Introduction to Trans Health Jaye Watts LICSW Trans



- Slides: 31
Introduction to Trans* Health Jaye Watts, LICSW Trans* Health Program Director jayew@thundermisthealth. org

Thundermist Health Center 3 communities: Woonsocket, West Warwick & Wakefield 42, 000+ patients in 2015 Federally Qualified Health Center Patient Centered Medical Home Medical, Dental, Behavioral Health, Case Management Trans Health Program Started in 2015 18 Primary Care Providers 515 patients across all sites New! Expansion to pediatric work
Health and Wellness Programming Trans* Swim Night Trans* Yoga
Why a Trans* Health Access Team? Vastly underserved group of people Providers not trained in trans* health needs Trans* people face a high rate of discrimination and violence Limited # of resources in state Increasing visibility Need for culturally competent professionals New population estimate: 4, 250 Transgender people in Rhode Island 1 1 Williams institute, UCLA (2016)
Stress of Accessing Health Care 2015 US Transgender Survey (n=27, 715)1 In the past year: 24% had to teach their health care provider about transgender people to get appropriate care 23% of respondents did not see a doctor when they needed to because of fear of being mistreated as a transgender person 33% of those who saw a health care provider had at least one negative experience related to being transgender 39% of respondents were currently experiencing serious psychological distress, nearly eight times the rate in the U. S. population (5%). 40% of respondents have attempted suicide in their lifetime— the national average is 4. 6%. NCTE, 2016
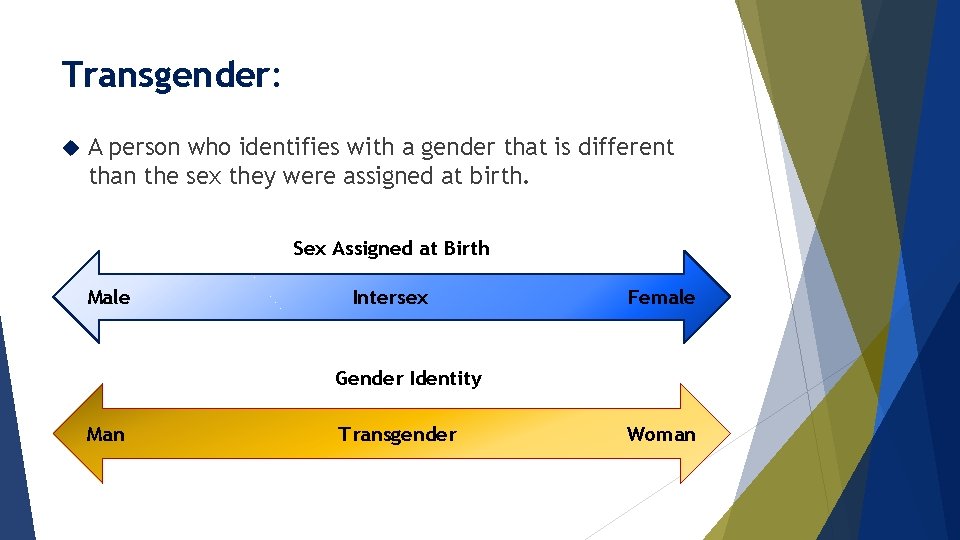
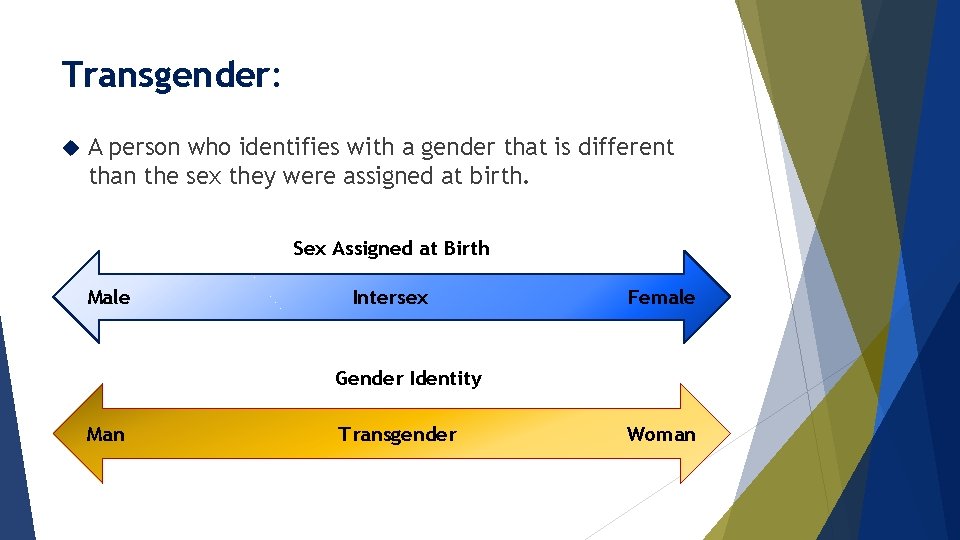
Transgender: A person who identifies with a gender that is different than the sex they were assigned at birth. Sex Assigned at Birth Male Intersex Female Gender Identity Man Transgender Woman
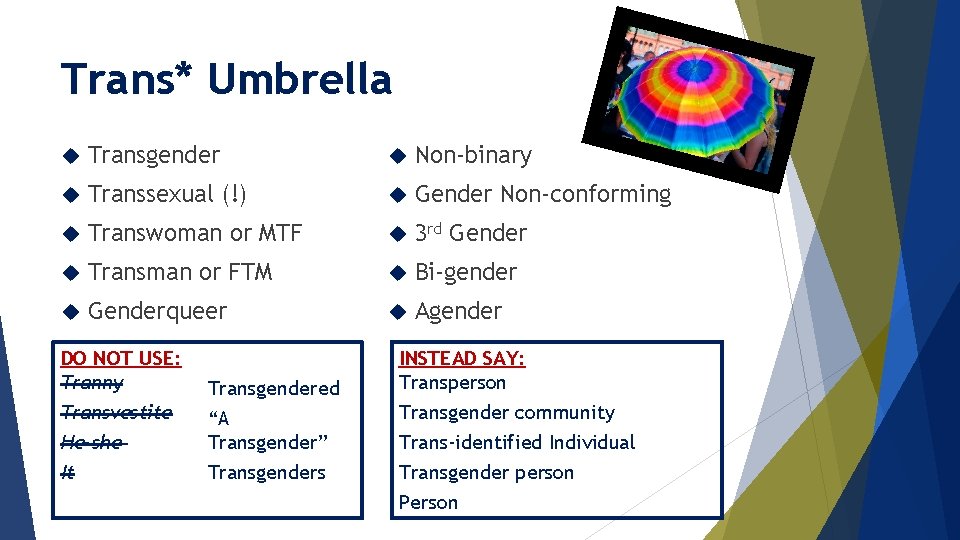
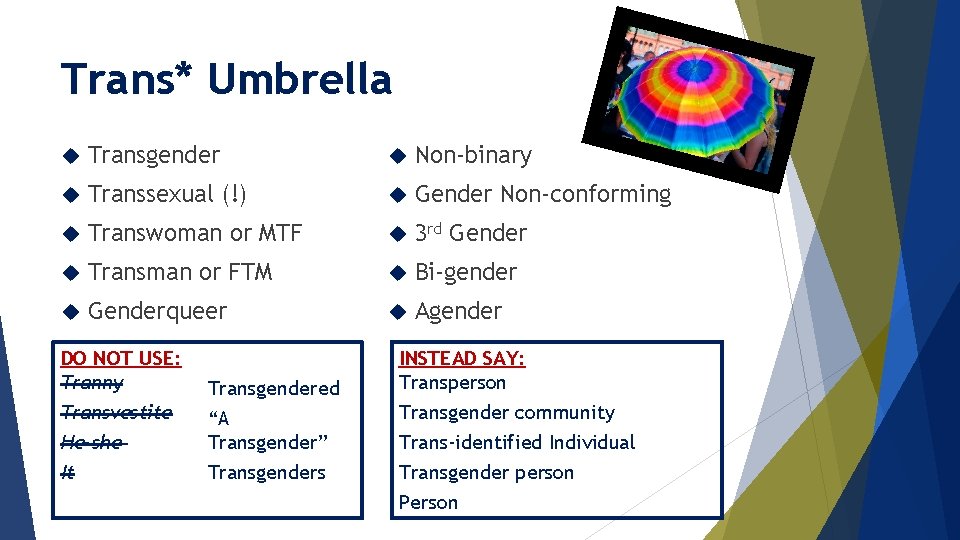
Trans* Umbrella Transgender Non-binary Transsexual (!) Gender Non-conforming Transwoman or MTF 3 rd Gender Transman or FTM Bi-gender Genderqueer Agender DO NOT USE: Tranny Transvestite He-she It Transgendered “A Transgender” Transgenders INSTEAD SAY: Transperson Transgender community Trans-identified Individual Transgender person Person
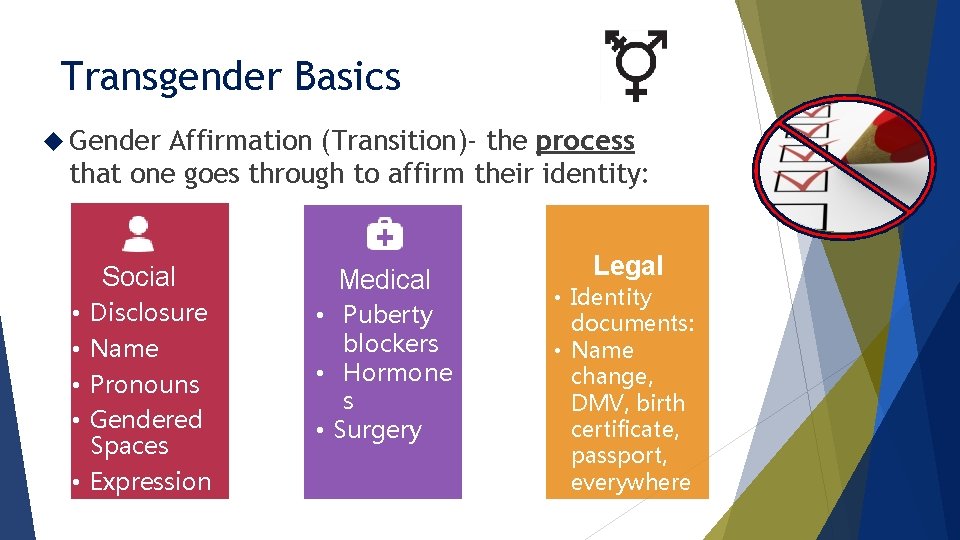
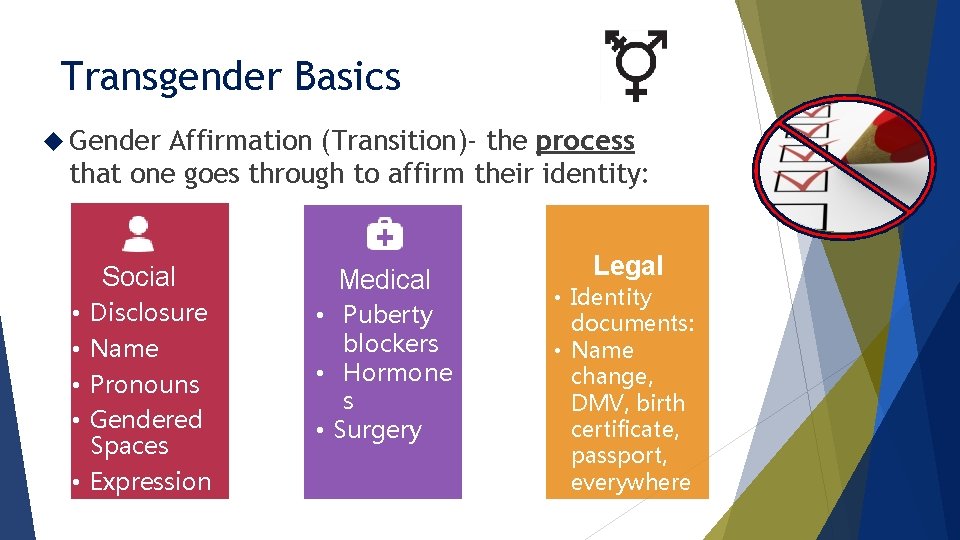
