Improving Clinical Quality in Womens Health Screenings and









- Slides: 39
Improving Clinical Quality in Women's Health Screenings and Beyond Kentucky Primary Care Association Spring Conference Anne Gaglioti, MD SERCN Director Assistant Professor of Family Medicine National Center for Primary Care Morehouse School of Medicine May 9, 2017 Funding Acknowledgement: This program was funded through a Patient-Centered Outcomes Research Institute (PCORI) Eugene Washington PCORI Engagement Award (EAIN-3315).



Vision: National Resource to Achieve Equitable and Optimal Health Through Primary Care For All. Mission: Strengthening the Primary Care System through Research, Education, and Training To improve Health Outcomes while Advancing and Sustaining Health Equity

Community Health Practice & Population Based Health Equity Research Policy Health Information Technology Quality Improvement Education and Training Primary Care
Southeast Regional Clinicians Network • Practice Based Research Network (PBRN) • Our GOAL: – to improve quality of care and outcomes to medically underserved patients in the Southeastern United States. • Our MEMBERS: – federally qualified health centers and state primary care associations located in the states of Alabama, Florida, Georgia, Kentucky, , Mississippi, North Carolina, South Carolina and Tennessee • Our HISTORY: – Partnership between the National Center for Primary Care and the Southeast Health Care Consortium – Funded as a PBRN by AHRQ in 1995
