Lecture 5 General med2 nd semester Development of
- Slides: 14
Lecture 5 General med_2 nd semester Development of external form of the embryo and fetus. The rule of Hasse Uterine growth during pregnancy Marks of the mature and full-term fetus Multiple pregnancy: mono- and dizygotic twins; arrangements of fetal membranes in twins Position, posture and presentation of the fetus
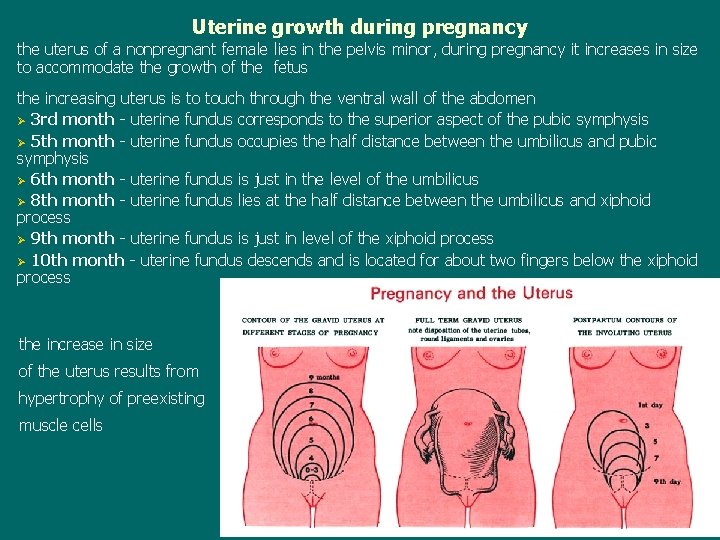
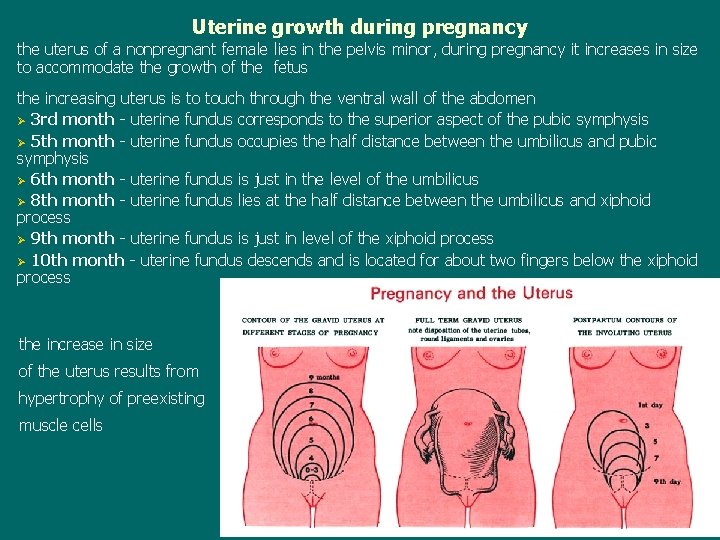
Uterine growth during pregnancy the uterus of a nonpregnant female lies in the pelvis minor, during pregnancy it increases in size to accommodate the growth of the fetus the increasing uterus is to touch through the ventral wall of the abdomen Ø 3 rd month - uterine fundus corresponds to the superior aspect of the pubic symphysis Ø 5 th month - uterine fundus occupies the half distance between the umbilicus and pubic symphysis Ø 6 th month - uterine fundus is just in the level of the umbilicus Ø 8 th month - uterine fundus lies at the half distance between the umbilicus and xiphoid process