Goals Give a detailed description of the superficial
- Slides: 21
Goals Give a detailed description of the superficial and internal anatomy of the heart, including the pericardium, the myocardium, and the cardiac muscle. Ch 21: Cardiovascular System - The Heart Explain the functioning of the valves of the heart and how they relate to the heart sounds. Discuss the conductive pathway of the heart, and relate that to clinical uses of the ECG.
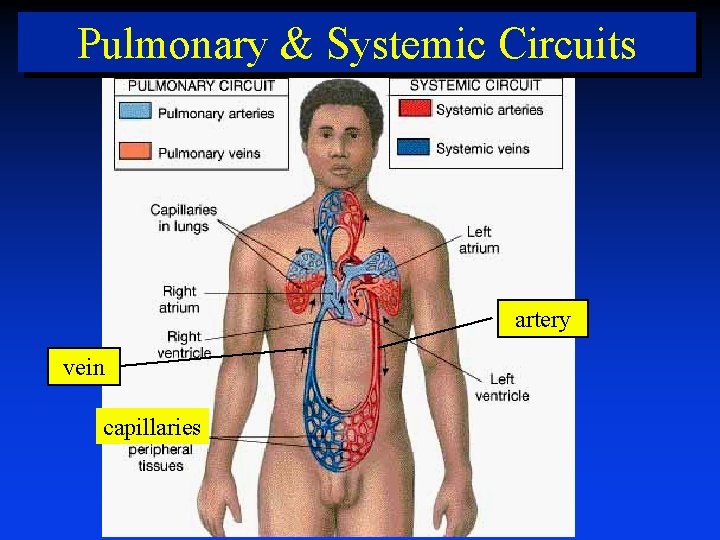
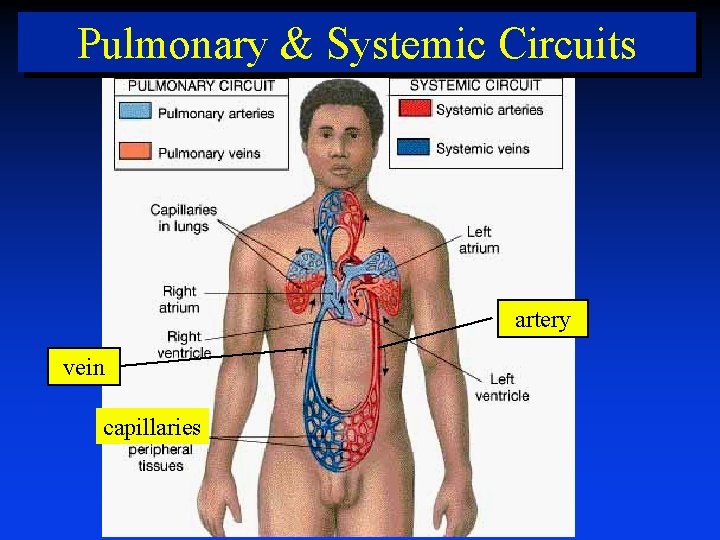
Pulmonary & Systemic Circuits artery vein capillaries
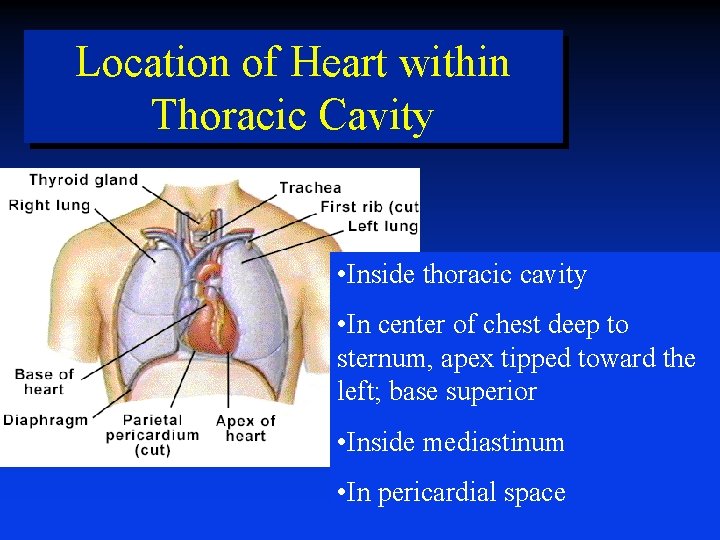
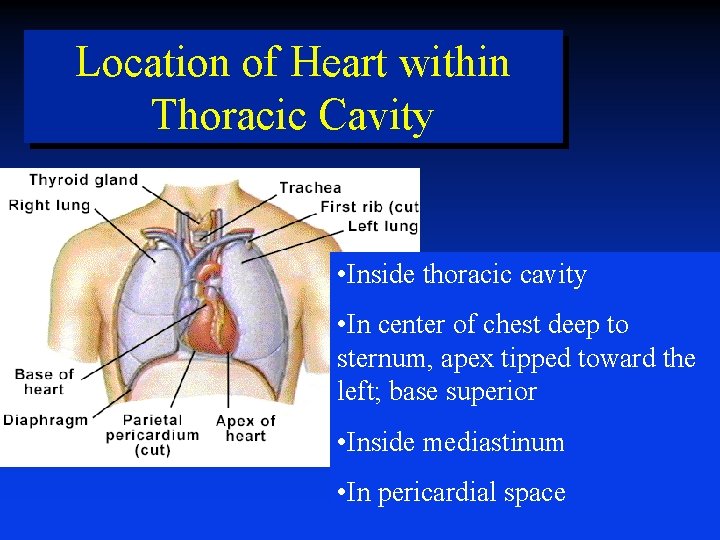
Location of Heart within Thoracic Cavity • Inside thoracic cavity • In center of chest deep to sternum, apex tipped toward the left; base superior • Inside mediastinum • In pericardial space