Objectives • Screening women throughout the lifecycle • Streamline despite differing intervals • Checklists, Templates, Resources • Data Collection and Evaluation The Family Doctor, Grant Wood (American 1892 -1942)
Why this is Difficult “To fully satisfy the USPSTF recommendations, 1773 hours of a physicians annual time, or 7. 4 hours per working day, is needed for the provision of preventive services. ”

Well Exam?
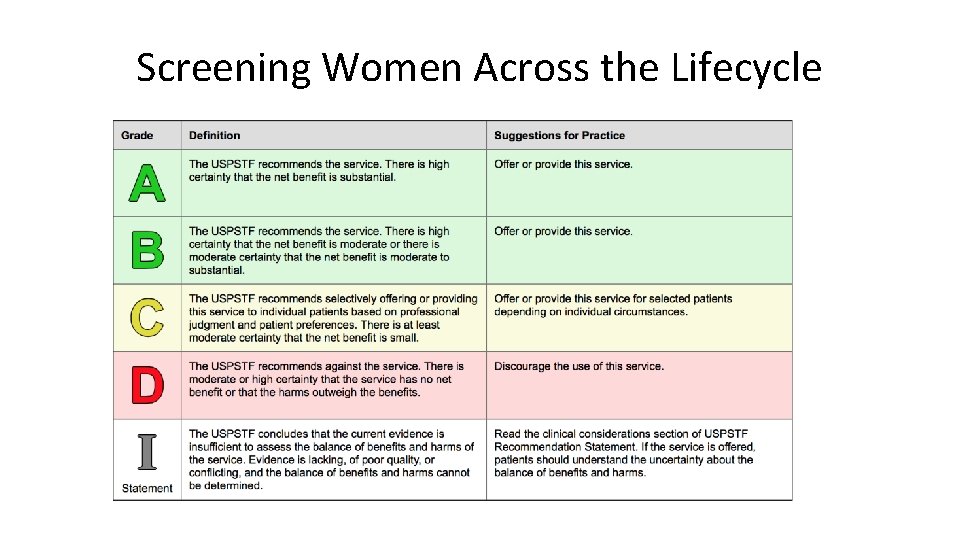
Screening Women Across the Lifecycle
Uniform Data System Measures for Women’s Health Screening • Cervical Cancer Screening – Proportion of women ages 21 -64 with a PAP smear in the last 3 years • Colorectal Cancer Screening – Proportion 50 through 75 years with a CRC screening test • BMI Screening • Tobacco Screening • Depression Screening
Healthy People 2020 Goals and USPSTF

What Improves Screening in Safety Net Settings? • For Cancer Screening Generally – Patient reminders, small media, and provider audit and feedback • For Breast cancer screening – Reducing out of pocket costs • For CRC and breast cancer screening – Reducing structural barriers

The Power of Checklists
Screening Women Across the Lifecycle Recommendations by Different Age Groups and Risk Factors • Focus on Key Screening Tests • Highlight differences across the lifecycle
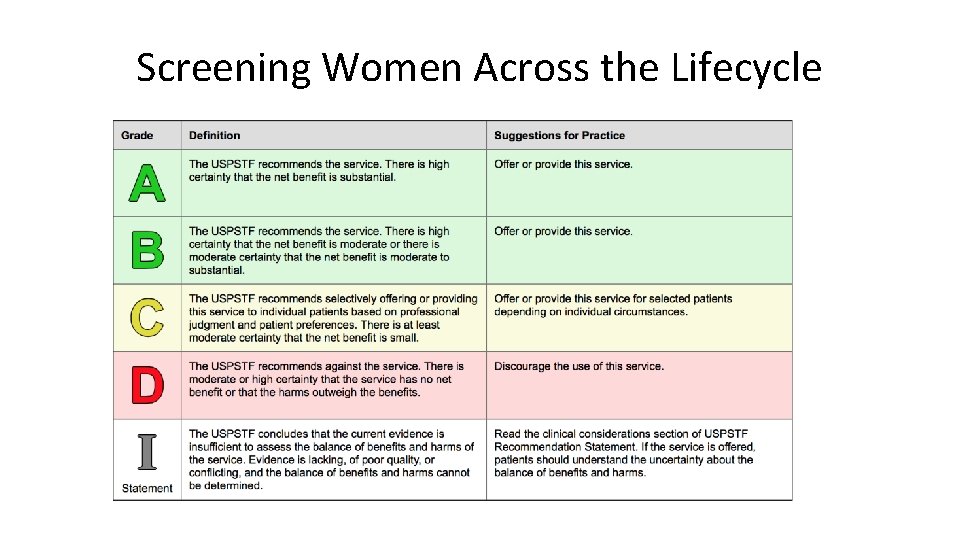
