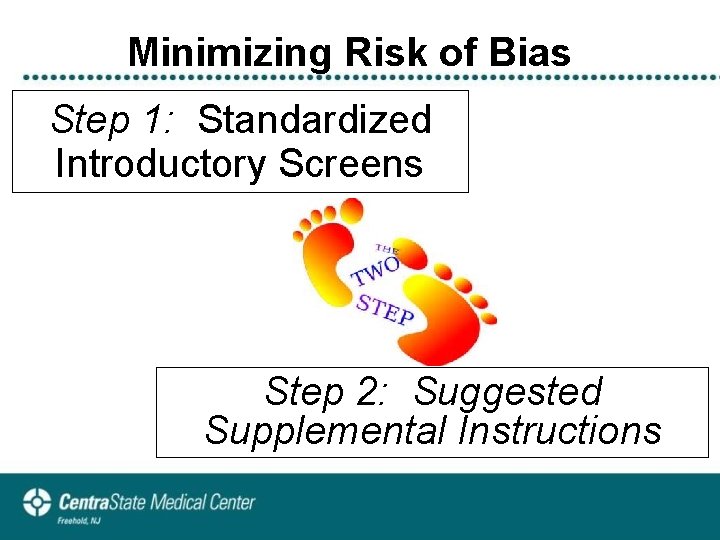
Minimizing Risk of Bias Step 1: Standardized Introductory Screens Step 2: Suggested Supplemental Instructions
Standardized Introduction Intake
Standardized Introduction Status
Minimizing Risk of Bias “How should I answer this? ” Avoid interpreting the questions for the patient.
Tips to Avoid Interpreting 1. 2. 3. Re-read Re-emphasize Objectively restate
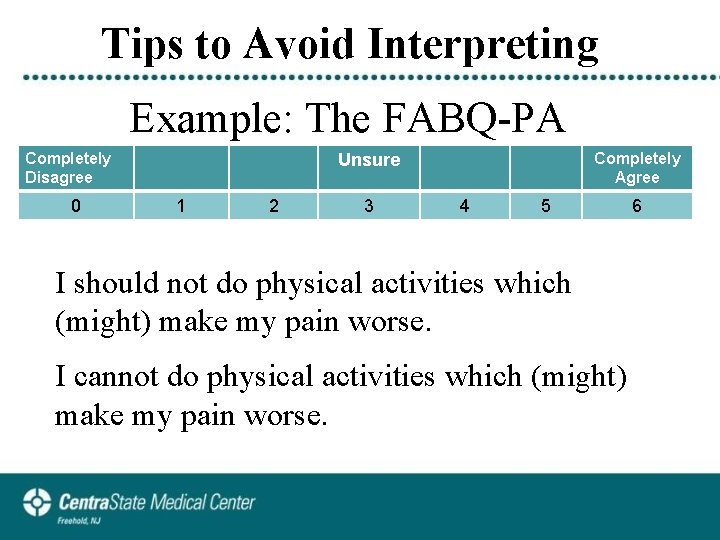
Tips to Avoid Interpreting Example: The FABQ-PA Completely Disagree 0 Completely Agree Unsure 1 2 3 4 5 6 I should not do physical activities which (might) make my pain worse. I cannot do physical activities which (might) make my pain worse.
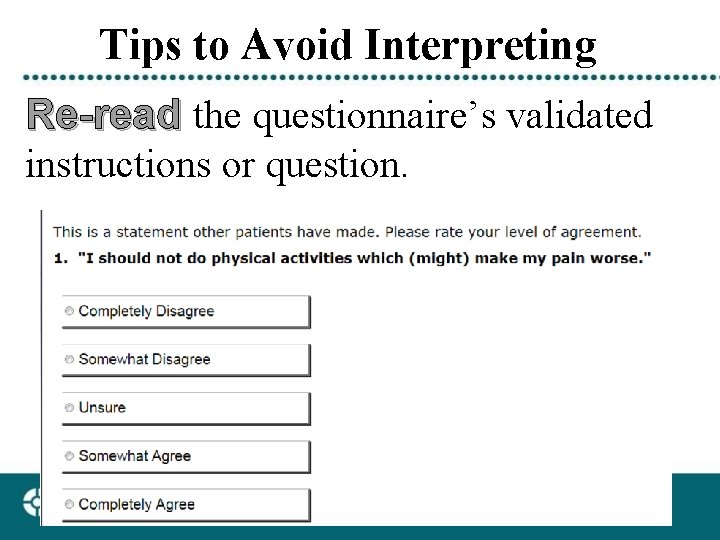
Tips to Avoid Interpreting Re-read the questionnaire’s validated instructions or question.
