General Practice Staff Risk Assessment Resource Pack 10
- Slides: 19
General Practice Staff Risk Assessment Resource Pack 10 July 2020 Version 1. 0 Next review: 10 August 2020
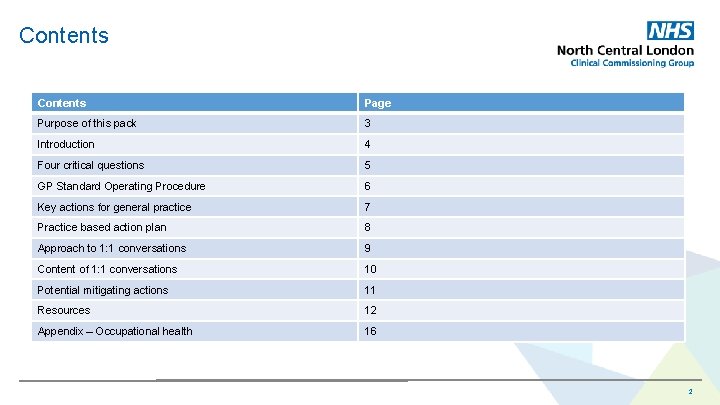
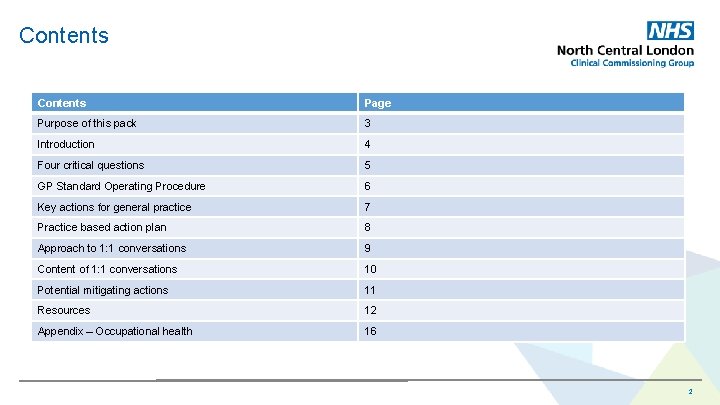
Contents Page Purpose of this pack 3 Introduction 4 Four critical questions 5 GP Standard Operating Procedure 6 Key actions for general practice 7 Practice based action plan 8 Approach to 1: 1 conversations 9 Content of 1: 1 conversations 10 Potential mitigating actions 11 Resources 12 Appendix – Occupational health 16 2
Purpose of this pack • NHSE/I has advised that to protect our workforce, staff should be risk assessed to identify those at increased risk from Covid-19. • Employers should risk-assess all staff. Prioritising black, Asian, minority and ethnic (BAME) and other high-risk groups, and develop plans to help mitigate the risks. • The following slides bring together current available resources to support the risk assessment process. • As national guidance is subject to change, you are advised to check that you are accessing the most recent documentation. NB: We have received many questions about the undertaking of this work and we expect there will be more formal national guidance to support this work in due course. Guidance has been sought from experts at national and regional level to support the work of GPs in North Central London. For any enquiries relating to this pack please contact: ncl. covid-19 enquiries@nhs. net The CCG and training hubs across North Central London are scheduling a series of webinars / educational events in July 2020 to support this work. 3
Introduction • Following the publication of national NHS guidance, the NHS and • Further to the publication of guidance from the Faculty of other employers are in the process of providing risk Occupational Medicine, many practices have started to undertake assessments for staff potentially exposed to Covid-19. this work. There a number of risk assessment tools available, but none are nationally recommended at this • Data demonstrates the virus has disproportionately affected moment. black, Asian and minority ethnic (BAME) staff, teams and the wider community, highlighting systemic health inequalities. • We recommend that practices proceed to undertake these There also recognised risks associated with worse outcomes in assessments making an independent and pragmatic decision relation to age and long-term conditions. regarding the tool they use. This is aligned with the recommended approach from Londonwide LMC (M-Word 24 th June • Overall, we recognise that for multiple reasons the impact of Covid- 2020). 