Screening Women Across the Lifecycle
Screening Women Across the Lifecycle: Cervical Cancer • Cervical Cancer Screening: – Start at 21 – Every 3 years; reflex High risk HPV testing – At age 30, HPV co-testing every 5 years if desired – Stop at age 65 if 2 previous PAPs normal and normal risk
Screening Women Across the Lifecycle: Breast Cancer • USPSTF: – Ages 40 -49: Individualize decision to begin biennial screening according to the patient’s circumstances and values (C) – Ages 50 -75: screen every two years (B) – Ages >75 : no recommendation due to insufficient evidence – Recommends against BSE (D) – Insufficient evidence for or against CBE (I)
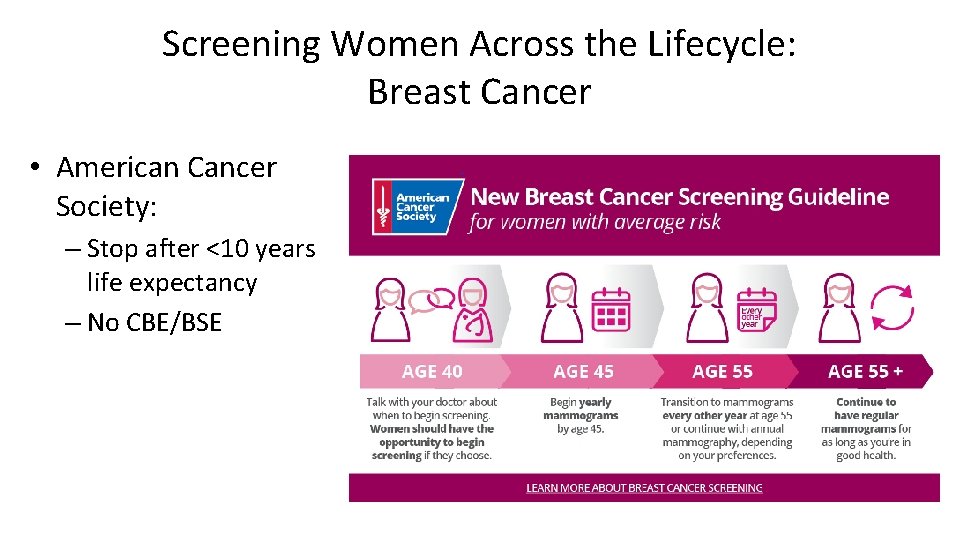
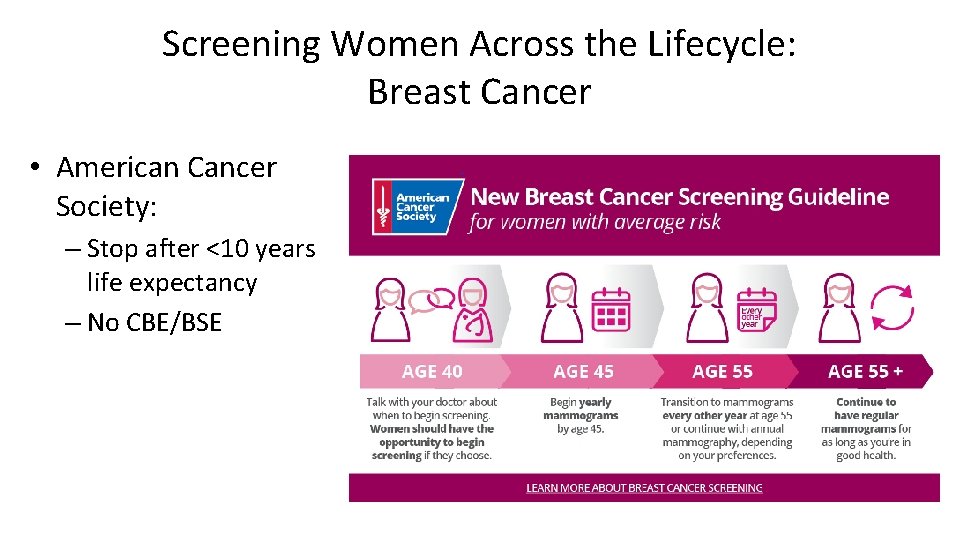
Screening Women Across the Lifecycle: Breast Cancer • American Cancer Society: – Stop after <10 years life expectancy – No CBE/BSE
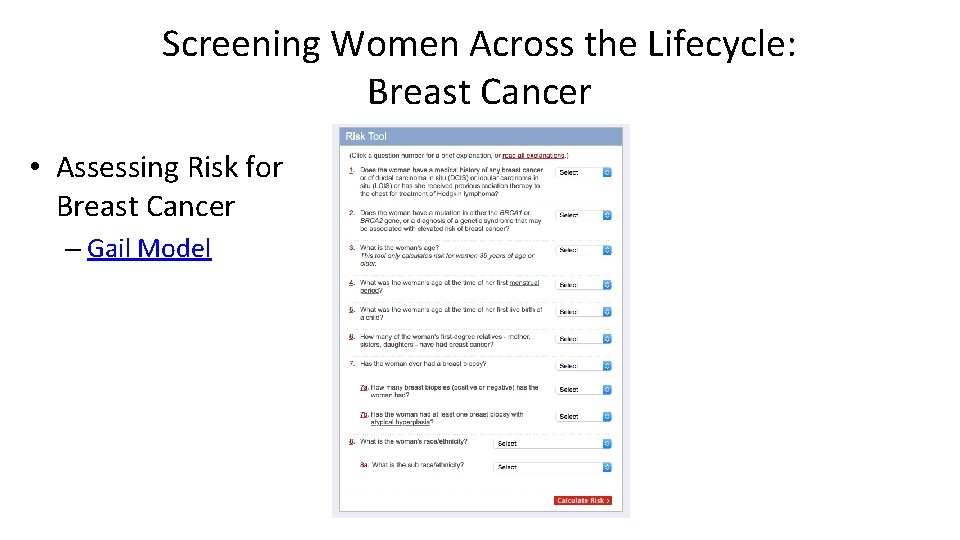
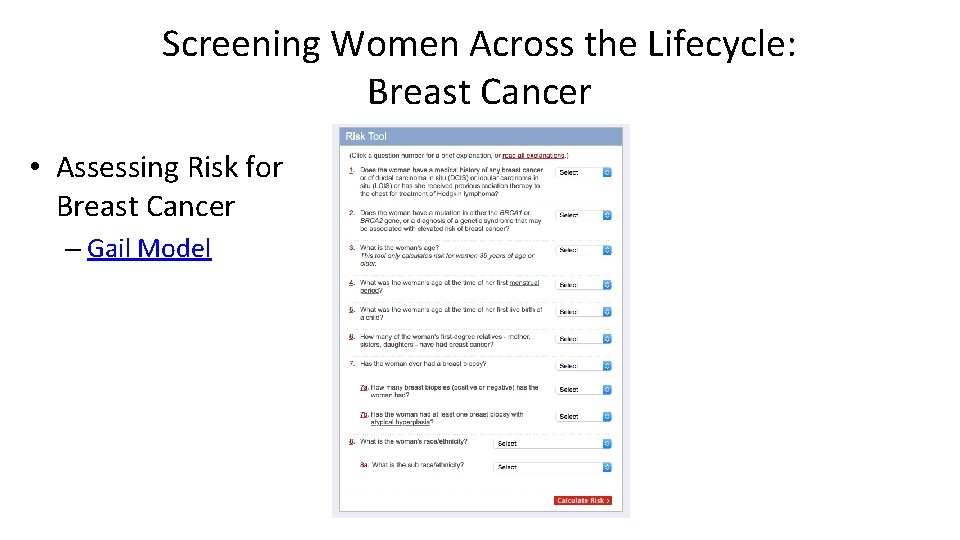
Screening Women Across the Lifecycle: Breast Cancer • Assessing Risk for Breast Cancer – Gail Model
Screening Women Across the Lifecycle: Lung Cancer • Screen ages 55 -80 with history of smoking using low dose CT – 30 pack years – Currently smoking or quit 15 years ago or less • Interval: yearly • Stop: 15 years since quit date, other life-limiting disease, or lack of willingness to have curative lung surgery
Screening Women Across the Lifecycle: Colorectal Cancer • Screen women ages 50 -75 • Ability to obtain colonoscopy testing if stool testing positive
