ND Suicide Prevention With Help There is Hope


- Slides: 20
ND Suicide Prevention With Help, There is Hope By Alison Traynor
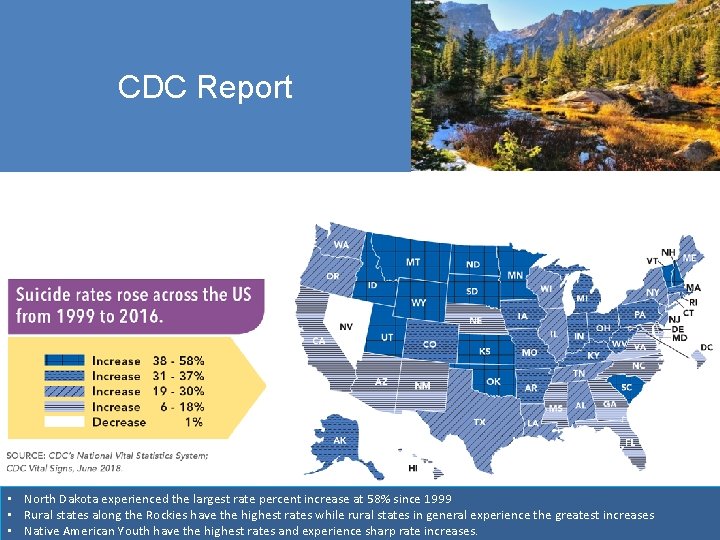
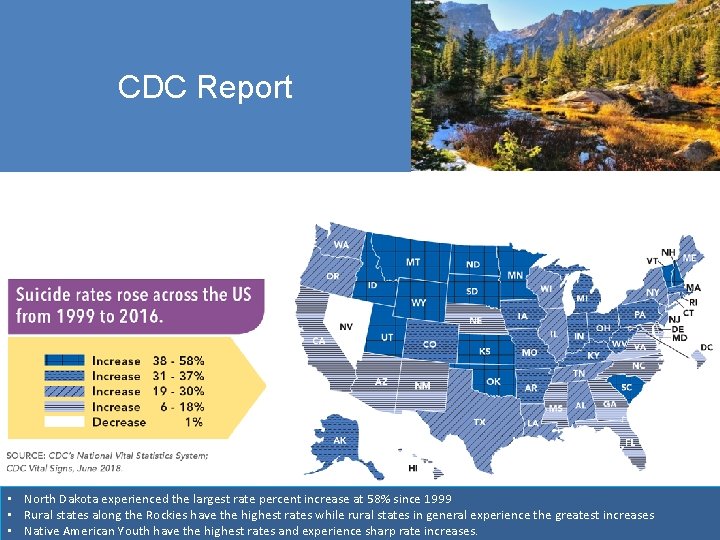
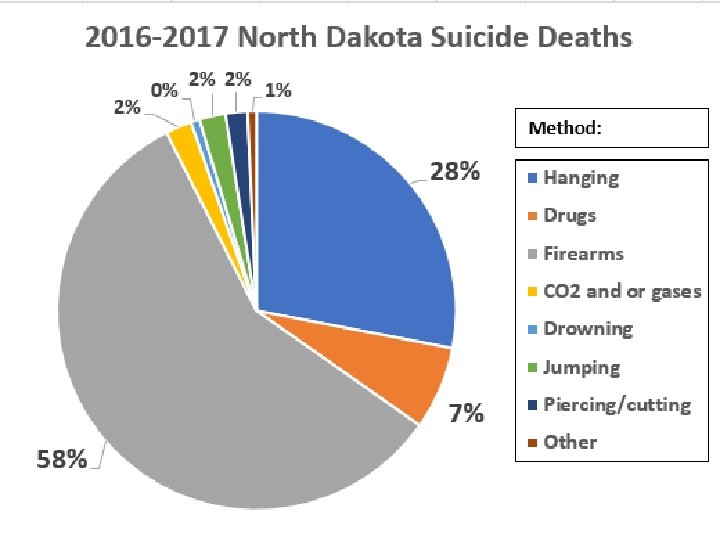
CDC Report CDC • North Dakota experienced the largest rate percent increase at 58% since 1999 • Rural states along the Rockies have the highest rates while rural states in general experience the greatest increases • Native American Youth have the highest rates and experience sharp rate increases.
