NHS Stoke on Trent Delivering the NHS Health

- Slides: 20

NHS Stoke on Trent Delivering the NHS Health Check and Lifestyle Programmes – boosting uptake and minimising costs – experiences of NHS Stoke on Trent November 2011
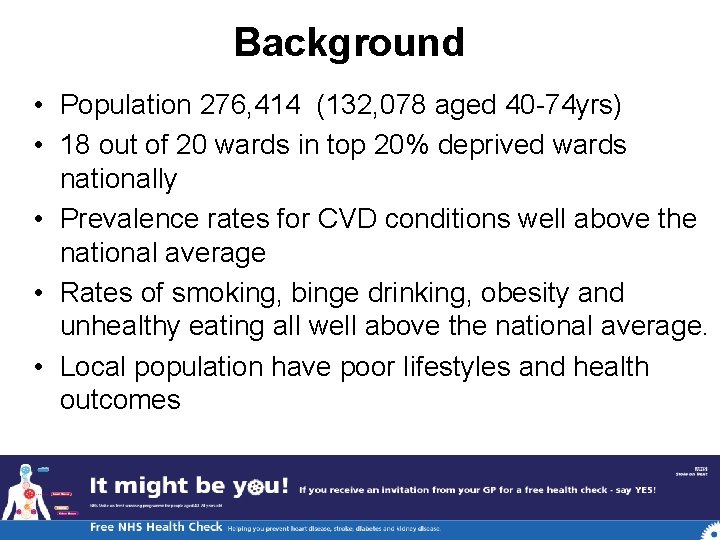
Background • Population 276, 414 (132, 078 aged 40 -74 yrs) • 18 out of 20 wards in top 20% deprived wards nationally • Prevalence rates for CVD conditions well above the national average • Rates of smoking, binge drinking, obesity and unhealthy eating all well above the national average. • Local population have poor lifestyles and health outcomes
Setting the scene Need for early identification and effective management of CVD risk amongst our population Started in 2008 Own approach to Health Trainers and Primary Prevention Clinical Criteria applied—more extensive than NHS HC Oberoi – prioritising patients
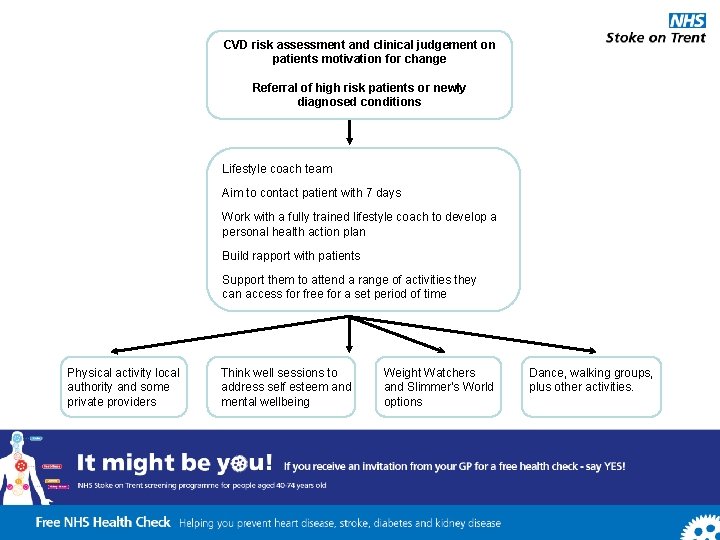
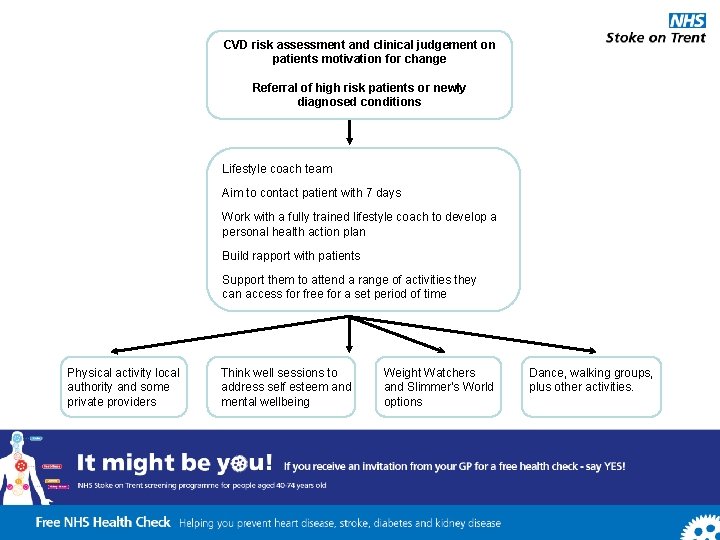
CVD risk assessment and clinical judgement on patients motivation for change Referral of high risk patients or newly diagnosed conditions Lifestyle coach team Aim to contact patient with 7 days Work with a fully trained lifestyle coach to develop a personal health action plan Build rapport with patients Support them to attend a range of activities they can access for free for a set period of time Physical activity local authority and some private providers Think well sessions to address self esteem and mental wellbeing Weight Watchers and Slimmer's World options Dance, walking groups, plus other activities.