Ø 9 th month - uterine fundus is just in level of the xiphoid process Ø 10 th month - uterine fundus descends and is located for about two fingers below the xiphoid process the increase in size of the uterus results from hypertrophy of preexisting muscle cells
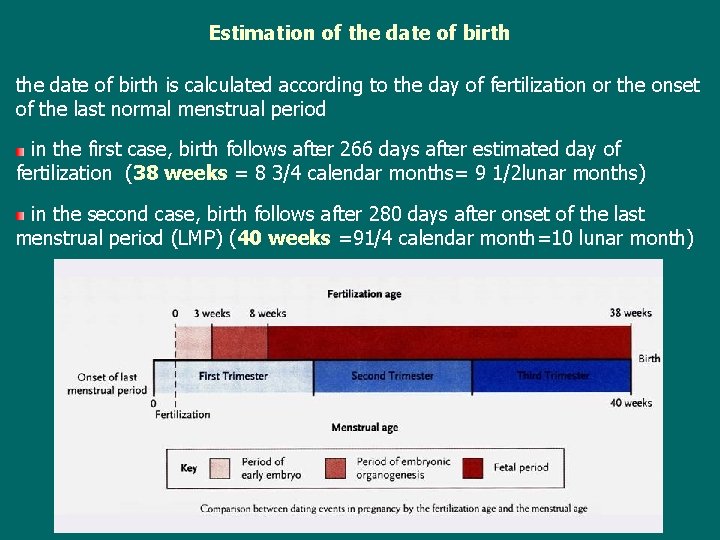
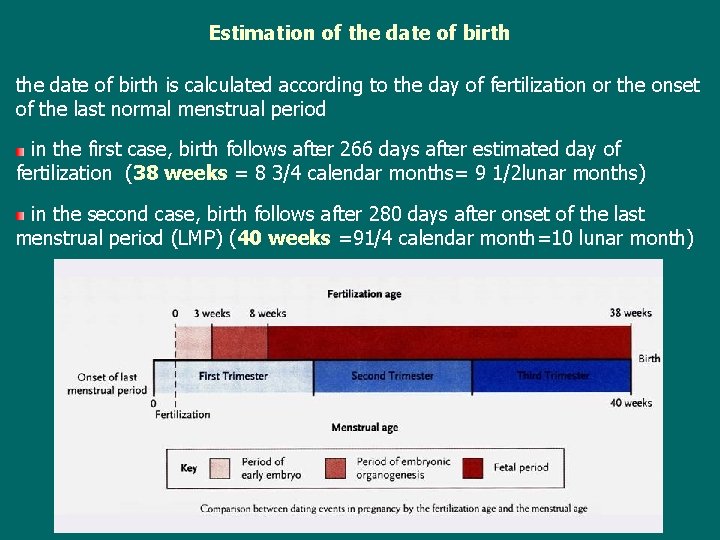
Estimation of the date of birth is calculated according to the day of fertilization or the onset of the last normal menstrual period in the first case, birth follows after 266 days after estimated day of fertilization (38 weeks = 8 3/4 calendar months= 9 1/2 lunar months) in the second case, birth follows after 280 days after onset of the last menstrual period (LMP) (40 weeks =91/4 calendar month=10 lunar month)
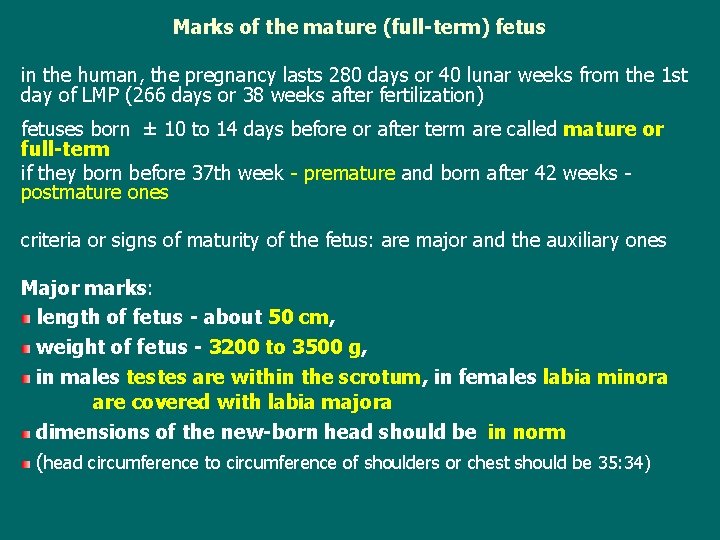
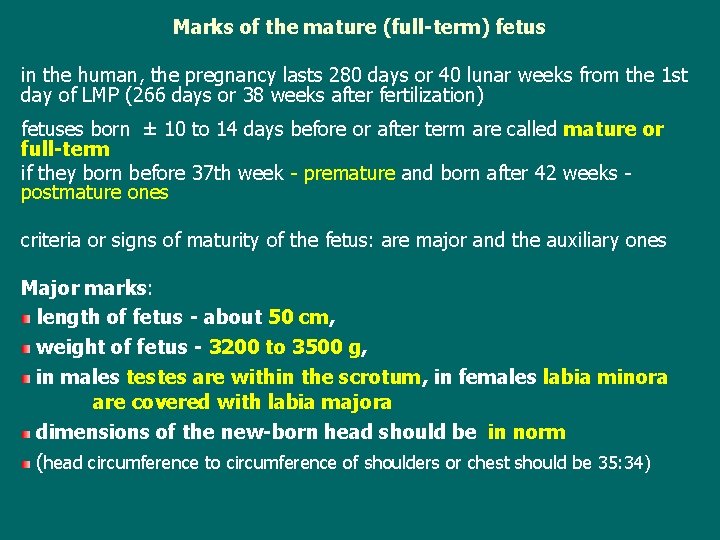
Marks of the mature (full-term) fetus in the human, the pregnancy lasts 280 days or 40 lunar weeks from the 1 st day of LMP (266 days or 38 weeks after fertilization) fetuses born ± 10 to 14 days before or after term