Transgender Basics Gender Affirmation (Transition)- the process that one goes through to affirm their identity: Social dical Disclosure Name Pronouns Gendered Spaces • Expression • • Medical • Puberty blockers • Hormone s • Surgery Legal • Identity documents: • Name change, DMV, birth certificate, passport, everywhere
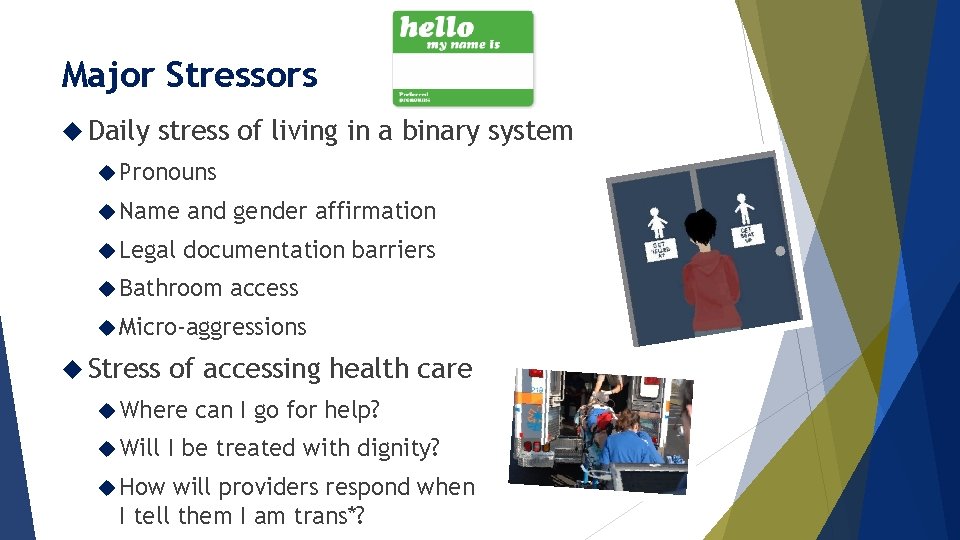
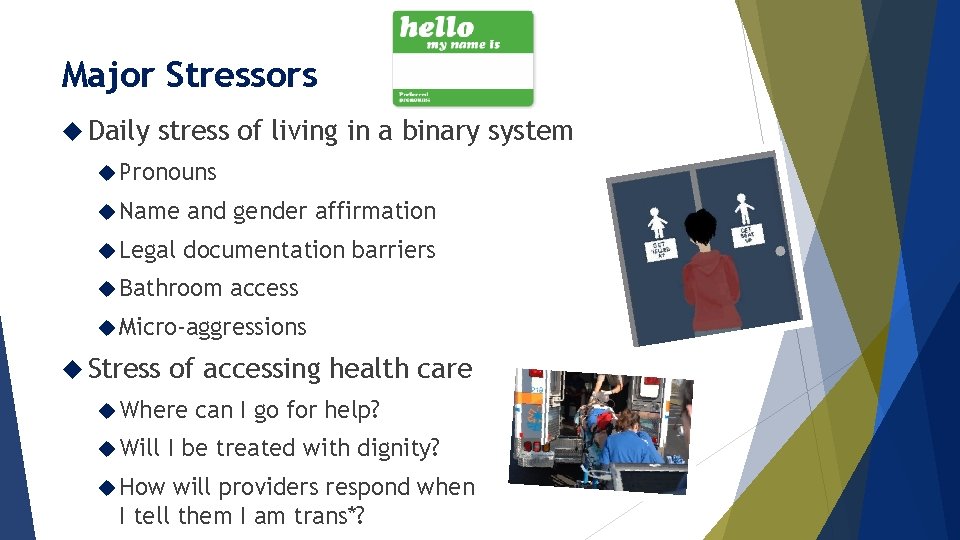
Major Stressors Daily stress of living in a binary system Pronouns Name and gender affirmation Legal documentation barriers Bathroom access Micro-aggressions Stress of accessing health care Where Will How can I go for help? I be treated with dignity? will providers respond when I tell them I am trans*?
What is Trans-Affirmative Health Care? Able to accurately report identity on existing documentation Be addressed and identified by preferred name & pronouns Access to gender neutral restrooms Trauma informed/sensitive care Interact with affirming staff from beginning to end Medical providers who are knowledgeable or willing to learn Receive care that is free of questions or exams unrelated to the presenting problem
Trans* Health Access Team: Informed Consent Practice Model UCSF Primary Care Protocol & Fenway Health Model Provider Assessment Consent forms BH referral only if needed (not contingent on starting hormones unless ability to consent to treatment is compromised)