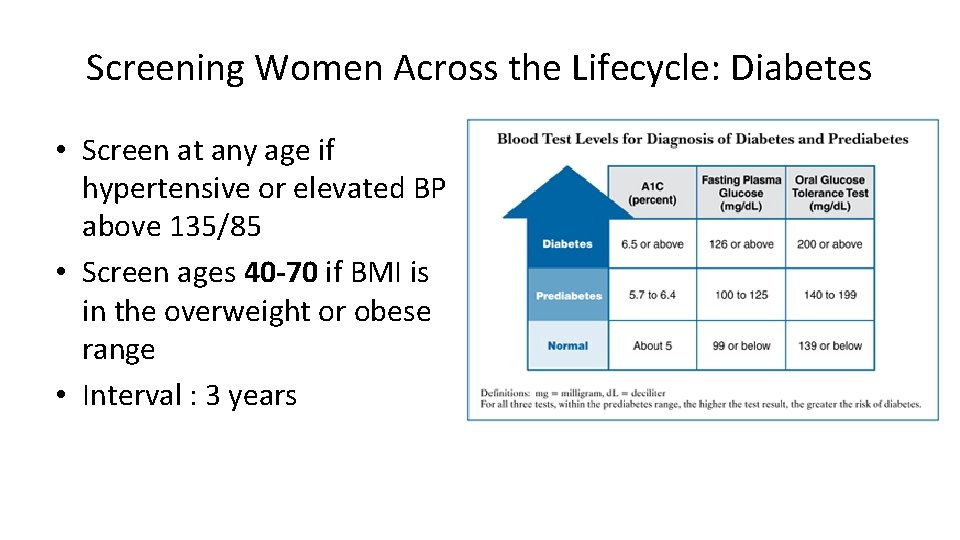
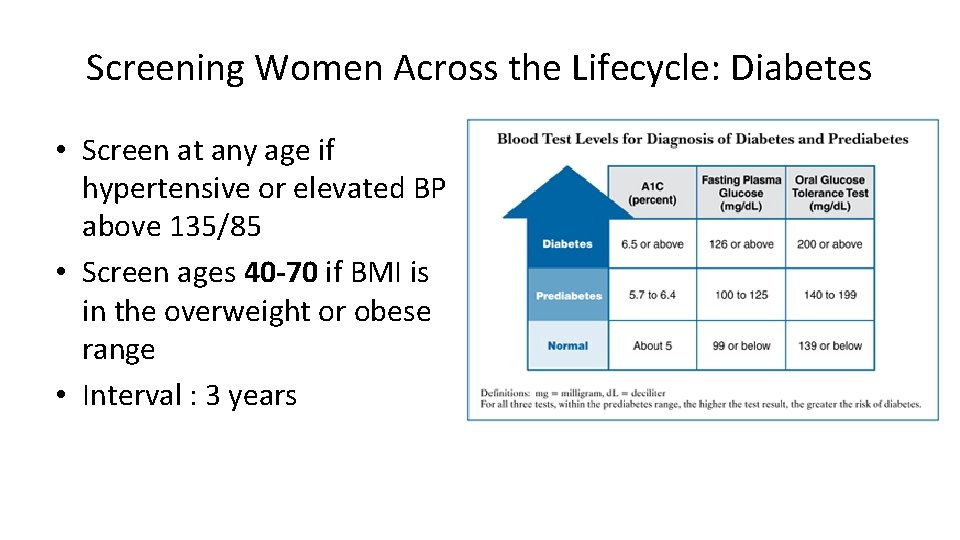
Screening Women Across the Lifecycle: Diabetes • Screen at any age if hypertensive or elevated BP above 135/85 • Screen ages 40 -70 if BMI is in the overweight or obese range • Interval : 3 years
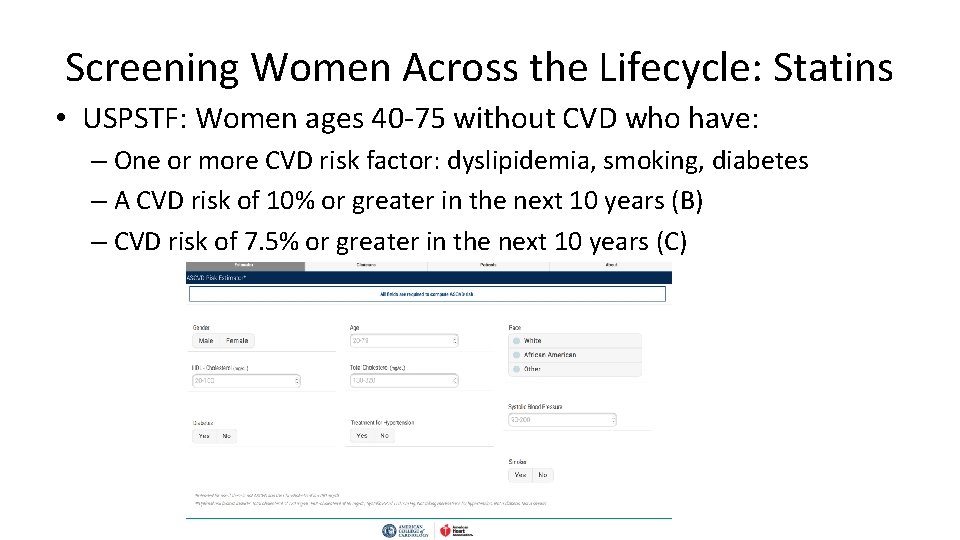
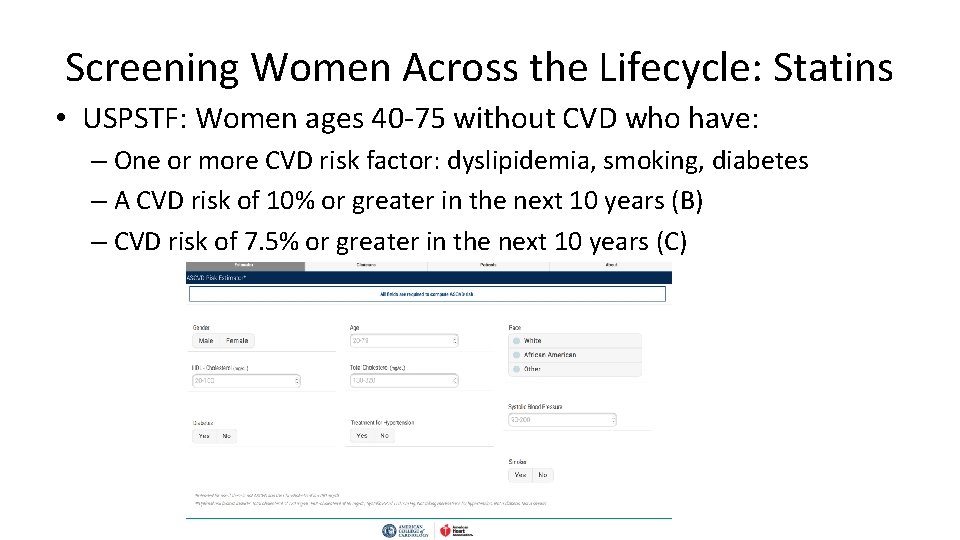
Screening Women Across the Lifecycle: Statins • USPSTF: Women ages 40 -75 without CVD who have: – One or more CVD risk factor: dyslipidemia, smoking, diabetes – A CVD risk of 10% or greater in the next 10 years (B) – CVD risk of 7. 5% or greater in the next 10 years (C)
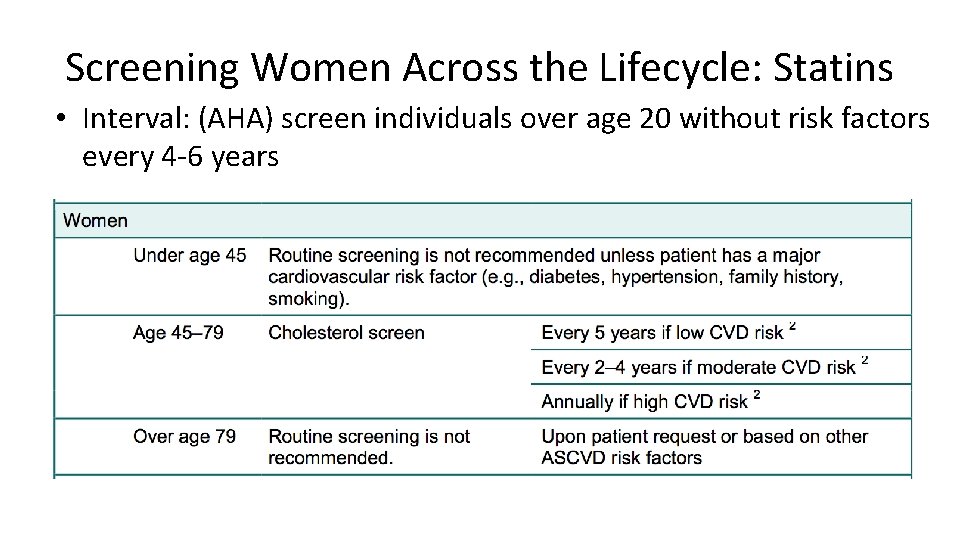
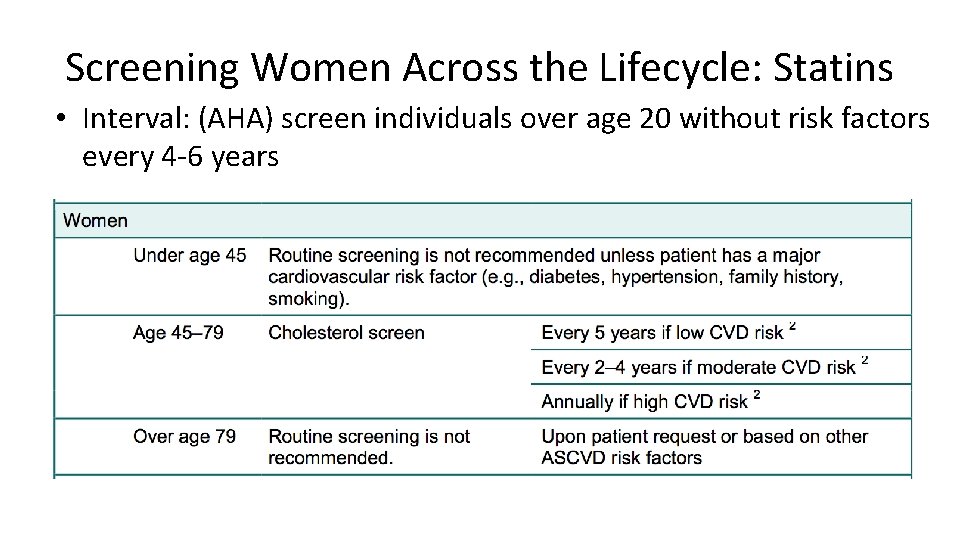
Screening Women Across the Lifecycle: Statins • Interval: (AHA) screen individuals over age 20 without risk factors every 4 -6 years
Screening Women Across the Lifecycle: Depression • Screen general adult population including pregnant/postpartum women using validated screening tool with adequate systems for diagnosis and referral to treatment • Interval: yearly/ using clinical judgment • Tools: PHQ-2/9; Beck Depression Inventory; Edinburgh Postnatal Depression Scale
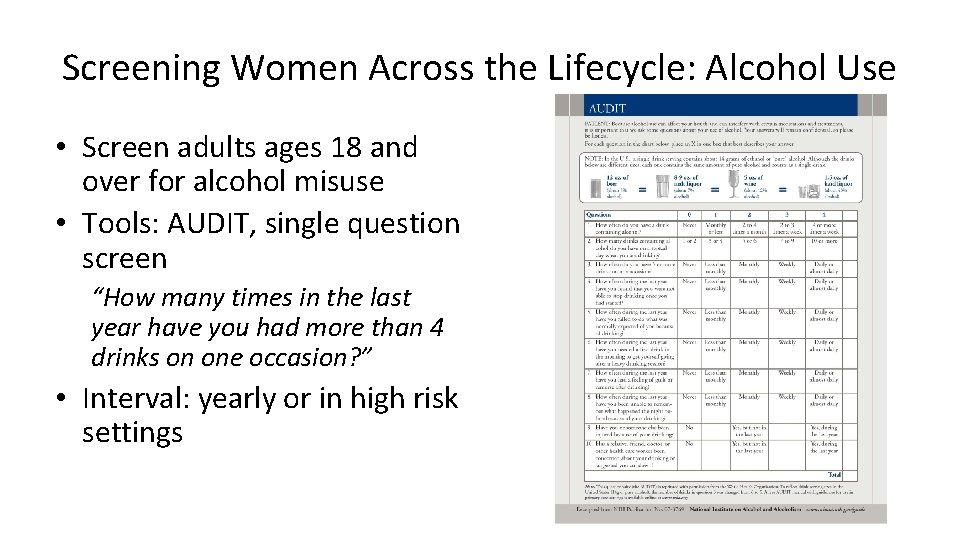
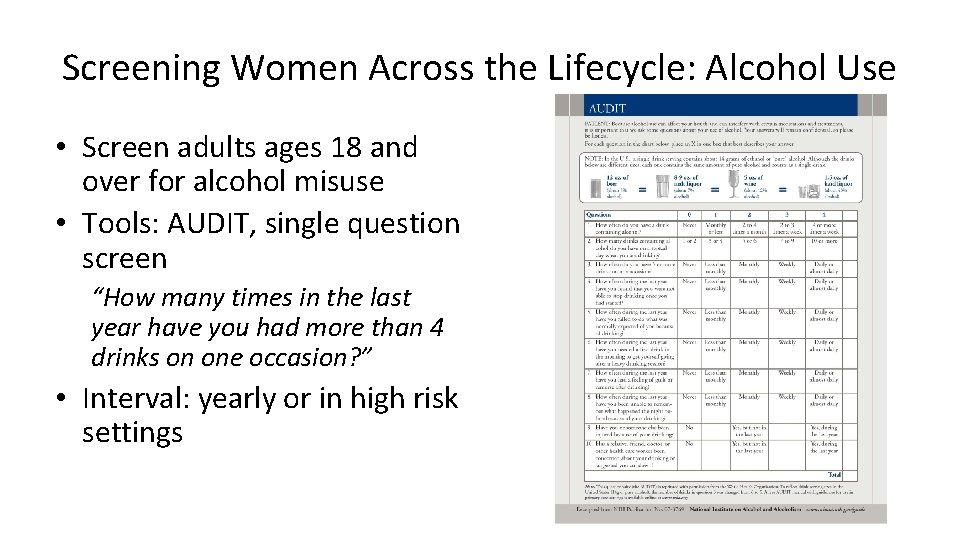