Tips to Avoid Interpreting Re-emphasize the questionnaire’s validated instructions or question “I should not do physical activities which (might) make my pain worse. ”
Tips to Avoid Interpreting Objectively re-state the questionnaire’s validated instructions or question. “Mr. Smith, how strongly do you agree or disagree with this statement: ‘I should not do physical activities which (might) make my pain worse. ’”
Reasons to Actively Help the Patient Proxy Recorder • Cognition • Under age 8 • Hand motor control • Language • Reading level
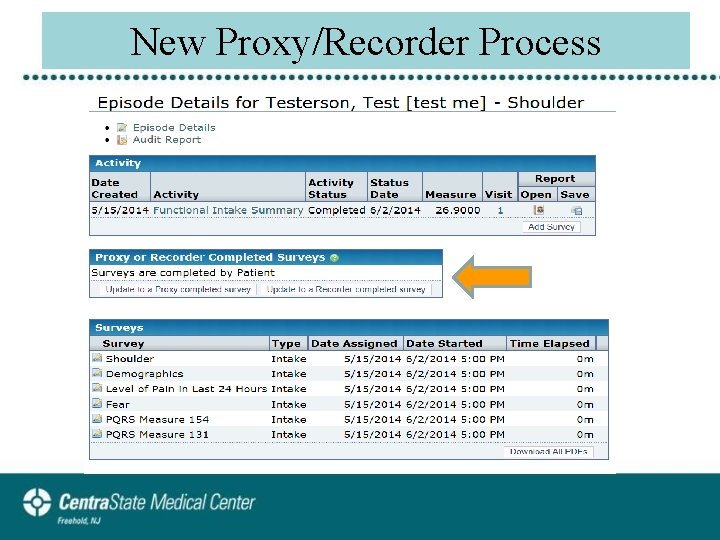
New Proxy/Recorder Process
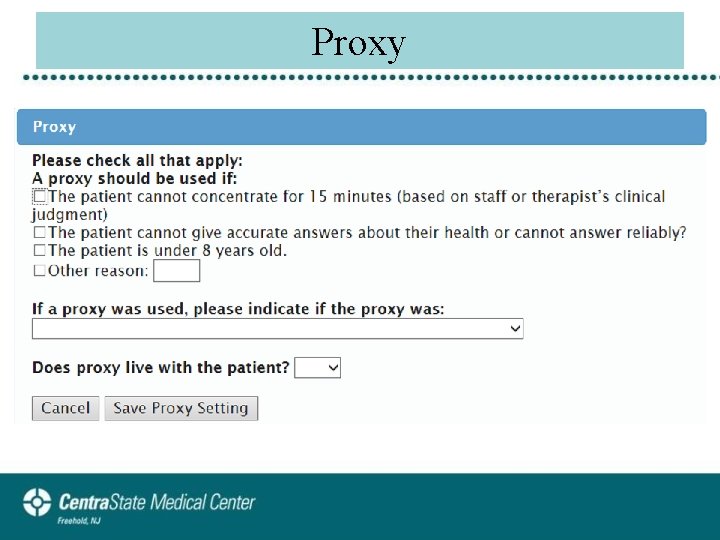
Proxy
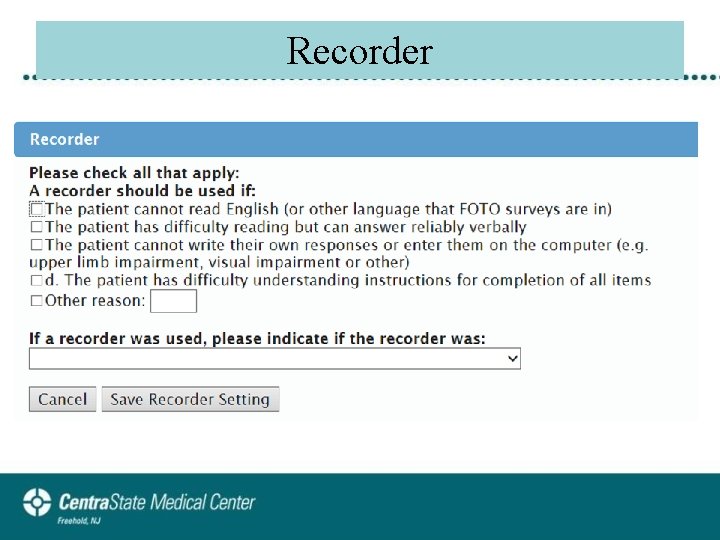
Recorder
Supplemental Instructions • There are no wrong answers. We want to know what YOU think. • If you are asked about something you haven’t done recently, estimate how hard it would be if you tried to do it now. • If a question does not seem to apply to you, choose the response closest to the right answer for you…select the “best fit” answer.