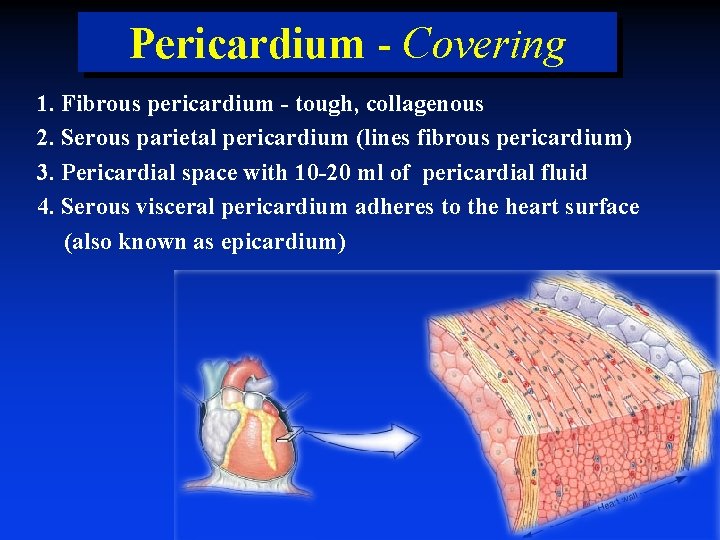
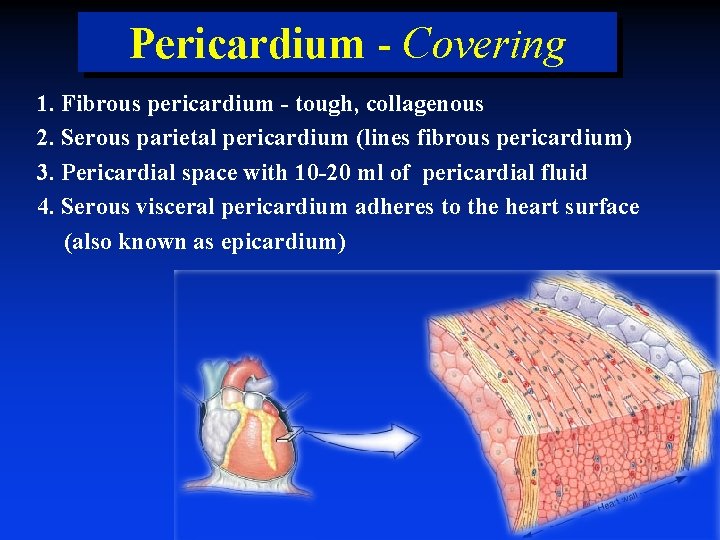
Pericardium - Covering 1. Fibrous pericardium - tough, collagenous 2. Serous parietal pericardium (lines fibrous pericardium) 3. Pericardial space with 10 -20 ml of pericardial fluid 4. Serous visceral pericardium adheres to the heart surface (also known as epicardium)
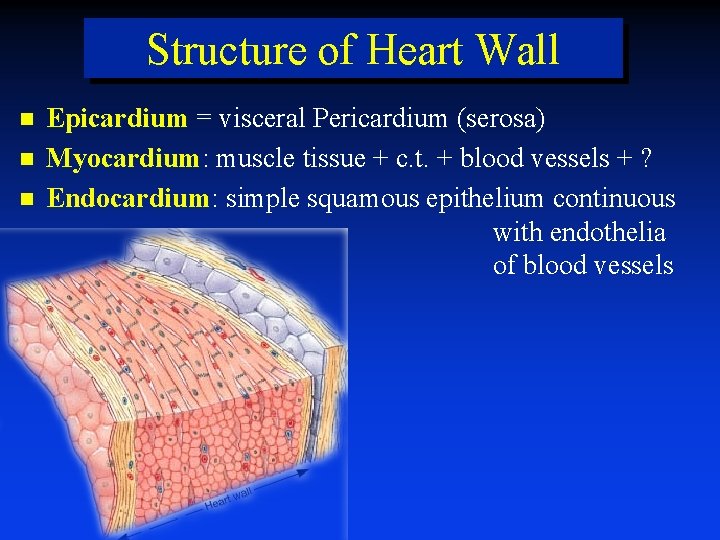
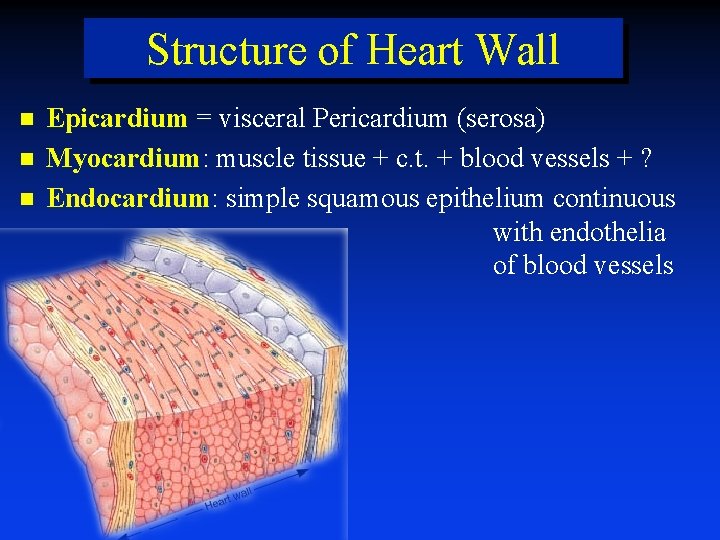
Structure of Heart Wall Epicardium = visceral Pericardium (serosa) Myocardium: muscle tissue + c. t. + blood vessels + ? Endocardium: simple squamous epithelium continuous with endothelia of blood vessels
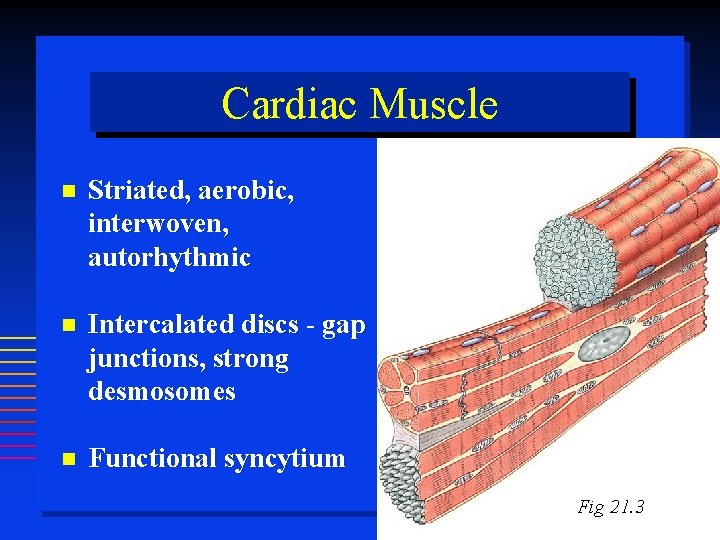
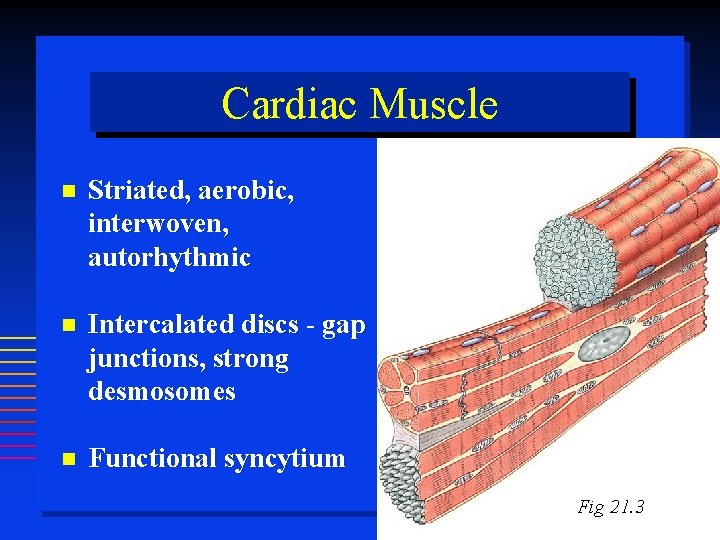