Screening Women Across the Lifecycle: Alcohol Use • Screen adults ages 18 and over for alcohol misuse • Tools: AUDIT, single question screen “How many times in the last year have you had more than 4 drinks on one occasion? ” • Interval: yearly or in high risk settings

Screening Women Across the Lifecycle: Intimate Partner Violence • Screen women of childbearing age for IPV and refer those who screen positive to intervention services (B) • Screening Tools: HITS English/Spanish • Interval: no evidence
Screening Women Across the Lifecycle: Sexually Transmitted Infections • HIV: ages 15 -65 – Interval USPSTF: very high risk annual, increased risk 3 -5 years, low risk once • CDC yearly • Gonorrhea/Chlamydia: – ages <24 routine screening – ages >24 with risk factors • Syphilis: screen all adults and adolescents at risk – MSM, commercial sex workers, incarceration, geography
Screening Women Across the Lifecycle: Hepatitis C • Screen adults born in 1945 -1965 for Hepatitis C once
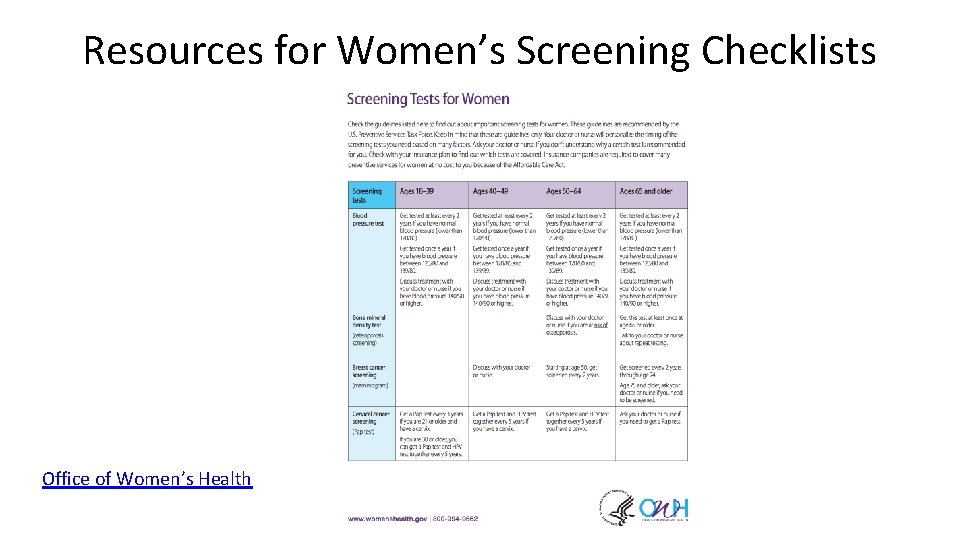
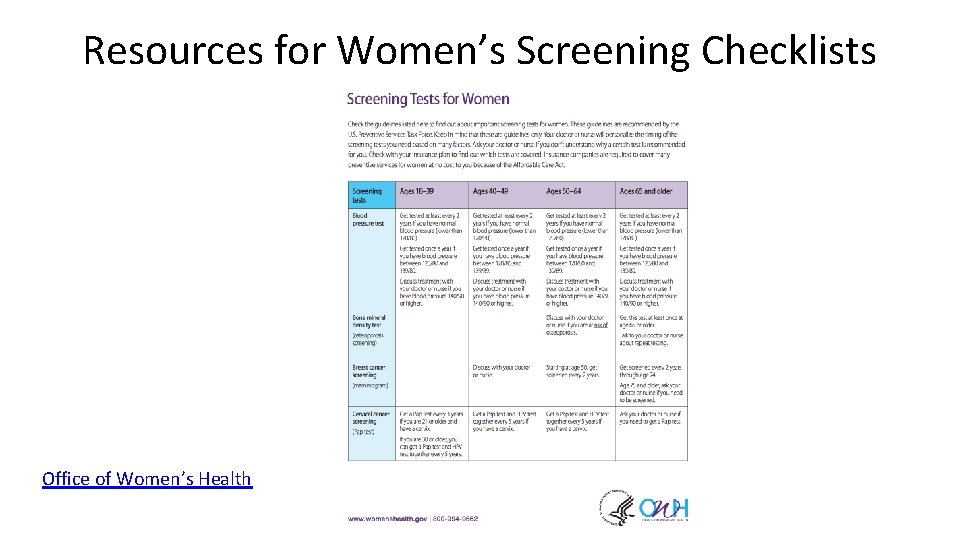
Resources for Women’s Screening Checklists Office of Women’s Health
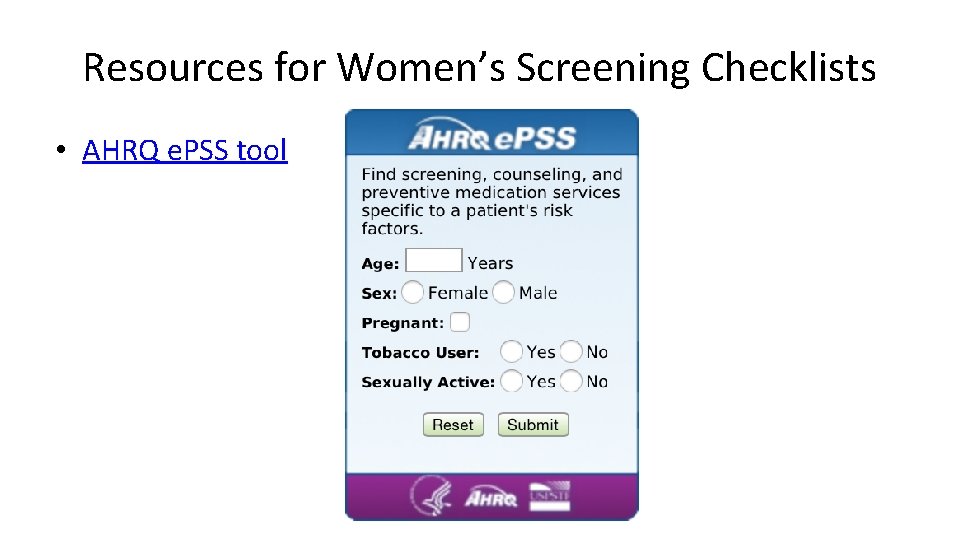
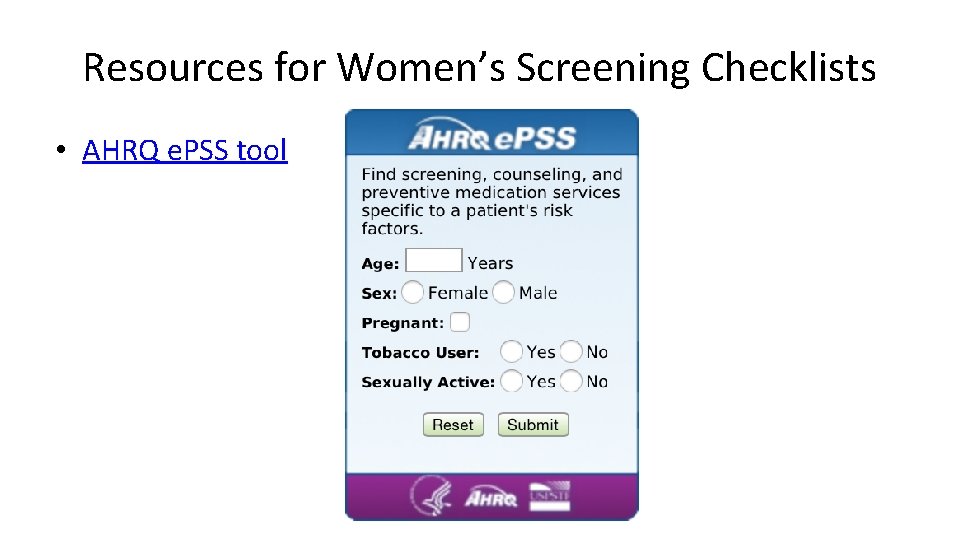
Resources for Women’s Screening Checklists • AHRQ e. PSS tool

Operationalize a Women’s Health Screening Checklist • • Construct as a team Designate pre-visit Designate during-visit Consider embedding in note
Operationalize a Women’s Health Screening Checklist • Pre-visit with MA or paper forms – Depression – AUDIT – HITS – BMI – BP