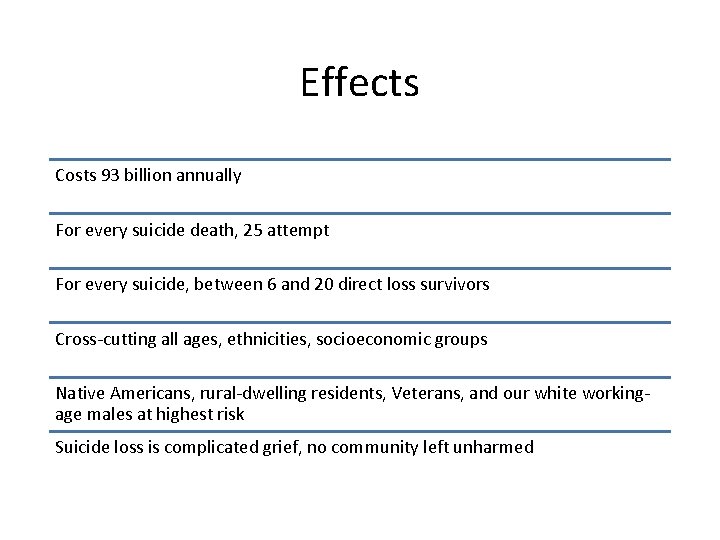
Effects Costs 93 billion annually For every suicide death, 25 attempt For every suicide, between 6 and 20 direct loss survivors Cross-cutting all ages, ethnicities, socioeconomic groups Native Americans, rural-dwelling residents, Veterans, and our white workingage males at highest risk Suicide loss is complicated grief, no community left unharmed
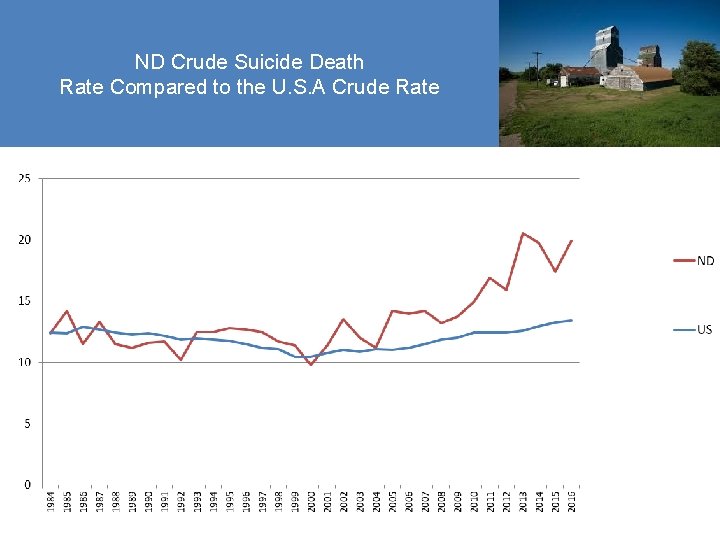
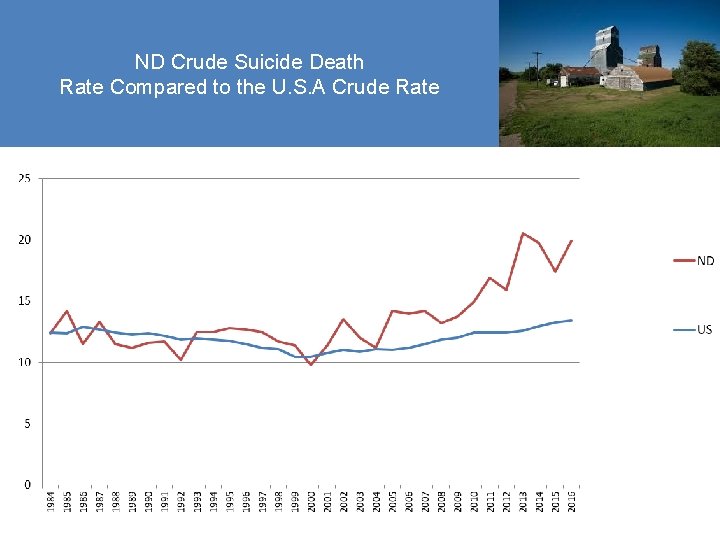
ND Crude Suicide Death Rate Compared to the U. S. A Crude Rate Source: ND Do. H Vital Records, (2016)
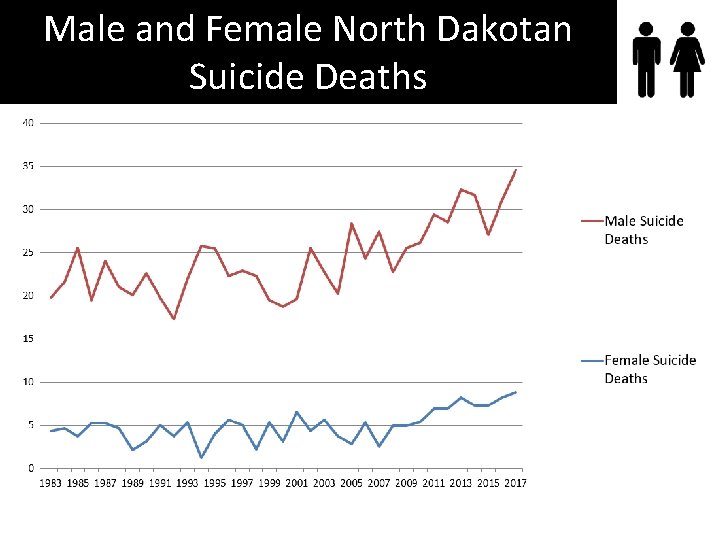
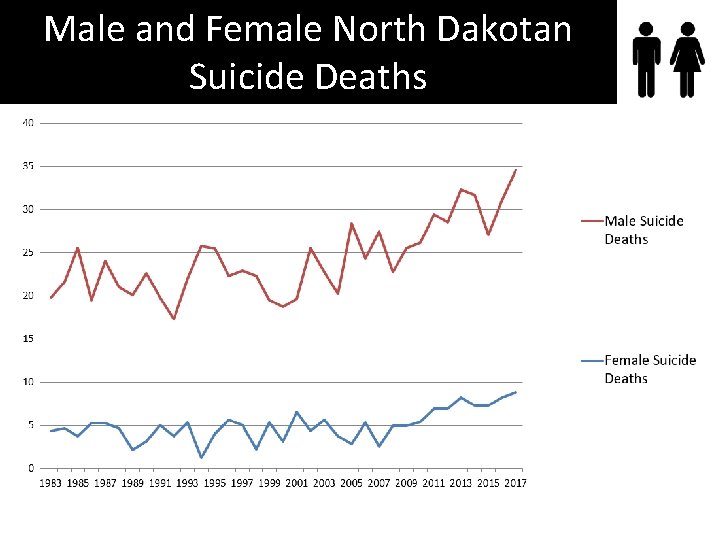
Male and Female North Dakotan Suicide Deaths
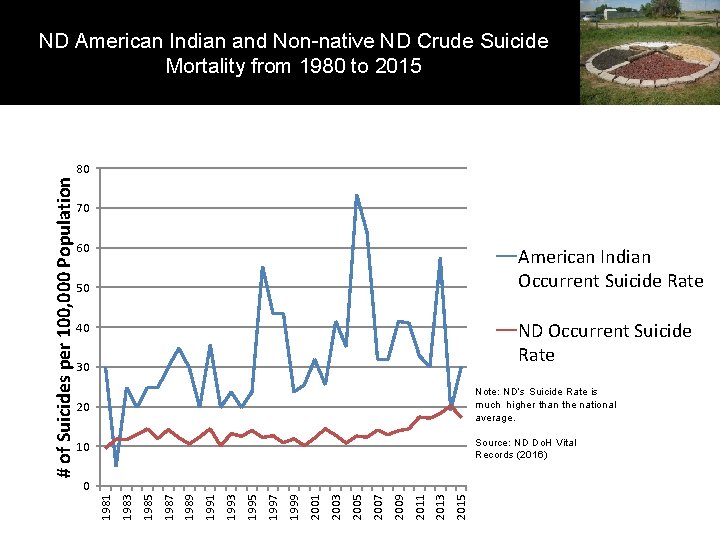
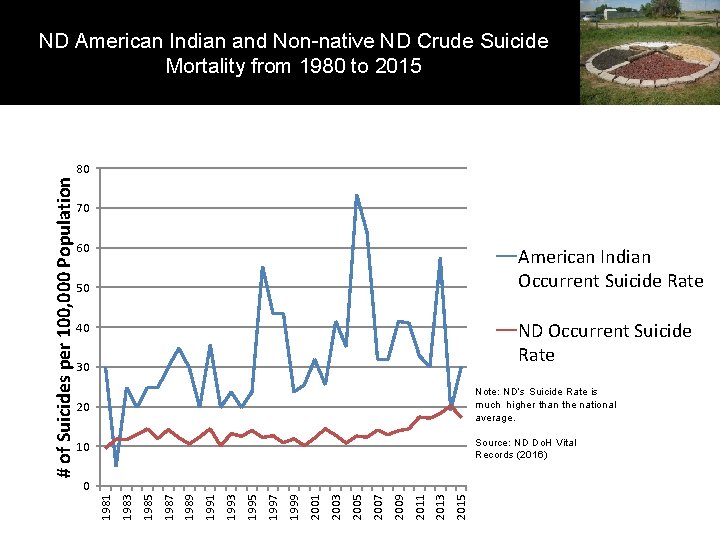
ND American Indian and Non-native ND Crude Suicide Mortality from 1980 to 2015 70 60 American Indian Occurrent Suicide Rate 50 ND Occurrent Suicide Rate 40 30 20 Note: ND’s Suicide Rate is much higher than the national average. 10 Source: ND Do. H Vital Records (2016) 2015 2013 2011 2009 2007 2005 2003 2001 1999 1997 1995 1993 1991 1989 1987 1985 1983 0 1981 # of Suicides per 100, 000 Population 80
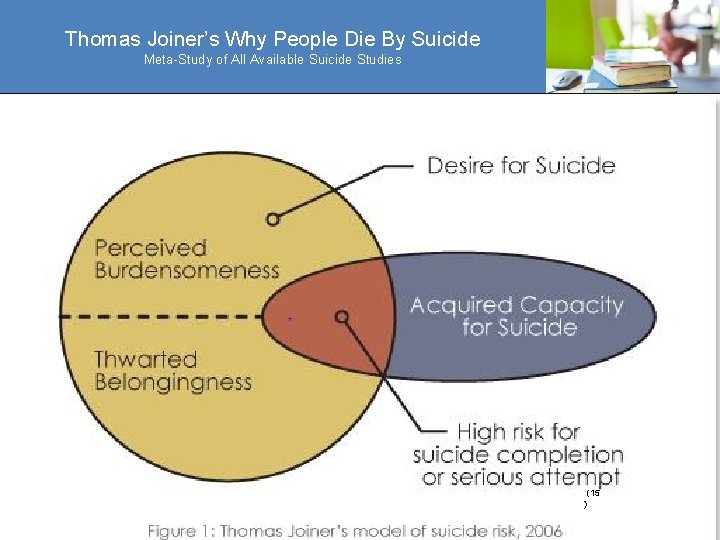
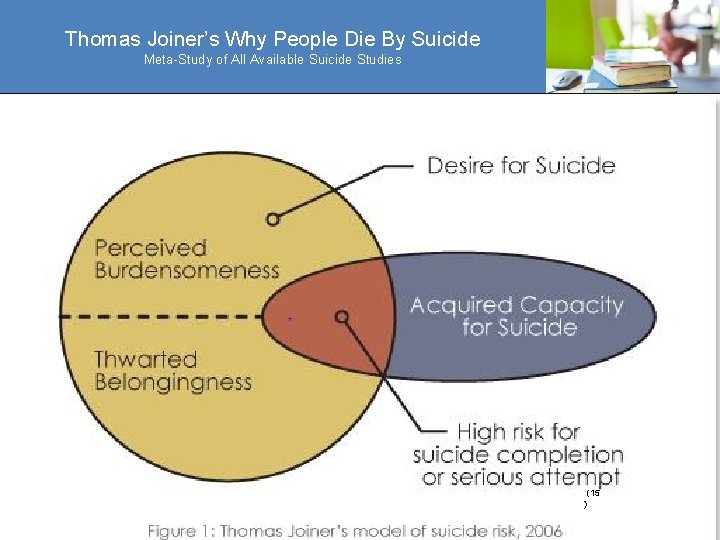
Thomas Joiner’s Why People Die By Suicide Meta-Study of All Available Suicide Studies (15 )
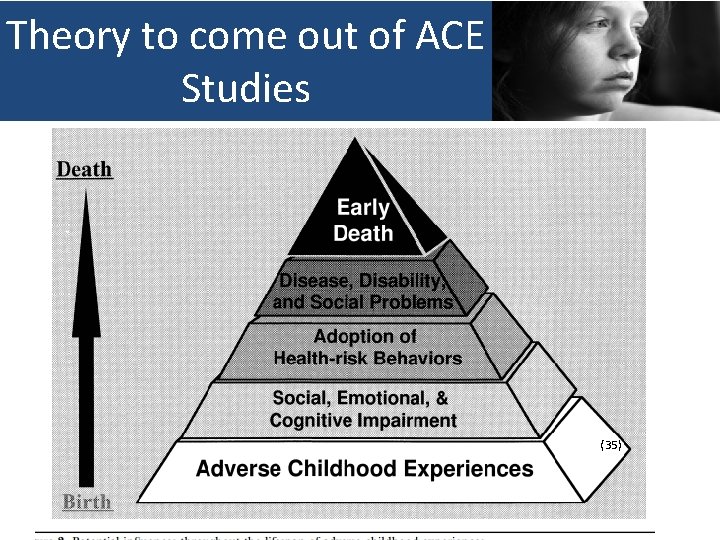
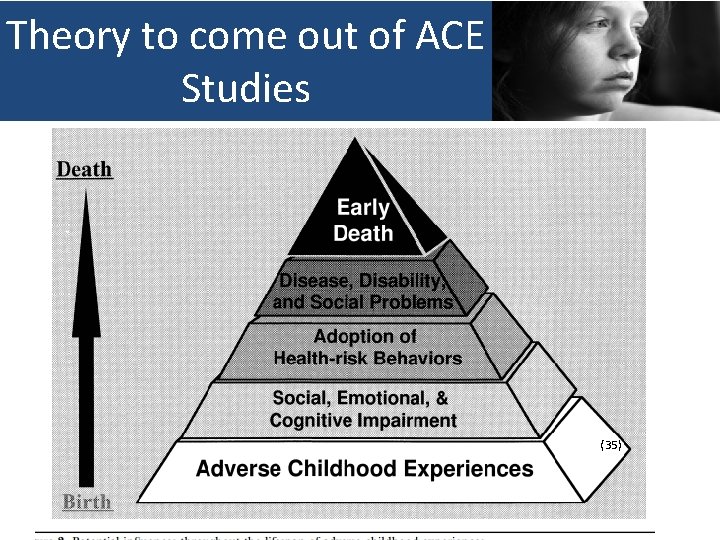
Theory to come out of ACE Studies (35)
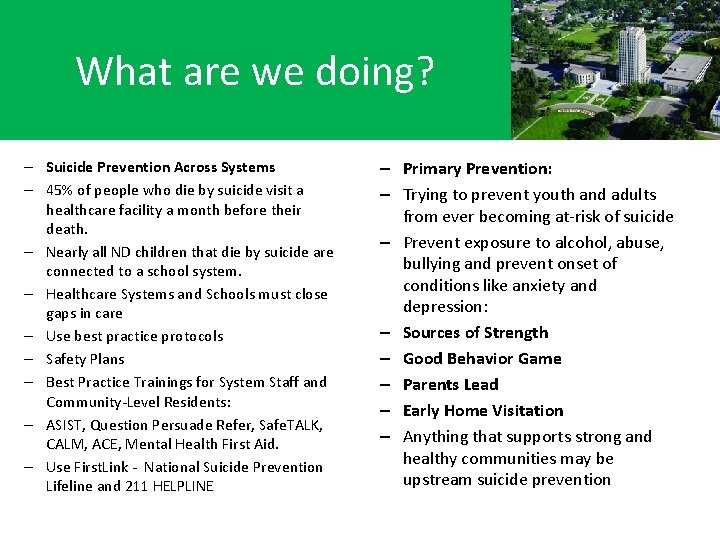
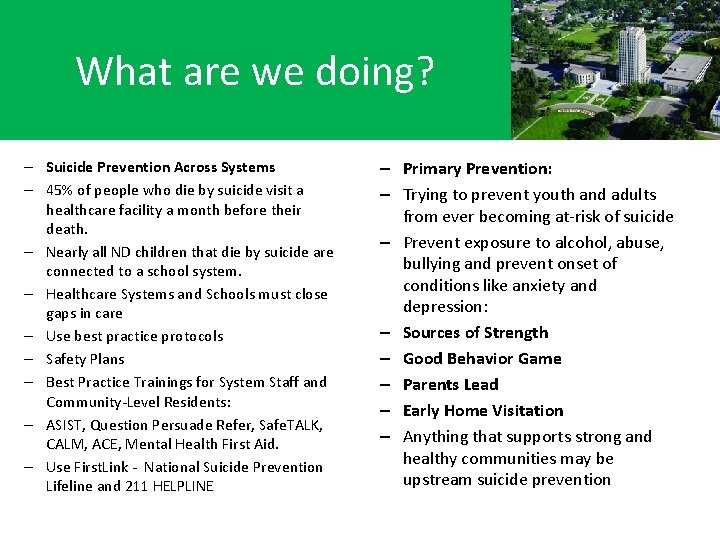