Lifestyle Programme – evolving referral criteria to meet other at risk groups • Antenatal/post natal with a BMI 30 or greater • IGT • Mental health register • Quota allocation
Key Learning from the early stages • PCT employed Project Support Workers – help to bridge gaps with practices • Slow uptake – embedding in primary care • Template issues – I. T. • GP Champion helped to secure support from practices/LES incentives • Networking learning events, Practice Champions, news letters, league tables
Cost effective delivery of NHS HC • HCC – 3 types of delivery GP, pharmacy and community outreach • Aimed to compare different delivery methods and judge cost effectiveness • From 2009 to 2010 • Worked with improvement foundation but took a local approach
Community based delivery • • Voluntary sector organisation Outcomes 512 HC in one year Cost per HC = £ 154. 34 Strengths : targeted a cross section of local people • Weakness : couldn’t check eligibility, costly and time intensive data transfer
Pharmacy delivery • Commissioned pharmacy with a 100 hour contract to deliver the service • Outcomes: 44 HC in one year • Cost per case: £ 192. 21 (inc software) £ 93. 64 (excluding software) • Strengths: out of hours provision • Weaknesses: costly consumables, software, data transfer.
GP delivery • • • GP LES Trial different ways of working Outcomes: 705 HC by 8 practice teams Costs per HC: £ 24. 96 Strengths: use of existing infrastructure patient notes, events, existing info, opportunistic checks • Weaknesses: competing pressures in PC
Hard to reach patients - further support for practices • Patients eligible for NHS HC are reaching saturation – what do we do with non responders • Outline of the plan to engage with these groups via extra support for practices – tele health care, extra capacity to practices, link to targeted awareness raising. Pilot awaiting commencement.
Key Learning • GP was most cost effective delivery • Eligible patients already accessing practice team regularly • Community delivery most suited to awareness raising • Need to provide extra support to practices when eligible population reaches saturation point
Where are we now? • • 6500 referrals to LP Over 20, 000 HC delivered since 2008 Evaluation of Lifestyle Programme RCT study of 600 patients (use of Lifestyle Programme v GP usual care) • Qualitative study – focus groups • How effective is NHS HC follow on care in general practice for high risk patients?
