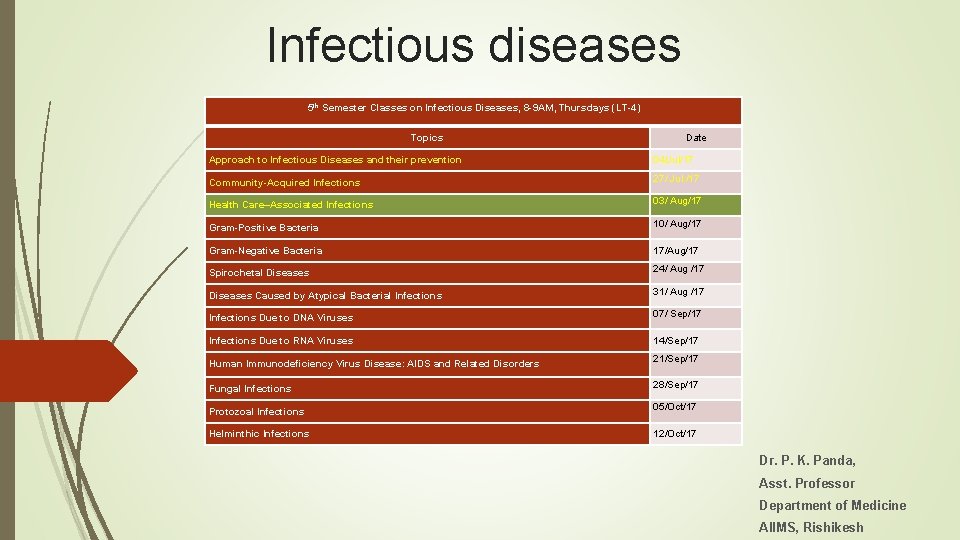
Infectious diseases 5 th Semester Classes on Infectious









- Slides: 21
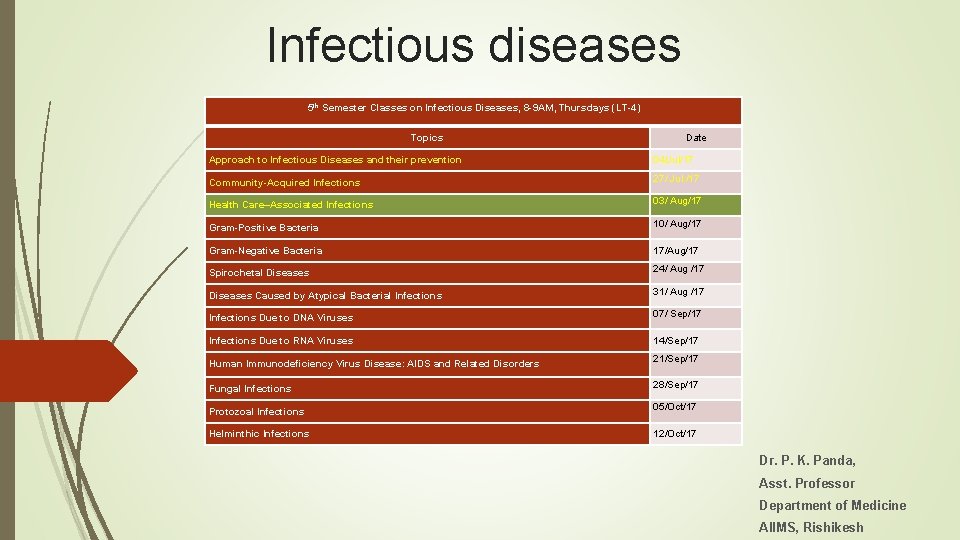
Infectious diseases 5 th Semester Classes on Infectious Diseases, 8 -9 AM, Thursdays (LT-4) Topics Date Approach to Infectious Diseases and their prevention 04/Jul/17 Community-Acquired Infections 27/ Jul /17 Health Care–Associated Infections 03/ Aug/17 Gram-Positive Bacteria 10/ Aug/17 Gram-Negative Bacteria 17/Aug/17 Spirochetal Diseases 24/ Aug /17 Diseases Caused by Atypical Bacterial Infections 31/ Aug /17 Infections Due to DNA Viruses 07/ Sep/17 Infections Due to RNA Viruses 14/Sep/17 Human Immunodeficiency Virus Disease: AIDS and Related Disorders 21/Sep/17 Fungal Infections 28/Sep/17 Protozoal Infections 05/Oct/17 Helminthic Infections 12/Oct/17 Dr. P. K. Panda, Asst. Professor Department of Medicine AIIMS, Rishikesh
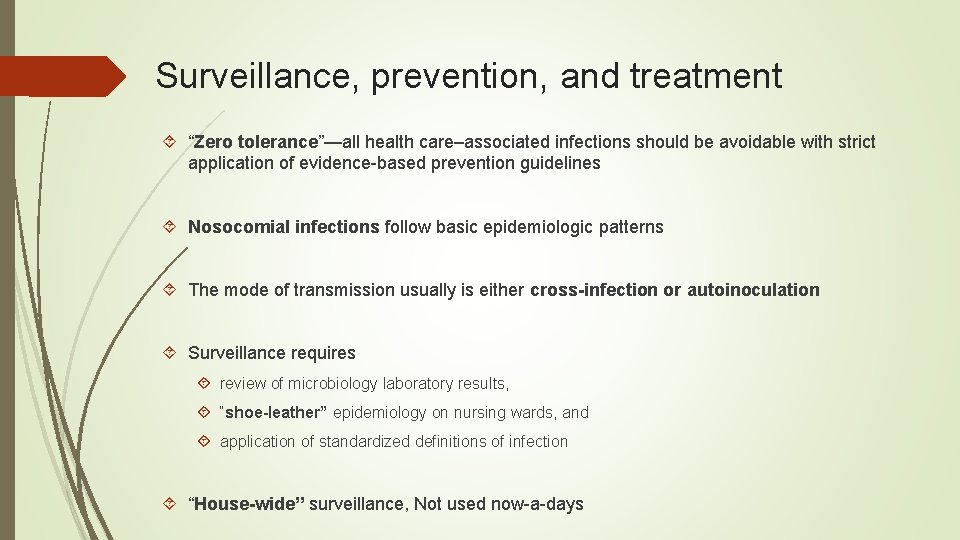
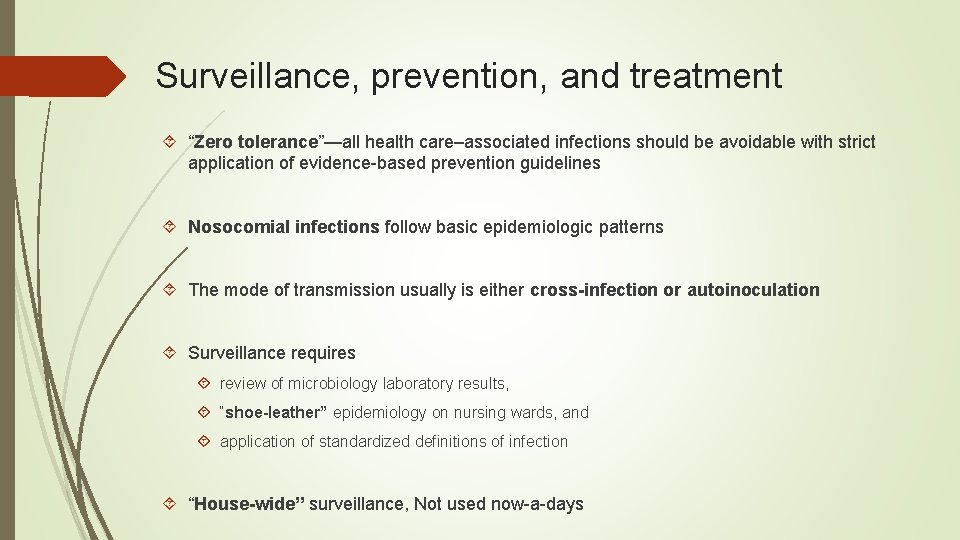