19 has been detrimental to the wellbeing and resilience of all our workforce. • Risk assessments for all staff including general practice is now a pressing undertaking and has a deadline for completion. The • Given the uncertainty of future surges of Covid-19, it is very uptake is to be monitored and reported as a monthly sitrep. important that we use this opportunity to ensure that our staff are fully aware and protected so as to minimise risks to themselves, their colleagues and patients, as well as attending to the environment within which they work. This is a responsibility as an employer and a commitment we make to support our colleagues. 4
Four critical questions Have you risk assessed staff? What mitigating actions have been taken? Are you compliant with the SOP? Have you provided access to wellbeing support? 5
GP Standard Operating Procedure Following feedback from GP practice colleagues and representatives, NHSE/I has revised the current GP SOP v 3 section about staff at increased risk from Covid-19 and risk assessments as follows: The government has issued guidance on shielding for people defined on medical grounds as extremely clinically vulnerable from Covid-19. Staff who fall into these categories should not see patients face-to-face, this takes precedence over any other risk assessments. All other staff including black, Asian, minority and ethnic (BAME) staff and people identified as clinically vulnerable who are asked to apply stringent social distancing should be risk assessed to consider if they should see patients face-to-face. The Faculty of Occupational Medicine has published the Risk Reduction Framework for NHS staff (including BAME staff) who are at risk of Covid-19 infection. NHS Employers has also published guidance on risk assessments for staff. Staff may also be referred to an occupational health professional for further advice and support. Details of local occupational health service are available in the appendix. 6
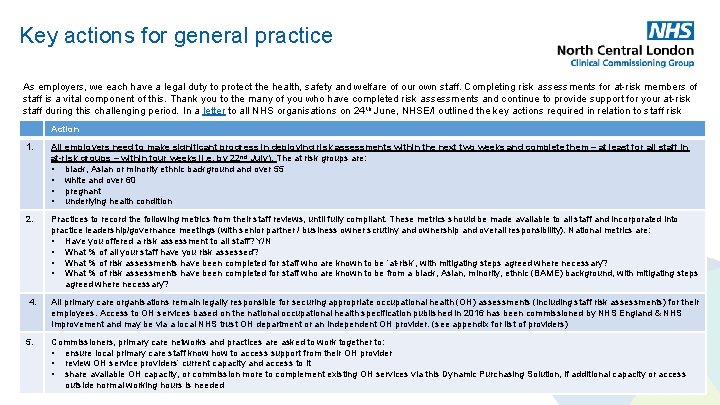
Key actions for general practice As employers, we each have a legal duty to protect the health, safety and welfare of our own staff. Completing risk assessments for at-risk members of staff is a vital component of this. Thank you to the many of you who have completed risk assessments and continue to provide support for your at-risk staff during this challenging period. In a letter to all NHS organisations on 24 th June, NHSE/I outlined the key actions required in relation to staff risk assessments: Action 1. All employers need to make significant progress in deploying risk assessments within the next two weeks and complete them – at least for all staff in at-risk groups – within four weeks (i. e. by 22 nd July). The at risk groups are: • black, Asian or minority ethnic background and over 55 • white and over 60 • pregnant • underlying health condition 2. Practices to record the following metrics from their staff reviews, until fully compliant. These