Supplemental Instructions Scenario: Optional surveys with potentially sensitive questions (e. g. , psychosocial depression screen) Keep in mind that the computer does not know who you are. These are standardized questions. Don’t worry if something doesn’t seem to directly apply to you, just indicate the closest answer. I’m interested in learning more about how your condition may or may not be affecting you either physically and/or emotionally.
Supplemental Instructions Scenario: 80 year old patient wants to know why they are being asked if they can run. “The computer does not know you. It doesn’t know if you are 18 or 100 years old. ” “The computer is assessing your present physical abilities. In order to find out what you can do, it has to find out what you cannot do. (like math testing in school)”
Supplemental Instructions Scenario: Function is limited by medical contraindications Example: post-op rotator cuff repair. Re-read Re-emphasize Objectively re-state
Biopsychosocial Model • Patients referred to physical therapy • 30 -50% show clear signs of depressive symptoms (Haggman Phys Ther 2004, Werneke JOSPT 2011) • 50% experience elevated fear of physical and/or work activities (Werneke. Spine 2001) • Nearly 20% classified at high risk based on psychosocial factors for poor outcomes (Werneke JOSPT 2011)
Screening for Psychosocial Factors • Psychosocial modules • Fear of physical and work activities Hart PTJ 2009 • Catastrophizing Sullivan PCS Psychol Assess 1995 • Psychosocial distress • Depression & somatization • Single item screen Hart J Qual Life Res 2010 • Dionne’s risk assessment Werneke JOSPT 2011 • STar. T risk classification Hill et al Arth Rheum 2008 • Self Efficacy Anderson et al Pain 1995
Biopsychosocial Science • Screening for patient’s beliefs, fears, illness perceptions, emotions and behaviors regarding his or her pain experience, & • Targeting patients at high psychosocial risk for cognitive behavioral therapy 5 # t e n e T (CBT by physical therapists)
Cognitive Behavioral Treatment • CBT techniques – Meaning response • “Therapeutic alliance (TA) Patient’s beliefs & behaviors – Patient-practitioner interaction • Clinician’s communication skills • Clinician’s mannerisms – Advanced CBT programs for patients classified as high risk
Cognitive Behavioral Technique • Meaning responses – TA between patient-practitioner • The patient is comfortable approaching you • Collaborative relationship • Patient has trust & confidence in your ability to function effectively on their behalf Vong et al APMR 2011