What are we doing? – Suicide Prevention Across Systems – 45% of people who die by suicide visit a healthcare facility a month before their death. – Nearly all ND children that die by suicide are connected to a school system. – Healthcare Systems and Schools must close gaps in care – Use best practice protocols – Safety Plans – Best Practice Trainings for System Staff and Community-Level Residents: – ASIST, Question Persuade Refer, Safe. TALK, CALM, ACE, Mental Health First Aid. – Use First. Link - National Suicide Prevention Lifeline and 211 HELPLINE – Primary Prevention: – Trying to prevent youth and adults from ever becoming at-risk of suicide – Prevent exposure to alcohol, abuse, bullying and prevent onset of conditions like anxiety and depression: – Sources of Strength – Good Behavior Game – Parents Lead – Early Home Visitation – Anything that supports strong and healthy communities may be upstream suicide prevention
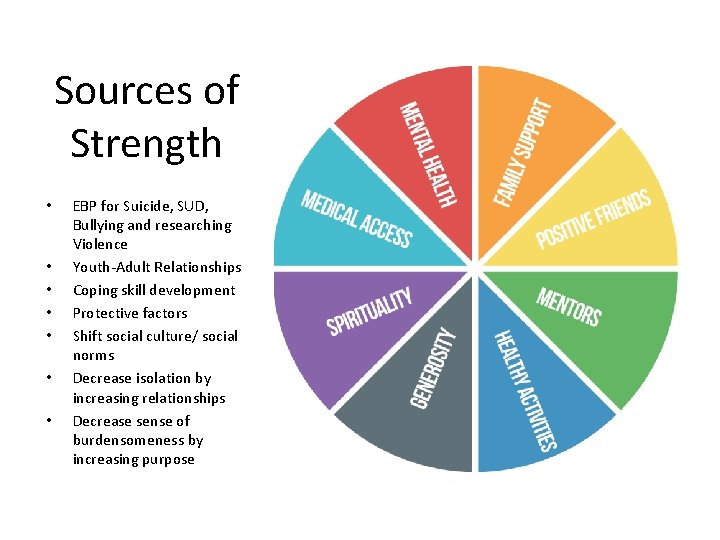
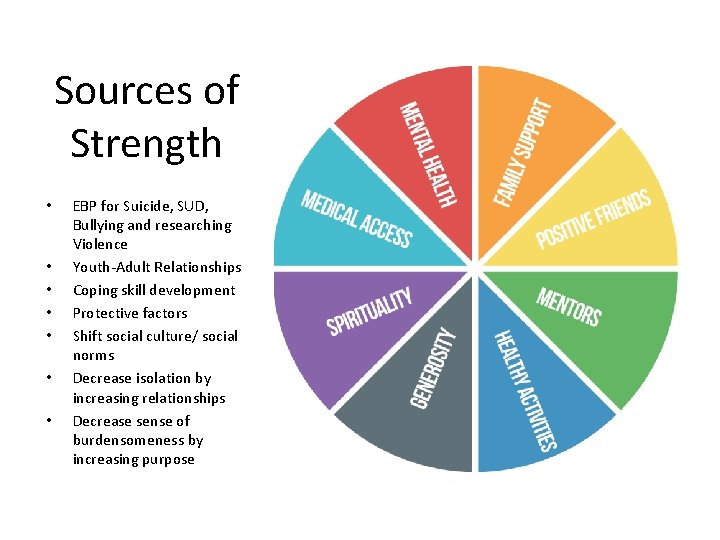
Sources of Strength • • EBP for Suicide, SUD, Bullying and researching Violence Youth-Adult Relationships Coping skill development Protective factors Shift social culture/ social norms Decrease isolation by increasing relationships Decrease sense of burdensomeness by increasing purpose
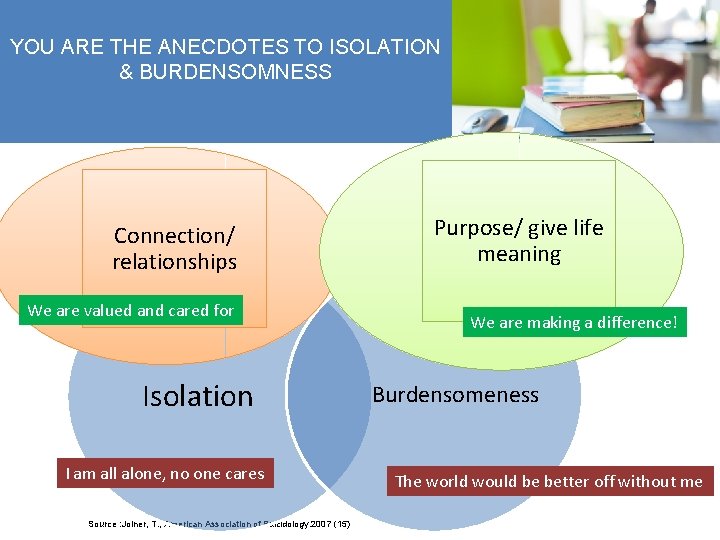
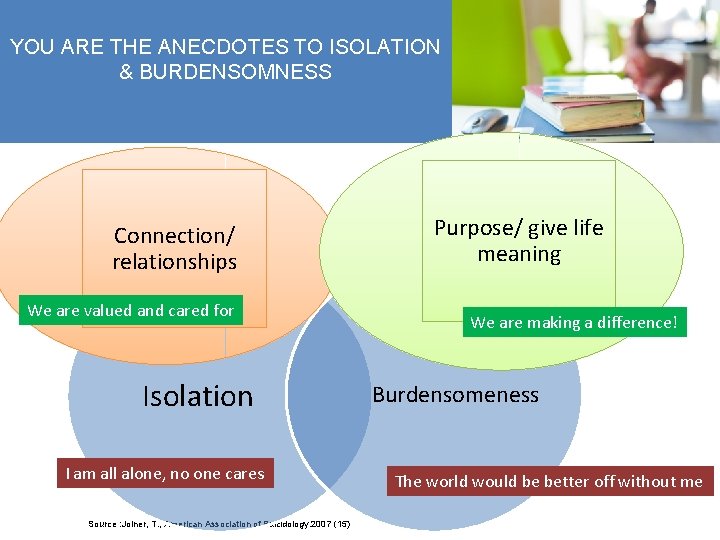
YOU ARE THE ANECDOTES TO ISOLATION & BURDENSOMNESS Connection/ relationships We are valued and cared for Isolation I am all alone, no one cares Source : Joiner, T. , American Association of Suicidology. 2007 (15) Purpose/ give life meaning We are making a difference! Burdensomeness The world would be better off without me
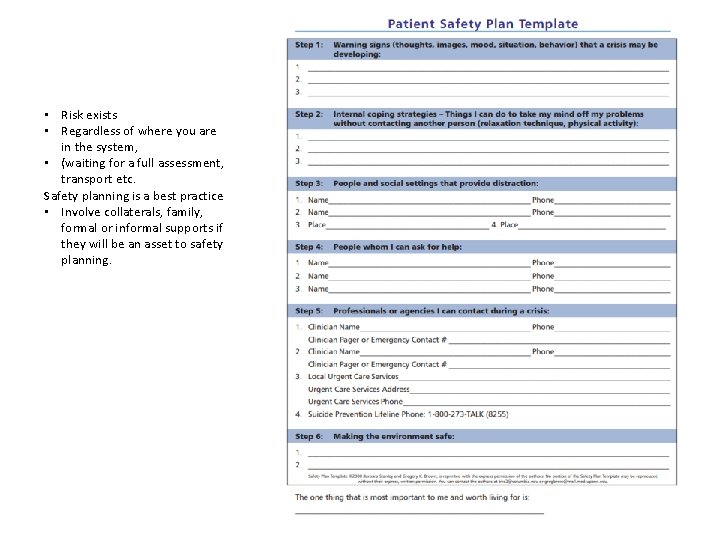
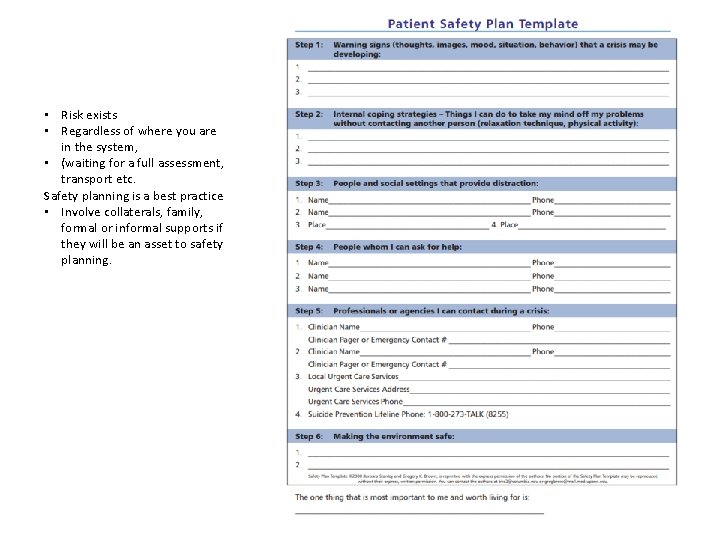