metrics should be made available to all staff and incorporated into practice leadership/governance meetings (with senior partner / business owner scrutiny and ownership and overall responsibility). National metrics are: • Have you offered a risk assessment to all staff? Y/N • What % of all your staff have you risk assessed? • What % of risk assessments have been completed for staff who are known to be ‘at-risk’, with mitigating steps agreed where necessary? • What % of risk assessments have been completed for staff who are known to be from a black, Asian, minority, ethnic (BAME) background, with mitigating steps agreed where necessary? 4. All primary care organisations remain legally responsible for securing appropriate occupational health (OH) assessments (including staff risk assessments) for their employees. Access to OH services based on the national occupational health specification published in 2016 has been commissioned by NHS England & NHS Improvement and may be via a local NHS trust OH department or an independent OH provider. (see appendix for list of providers) 5. Commissioners, primary care networks and practices are asked to work together to: • ensure local primary care staff know how to access support from their OH provider • review OH service providers’ current capacity and access to it • share available OH capacity, or commission more to complement existing OH services via this Dynamic Purchasing Solution, if additional capacity or access outside normal working hours is needed 7
Practice based action plans should include: • Plan for scheduling 1: 1 risk assessment meetings with all members of staff. • Mechanism for recording national reporting metrics. • Remind all staff of the importance of proper use of PPE and IPC as a means to ensuring they stay safe and maintain a safe environment for other staff and patients alike. • Refresh understanding on guidance on the use of PPE. • Refresh understanding on Guidance of Infection Prevention & Control for Primary Care. • Refresh understanding on Guidance in management of social distancing in the workplace. • Review all staff risk status. Maintain appropriate documentation of the conversation in the staff record. • Review approach for the practice team collectively, with sensitivity to the confidentiality of individual staff members. • Be able to sign-post to local services to for staff support (see resources and wellbeing slides). NB: The risk assessment process may need to be repeated at a future date, subject to changes in circumstances. 8
