HEART DISEASE IN PREGNANCY The incidence of cardiac

- Slides: 8
HEART DISEASE IN PREGNANCY
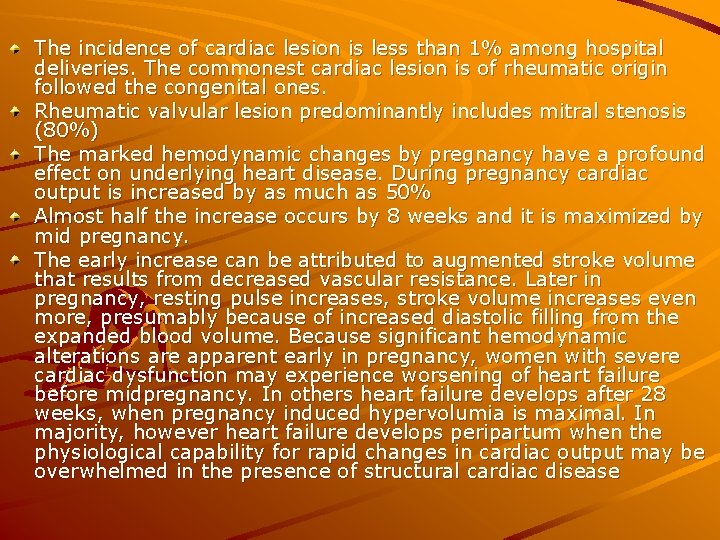
The incidence of cardiac lesion is less than 1% among hospital deliveries. The commonest cardiac lesion is of rheumatic origin followed the congenital ones. Rheumatic valvular lesion predominantly includes mitral stenosis (80%) The marked hemodynamic changes by pregnancy have a profound effect on underlying heart disease. During pregnancy cardiac output is increased by as much as 50% Almost half the increase occurs by 8 weeks and it is maximized by mid pregnancy. The early increase can be attributed to augmented stroke volume that results from decreased vascular resistance. Later in pregnancy, resting pulse increases, stroke volume increases even more, presumably because of increased diastolic filling from the expanded blood volume. Because significant hemodynamic alterations are apparent early in pregnancy, women with severe cardiac dysfunction may experience worsening of heart failure before midpregnancy. In others heart failure develops after 28 weeks, when pregnancy induced hypervolumia is maximal. In majority, however heart failure develops peripartum when the physiological capability for rapid changes in cardiac output may be overwhelmed in the presence of structural cardiac disease
History in cardiac disease aims at Diagnosing the heart disease To clinically classify the heart disease Clinical indicators of heart disease during pregnancy History of progressive dyspnoea/orthopnoea Nocturnal cough Hemoptysis Syncope Chest pain Palpitations

Clinical classification: 1928 by New York Heart Association (NYHA) Class I: Uncompromised - No limitation of physical activity Class II: Slight limitation of physical activity. Women are comfortable at rest But if ordinary physical activity is undertaken discomfort results in the form of excessive fatigue, palpitation, dyspnoea or chest pain Class III: Marked limitation of physical activity Women are comfortable at rest, but less than ordinary activity causes fatigue, palpitation, dyspnoea and chest pain Class IV: Severely compromised - Symptoms even at rest
Past History of cardiac failure in past pregnancy in multi History of rheumatic fever/arthritis/ RHD History of CHD History of Surgery before or in present pregnancy Drug therapy like anticoagulants or penidure prophylaxis Personal History of alcohol or smoking should be asked
Examination - Patient may be uncomfortable at rest Temperature may be increased due to secondary infection Cyanosis: Peripheral or central Clubbing Pulse – Rate: Tachycardia Rhythm: Irregularly irregular pulse-AF, ectopic beats Volume High volume pulse. Aortic regurgitition Thyrotoxicosis Associated anaemia Low volume - Mitral stenosis Collapsing pulse – Aortic regurgitition Respiratory rate increased, orthopnoea may be present B. P. : May reveal associated PIH Wide pulse pressure as in aortic regurgitition Patient in failure: JVP is raised Pedal oedema Tender hepatomegaly Associated Anaemia Thyroid enlargement Dental caries
Cardiac examination in detail Inspection: Precordial bulge Abnormal pulsations - Parasternal heave - Right ventricular hypertrophy Forceful Apical impulse - left ventricular enlargement Palpation: Mitral area - apical impulse location and quality Pulmonary area - Palpable II heart sound Palpation of thrill Percussion: Cardiac borders to be located Auscultation: Mitral area- Opening snap } Mid diastolic murmur } MS Loud S 1 } Pansystolic murmur - MR VSD Aortic area - Ejection systolic murmur conducted to carotids –Aortic stenosis Early Diastolic murmur Aortic regurgitition Pulmonary area - Loud second sound - Pulmonary hypertension Split fixed second sound - ASD Tricuspid area - Pansystolic murmur more during inspiration - TR
Abdominal examination Hepatomegaly Ascitis Fundal Height May be less than expected because of IUGR To rule out CPD as there is no place for trial of labour Respiratory system Basal crepitations - Pulmonary oedema Associated Infections