Cardiac Muscle Striated, aerobic, interwoven, autorhythmic Intercalated discs - gap junctions, strong desmosomes Functional syncytium Fig 21. 3
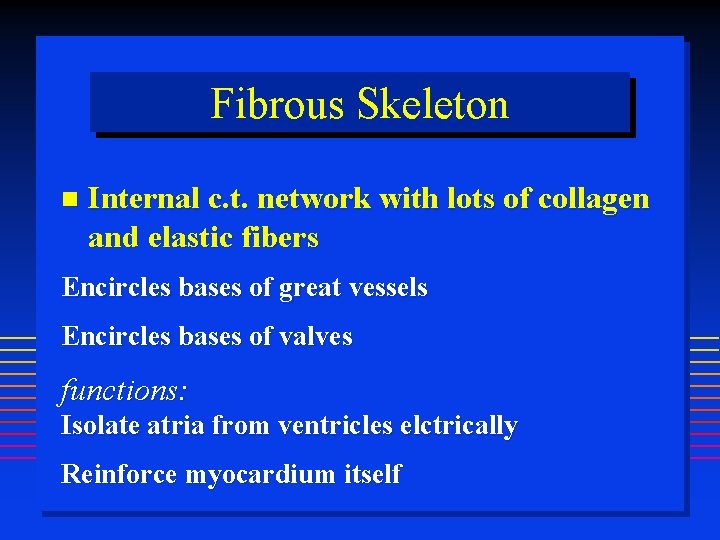
Fibrous Skeleton Internal c. t. network with lots of collagen and elastic fibers Encircles bases of great vessels Encircles bases of valves functions: Isolate atria from ventricles elctrically Reinforce myocardium itself
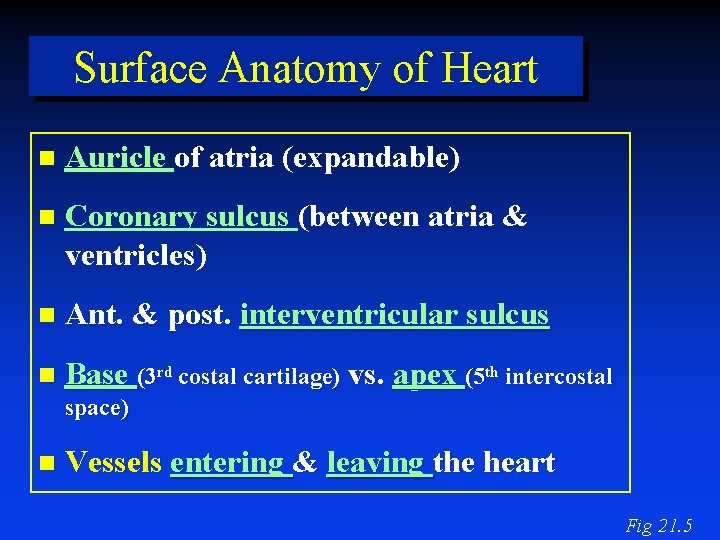
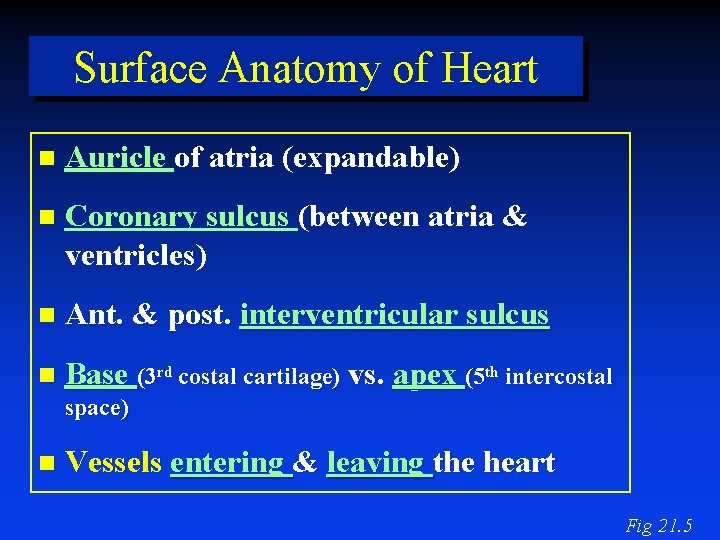
Surface Anatomy of Heart Auricle of atria (expandable) Coronary sulcus (between atria & ventricles) Ant. & post. interventricular sulcus Base (3 rd costal cartilage) vs. apex (5 th intercostal space) Vessels entering & leaving the heart Fig 21. 5
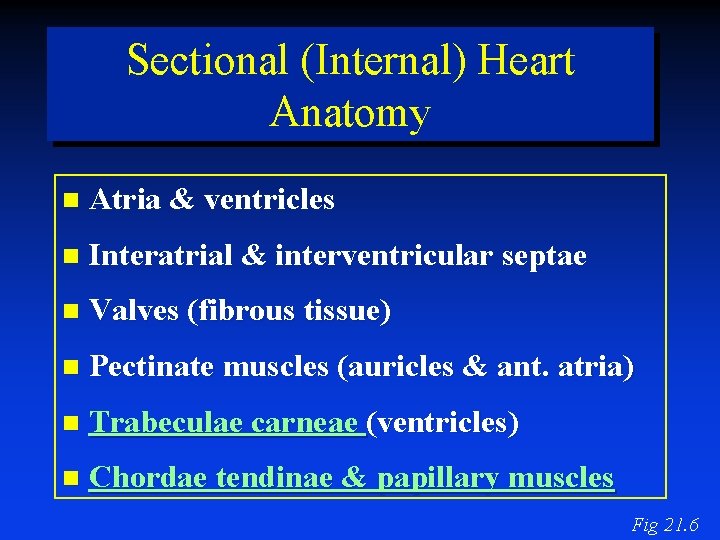