are called mature or full-term if they born before 37 th week - premature and born after 42 weeks postmature ones criteria or signs of maturity of the fetus: are major and the auxiliary ones Major marks: length of fetus - about 50 cm, weight of fetus - 3200 to 3500 g, in males testes are within the scrotum, in females labia minora are covered with labia majora dimensions of the new-born head should be in norm (head circumference to circumference of shoulders or chest should be 35: 34)
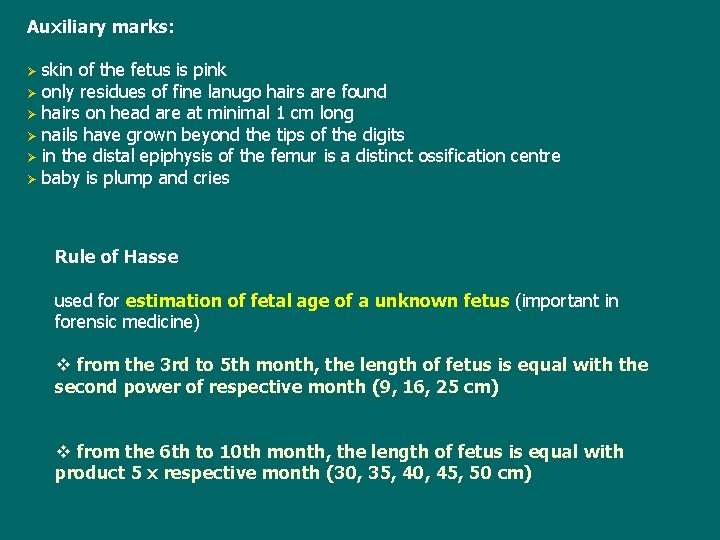
Auxiliary marks: Ø Ø Ø skin of the fetus is pink only residues of fine lanugo hairs are found hairs on head are at minimal 1 cm long nails have grown beyond the tips of the digits in the distal epiphysis of the femur is a distinct ossification centre baby is plump and cries Rule of Hasse used for estimation of fetal age of a unknown fetus (important in forensic medicine) v from the 3 rd to 5 th month, the length of fetus is equal with the second power of respective month (9, 16, 25 cm) v from the 6 th to 10 th month, the length of fetus is equal with product 5 x respective month (30, 35, 40, 45, 50 cm)