Surveillance, prevention, and treatment “Zero tolerance”—all health care–associated infections should be avoidable with strict application of evidence-based prevention guidelines Nosocomial infections follow basic epidemiologic patterns The mode of transmission usually is either cross-infection or autoinoculation Surveillance requires review of microbiology laboratory results, “shoe-leather” epidemiology on nursing wards, and application of standardized definitions of infection “House-wide” surveillance, Not used now-a-days
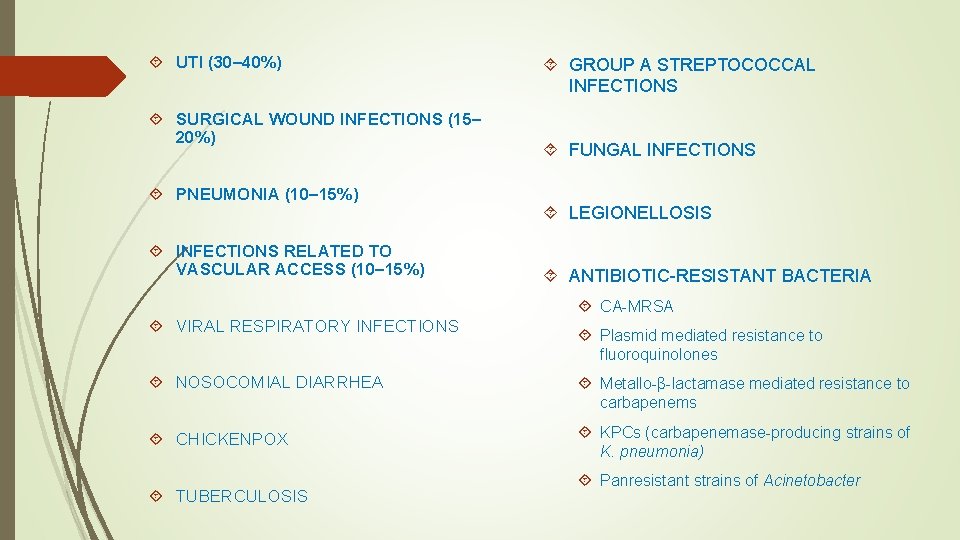
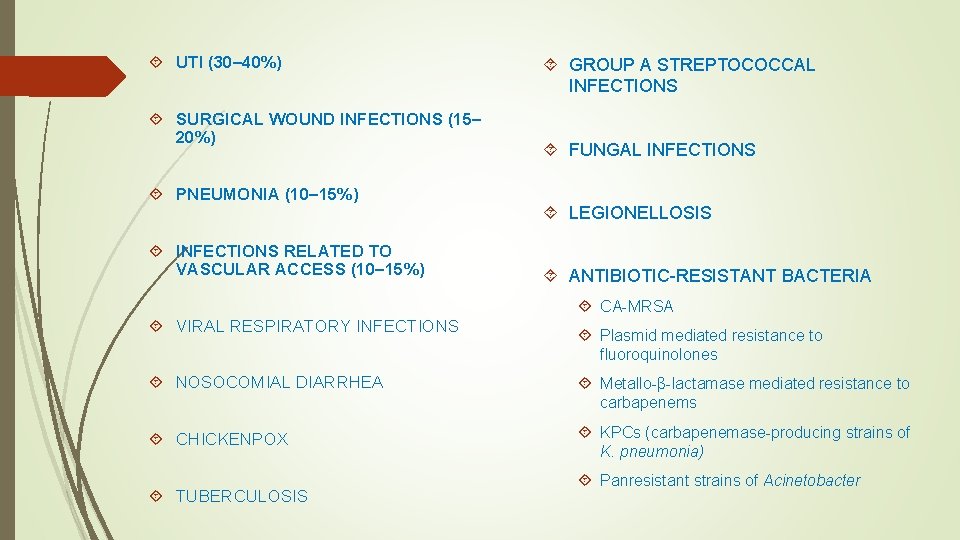
UTI (30– 40%) SURGICAL WOUND INFECTIONS (15– 20%) PNEUMONIA (10– 15%) INFECTIONS RELATED TO VASCULAR ACCESS (10– 15%) GROUP A STREPTOCOCCAL INFECTIONS FUNGAL INFECTIONS LEGIONELLOSIS ANTIBIOTIC-RESISTANT BACTERIA CA-MRSA VIRAL RESPIRATORY INFECTIONS Plasmid mediated resistance to fluoroquinolones NOSOCOMIAL DIARRHEA Metallo-β-lactamase mediated resistance to carbapenems CHICKENPOX KPCs (carbapenemase-producing strains of K. pneumonia) TUBERCULOSIS Panresistant strains of Acinetobacter
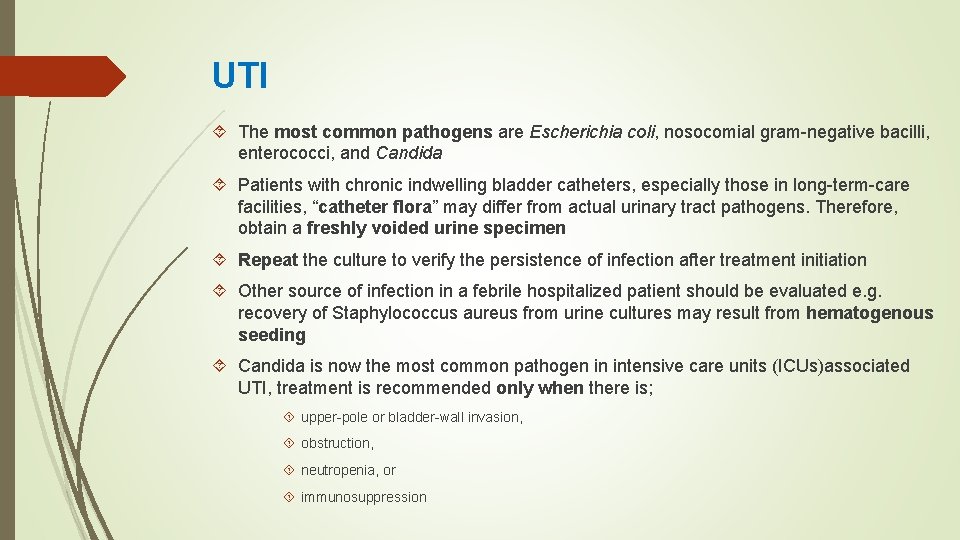
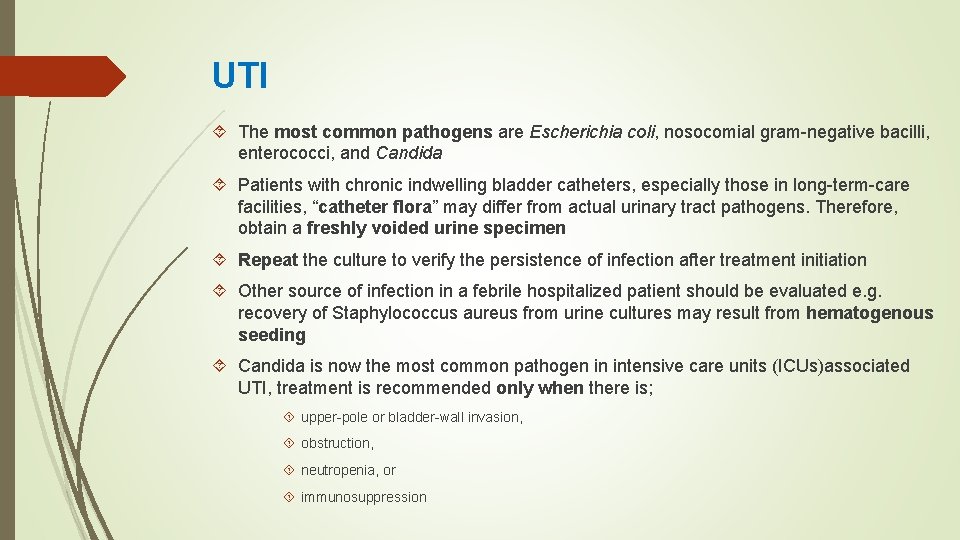