Sectional (Internal) Heart Anatomy Atria & ventricles Interatrial & interventricular septae Valves (fibrous tissue) Pectinate muscles (auricles & ant. atria) Trabeculae carneae (ventricles) Chordae tendinae & papillary muscles Fig 21. 6
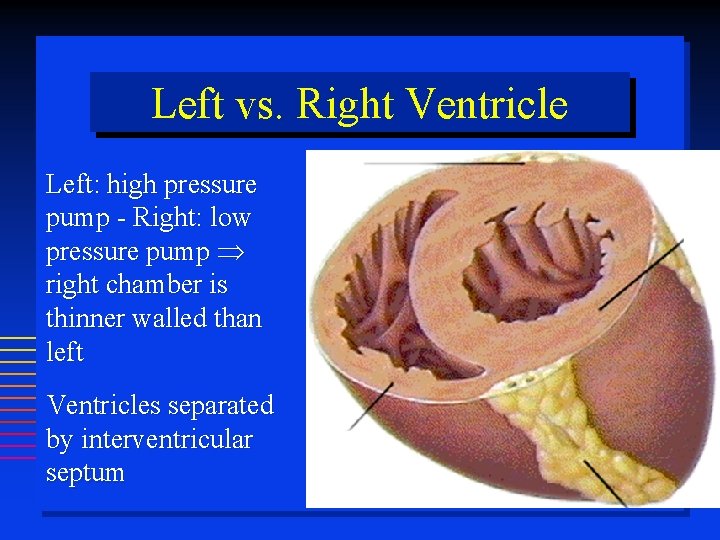
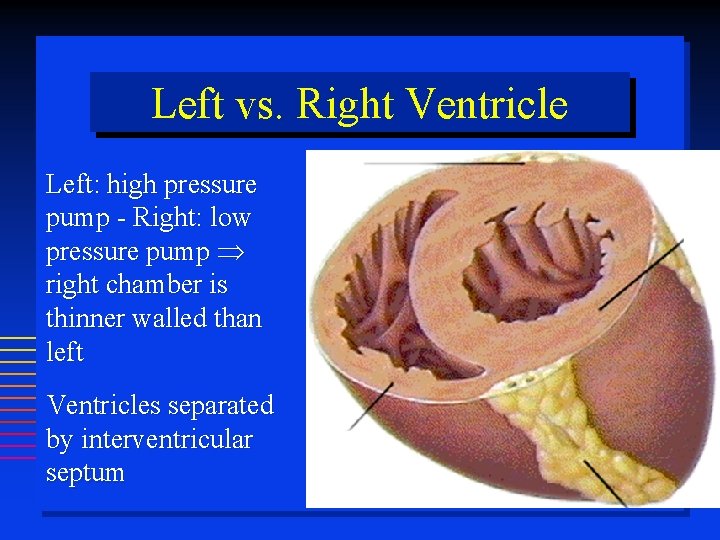
Left vs. Right Ventricle Left: high pressure pump - Right: low pressure pump right chamber is thinner walled than left Ventricles separated by interventricular septum
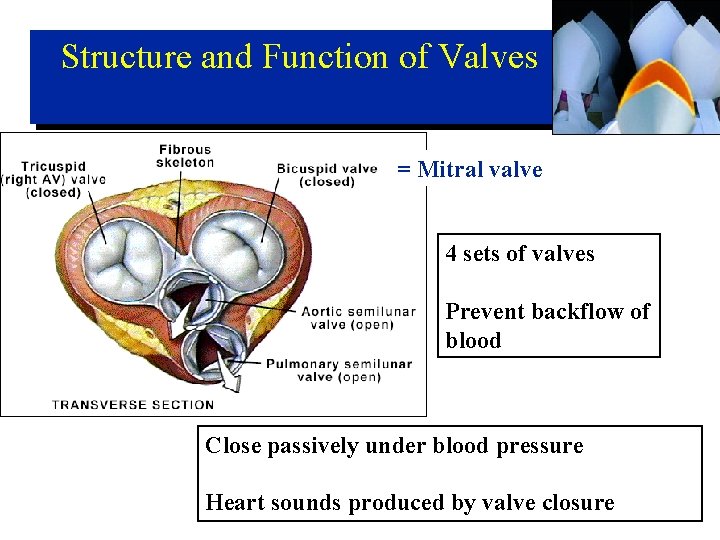
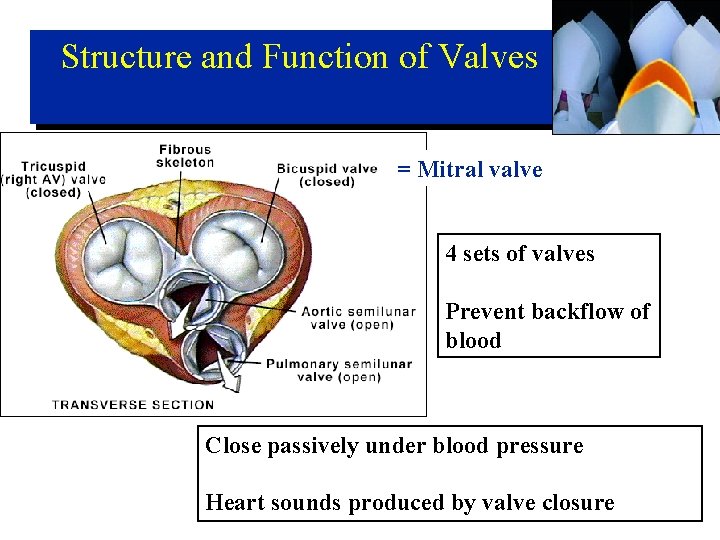
Structure and Function of Valves = Mitral valve 4 sets of valves Prevent backflow of blood Close passively under blood pressure Heart sounds produced by valve closure
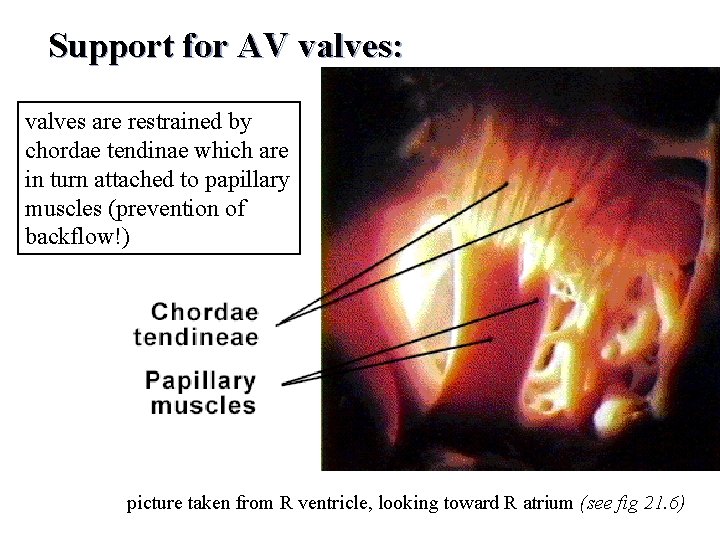
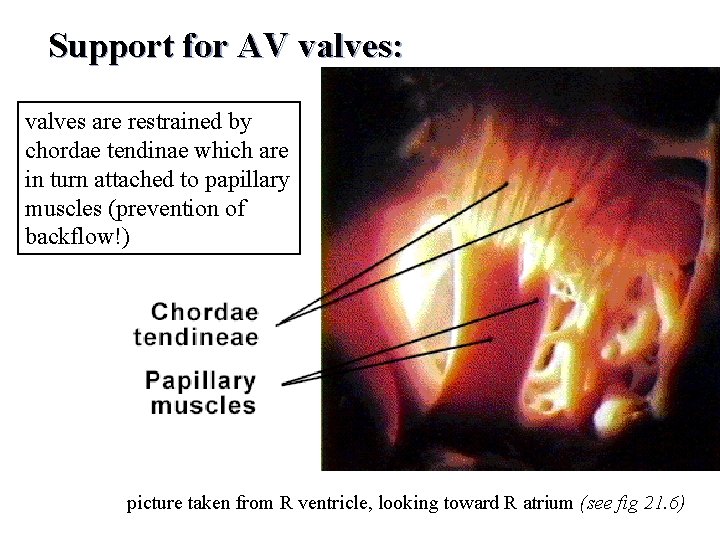