• Risk exists • Regardless of where you are in the system, • (waiting for a full assessment, transport etc. Safety planning is a best practice • Involve collaterals, family, formal or informal supports if they will be an asset to safety planning.

Connection • Community Connection inversely linked to suicide and other negative health outcomes.

Free Resources • Sources of Strength (comprehensive youthfocused) • Gatekeeper trainings like Question, Persuade, Refer (QPR) and Counseling on Access to Lethal Means (CALM) • Zero Suicide Toolkit Resources • Statewide Coalition and statewide network of resources
What you can do today • Put the National Suicide Prevention Lifeline in your phone • 1. 800. 273. 8255 • Not be afraid to ask about suicide and take action • Join the ND Suicide Prevention Coalition • Contact Darcie, Patrick, or Alison about training opportunities.
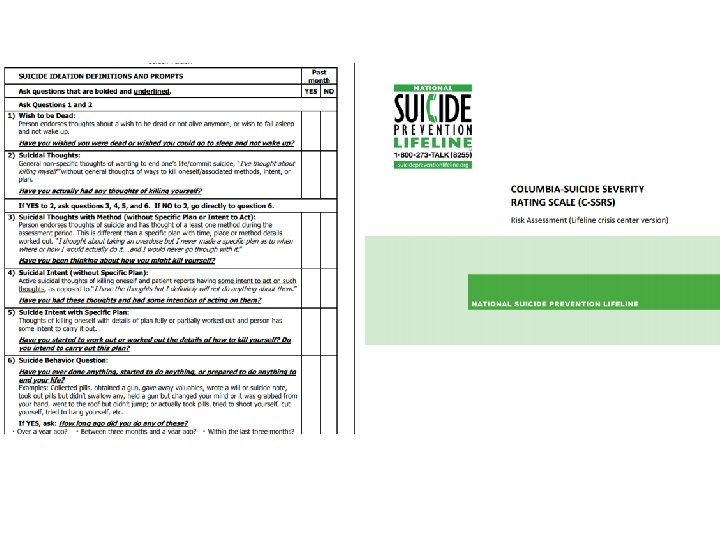
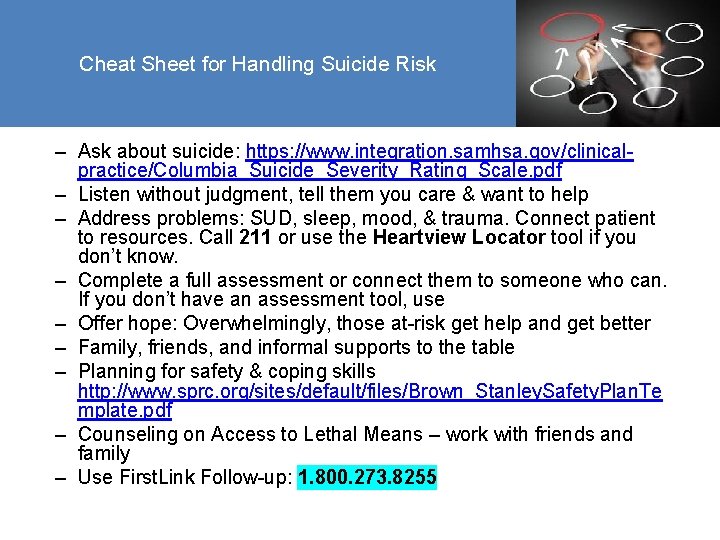
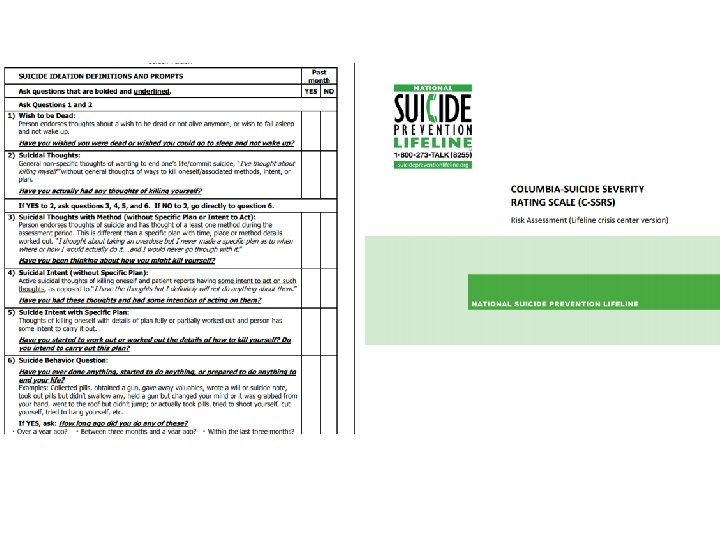
Cheat Sheet for Handling Suicide Risk – Ask about suicide: https: //www. integration. samhsa. gov/clinicalpractice/Columbia_Suicide_Severity_Rating_Scale. pdf – Listen without judgment, tell them you care & want to help – Address problems: SUD, sleep, mood, & trauma. Connect patient to resources. Call 211 or use the Heartview Locator tool if you don’t know. – Complete a full assessment or connect them to someone who can. If you don’t have an assessment tool, use – Offer hope: Overwhelmingly, those at-risk get help and get better – Family, friends, and informal supports to the table – Planning for safety & coping skills http: //www. sprc. org/sites/default/files/Brown_Stanley. Safety. Plan. Te mplate. pdf – Counseling on Access to Lethal Means – work with friends and family – Use First. Link Follow-up: 1. 800. 273. 8255