Approach to 1: 1 conversations The following are some key points to consider as you embark on the risk assessment interviews Some of the reference material included is written for use in a hospital settings, however provides useful contextual understanding around how to do this. Approach: • This is a person-centred conversation that needs to be undertaken with sensitivity. • It is good practice for the interview to be conducted in the context of a wellbeing conversation, using open, coaching style questions. • The interviews should be undertaken by a senior line manager or partner. • The 1 -2 -1 template can be shared with staff in advance of the interview [see template on next page]. • The staff member should also be offered the opportunity for an independent assessor should this be preferred. • Where the risk assessment is completed by someone other than the line manager, the confidentiality of the conversation should be respected and only the risk status returned. • In addition to recording the metrics requested nationally, it is good practice to track and capture mitigation and redeployments. • In circumstances of complexity it may be necessary to refer a member of staff for an occupational health assessment (see appendix). Referral to an independent third party • Signposting to an independent third party is important should the staff member feel uncomfortable having the conversation with a named line manager or be dissatisfied with the outcome or action taken. • NCL CCG has identified a Freedom to Speak Up Guardian to provide independent oversight and advice. Please contact Dr Dominic Roberts dominicroberts@nhs. net, to learn more. • Where staff decline to agree to a risk assessment with their line manager it may be helpful for an external party to follow up to address any concerns from the individual and as an alternative method of completing risk assessments. 9
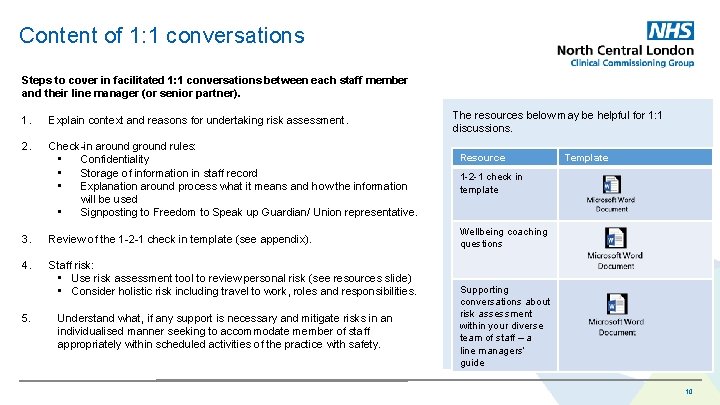
Content of 1: 1 conversations Steps to cover in facilitated 1: 1 conversations between each staff member and their line manager (or senior partner). 1. Explain context and reasons for undertaking risk assessment. 2. Check-in around ground rules: • Confidentiality • Storage of information in staff record • Explanation around process what it means and how the information will be used • Signposting to Freedom to Speak up Guardian/ Union representative. 3. Review of the 1 -2 -1 check in template (see appendix). 4. Staff risk: • Use risk assessment tool to review personal risk (see resources slide) • Consider holistic risk including travel to work, roles and responsibilities. 5. Understand what, if any support is necessary and mitigate risks in an individualised manner seeking to accommodate member of staff appropriately within scheduled activities of the practice with safety. The resources below may be helpful for 1: 1 discussions. Resource Template 1 -2 -1 check in template Wellbeing coaching questions Supporting conversations about risk assessment within your diverse team of staff – a line managers’ guide 10