Support for AV valves: valves are restrained by chordae tendinae which are in turn attached to papillary muscles (prevention of backflow!) picture taken from R ventricle, looking toward R atrium (see fig 21. 6)
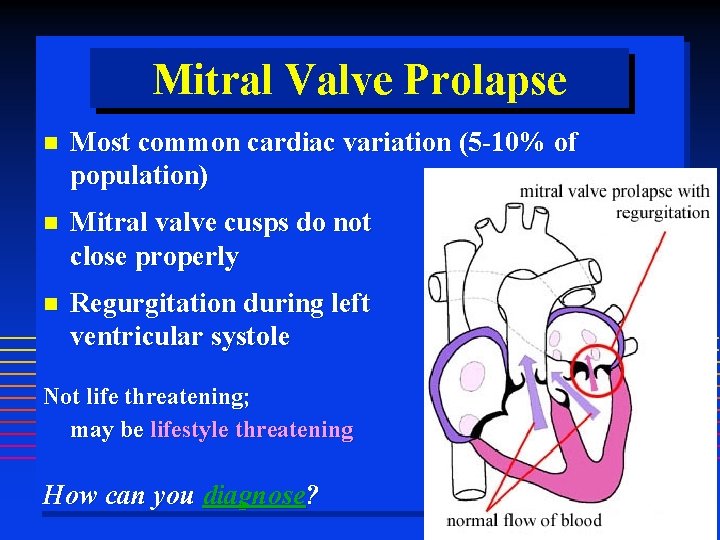
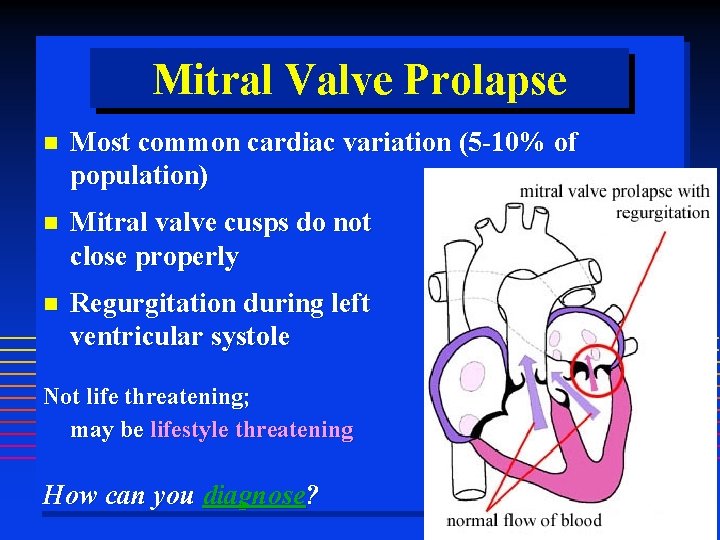
Mitral Valve Prolapse Most common cardiac variation (5 -10% of population) Mitral valve cusps do not close properly Regurgitation during left ventricular systole Not life threatening; may be lifestyle threatening How can you diagnose?
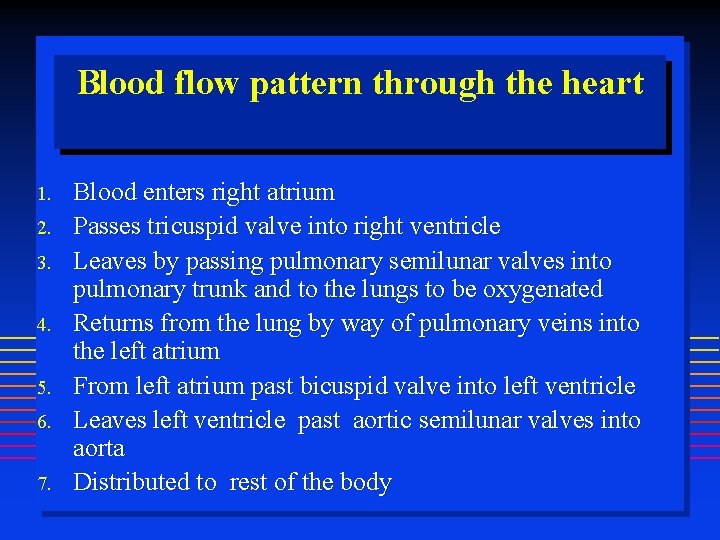
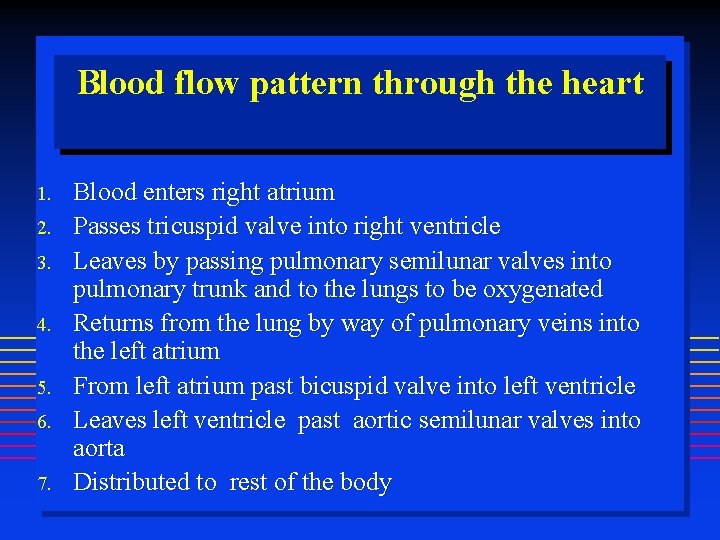
Blood flow pattern through the heart 1. 2. 3. 4. 5. 6. 7. Blood enters right atrium Passes tricuspid valve into right ventricle Leaves by passing pulmonary semilunar valves into pulmonary trunk