Operationalize a Women’s Health Screening Checklist • Embed Table/List in note that includes – Recommendation – Completed – Due date
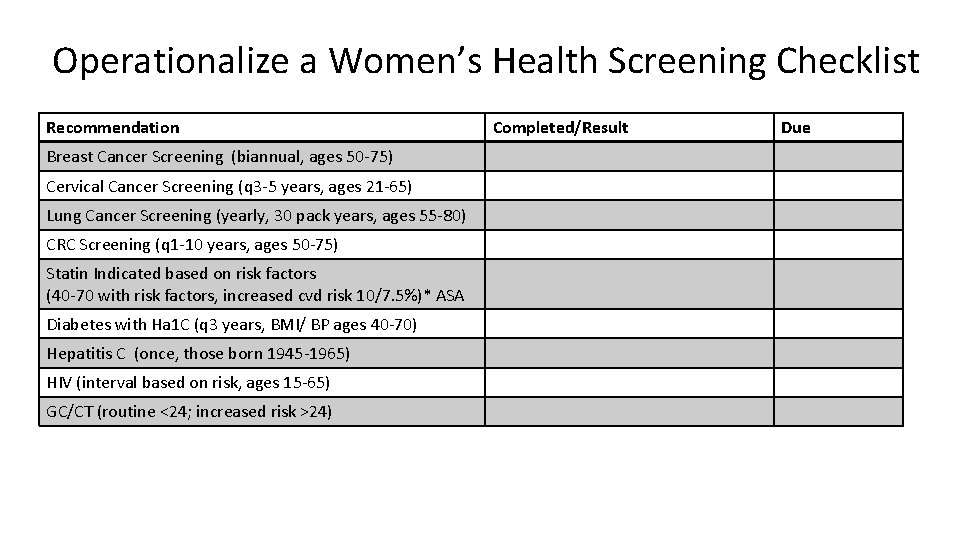
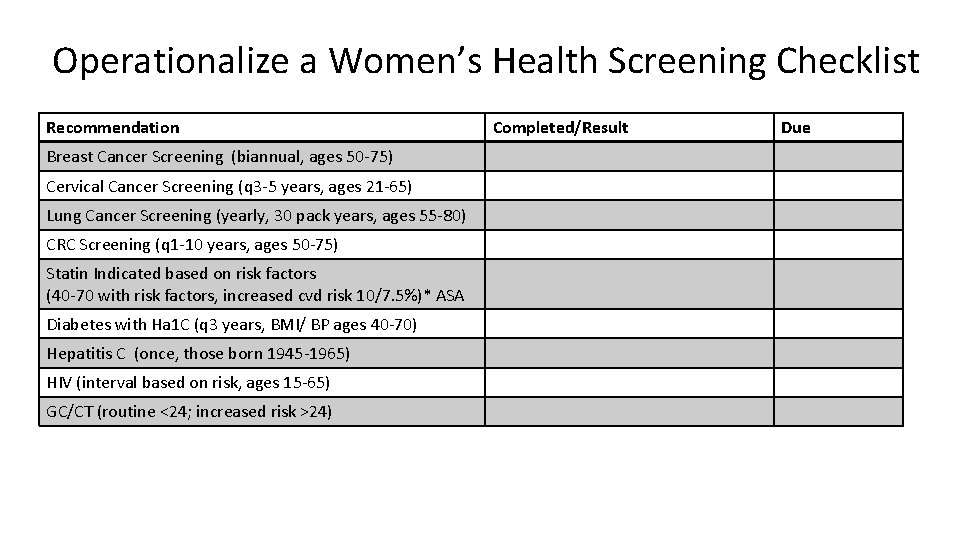
Operationalize a Women’s Health Screening Checklist Recommendation Breast Cancer Screening (biannual, ages 50 -75) Cervical Cancer Screening (q 3 -5 years, ages 21 -65) Lung Cancer Screening (yearly, 30 pack years, ages 55 -80) CRC Screening (q 1 -10 years, ages 50 -75) Statin Indicated based on risk factors (40 -70 with risk factors, increased cvd risk 10/7. 5%)* ASA Diabetes with Ha 1 C (q 3 years, BMI/ BP ages 40 -70) Hepatitis C (once, those born 1945 -1965) HIV (interval based on risk, ages 15 -65) GC/CT (routine <24; increased risk >24) Completed/Result Due
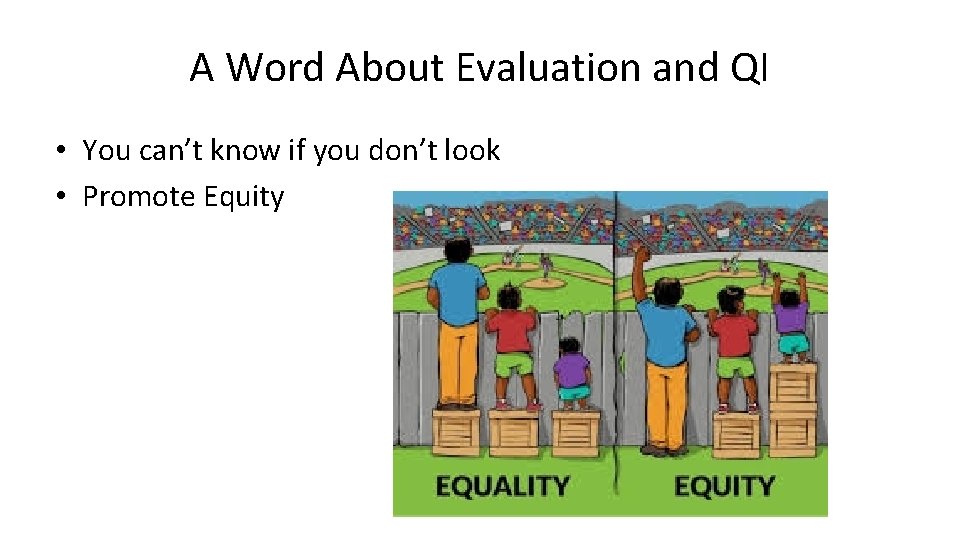
A Word About Evaluation and QI • You can’t know if you don’t look • Promote Equity
What Questions do you Have? Anne Gaglioti: agaglioti@msm. edu NCPC Website: www. primarycarematters. org SERCN Email: sercn@msm. edu SERCN Website: www. sercn. org Twitter: @sercn_ncpc
References • Kimberly S. H. Yarnall, Kathryn I. Pollak, Truls Østbye, Katrina M. Krause, and J. Lloyd Michener. Primary Care: Is There Enough Time for Prevention? American Journal of Public Health April 2003: Vol. 93, No. 4, pp. 635 -641. • Brouwers MC, De Vito C, Bahirathan L, et al. What implementation interventions increase cancer screening rates? a systematic review. Implementation Science IS. 2011; 6: 111. doi: 10. 