Potential mitigating actions Line managers and senior partners should listen carefully to concerns and provide support and consider adjustments or redeployment, where possible, for any staff identified as being at greater risk. Adjustments may include: 1. Limiting duration of close interaction with the patient (for example, preparing everything in advance away from them). 2. Avoiding public transport/rush hour through adjustments to work hours. 3. Asking patients to wear a mask for staff member interaction. 4. Asking that only the patient is in attendance for home visits/outreach where possible. 5. Providing appropriate PPE for staff members for all interactions with patients or specimens. 6. Redeploying staff to a lower risk area. 7. Encouraging remote working. 8. Varying working patterns. More information is available from NHS Employers 11
Resources Risk assessment tools NB: There a number of risk assessment tools available, but none are nationally recommended at this moment. • NHS Employers guidance on carrying out risk assessments • Londonwide LMC Guidance on maintaining staff safety in general practice - including signposting to scoring systems • The Faculty of Occupational Medicine has published the Risk Reduction Framework for NHS staff. • British association of physicians of Indian origin: https: //www. bapio. co. uk/risk-assessment/ and https: //www. bapio. co. uk/wp-content/uploads/2020/05/Risk-Assessment. Tool. pdf • Safety Assessment and Decision (SAAD) Score 12
Staff wellbeing These are exceptionally difficult times for staff some of whom may have experienced personal loss as a result of covid-19 or are finding it generally difficult to cope in the new working In new and very different ways. It is therefore vitally important that staff are provided with access to support. Staff wellbeing Confidential help for NHS staff: • Confidential support by phone or text • Bereavement support line • RCN counselling service Other resources: • • • Wellbeing apps (also see next slide) NCL CCG health and wellbeing NHS E webpage for wellbeing for staff LMC – caring for yourself and your practice team Together in mind – a wellbeing and mental health resource for NCL and NEL health and care staff 13
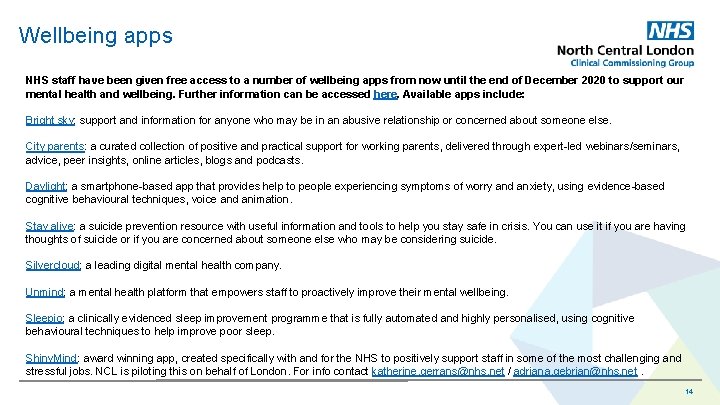
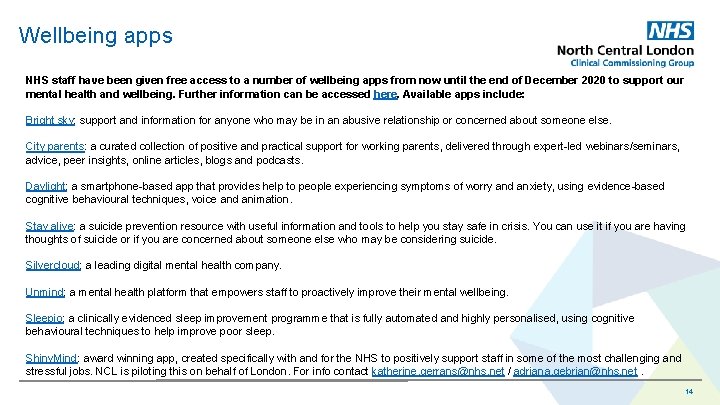
Wellbeing apps NHS staff have been given free access to a number of wellbeing apps from now until the end of December 2020 to support our mental health and wellbeing. Further information can be accessed here. Available apps include: Bright sky: support and information for anyone who may be in an abusive relationship or concerned about someone else. City parents: a curated collection of positive and practical support for working parents, delivered through expert-led webinars/seminars, advice, peer insights, online articles, blogs and podcasts. Daylight: a