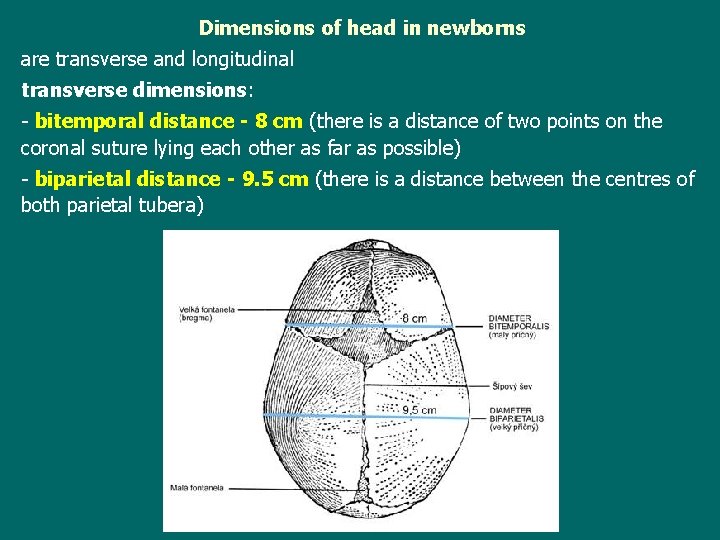
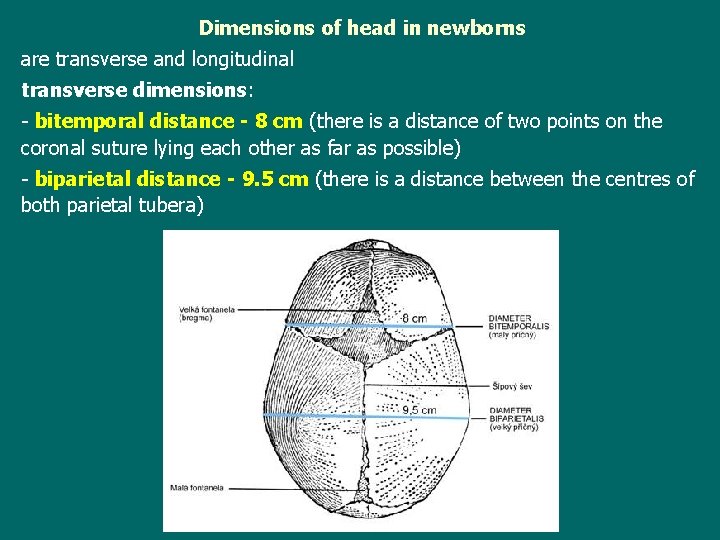
Dimensions of head in newborns are transverse and longitudinal transverse dimensions: - bitemporal distance - 8 cm (there is a distance of two points on the coronal suture lying each other as far as possible) - biparietal distance - 9. 5 cm (there is a distance between the centres of both parietal tubera)
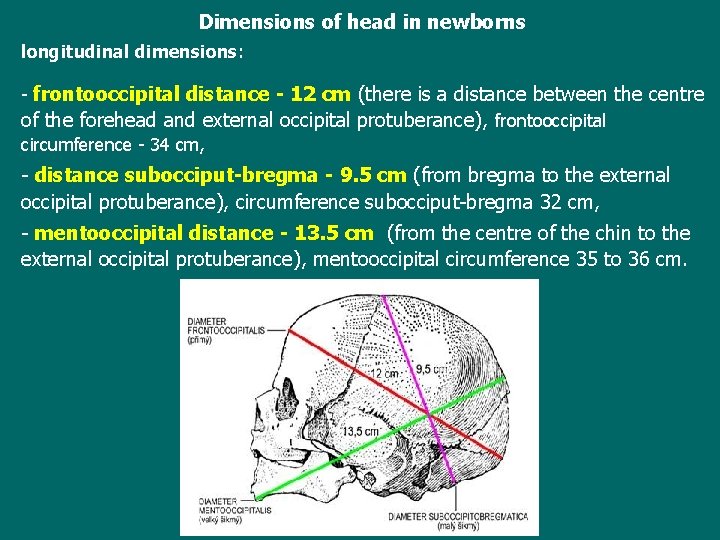
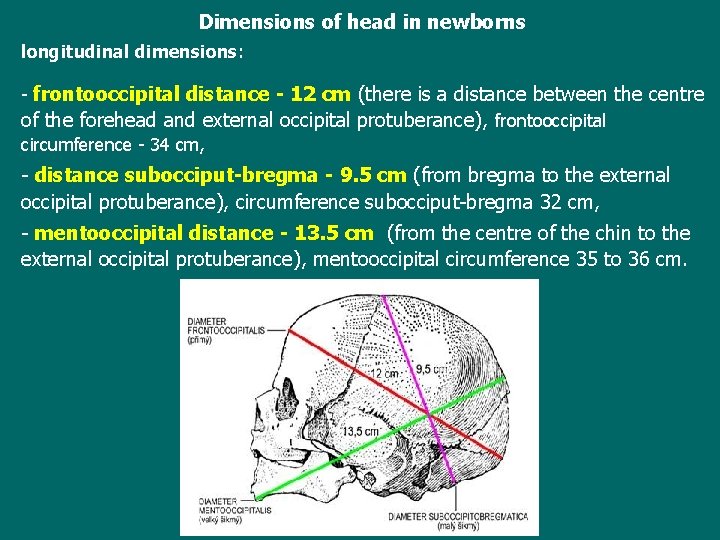
Dimensions of head in newborns longitudinal dimensions: - frontooccipital distance - 12 cm (there is a distance between the centre of the forehead and external occipital protuberance), frontooccipital circumference - 34 cm, - distance subocciput-bregma - 9. 5 cm (from bregma to the external occipital protuberance), circumference subocciput-bregma 32 cm, - mentooccipital distance - 13. 5 cm (from the centre of the chin to the external occipital protuberance), mentooccipital circumference 35 to 36 cm.