1186/1748 -5908 -6 -111. • Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, De. Vinney B, Melillo S, Carvalho M, Taplin S, Bastani R, Rimer BK. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. American journal of preventive medicine. 2012 Jul 31; 43(1): 97 -118 • Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Academic Medicine. 2011 Mar 1; 86(3): 307 -13.
 Service quality and productivity
Service quality and productivity Methods of improving quality business a level
Methods of improving quality business a level Listening gap examples
Listening gap examples Gaps model for improving service quality
Gaps model for improving service quality Differences between men's and women's soccer
Differences between men's and women's soccer Womens ministry activities
Womens ministry activities Womens rights
Womens rights Late night womens hour
Late night womens hour Claire paine
Claire paine Womens right
Womens right Womens college kumbakonam
Womens college kumbakonam Womens college kumbakonam
Womens college kumbakonam Womens right
Womens right Womens shelter edmonton
Womens shelter edmonton Womens rights
Womens rights Female anatomy
Female anatomy Womens history month door
Womens history month door Womens community shelters
Womens community shelters Ballybeen womens centre
Ballybeen womens centre Scarborough womens centre
Scarborough womens centre Womens lacrosse helmets
Womens lacrosse helmets Bristol womens voice
Bristol womens voice Neqapp
Neqapp Cql clinical quality language
Cql clinical quality language Clinical trials quality by design
Clinical trials quality by design Administrative information system
Administrative information system Quality assurance vs quality control
Quality assurance vs quality control Basic concept of quality control and quality assurance pdf
Basic concept of quality control and quality assurance pdf Whole health clinical group
Whole health clinical group Improving own learning and performance examples
Improving own learning and performance examples Improving vocabulary with word parts and context clues
Improving vocabulary with word parts and context clues Improving vocabulary with word parts and context clues
Improving vocabulary with word parts and context clues Improving decision making and managing knowledge
Improving decision making and managing knowledge Project quality management pmp
Project quality management pmp Pmp gold plating
Pmp gold plating Quality assurance model in nursing
Quality assurance model in nursing Quality improvement vs quality assurance
Quality improvement vs quality assurance Quality gurus meaning
Quality gurus meaning Crosby's fourteen steps to quality improvement
Crosby's fourteen steps to quality improvement What is tqm
What is tqm