Cognitive Behavioral Technique • Meaning responses – Communication • • Praise & attention to (+) behavioral change Ask questions that build self-efficacy beliefs Patient centered interviewing & goal setting Positivity & problem framing Zolnierek et al. Med Care 2009
Cognitive Behavioral Technique • Meaning responses – Clinician’s mannerisms • Enthusiastic vs. lukewarm • Behavioral and verbal messages Moerman et al. Annals Int Med 2002
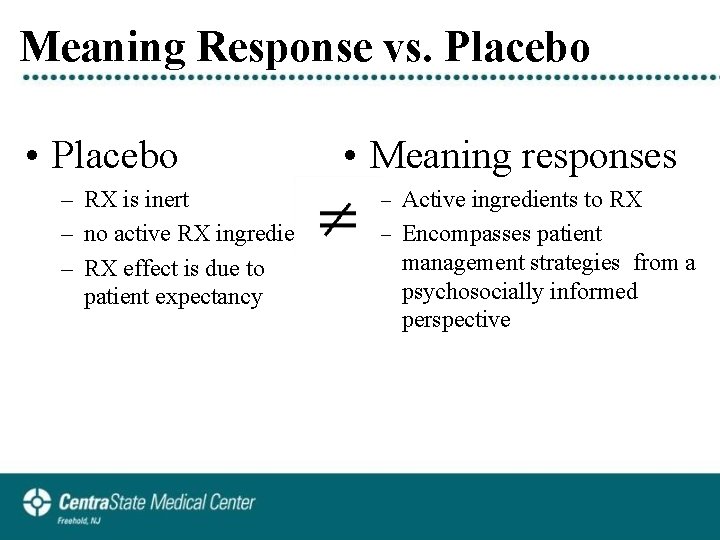
Meaning Response vs. Placebo • Placebo – RX is inert – no active RX ingredient – RX effect is due to patient expectancy • Meaning responses – Active ingredients to RX – Encompasses patient management strategies from a psychosocially informed perspective
Meaning or Non-Specific Response • Meaning response = non-specific factors • Linde et al BMC Medicine 2010 – Meta analyses of 37 acupuncture trials with a total of 5754 patients – Reported large meaning response effects which made it difficult to detect small additional specific effects of the actual treatment rendered
Meaning or Non-Specific Response • Meaning response = non-specific factors • Menke M. Do manual therapies help LBP. Spine 2014 – Meta analyses of 336 spinal manipulation studies – Non-specific factors explained: • 97% of outcomes for acute LBP – 3% of treatment (SMT) • 67% of outcomes for chronic LBP – 32% of treatment » Exercise with support considered most effective strategy
Summary: Literature Review Best Patient Outcomes 5 # t e n e T Therapists who are skilled at the enhancement of meaning responses while embracing evidence-based interventions are providers of choice to produce best outcomes
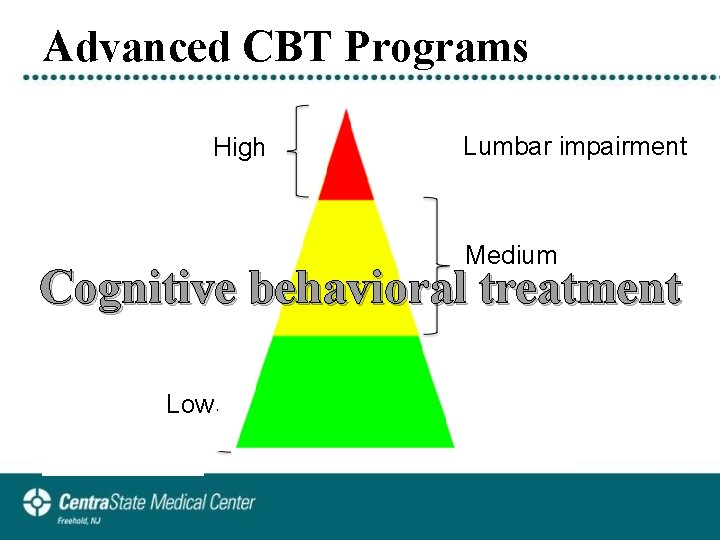
Advanced CBT Programs High Lumbar impairment Medium Cognitive behavioral treatment Low
Advanced CBT Programs • Recommended for physical therapists • Two types Formal task-specific activity/exercise approaches • Graded exercise (operant) conditioning program Fordyce JC APMR 1973 • Graded exposure program Vlaeyen JW Behav Res Ther 2001
Advanced CBT Programs • Graded exposure (task-specific training) • Function-focused program • 5 steps – – – Education Hierarchy of tasks/activities reported as least to most difficult Practice (graded exposure) specific activities & tasks Task-specific strengthening exercises* Problem solving skills & goal setting * Modified from Vlaeyen JW. Pain 2000