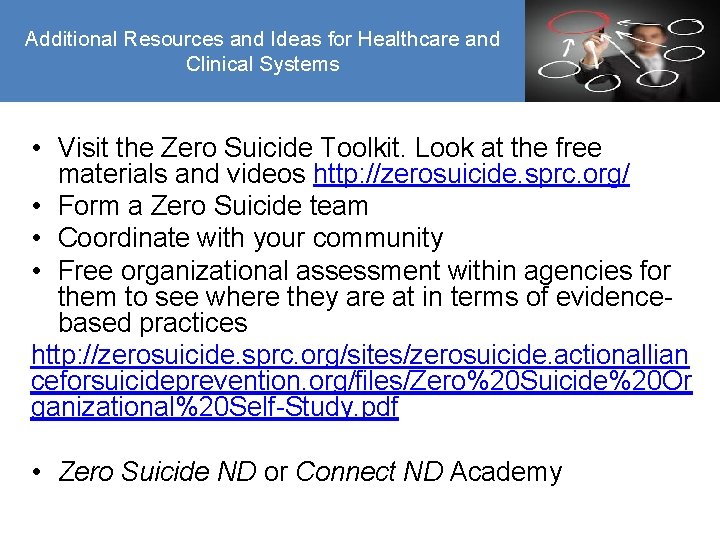
Additional Resources and Ideas for Healthcare and Clinical Systems • Visit the Zero Suicide Toolkit. Look at the free materials and videos http: //zerosuicide. sprc. org/ • Form a Zero Suicide team • Coordinate with your community • Free organizational assessment within agencies for them to see where they are at in terms of evidencebased practices http: //zerosuicide. sprc. org/sites/zerosuicide. actionallian ceforsuicideprevention. org/files/Zero%20 Suicide%20 Or ganizational%20 Self-Study. pdf • Zero Suicide ND or Connect ND Academy
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. Allen, J. , Levintova, M. , & Mohatt, G. (2011). Suicide and alcohol-related disorders in the U. S. arctic: Boosting research to address a primary determinant of health disparities. International Journal of Circumpolar Health, 70(5), 473 -487. doi: 1134 [pii] Anestis, M. D. , & Anestis, J. C. (2015). Suicide rates and state laws regulating access and exposure to handguns. American Journal of Public Health, 105(10), 2049 -2058. doi: 10. 2105/AJPH. 2015. 302753 [doi] Bagge, C. L. , & Borges, G. (2017). Acute substance use as a warning sign for suicide attempts: A case-crossover examination of the 48 hours prior to a recent suicide attempt. The Journal of Clinical Psychiatry, 78(6), 691 -696. doi: 10. 4088/JCP. 15 m 10541 [doi] Bentham, G. (1986). Proximity to hospital and mortality from motor vehicle traffic accidents. Social Science & Medicine (1982), 23(10), 1021 -1026. Bridges, F. S. (2004). Gun control law (bill C-17), suicide, and homicide in canada. Psychological Reports, 94(3 Pt 1), 819 -826. doi: 10. 