Medical Primer Hormone treatment: Pubertal Gn. RH Blocker: (pre/peri puberty) Analogs Feminizing: Estrogen: Pills, patches, creams, injections (anti-androgen) Progesterone: Spironolactone, Finasteride: pills, creams Masculinizing: Testosterone: injection, gels, patches, pellets (implant) Fenway Health (2015); Deutsch(2016)
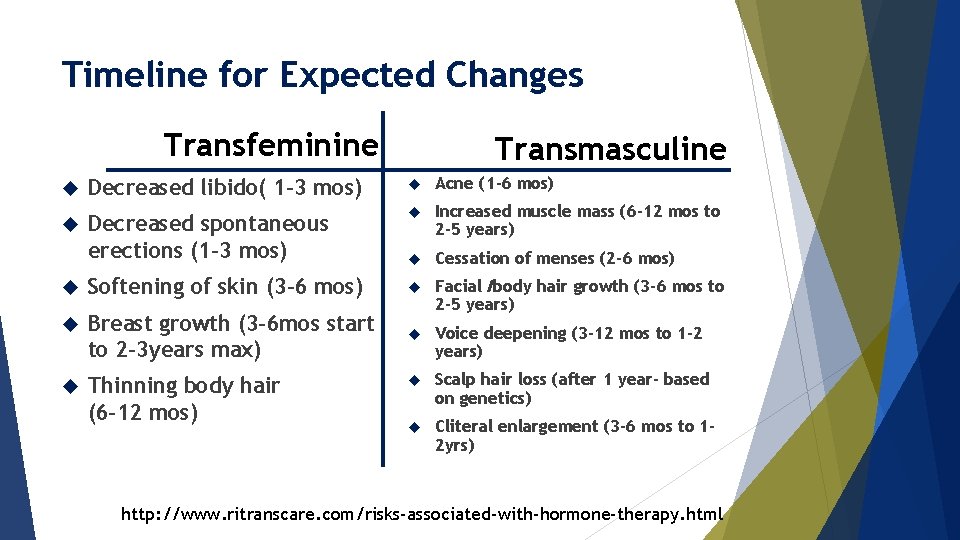
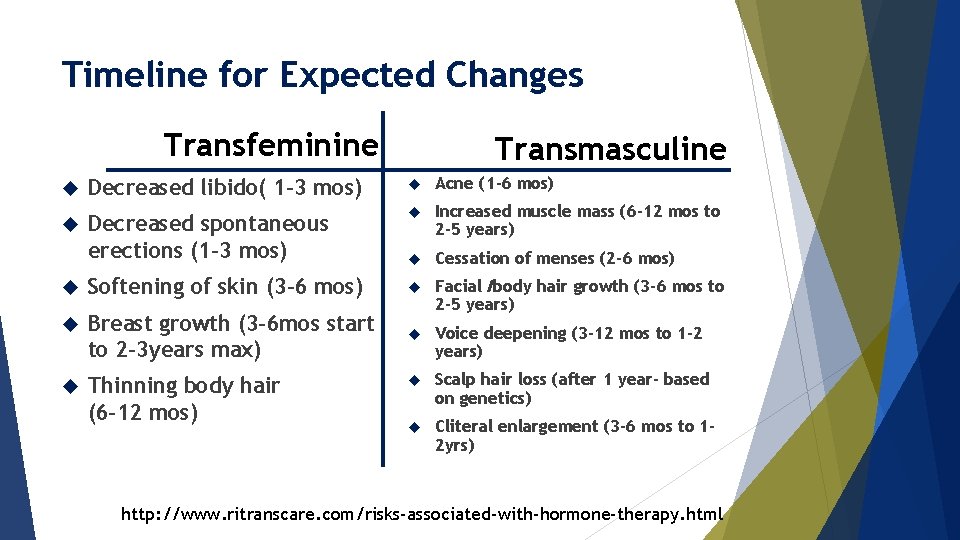
Timeline for Expected Changes Transfeminine Transmasculine Decreased libido( 1 -3 mos) Acne (1 -6 mos) Decreased spontaneous erections (1 -3 mos) Increased muscle mass (6 -12 mos to 2 -5 years) Cessation of menses (2 -6 mos) Softening of skin (3 -6 mos) Breast growth (3 -6 mos start to 2 -3 years max) Facial /body hair growth (3 -6 mos to 2 -5 years) Voice deepening (3 -12 mos to 1 -2 years) Thinning body hair (6 -12 mos) Scalp hair loss (after 1 year- based on genetics) Cliteral enlargement (3 -6 mos to 12 yrs) http: //www. ritranscare. com/risks-associated-with-hormone-therapy. html
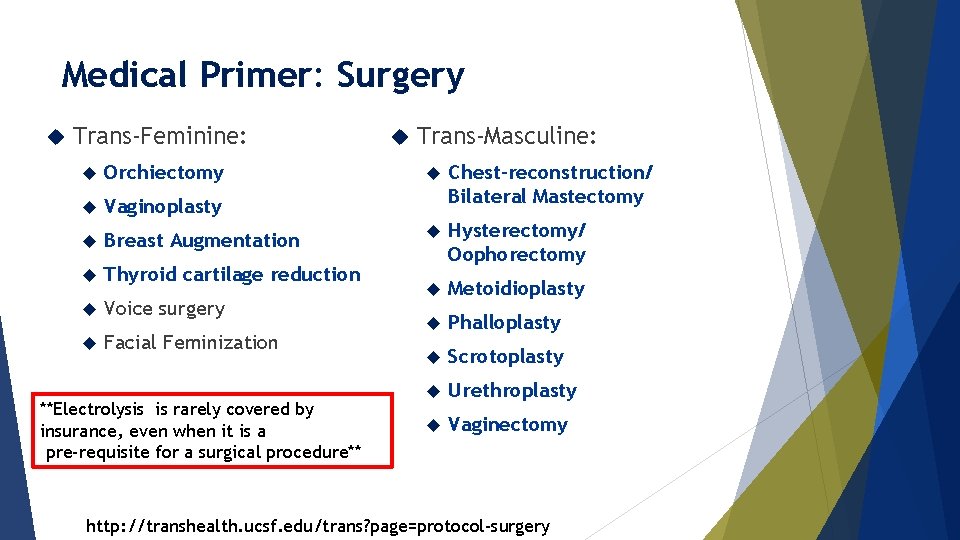
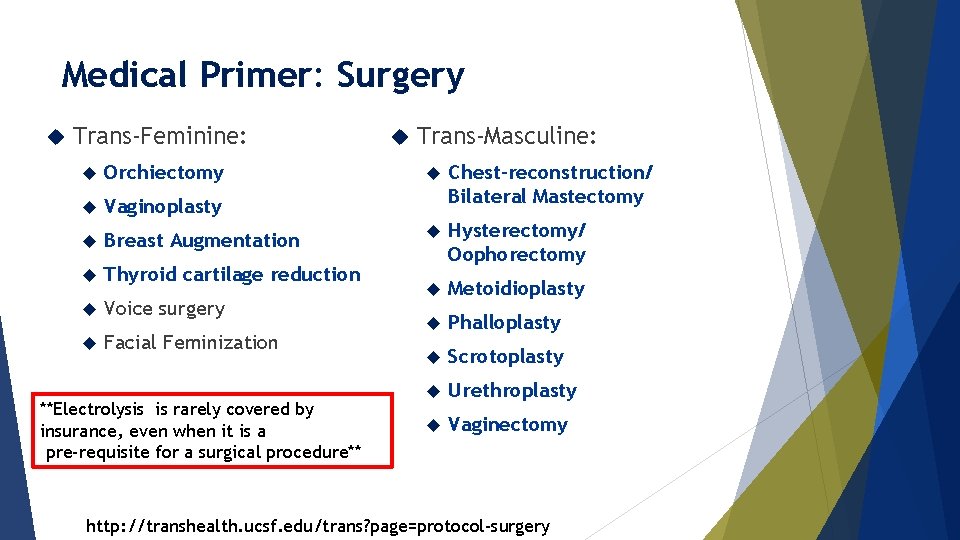