smartphone-based app that provides help to people experiencing symptoms of worry and anxiety, using evidence-based cognitive behavioural techniques, voice and animation. Stay alive: a suicide prevention resource with useful information and tools to help you stay safe in crisis. You can use it if you are having thoughts of suicide or if you are concerned about someone else who may be considering suicide. Silvercloud: a leading digital mental health company. Unmind: a mental health platform that empowers staff to proactively improve their mental wellbeing. Sleepio: a clinically evidenced sleep improvement programme that is fully automated and highly personalised, using cognitive behavioural techniques to help improve poor sleep. Shiny. Mind: award winning app, created specifically with and for the NHS to positively support staff in some of the most challenging and stressful jobs. NCL is piloting this on behalf of London. For info contact katherine. gerrans@nhs. net / adriana. gebrian@nhs. net. 14
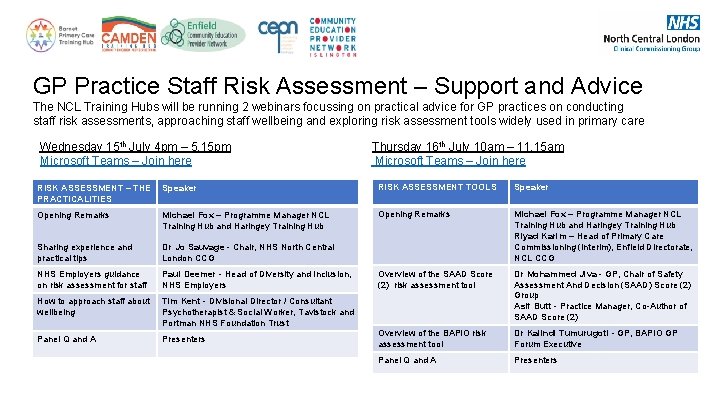
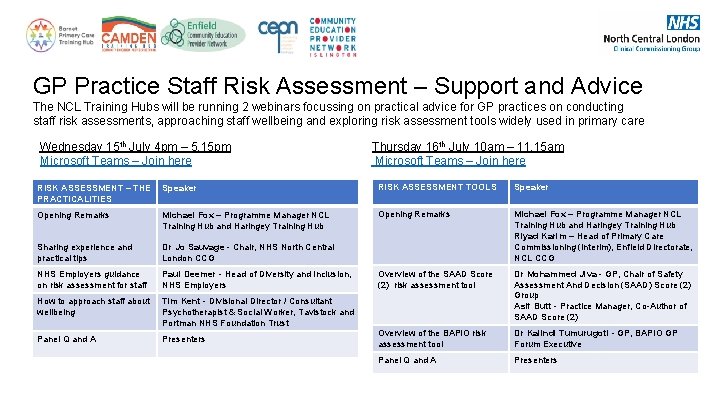
GP Practice Staff Risk Assessment – Support and Advice The NCL Training Hubs will be running 2 webinars focussing on practical advice for GP practices on conducting staff risk assessments, approaching staff wellbeing and exploring risk assessment tools widely used in primary care Wednesday 15 th July 4 pm – 5. 15 pm Thursday 16 th July 10 am – 11. 15 am Microsoft Teams – Join here Microsoft Teams – Join here RISK ASSESSMENT – THE PRACTICALITIES Speaker RISK ASSESSMENT TOOLS Speaker Opening Remarks Michael Fox – Programme Manager NCL Training Hub and Haringey Training Hub Opening Remarks Sharing experience and practical tips Dr Jo Sauvage - Chair, NHS North Central London CCG Michael Fox – Programme Manager NCL Training Hub and Haringey Training Hub Riyad Karim – Head of Primary Care Commissioning (interim), Enfield Directorate, NCL CCG NHS Employers guidance on risk assessment for staff Paul Deemer - Head of Diversity and Inclusion, NHS Employers Overview of the SAAD Score (2) risk assessment tool How to approach staff about wellbeing Tim Kent - Divisional Director / Consultant Psychotherapist & Social Worker, Tavistock and Portman NHS Foundation Trust Dr Mohammed Jiva - GP, Chair of Safety Assessment And Decision (SAAD) Score (2) Group Asif Butt - Practice Manager, Co-Author of SAAD Score (2) Panel Q and A Presenters Overview of the BAPIO risk assessment tool Dr Kalindi Tumurugoti - GP, BAPIO GP Forum Executive Panel Q and A Presenters
Appendix – Occupational health services
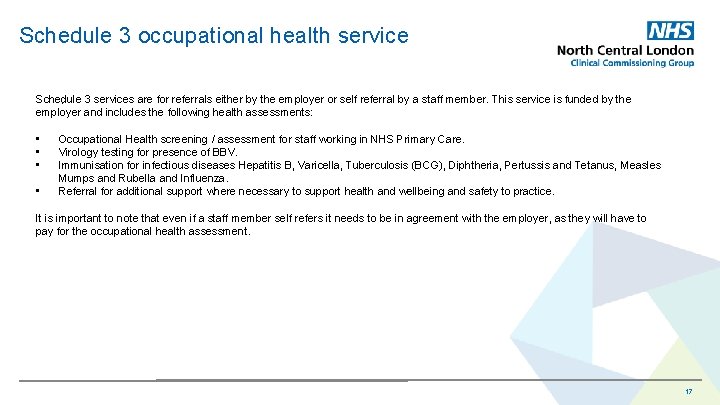
