NUR 213 Ventral Septal Defect Unfolding Case Study
- Slides: 15
NUR 213 Ventral Septal Defect Unfolding Case Study Developed by Benita Beard, MSN, RN Brenda Stepp, MSN, RN
Outcomes for Case Study � Determine current best practice for nursing and collaborative care strategies in the treatment of individuals with ventral septal defect. � Determine pharmacological considerations related to the management of individuals with a ventral septal defect. � Incorporate principles of growth and development, prioritize the plan of care for the family of and the individual with a ventral septal defect. � Determine other physiological and psychosocial concepts and/or exemplars related to ventral septal defect.
Outcomes for Case Study � Determine the incidence, etiology, populations at risk, and epidemiology of ventral septal defect. � Determine assessment findings and diagnostic testing related to ventral septal defect. � Review fetal circulation and newborn assessment. � Recognizing cultural diversity, incorporate the nursing process in providing primary, secondary, and tertiary care for, and prevention of, ventral septal defect.
What if ? � Baby Girl H was admitted to the Well-Baby Nursery at 0742. � Admission Data: Temp: 97. 2 ®; Heart Rate: 144; Respiratory Rate: 42
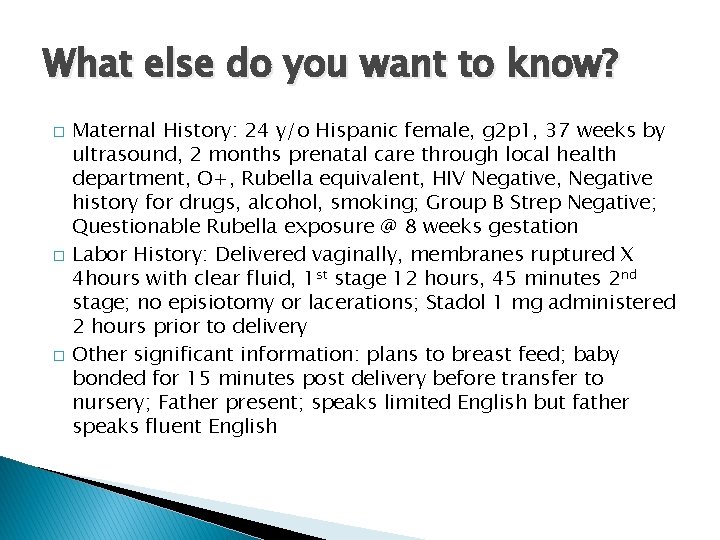
What else do you want to know? � � � Maternal History: 24 y/o Hispanic female, g 2 p 1, 37 weeks by ultrasound, 2 months prenatal care through local health department, O+, Rubella equivalent, HIV Negative, Negative history for drugs, alcohol, smoking; Group B Strep Negative; Questionable Rubella exposure @ 8 weeks gestation Labor History: Delivered vaginally, membranes ruptured X 4 hours with clear fluid, 1 st stage 12 hours, 45 minutes 2 nd stage; no episiotomy or lacerations; Stadol 1 mg administered 2 hours prior to delivery Other significant information: plans to breast feed; baby bonded for 15 minutes post delivery before transfer to nursery; Father present; speaks limited English but father speaks fluent English
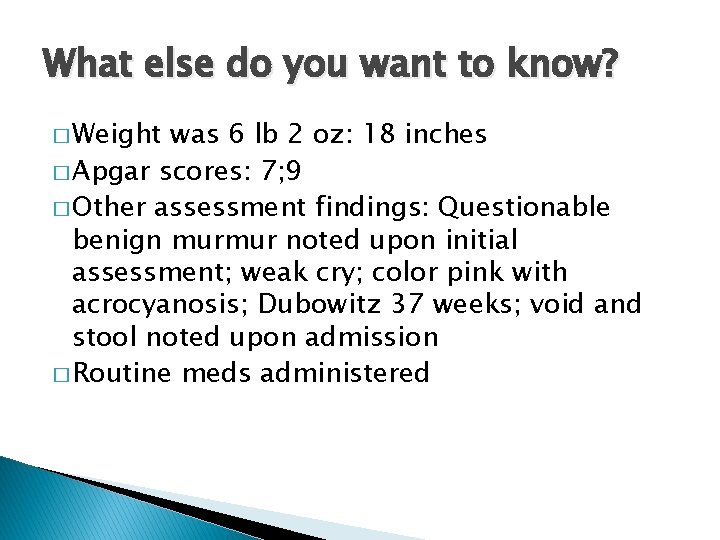