2466/pr 0. 94. 3. 819 -826 [doi] Carr, B. G. , Nance, M. L. , Branas, C. C. , Wolff, C. S. , Kallan, M. J. , Myers, S. R. , & Wiebe, D. J. (2012). Unintentional firearm death across the urban-rural landscape in the united states. The Journal of Trauma and Acute Care Surgery, 73(4), 1006 -1010. doi: 10. 1097/TA. 0 b 013 e 318265 d 10 a Chen, C. , Yeh, H. , Huang, N. , & Lin, Y. (2014). Socioeconomic and clinical characteristics associated with repeat suicide attempts among young people. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 54(5), 550 -557. doi: 10. 1016/j. jadohealth. 2013. 10. 008 Chung, D. T. , Ryan, C. J. , Hadzi-Pavlovic, D. , Singh, S. P. , Stanton, C. , & Large, M. M. (2017). Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry, 74(7), 694 -702. doi: 10. 1001/jamapsychiatry. 2017. 1044 Fontanella, C. A. , Hiance-Steelesmith, D. L. , Phillips, G. S. , Bridge, J. A. , Lester, N. , Sweeney, H. A. , & Campo, J. V. (2015). Widening rural-urban disparities in youth suicides, united states, 19962010. JAMA Pediatrics, 169(5), 466 -473. doi: 10. 1001/jamapediatrics. 2014. 3561 [doi] Garcia-Williams, A. G. , Moffitt, L. , & Kaslow, N. J. (2014). Mental health and suicidal behavior among graduate students. Academic Psychiatry: The Journal of the American Association of Directors of Psychiatric Residency Training and the Association for Academic Psychiatry, 38 (5), 554 -560. doi: 10. 1007/s 40596 -014 -0041 -y Heisel, M. J. , Duberstein, P. R. , Lyness, J. M. , & Feldman, M. D. (2010). Screening for suicide ideation among older primary care patients. Journal of the American Board of Family Medicine: JABFM, 23(2), 260 -269. doi: 10. 