Medical Primer: Surgery Trans-Feminine: Orchiectomy Vaginoplasty Breast Augmentation Thyroid cartilage reduction Voice surgery Facial Feminization **Electrolysis is rarely covered by insurance, even when it is a pre-requisite for a surgical procedure** Trans-Masculine: Chest-reconstruction/ Bilateral Mastectomy Hysterectomy/ Oophorectomy Metoidioplasty Phalloplasty Scrotoplasty Urethroplasty Vaginectomy http: //transhealth. ucsf. edu/trans? page=protocol-surgery
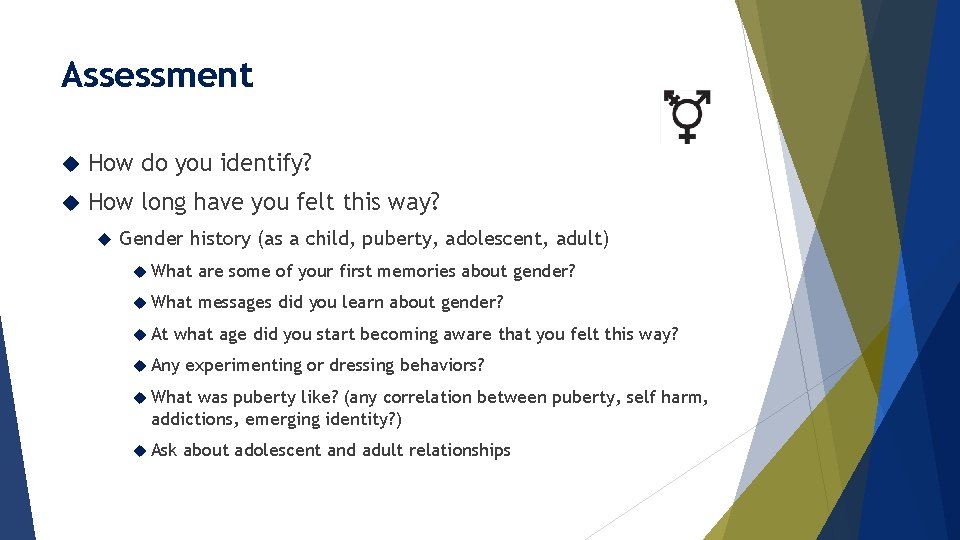
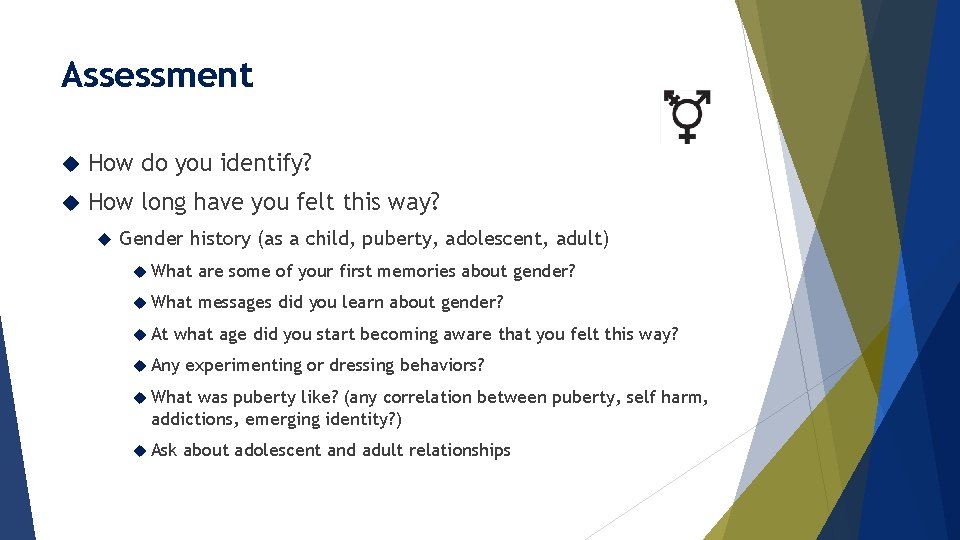
Assessment How do you identify? How long have you felt this way? Gender history (as a child, puberty, adolescent, adult) What are some of your first memories about gender? What messages did you learn about gender? At what age did you start becoming aware that you felt this way? Any experimenting or dressing behaviors? What was puberty like? (any correlation between puberty, self harm, addictions, emerging identity? ) Ask about adolescent and adult relationships
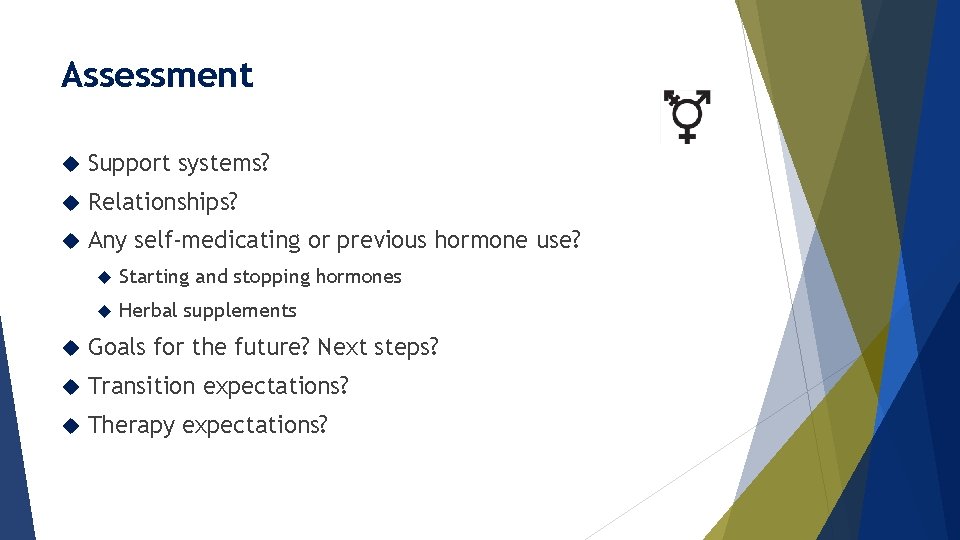
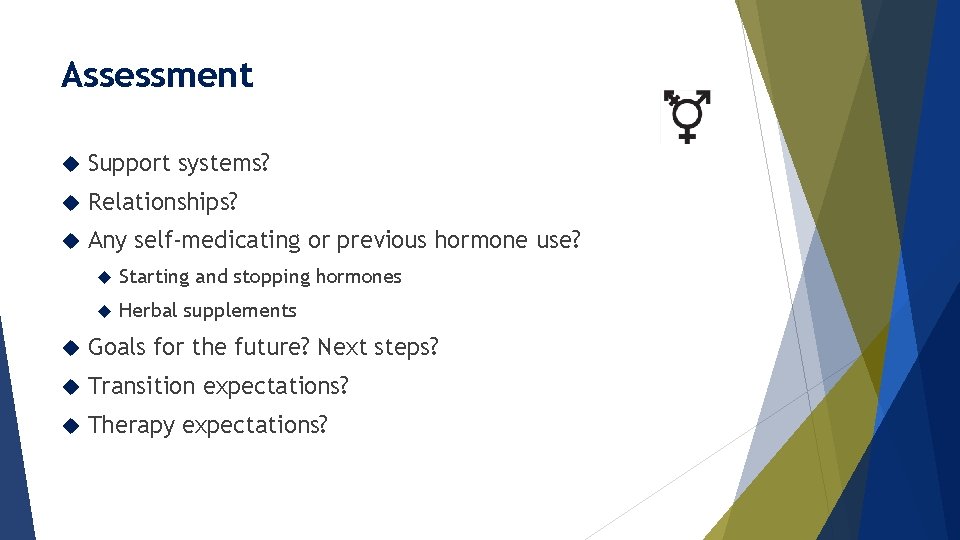
Assessment Support systems? Relationships? Any self-medicating or previous hormone use? Starting and stopping hormones Herbal supplements Goals for the future? Next steps? Transition expectations? Therapy expectations?