Schedule 3 occupational health service Schedule 3 services are for referrals either by the employer or self referral by a staff member. This service is funded by the . employer and includes the following health assessments: • • Occupational Health screening / assessment for staff working in NHS Primary Care. Virology testing for presence of BBV. Immunisation for infectious diseases Hepatitis B, Varicella, Tuberculosis (BCG), Diphtheria, Pertussis and Tetanus, Measles Mumps and Rubella and Influenza. Referral for additional support where necessary to support health and wellbeing and safety to practice. It is important to note that even if a staff member self refers it needs to be in agreement with the employer, as they will have to pay for the occupational health assessment. 17
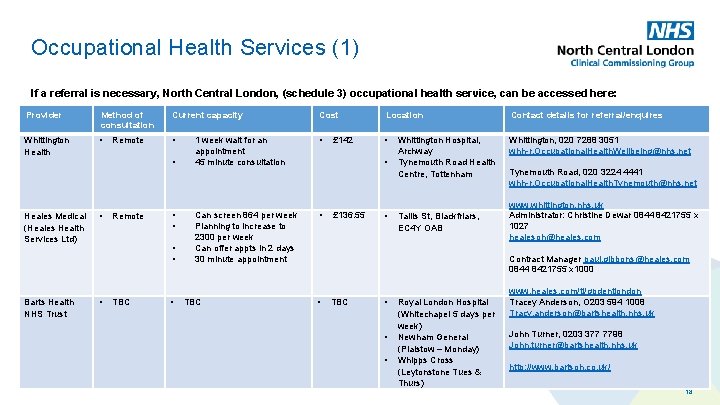
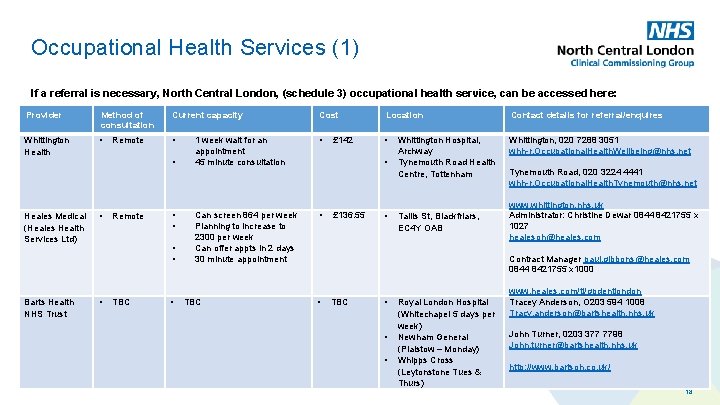
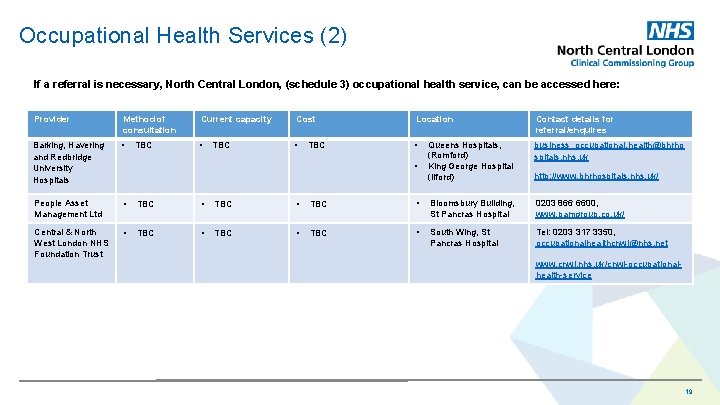
Occupational Health Services (1) If a referral is necessary, North Central London, (schedule 3) occupational health service, can be accessed here: Provider Method of consultation Current capacity Cost Location Contact details for referral/enquires Whittington Health • • Whittington, 020 7288 3051 whh-r. Occupational. Health. Wellbeing@nhs. net Heales Medical (Heales Health . Services Ltd) Barts Health NHS Trust Remote • • • TBC • 1 week wait for an appointment 45 minute consultation Can screen 864 per week Planning to increase to 2300 per week Can offer appts in 2 days 30 minute appointment TBC £ 142 • • £ 136. 55 • Whittington Hospital, Archway Tynemouth Road Health Centre, Tottenham Tallis St, Blackfriars, EC 4 Y OAB Tynemouth Road, 020 3224 4441 whh-r. Occupational. Health. Tynemouth@nhs. net www. whittington. nhs. uk Administrator: Christine Dewar 0844 8421755 x 1027 healesoh@heales. com Contract Manager paul. gibbons@heales. com 0844 8421755 x 1000 • TBC • • • Royal London Hospital (Whitechapel 5 days per week) Newham General (Plaistow – Monday) Whipps Cross (Leytonstone Tues & Thurs) www. heales. com/tl/gpdentlondon Tracey Anderson, O 203 594 1008 Tracy. anderson@bartshealth. nhs. uk John Turner, 0203 377 7798 John. turner@bartshealth. nhs. uk http: //www. bartsoh. co. uk/ 18
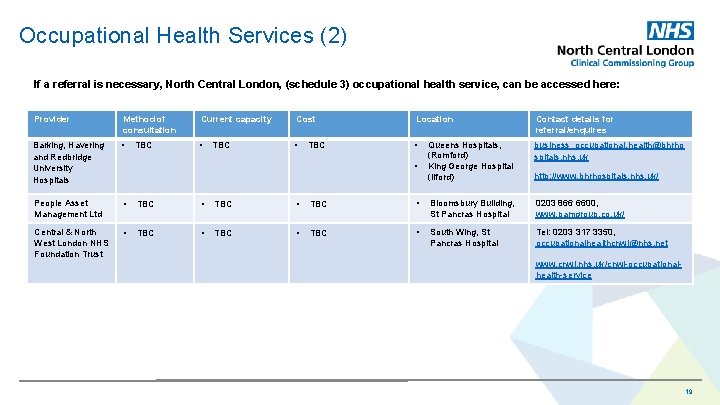
Occupational Health Services (2) If a referral is necessary, North Central London, (schedule 3) occupational health service, can be accessed here: Provider Method of consultation Current capacity Cost Location Contact details for referral/enquires Barking, Havering and Redbridge University Hospitals • • Queens Hospitals, (Romford) King George Hospital (Ilford) business_occupational. health@bhrho spitals. nhs. uk People Asset Management Ltd • TBC • Bloomsbury Building, St Pancras Hospital 0203 866 6600, www. pamgroup. co. uk/ Central & North West London NHS Foundation Trust • TBC • South Wing, St Pancras Hospital Tel: 0203 317 3350, occupationalhealthcnwl@nhs. net TBC TBC • . http: //www. bhrhospitals. nhs. uk/ www. cnwl. nhs. uk/cnwl-occupationalhealth-service 19