3122/jabfm. 2010. 02. 080163 Heron, M. (2016). Deaths: Leading causes for 2013. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 65(2), 1 -95. Hsu, C. , Chang, S. , Lee, E. S. T. , & Yip, P. S. F. (2015). "Geography of suicide in hong kong: Spatial patterning, and socioeconomic correlates and inequalities". Social Science & Medicine (1982), 130, 190 -203. doi: 10. 1016/j. socscimed. 2015. 02. 019 Joiner, T. E. (2005). Why people die by suicide. Cambridge, Mass. : Harvard University Press. Kegler, S. R. , Stone, D. M. , & Holland, K. M. (2017 a). Trends in suicide by level of urbanization - united states, 1999 -2015. MMWR: Morbidity & Mortality Weekly Report, 66(10), 270 -273. doi: 10. 15585/mmwr. mm 6610 a 2 Luoma, J. B. , Martin, C. E. , & Pearson, J. L. (2002). Contact with mental health and primary care providers before suicide: A review of the evidence. The American Journal of Psychiatry, 159(6), 909 -916. doi: 10. 1176/appi. ajp. 159. 6. 909 Mc. Carthy, J. F. , Blow, F. C. , Ignacio, R. V. , Ilgen, M. A. , Austin, K. L. , & Valenstein, M. (2012). Suicide among patients in the veterans affairs health system: Rural-urban differences in rates, risks, and methods. American Journal of Public Health, 102 Suppl 1(S 1), S 117. doi: 10. 2105/AJPH. 2011. 300463 Mc. Carthy, M. (2015). Youth suicide rate in rural US is nearly double that of urban areas, study finds. BMJ (Clinical Research Ed. ), 350, h 1376. doi: 10. 