and to the lungs to be oxygenated Returns from the lung by way of pulmonary veins into the left atrium From left atrium past bicuspid valve into left ventricle Leaves left ventricle past aortic semilunar valves into aorta Distributed to rest of the body
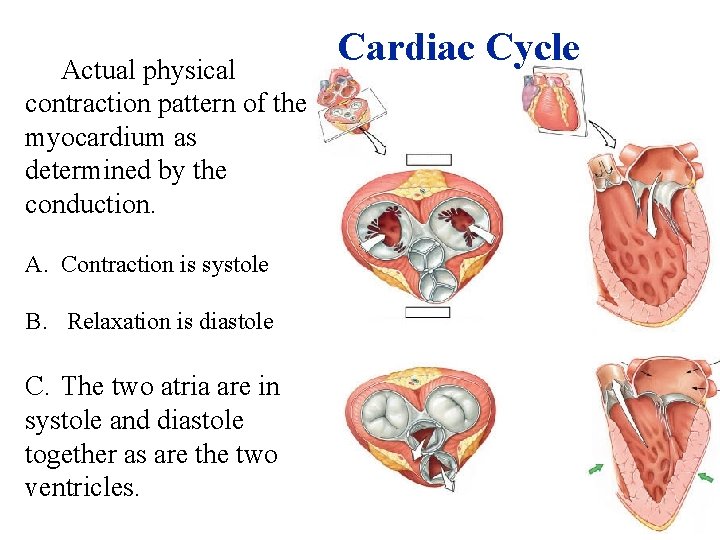
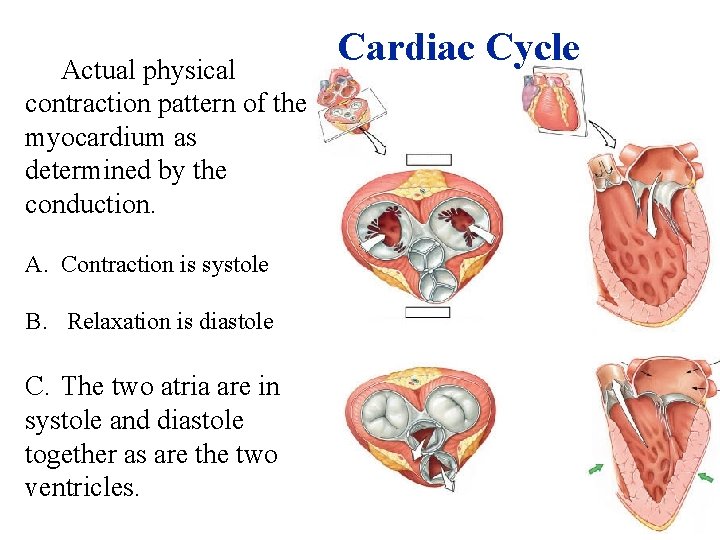
Actual physical contraction pattern of the myocardium as determined by the conduction. A. Contraction is systole B. Relaxation is diastole C. The two atria are in systole and diastole together as are the two ventricles. Cardiac Cycle
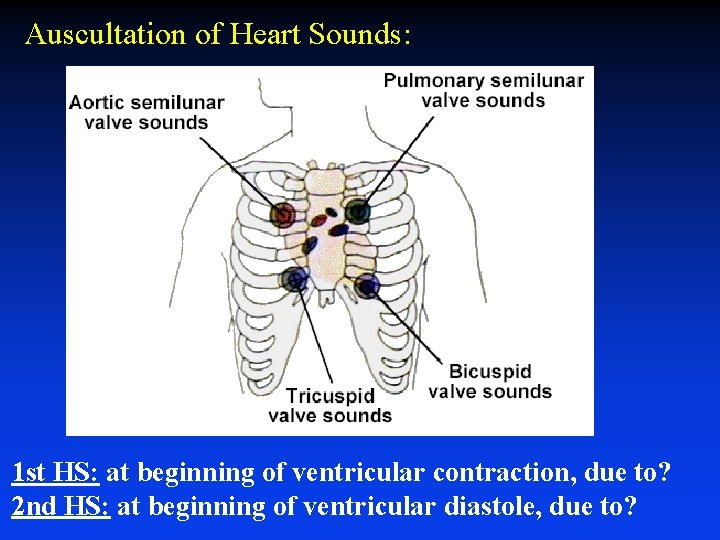
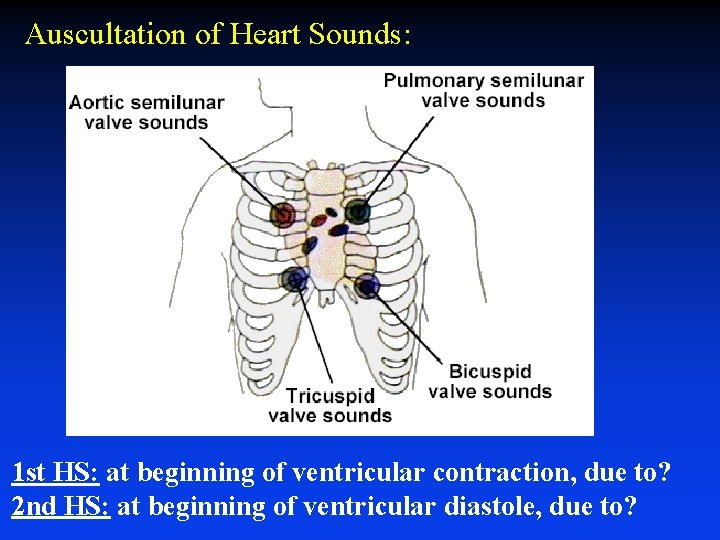
Auscultation of Heart Sounds: 1 st HS: at beginning of ventricular contraction, due to? 2 nd HS: at beginning of ventricular diastole, due to?