UTI The most common pathogens are Escherichia coli, nosocomial gram-negative bacilli, enterococci, and Candida Patients with chronic indwelling bladder catheters, especially those in long-term-care facilities, “catheter flora” may differ from actual urinary tract pathogens. Therefore, obtain a freshly voided urine specimen Repeat the culture to verify the persistence of infection after treatment initiation Other source of infection in a febrile hospitalized patient should be evaluated e. g. recovery of Staphylococcus aureus from urine cultures may result from hematogenous seeding Candida is now the most common pathogen in intensive care units (ICUs)associated UTI, treatment is recommended only when there is; upper-pole or bladder-wall invasion, obstruction, neutropenia, or immunosuppression

SURGICAL WOUND INFECTIONS The most common pathogens are S. aureus, coagulase-negative staphylococci, and enteric and anaerobic bacteria. In rapidly progressing postoperative infections manifesting within 24– 48 h of a surgical procedure, group A streptococcal or clostridial infection more common

PNEUMONIA Early-onset nosocomial pneumonia, which manifests within the first 4 days of hospitalization, is most often caused by community-acquired pathogens such as Streptococcus pneumonia and Haemophilus species Late-onset pneumonias most commonly are due to S. aureus, P. aeruginosa, Enterobacter species, Klebsiella pneumoniae, or Acinetobacter

INFECTIONS RELATED TO VASCULAR ACCESS The most common pathogens include coagulase-negative staphylococci, S. aureus, enterococci, nosocomial gram-negative bacilli, and Candida

Hospitals’ infection-control programs

Standard precautions are designed for the care of all patients in hospitals and aim to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources These precautions include gloving as well as hand cleansing for potential contact with (1) blood; (2) all other body fluids, secretions, and excretions, whether or not they contain visible blood; (3) nonintact skin; and (4) mucous Membranes. Depending on exposure risks, standard precautions also include use of N 95 respirators, surgical face masks, or glove and gown for airborne, droplet, or contact exposure respectively Other measures of standard precautions; Prevention of needle stick injury Environmental cleansing and spill management Waste management




EMPLOYEE HEALTH SERVICE Contagious-disease history can be taken; Evidence of immunity to a variety of diseases, such as hepatitis B, chickenpox, measles, mumps, and rubella, can be sought; Immunizations for hepatitis B, measles, mumps, rubella, varicella, Influenza, and pertussis can be given as needed; Baseline tuberculosis testing can be performed; Education about personal responsibility for infection control can be initiated
Protocols for dealing with workers exposed to contagious diseases (e. g. , influenza) and those percutaneously or mucosally exposed to the blood of patients infected with HIV or hepatitis B or C virus. For example, postexposure HIV prophylaxis (PEP) Protocols for dealing with caregivers who have common contagious diseases (such as chickenpox, group A streptococcal infection, influenza or another respiratory infection, or infectious diarrhea) and for those who have less common but high-visibility public health problems (such as chronic hepatitis B or C or HIV infection)
Thank you Next Class Gram-Positive Bacteria 10/ Aug/17