What else do you want to know? � Weight was 6 lb 2 oz: 18 inches � Apgar scores: 7; 9 � Other assessment findings: Questionable benign murmur noted upon initial assessment; weak cry; color pink with acrocyanosis; Dubowitz 37 weeks; void and stool noted upon admission � Routine meds administered
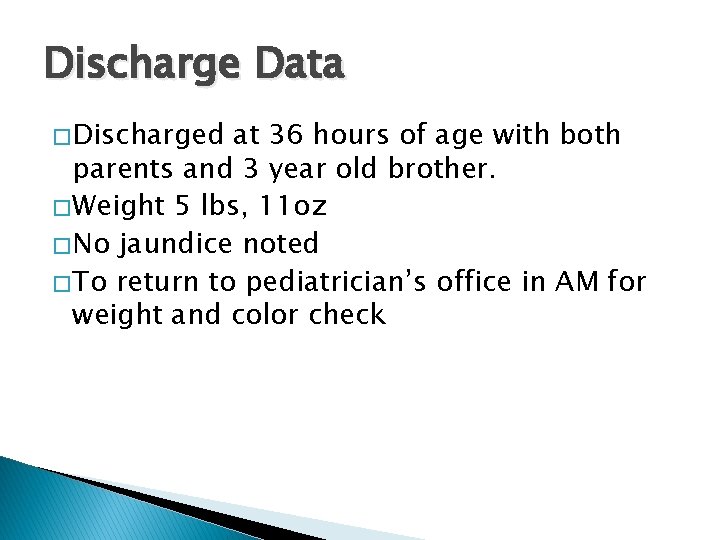
Discharge Data � Discharged at 36 hours of age with both parents and 3 year old brother. � Weight 5 lbs, 11 oz � No jaundice noted � To return to pediatrician’s office in AM for weight and color check
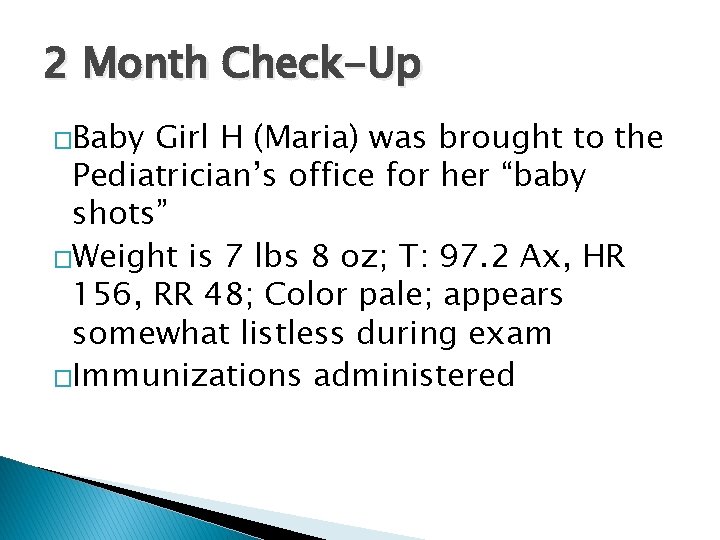
2 Month Check-Up �Baby Girl H (Maria) was brought to the Pediatrician’s office for her “baby shots” �Weight is 7 lbs 8 oz; T: 97. 2 Ax, HR 156, RR 48; Color pale; appears somewhat listless during exam �Immunizations administered
What education/follow-up is indicated based on these assessment findings? � Nutritional Assessment: Maria is breast fed but continually falls asleep during feedings. Maria feeds every four hours for a total of 10 to 15 minutes each feeding. Awakes at least twice during the night to feed. � Bonding: Mother is very attentive, smiles at Maria and talks to her during assessment.
Follow-up �Weight check in 2 weeks �Feedings every two to three hours �Other diagnostics that might be indicated?
2 week follow-up visit � Weight is 7 lbs 10 oz; T: 97. 2 Ax, HR 164 while sleeping, RR 52; Color pale, skin cool and dry except on forehead which is sweaty; sleeps during exam but weak cry noted during lab draws; Murmur present; Pa. SO 2 94%
Diagnostics � Ultrasound of heart reveals large Ventral Septal Defect � Labs: Hct 42, HGB 17 � Plan is to send to pediatric referral center for Cardiac Catheterization
Care of the Child Undergoing a Cardiac Catheterization �Pre-Procedural management �Post-Procedural management
Follow-Up Visit with Cardiologist � Assessment Findings: Weight 7 lbs 6 oz; T: 97. 0 Ax, HR 176 while sleeping, RR 58; Color remains pale, skin cool and dry at time of exam; Hard to arouse during exam; Murmur present; Pa. SO 2 93% at rest
Plan of Care for the Child with Heart Failure � Nutritional Management � Medical Management � Other Medical and Nursing Strategies that should be considered in the management of a child with heart failure related to a congenital heart defect � Teaching Needs