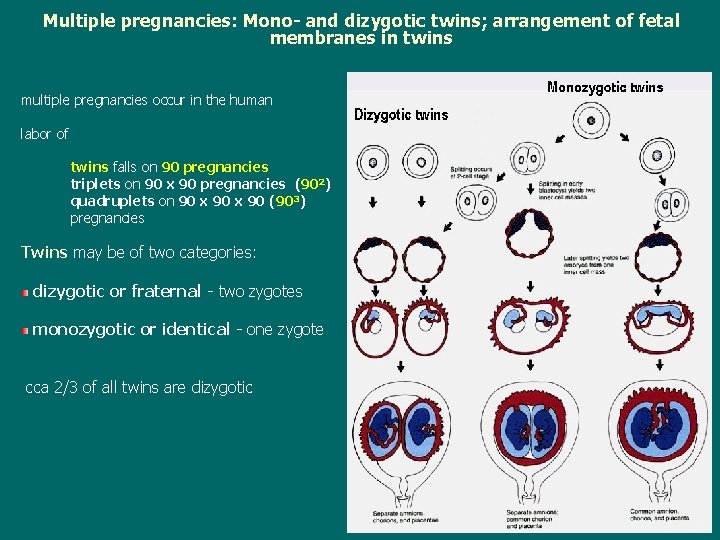
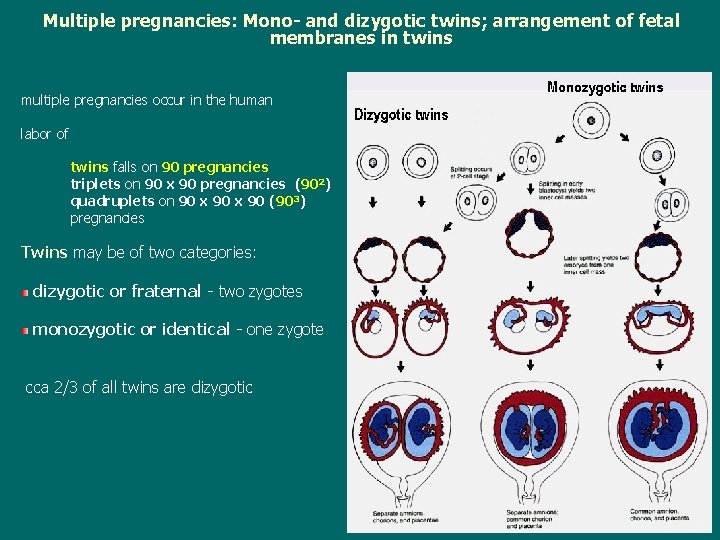
Multiple pregnancies: Mono- and dizygotic twins; arrangement of fetal membranes in twins multiple pregnancies occur in the human labor of twins falls on 90 pregnancies triplets on 90 x 90 pregnancies (902) quadruplets on 90 x 90 (903) pregnancies Twins may be of two categories: dizygotic or fraternal - two zygotes monozygotic or identical - one zygote cca 2/3 of all twins are dizygotic
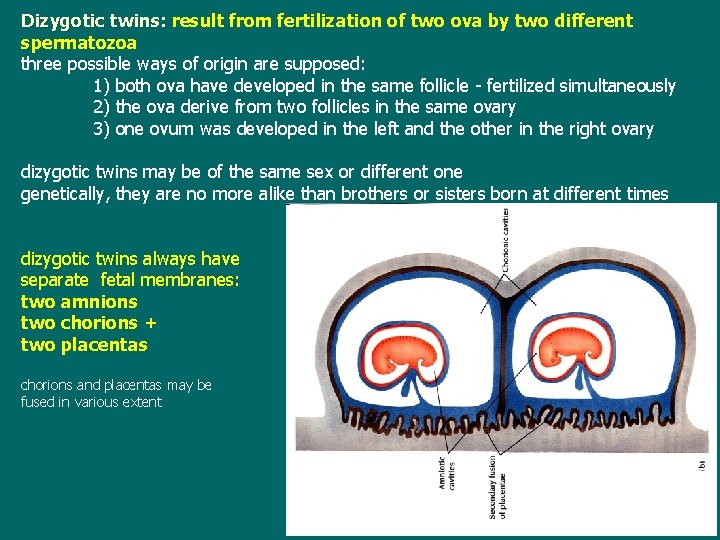
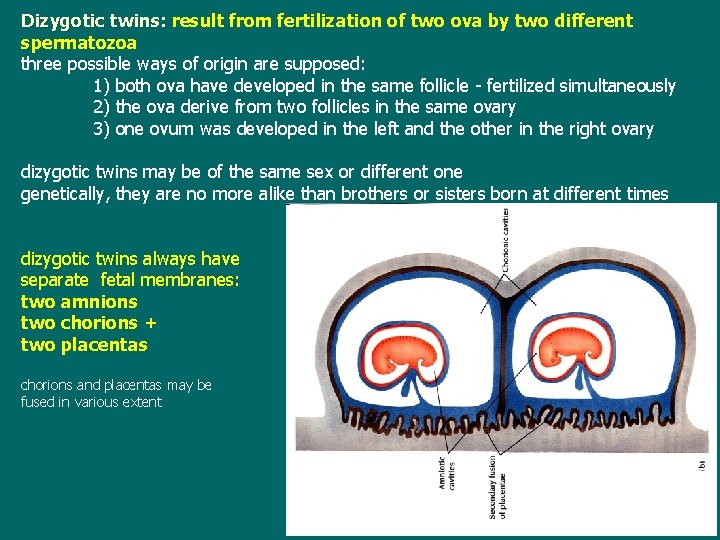
Dizygotic twins: result from fertilization of two ova by two different spermatozoa three possible ways of origin are supposed: 1) both ova have developed in the same follicle - fertilized simultaneously 2) the ova derive from two follicles in the same ovary 3) one ovum was developed in the left and the other in the right ovary dizygotic twins may be of the same sex or different