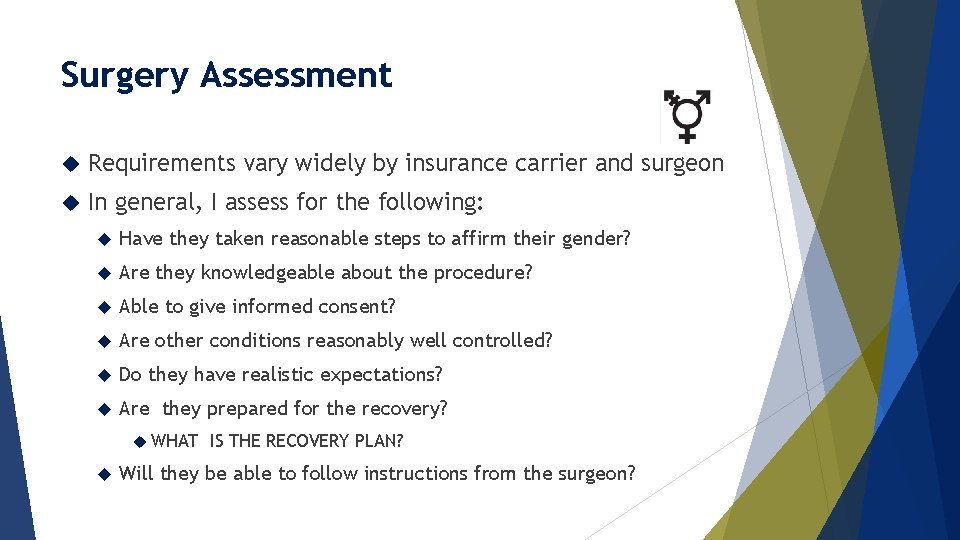
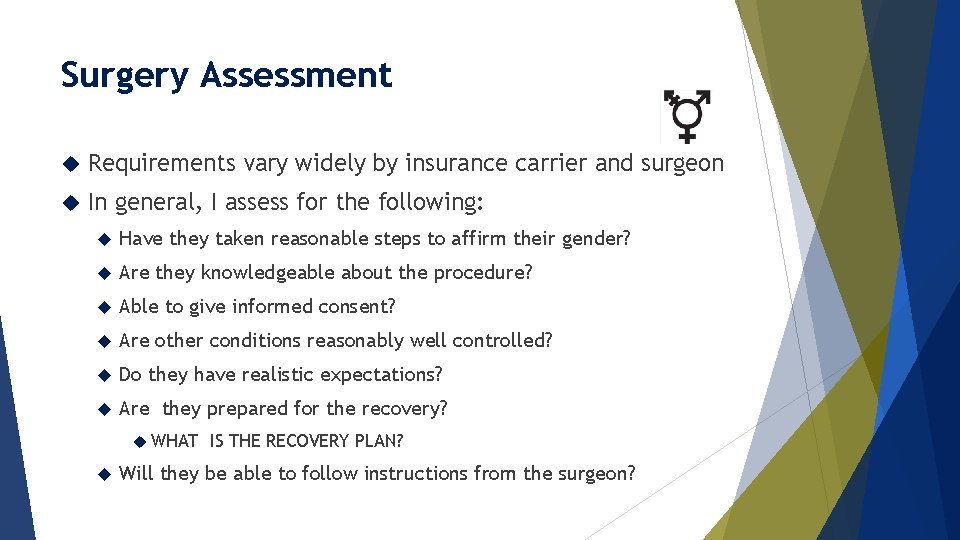
Surgery Assessment Requirements vary widely by insurance carrier and surgeon In general, I assess for the following: Have they taken reasonable steps to affirm their gender? Are they knowledgeable about the procedure? Able to give informed consent? Are other conditions reasonably well controlled? Do they have realistic expectations? Are they prepared for the recovery? WHAT IS THE RECOVERY PLAN? Will they be able to follow instructions from the surgeon?
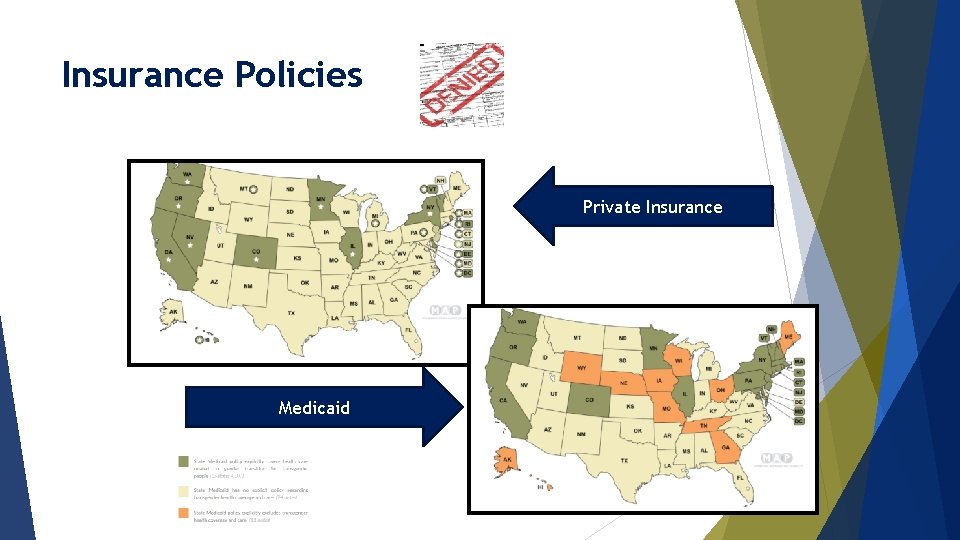
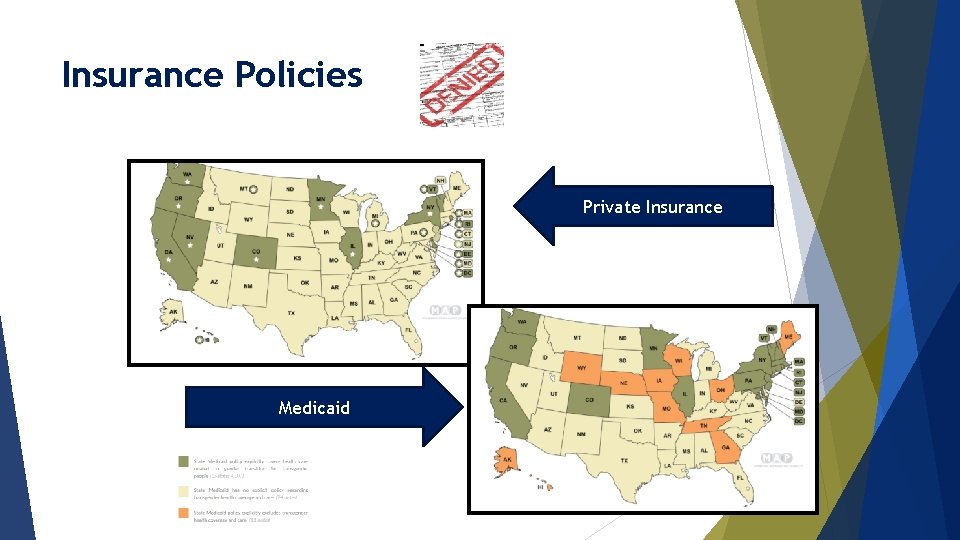
Insurance Policies Private Insurance Medicaid
Trauma Informed approach to history taking Know there are higher rates of sexual assault, violence (James, 2016) Objectifying of trans bodies, people could have had negative experiences Higher rates of survival sex/sex work Preface reason for taking sexual health history Tell people it is ok to decline, especially at a first visit Use reflective language
Sexual Health History Taking No assumptions about what people are doing and with whom Gay, queer etc. tell you nothing about risk and behaviors Same with relationship status Higher rates of ethical non-monogamy Lots of overlap with the BDSM/Kink community Body inventories Gender marker on the record tells you nothing about their anatomy
Sexual Health History- 8 P's Preferences Partners Practices Protection Past from STIs History of STIs Pregnancy Pleasure Partner Violence From Dr. Tim Cavanaugh at Fenway Health's Excellence in Transgender Health Conference October 14, 2017
Other considerations HIV prevalence among transwomen of color is over 25% Pr. EP Reproductive options Hormone therapy is not birth control Freezing eggs, banking sperm Stopping HRT, having children and restarting is becoming more common Be knowledgeable about different types of barriers that can be used Ask about toys or prosthetics- counsel around care and cleaning Lube discussion- no glycerin Atrophy, bleeding and pain (transmen) Post- surgical care and sexual health
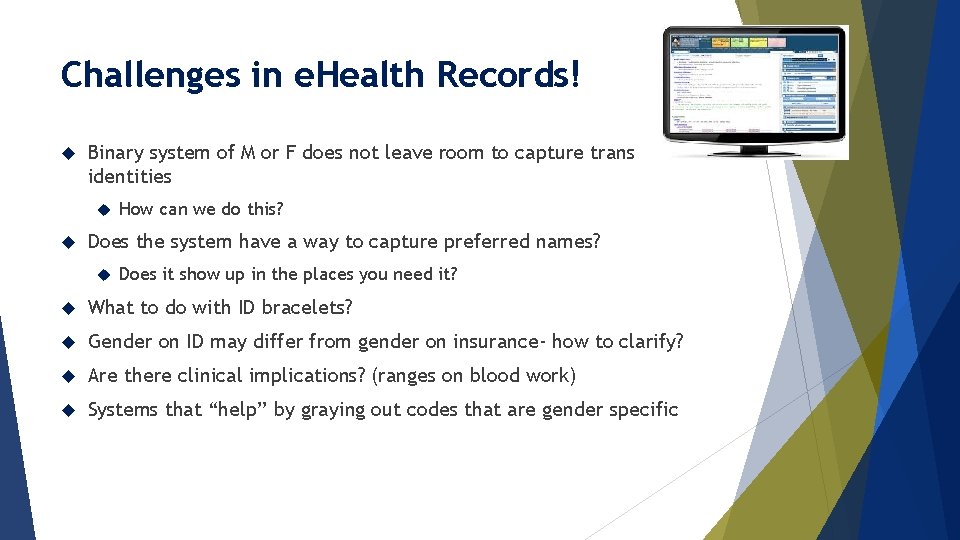
