Occupational Health III Occupational Cancer Commonly affected sites





- Slides: 26

Occupational Health III
Occupational Cancer • Commonly affected sites: skin, lungs , bladder and blood forming organs • Skin cancer: Ca scrotum and Ca skin because of coal tar, x-rays, oil and dyes • Seen in gas workers, tar distillers, oil refiners, dye stuff makers
Lung cancer • Seen in gas industry, asbestos industry, nickel and chromium work • Most of the lung cancers are attributed to tobacco smoking, air pollution and occupational exposure.
Bladder cancer • • First noted in aniline industry workers Caused by aromatic amines Dye stuff, rubber gas, electric cable industries Possible bladder carcinogens: Beta napthyl amine, benzidine, auramines
Leukemia • Exposure to benzol, roentgen rays and radioactive substances

Characteristics of occupational cancer i. Appears after prolonged exposure ii. Period between exposure and disease development may be as long as 10 -25 years iii. Disease may develop even after cessation of exposure iv. Average incidence is earlier v. Constant localisation

Control of industrial cancer 1. Elimination or control of industrial carcinogens 2. Exclusion of carcinogen from the industry 3. Well designed building, closed system of production 4. Inspection of factories 5. Medical examination 6. Notification 7. Licensing 8. Personal hygiene 9. Education of workers and management 10. Research
Occupational dermatitis • Causes: 1. Physical : Heat, cold, friction, x-rays 2. Chemical: Acid, alkali, dyes, solvents 3. Biological: Bacteria, fungi, viruses 4. Plant products: Flowers, leaves, vegetables
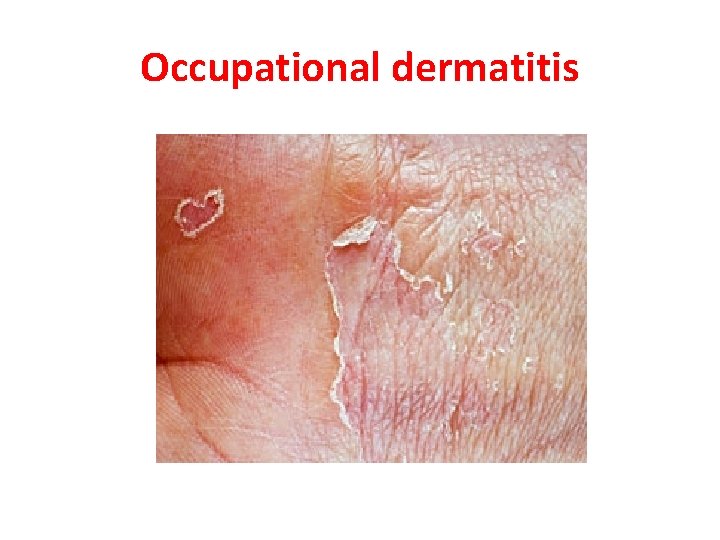
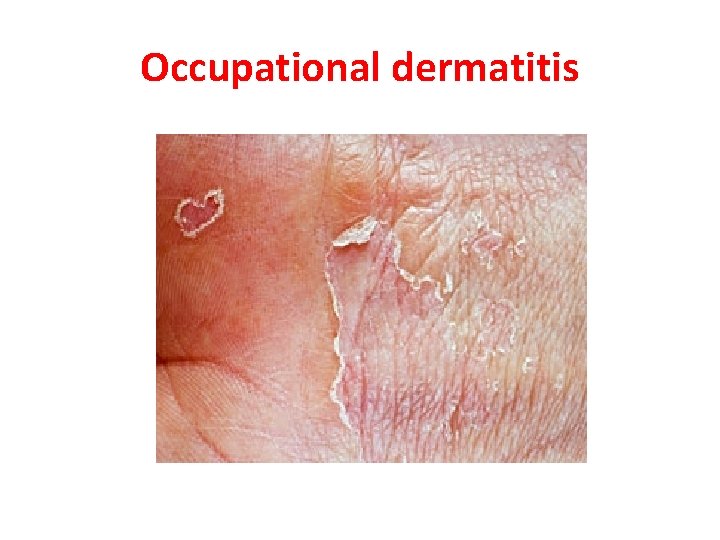
Occupational dermatitis
Dermatitis causing agents 1. Primary irritants: Acids, alkalies : in workers exposed in sufficient concentration and long period of time 2. Sensitizing/ Allergic: Due to skin sensitization Ø Commonest Sites: Ø Hands and forearm Ø Face: Airborne contact dermatitis
Diagnostic Criteria 1. Disease appears during a period of occupational exposure or within a reasonable period of time after the exposure ceases 2. Occurs first on the exposed part 3. Disease has not been present previously
4. Disease improves after the termination of exposure 5. Disease recurs after exposure 6. Morphology of the disease is similar to the well known cases resulting from similar exposure and other fellows with similar exposure similarly affected.
Control measures i. iii. iv. v. Preselection Protection Personal hygiene Periodic inspection Zero contact: Substitution, Engineering controls, tools, PPE
Prevention • Easy to prevent than to cure 1. Protect with pre-work creams 2. Cleansing products 3. Effective skin disinfection after contamination with harmful germs 4. Reconditioning creams to keep the skin in healthy condition.