one genetically, they are no more alike than brothers or sisters born at different times dizygotic twins always have separate fetal membranes: two amnions two chorions + two placentas chorions and placentas may be fused in various extent
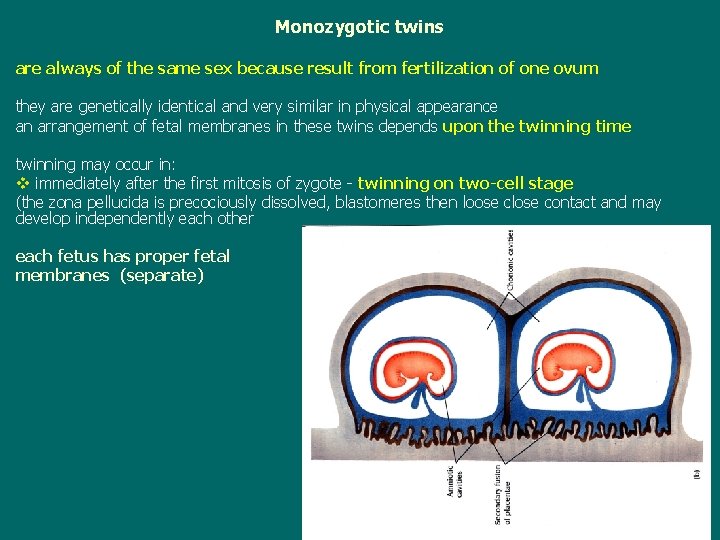
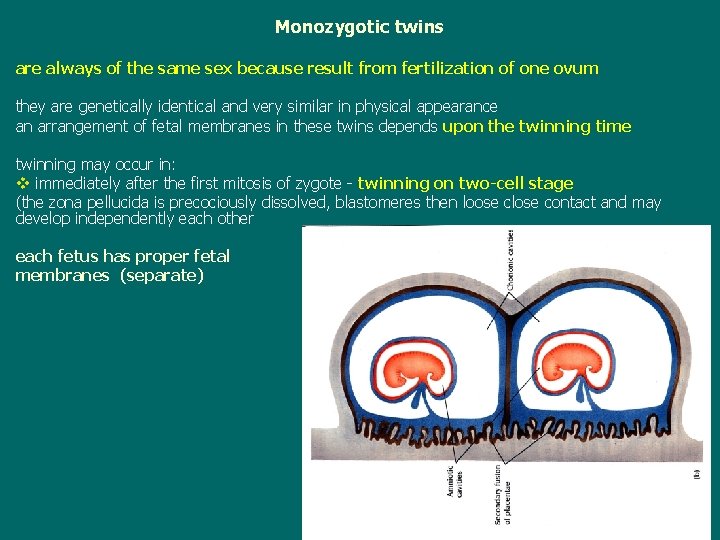
Monozygotic twins are always of the same sex because result from fertilization of one ovum they are genetically identical and very similar in physical appearance an arrangement of fetal membranes in these twins depends upon the twinning time twinning may occur in: v immediately after the first mitosis of zygote - twinning on two-cell stage (the zona pellucida is precociously dissolved, blastomeres then loose close contact and may develop independently each other each fetus has proper fetal membranes (separate)
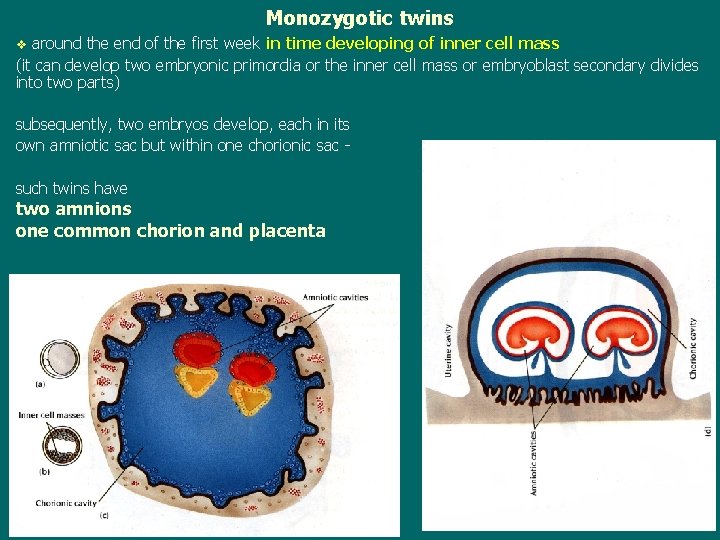
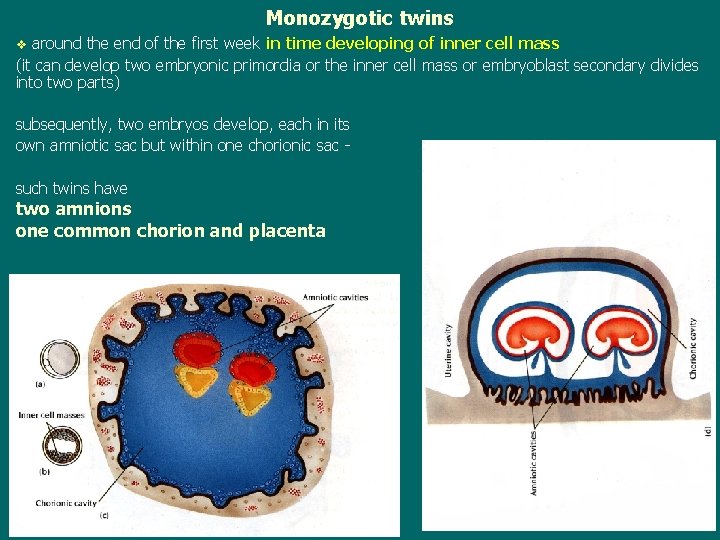