Challenges in e. Health Records! Binary system of M or F does not leave room to capture trans identities How can we do this? Does the system have a way to capture preferred names? Does it show up in the places you need it? What to do with ID bracelets? Gender on ID may differ from gender on insurance- how to clarify? Are there clinical implications? (ranges on blood work) Systems that “help” by graying out codes that are gender specific
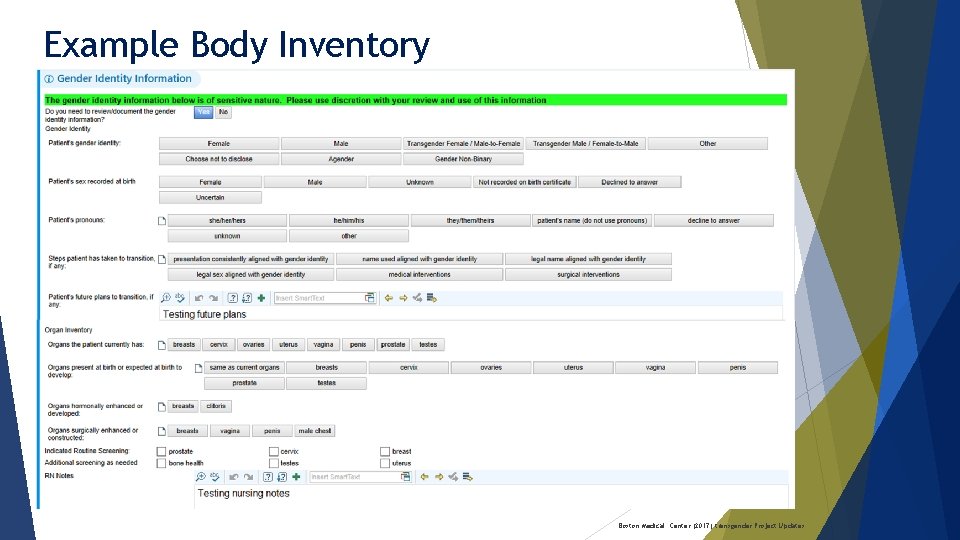
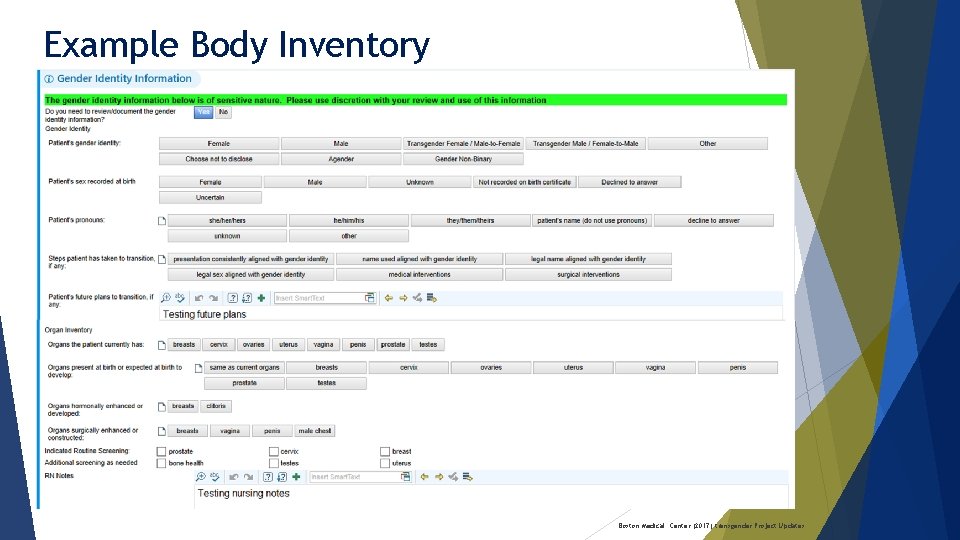
Example Body Inventory Boston Medical Center (2017) transgender Project Updates
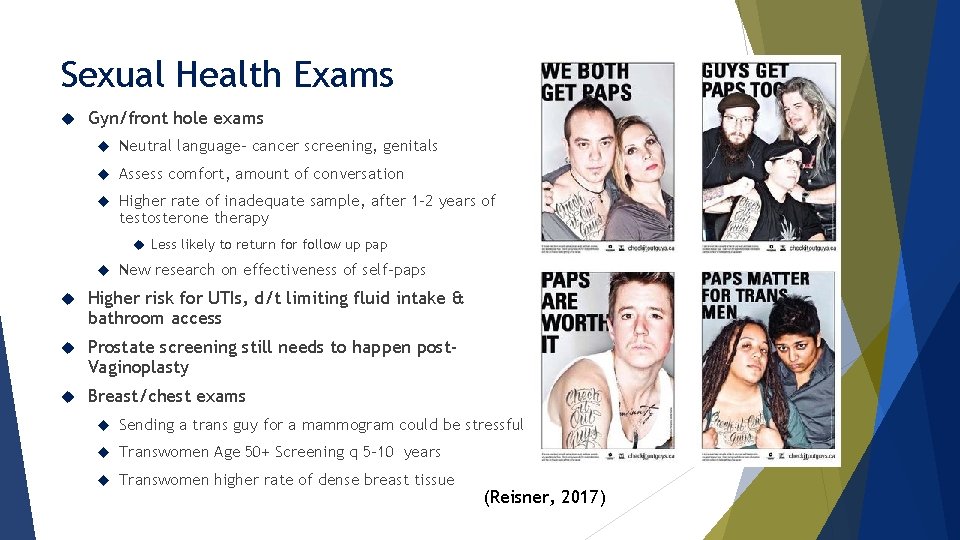
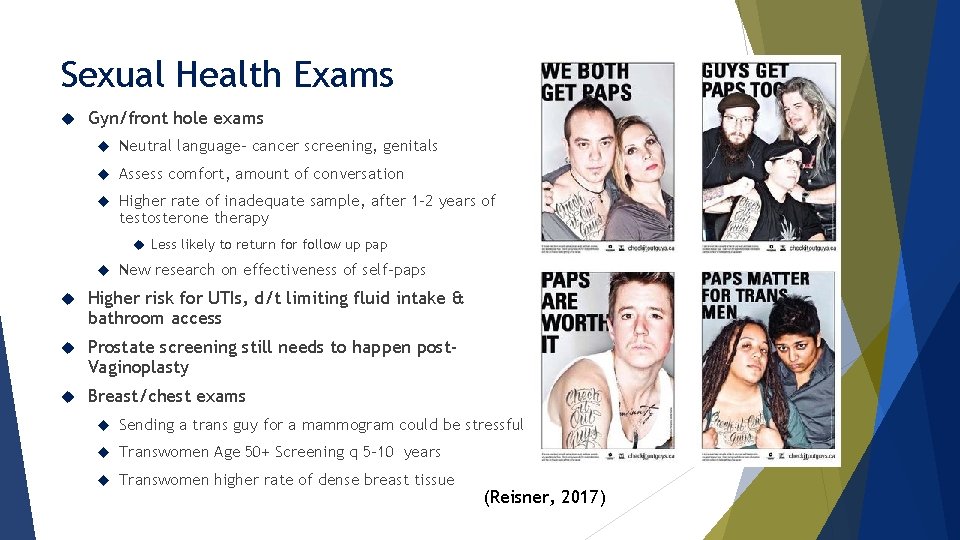
Sexual Health Exams Gyn/front hole exams Neutral language- cancer screening, genitals Assess comfort, amount of conversation Higher rate of inadequate sample, after 1 -2 years of testosterone therapy Less likely to return for follow up pap New research on effectiveness of self-paps Higher risk for UTIs, d/t limiting fluid intake & bathroom access Prostate screening still needs to happen post. Vaginoplasty Breast/chest exams Sending a trans guy for a mammogram could be stressful Transwomen Age 50+ Screening q 5 -10 years Transwomen higher rate of dense breast tissue (Reisner, 2017)
Quick Tips When in doubt, ASK- “what pronouns do you prefer? ” or “Is there another name that you go by” Use of affirmed names and pronouns is PARAMOUNT If you make a mistake: apologize, correct it and move on Ask what gender the pt wants listed on their record, or what gender they have listed with their insurance. Be respectful and use discretion Transgender status is PHI – calling someone by the wrong name in a public space can compromise privacy and safety Clarify information in private Know that there is no such thing as the “full surgery” or for someone to have “completed transition”
Quick Tips Preface your history taking, acknowledge that questions may be personal “I understand that this may be sensitive, I need to ask a couple more questions to make sure we are giving you the best care possible” Avoid gratuitous questions or statements: “What does your family think about you? ” “You look so good for a trans person” “I never would have known you used to be a boy!” “What do you think about Caitlyn Jenner? ” “What was your name before you transitioned? ”