Graded Exposure Step 1 • Education “The Message” Spine is strong Control not cure Stay active Therapy alliance Hurt vs. harm Buchbinder R et al. Spine 2001 Burton AK et al Spine 1999 (Back Bk) Sullivan MJ et al. PT Canada
Graded Exposure Step 2 • Develop hierarchy of activities & tasks w patient – FOTO report: lists patient’s difficulties and limitations Important to know which with performing activities: e. g. no difficulty to extreme functional tasks are most difficulty problematic so that task– Fear of Daily Activity Questionnaire specific programs can be • (George JOSPT 2009) designed to target these tasks • Open-ended questions for additional activities and activities patient expresses fear or difficulty doing Tenet #1
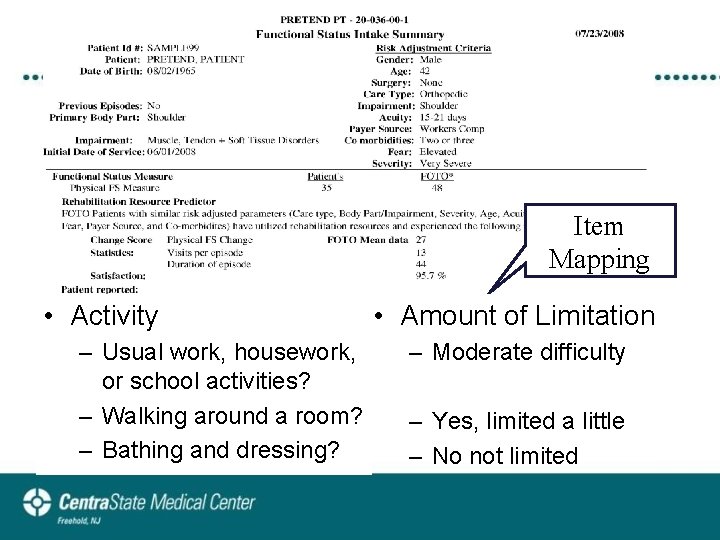
Item Mapping • Activity – Usual work, housework, or school activities? – Walking around a room? – Bathing and dressing? • Amount of Limitation – Moderate difficulty – Yes, limited a little – No not limited
Graded Exposure Step 3 • Practice (graded exposure) least to more difficult tasks/activities – Ask patient to perform task-specific activities reported as difficult e. g. lift groceries, push vacuum, mop floor. . • Purpose – Allow correction of patient’s misconception of pain – Learn “hurt” vs “harm” principles
Graded Exposure Step 3 • Task-specific training • Philosophical shift in strength training – Instead of prescribing a series of traditional & typical isolated extremity or trunk strengthening exercises, therapist develops a strength training program utilizing task specific exercises i. e. patient is exposed to tasks rated as fearful or difficult (George JOSPT 2009)
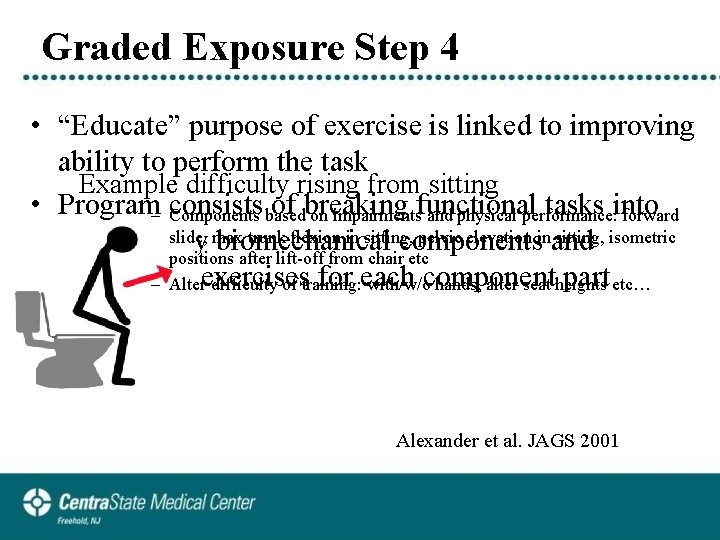
Graded Exposure Step 4 • “Educate” purpose of exercise is linked to improving ability to perform the task Example difficulty rising from sitting • Program consists of breaking functional tasks into – Components based on impairments and physical performance: forward slide, max trunk flexion in sitting, pelvic elevation in sitting, isometric multiple key biomechanical components and positions after lift-off from chair etc prescribing exercises for each component part – Alter difficulty of training: with/w/o hands, alter seat heights etc… Alexander et al. JAGS 2001
Graded Exposure Step 5 • Develop problem solving skills – Across a wide variety of work and home tasks • Crombez et al. Health Psychology 2002 – Progress to new tasks rated more difficult – Key educational message: “hurt vs. harm” • although your back hurts does your back limit you from doing the task?
Thank you Any Questions?
- Slides: 42