1136/bmj. h 1376 [doi] Mota, N. , Elias, B. , Tefft, B. , Medved, M. , Munro, G. , & Sareen, J. (2012). Correlates of suicidality: Investigation of a representative sample of manitoba first nations adolescents. American Journal of Public Health, 102(7), 1353 -1361. doi: 10. 2105/AJPH. 2011. 300385 [doi] North Dakota Department of Health, Vital Statistics. (2016). North Dakota Resident Vital Event Summary Data 2002 to 2016. Page 9. Online resource http: //www. ndhealth. gov/vital/pubs/2016 VES. pdf Schaffer, A. , Sinyor, M. , Kurdyak, P. , Vigod, S. , Sareen, J. , Reis, C. , . . . Cheung, A. (2016). Population-based analysis of health care contacts among suicide decedents: Identifying opportunities for more targeted suicide prevention strategies. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 15(2), 135 -145. doi: 10. 1002/wps. 20321 Shepard, D. S. , Gurewich, D. , Lwin, A. K. , Reed, G. A. , & Silverman, M. M. (2016). Suicide and suicidal attempts in the united states: Costs and policy implications. Suicide & Life-Threatening Behavior, 46(3), 352 -362. Simkin, S. , Hawton, K. , Sutton, L. , Gunnell, D. , Bennewith, O. , & Kapur, N. (2005). Co-proxamol and suicide: Preventing the continuing toll of overdose deaths. QJM : Monthly Journal of the Association of Physicians, 98(3), 159 -170. doi: 98/3/159 [pii] Singh, G. K. , & Siahpush, M. (2002). Increasing rural-urban gradients in US suicide mortality, 1970 -1997. American Journal of Public Health, 92(7), 1161 -1167. Sullivan, E. M. , Annest, J. L. , Simon, T. R. , Luo, F. , Dahlberg, L. L. , & Centers for Disease Control and Prevention, (CDC). (2015). Suicide trends among persons aged 10 -24 years--united states, 1994 -2012. MMWR. Morbidity and Mortality Weekly Report, 64(8), 201 -205. doi: mm 6408 a 1 [pii]