Rhode Island Resources Youth Pride Inc. www. youthprideri. org TGI Network of RI www. tginetwork. org Options News Magazine www. optionsri. org GLBT Advocates & Defencers (GLAD) www. glad. org Dr. Michelle Forcier, Lifespan
National Resources-Medical Trans Line – free consultation resource http: //project-health. org/transline/ Primary Care Protocol for Transgender Patients http: //transhealth. ucsf. edu/ National LGBT Health Education Center at Fenway Health http: //www. lgbthealtheducation. org/
National Resources-Advocacy National Center for Transgender Equality www. transequality. org National Transgender Law Center www. transgenderlawcenter. org Family Acceptance Project www. familyproject. sfsu. edu/ Trans Youth Family Allies www. imatyfa. org

Jaye Watts jayew@thundermisthealth. org
 Quality by design approach
Quality by design approach Shelley jaye
Shelley jaye Parasha jaie sara
Parasha jaie sara Dave jaye
Dave jaye Minimal polynomial of a matrix
Minimal polynomial of a matrix Watts volts amps ohms
Watts volts amps ohms Ohm's law watts
Ohm's law watts Watts electricidad
Watts electricidad Elizabeth watts ship
Elizabeth watts ship Eaton arc flash handbook
Eaton arc flash handbook Watts vs united states
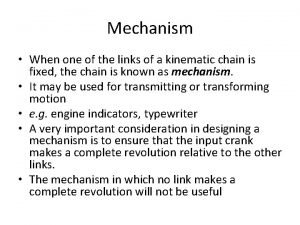
Watts vs united states Watt's indicator mechanism
Watt's indicator mechanism Dr jacqueline watts
Dr jacqueline watts Watts-strogatz
Watts-strogatz Mustang way schedule
Mustang way schedule Tva
Tva A dishwasher uses 700 watts
A dishwasher uses 700 watts Watts v morrow
Watts v morrow My doom
My doom Charlie watts
Charlie watts Solia lumii
Solia lumii Mettre les watts
Mettre les watts Scotch yoke mechanism
Scotch yoke mechanism Watts humphrey
Watts humphrey Mark attalla
Mark attalla Justin kibler
Justin kibler Understanding trans health
Understanding trans health Role and responsibility of occupational health nurse
Role and responsibility of occupational health nurse National program for mother and child
National program for mother and child Louisiana department of health and hospitals
Louisiana department of health and hospitals Difference between health education and counselling
Difference between health education and counselling Whole health circle of health
Whole health circle of health