Monozygotic twins around the end of the first week in time developing of inner cell mass (it can develop two embryonic primordia or the inner cell mass or embryoblast secondary divides into two parts) v subsequently, two embryos develop, each in its own amniotic sac but within one chorionic sac such twins have two amnions one common chorion and placenta
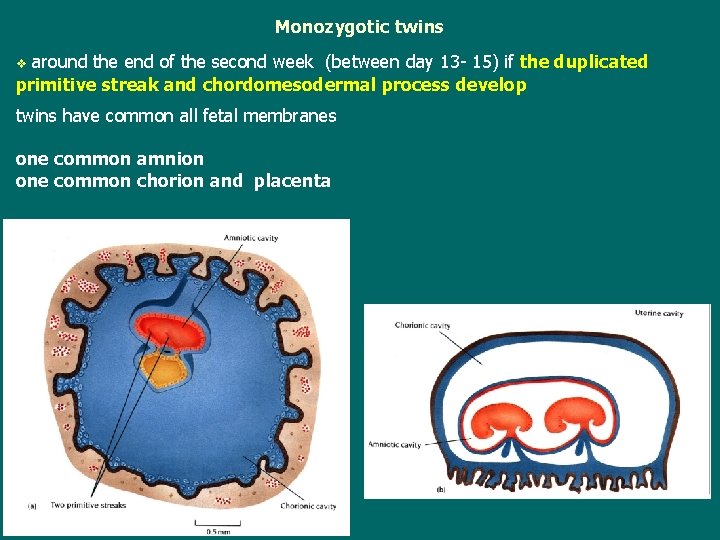
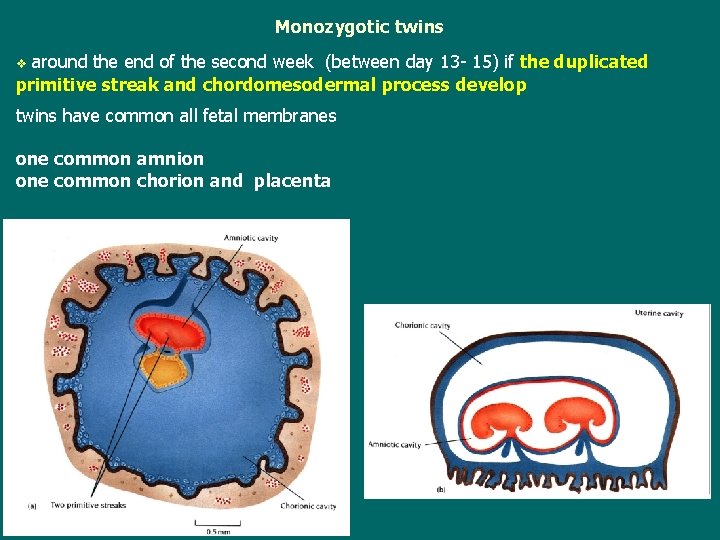
Monozygotic twins around the end of the second week (between day 13 - 15) if the duplicated primitive streak and chordomesodermal process develop v twins have common all fetal membranes one common amnion one common chorion and placenta
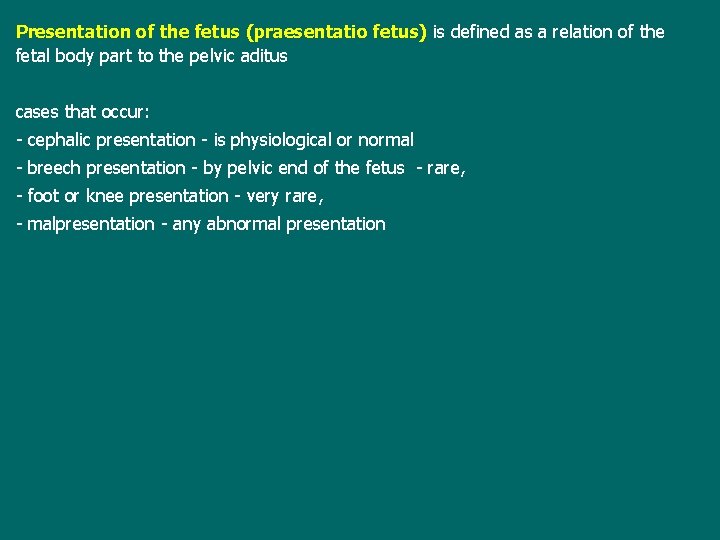
Position, posture and presentation of the fetus (in the uterus) Position of the fetus (situs fetus) is defined as a relation of its longitudinal axis to the longitudinal axis of the uterus 3 positions are distinguished: - longitudinal position - both axes run parallel - in 99, 5 per cent - transverse position - both axes are rectangle - oblique position - axes are passing (instable position) The longitudinal position: by head (96, 5 %) or by breech (pelvic end of the fetus) - 3 %. The back of the fetus is most often oriented to the left edge of the uterus Posture of the fetus (habitus fetus) is defined as a relation of fetal body parts to each other may be regular and irregular posture = the head is in flexion, the chin is in close contact with the chest, upper and lower limbs are flexed in both articulations and are folded
Presentation of the fetus (praesentatio fetus) is defined as a relation of the fetal body part to the pelvic aditus cases that occur: - cephalic presentation - is physiological or normal - breech presentation - by pelvic end of the fetus - rare, - foot or knee presentation - very rare, - malpresentation - any abnormal presentation