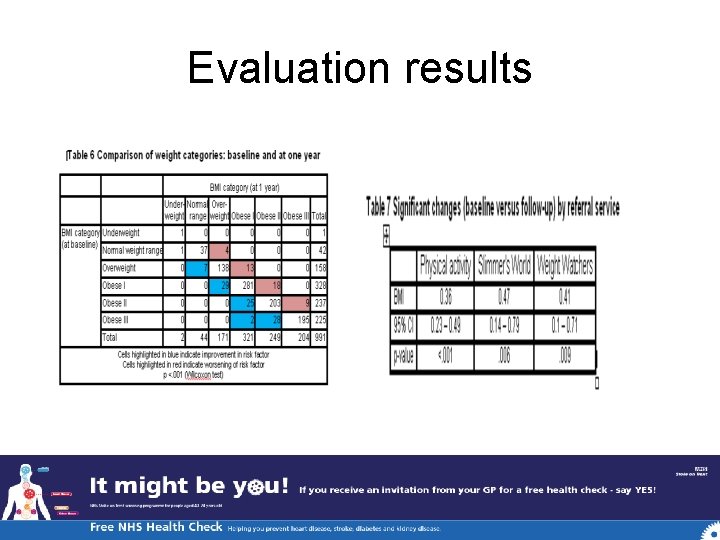
Evaluation 1000 LP patients • Baseline and 12 month follow up; utilising multiple data sources • Results show weight loss and weight gain! • Show the programme is effective for individual patients, rather than status quo
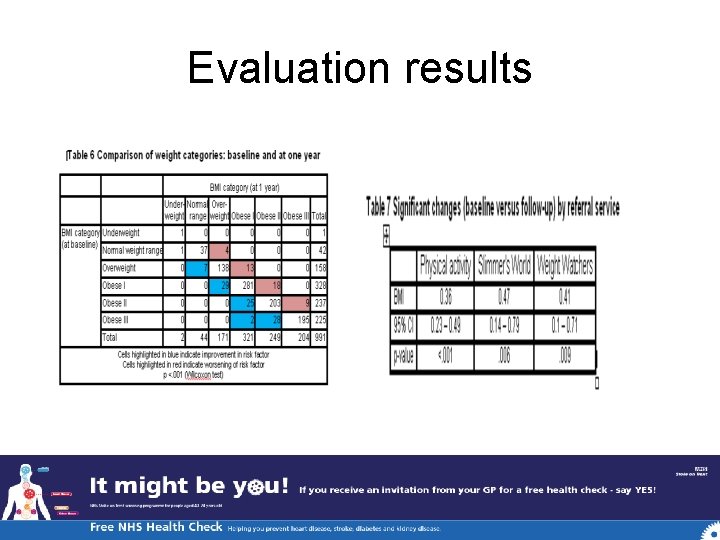
Evaluation results
Qualitative evaluation of LP • Focus groups and interviews with lifestyle coaches, engaged and dis-engaged patients, practice managers • Even dis-engaged patients valued the Lifestyle Programme
High risk patients – what happened to them • Follow up searches to identify how many patients identified at high risk or with new condition • Manual trawl to notes to see what happened to them
RCT • Results pending ! • Findings and analysis by Staffordshire University academics- now based in Australia • Planning national conference /present findings in Stoke on Trent in summer 2012 – do come
Key Learning • Constant formal and informal evaluation • Constant liaison with practices • Fair LES for NHS Health Check (half funded by PH baseline & half by CCG) • Practices allow us to follow patients – part of wider CCG agenda of reducing unwarranted clinical variation between practice teams • Public health need to maintain interaction with CCG (board / throughout) • Referral criteria for Lifestyle Programme updated
Questions/discussion Contact details: Yvonnne Mawby yvonne. mawby@stoke. nhs. uk Dr Ruth Chambers Ruth. chambers@stoke. nhs. uk Jagdish Kumar Jagdish. kumar@stoke. nhs. uk
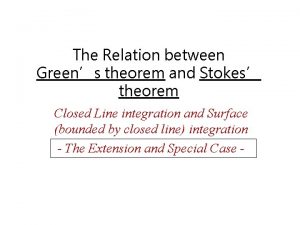
 Stokes and green's theorem
Stokes and green's theorem Stoke lodge ramblers
Stoke lodge ramblers Chynestoke
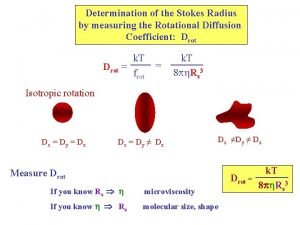
Chynestoke Stokes radius
Stokes radius Trent hoover wrestling
Trent hoover wrestling Trent global college
Trent global college Trent 8104
Trent 8104 The final decrees of the council of trent
The final decrees of the council of trent Trent global
Trent global Protestant vs catholic war
Protestant vs catholic war Trent 2018
Trent 2018 Jaeger flask
Jaeger flask Trent harkrader
Trent harkrader Council of trent ap euro
Council of trent ap euro Emma notts
Emma notts Trent jaeger
Trent jaeger Trent deckard
Trent deckard Trent-severn waterway national historic site
Trent-severn waterway national historic site Trent university campus
Trent university campus Trent global college review
Trent global college review 1 989e30 kg
1 989e30 kg