Review Ø Occupational cancer : characteristics, Prevention Ø Occupational dermatitis: Agents, Diagnostic criteria, Protection and prevention
Lead Poisoning • Introduction: Widely used in a variety of industries Characteristics of lead: i. Low boiling point ii. Mixes with other metals easily to form alloys iii. Easily oxidised iv. Anti-corrosive
• All lead compounds: • Toxic : Lead arsenate, lead oxide and lead carbonate • Least toxic: Lead sulphide • Industrial use: storage batteries, glass manufacture, ship building, rubber industry • Non- occupational sources: Thousands of tons of lead exhausted from automobiles per year

• Mode of absorption: i. Inhalation of fumes and dust: industries ii. Ingestion through contaminated hands iii. Skin: For tetraethyl lead Body stores: in average adult: 150 -400 mg Blood level: 25 µg per 100 ml 70 µg: Associated with clinical features
• Body distribution: • 90% of ingested lead : Fecal excretion • Absorbed lead : enters gut : 95% enters RBC’s • Liver and kidney • Bones with other minerals
• Clinical picture: Lead Poisoning / Plumbism • Inorganic lead: Abdominal colic, constipation, loss of appetite, blue line on gums, stippling of red cells, Anemia, wrist drop and foot drop. • Organic lead: On CNS: Insomnia, headache, delirium, Mental confusion
• Diagnosis: 1. History: of lead exposure 2. Clinical features
1. Lab tests: i) Coproporphyrin in urine Measure of CPU : Non exposed: 150 µg / ltr ii) Aminolevulinic acid in urine: > 5 mg/ ltr : lead absorption iii) Lead in blood and urine: Lead in urine: > 0. 8 mg/ ltr (Normal: 0. 2 to 0. 8) Blood level : 70 µg / 100 ml : Clinical features seen iv) Basophilic stippling of RBC
Preventive measures i. Substitution: with less toxic materials ii. Isolation: All such processes enclosed/ segregated iii. Local exhaust ventilation: To remove fumes/ dust iv. Personal protection: Workers: Approved respirators v. Good housekeeping: Wet sweeping vi. Working atmosphere: Lead concentration: <2 mg/10 cu mm air Permissible limit
vii. Periodic examination of workers: Lab determination of urine lead, blood lead, RBC count, Haemoglobin and coproporphyrin test of urine viii. Personal hygiene: Hand washing ix. Health Education: On risks involved and personal protection measures
Management of lead poisoning • Prevention of further absorption • Removal of lead from soft tissues • Early recognition of cases : To prevent further absorption • Saline purge : To remove unabsorbed lead from gut • Use of chelating agents: Promotes lead excretion in urine: d-Penicillamine – Notifiable disease and with compensation in India since 1924
Lead Poisoning Ø Introduction Ø MOA Ø Clinical Picture Ø Diagnosis Ø Management Ø Prevention
 Role of occupational health nurse
Role of occupational health nurse Occupational cancer
Occupational cancer Hamlet act iii scene iii
Hamlet act iii scene iii Occupational safety and health objectives
Occupational safety and health objectives Chcp occupational health
Chcp occupational health Occupational safety and health act 1984
Occupational safety and health act 1984 Occupational health and safety presentation
Occupational health and safety presentation Occupational health and safety act ontario
Occupational health and safety act ontario Define occupational health nursing
Define occupational health nursing Ipac online course
Ipac online course Global strategy on occupational safety and health
Global strategy on occupational safety and health Occupational health and safety assessment series
Occupational health and safety assessment series Ecology of human performance model
Ecology of human performance model Occupational health services renton
Occupational health services renton Aims and objectives of occupational health
Aims and objectives of occupational health Stanford ohc
Stanford ohc Occupational health and safety course outline
Occupational health and safety course outline What is occupational health
What is occupational health Occupational safety and health
Occupational safety and health Uhcw site map
Uhcw site map Abu dhabi occupational health
Abu dhabi occupational health Aota occupational profile template
Aota occupational profile template Korea occupational safety & health agency
Korea occupational safety & health agency Occupational safety and health
Occupational safety and health Occupational health clinic for ontario workers
Occupational health clinic for ontario workers Mobile occupational health screening unit
Mobile occupational health screening unit Conclusion of health and disease
Conclusion of health and disease