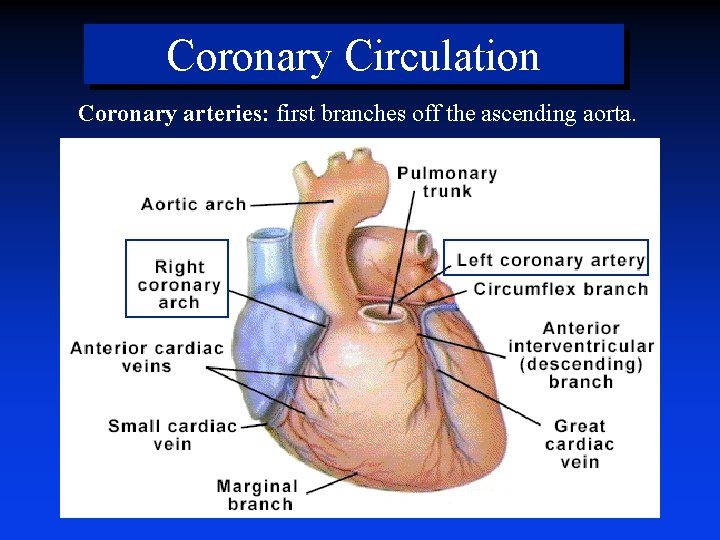
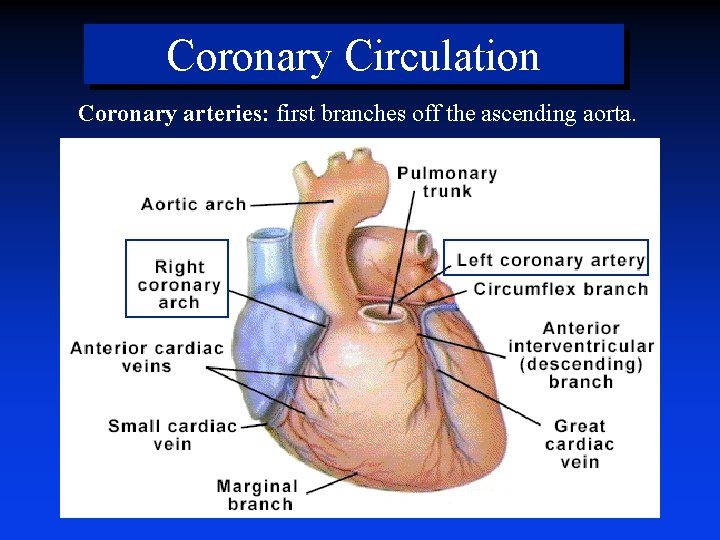
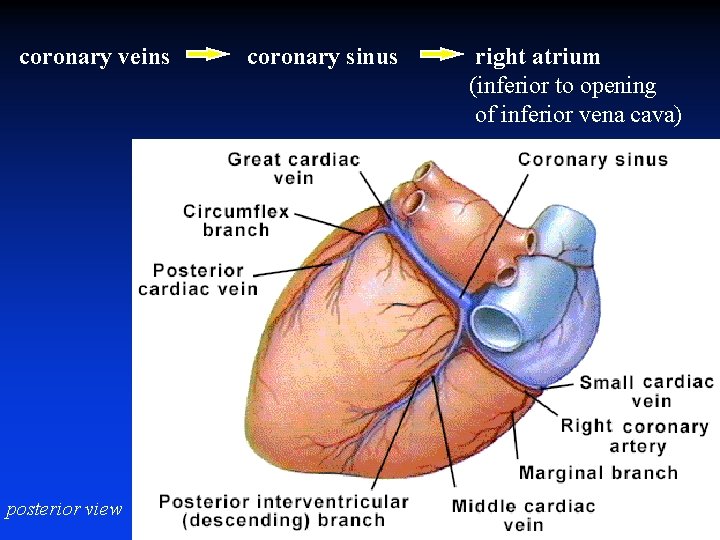
Coronary Circulation Coronary arteries: first branches off the ascending aorta.
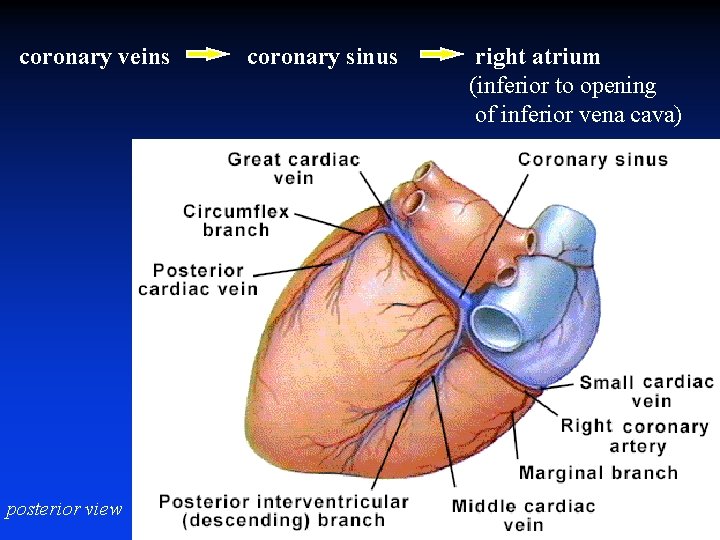
coronary veins posterior view coronary sinus right atrium (inferior to opening of inferior vena cava)
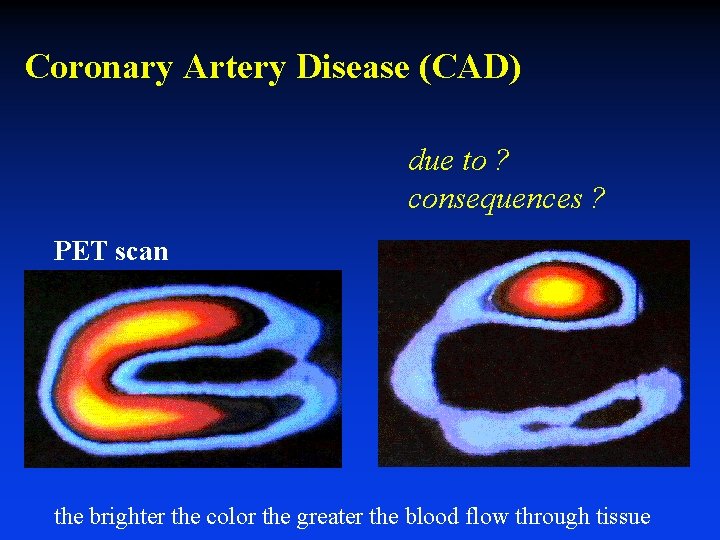
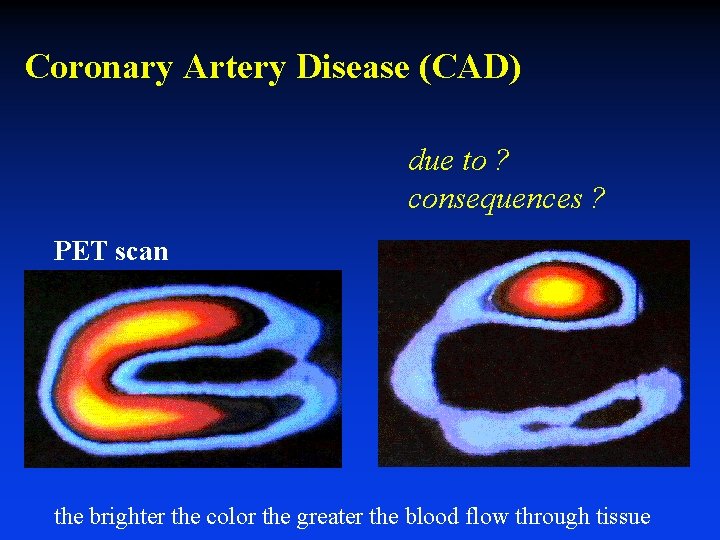
Coronary Artery Disease (CAD) due to ? consequences ? PET scan the brighter the color the greater the blood flow through tissue
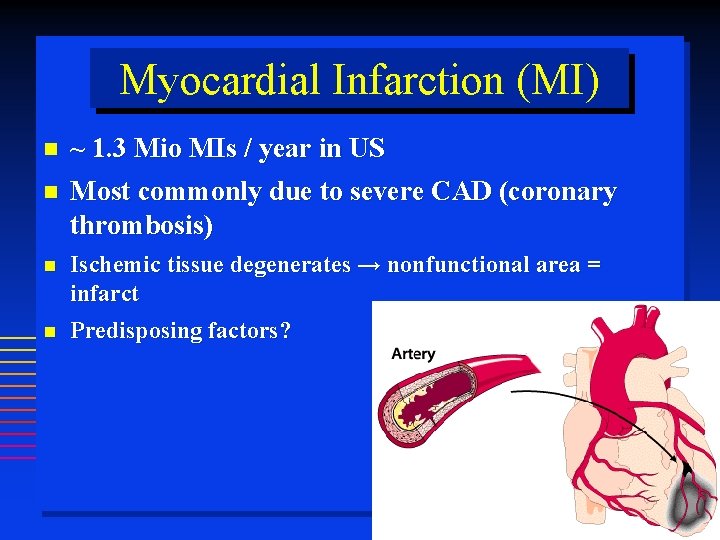
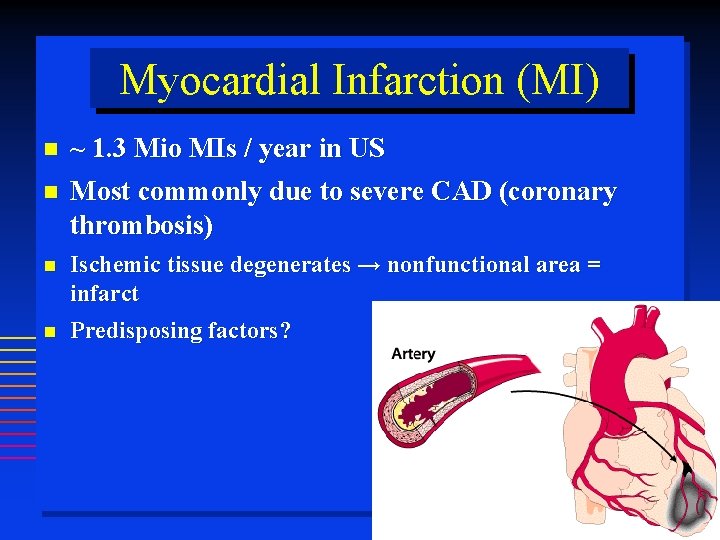
Myocardial Infarction (MI) ~ 1. 3 Mio MIs / year in US Most commonly due to severe CAD (coronary thrombosis) Ischemic tissue degenerates → nonfunctional area = infarct Predisposing factors?
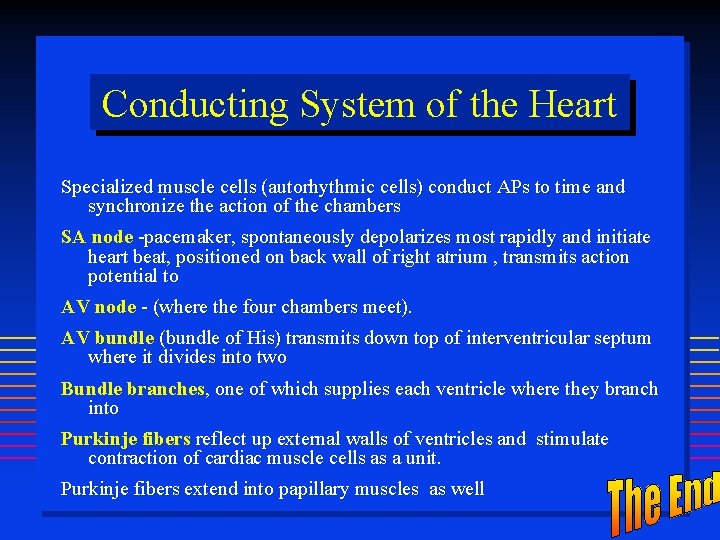
Conducting System of the Heart Specialized muscle cells (autorhythmic cells) conduct APs to time and synchronize the action of the chambers SA node -pacemaker, spontaneously depolarizes most rapidly and initiate heart beat, positioned on back wall of right atrium , transmits action potential to AV node - (where the four chambers meet). AV bundle (bundle of His) transmits down top of interventricular septum where it divides into two Bundle branches, one of which supplies each ventricle where they branch into Purkinje fibers reflect up external walls of ventricles and stimulate contraction of cardiac muscle cells as a unit. Purkinje fibers extend into papillary muscles as well
 Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Use case model
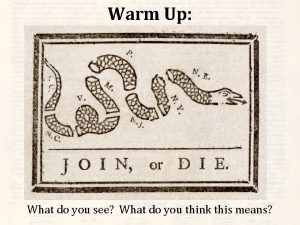
Use case model What is the main idea of give me liberty or give me death
What is the main idea of give me liberty or give me death General goals and specific goals
General goals and specific goals Motivation in consumer behaviour
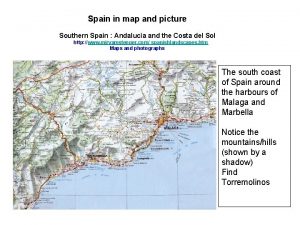
Motivation in consumer behaviour Map of southern spain
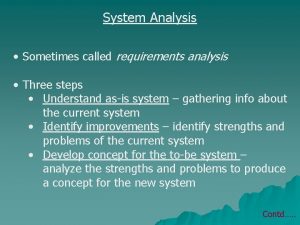
Map of southern spain Analysis is sometimes called
Analysis is sometimes called Short summary of heart of darkness by joseph conrad
Short summary of heart of darkness by joseph conrad Objectives of proposed system
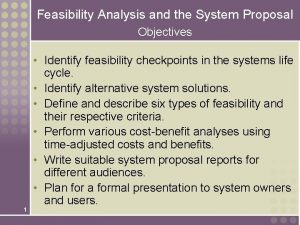
Objectives of proposed system Cima existing requirements
Cima existing requirements Skim listening
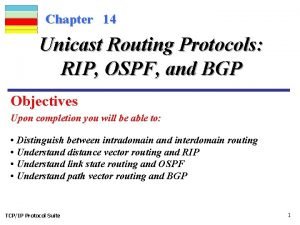
Skim listening Write a detailed note on unicast routing protocols
Write a detailed note on unicast routing protocols Detailed lesson plan about problem solving
Detailed lesson plan about problem solving Assembly drawing engineering
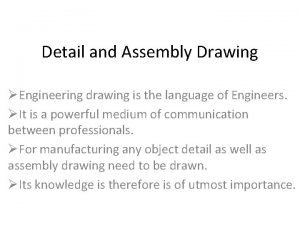
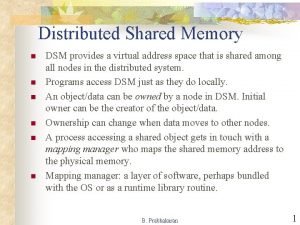
Assembly drawing engineering Show the detailed abstract view of dsm
Show the detailed abstract view of dsm Solid in engineering drawing
Solid in engineering drawing Reading for detail
Reading for detail Function oriented design
Function oriented design Elizabeth bishop themes
Elizabeth bishop themes Uml book
Uml book What is detail drawing
What is detail drawing