GCWMS Assessment key factors Dr Ross Shearer Clinical
- Slides: 24
GCWMS Assessment key factors Dr. Ross Shearer, Clinical Psychologist & Rhonda Wilkie, Specialist Dietitian GCWMS
Traditional process Appointed n 1: 1 n Diet and weight history→ Nutrition therapy targeted at weight loss + (Advice on physical activity) + (Advice on behaviour change strategies) n Variable monitoring n 2
Traditional approach Didactic n Emphasis on dietary change n Variable emphasis on behaviour change n Variable emphasis on physical activity n Goal oriented n n therapist goals vs client’s goals 3
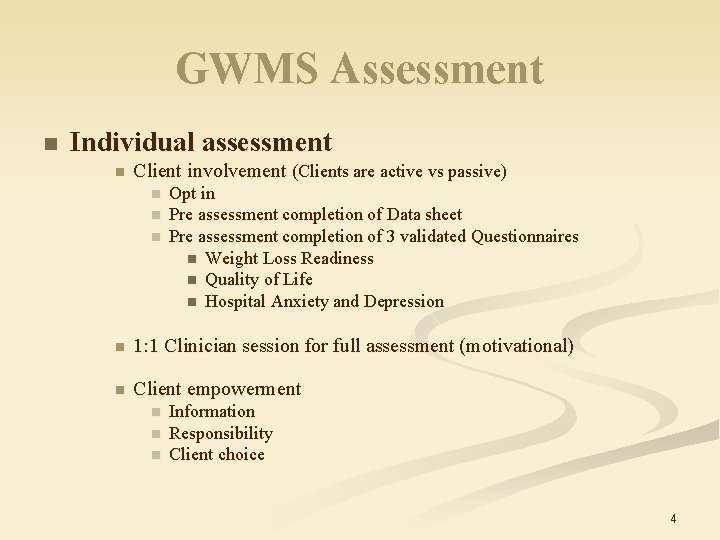
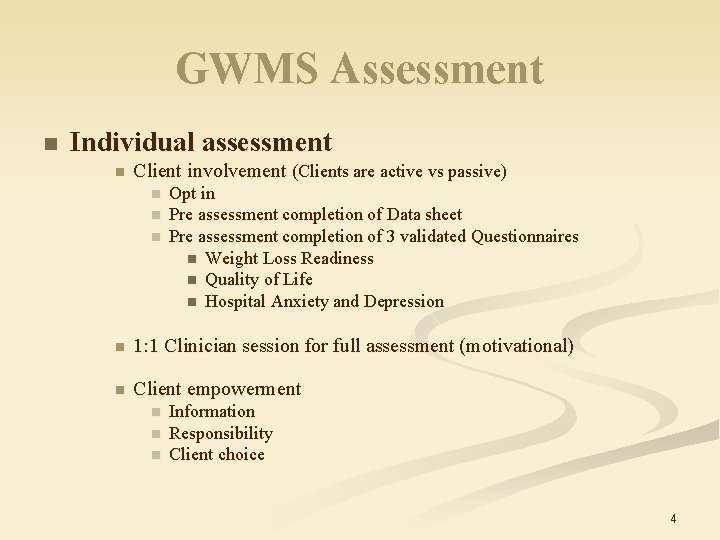
GWMS Assessment n Individual assessment n Client involvement (Clients are active vs passive) n n n Opt in Pre assessment completion of Data sheet Pre assessment completion of 3 validated Questionnaires n Weight Loss Readiness n Quality of Life n Hospital Anxiety and Depression n 1: 1 Clinician session for full assessment (motivational) n Client empowerment n n n Information Responsibility Client choice 4
Client empowerment - Information n n Group size / frequency Group Content n n (what) (how) Role of Group n n Diet Activity Behaviour change Support Learning from others normalisation Lead clinicians 5
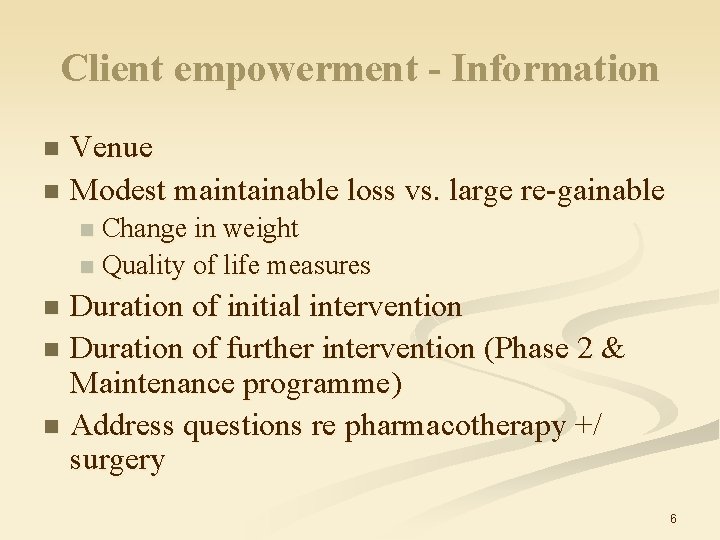
Client empowerment - Information Venue n Modest maintainable loss vs. large re-gainable n Change in weight n Quality of life measures n Duration of initial intervention n Duration of further intervention (Phase 2 & Maintenance programme) n Address questions re pharmacotherapy +/ surgery n 6
Client responsibility Commitment n Attendance in full (encouraged) n Participation n Sessions n Intervention n n Diet, Activity and Behaviour changes n Self monitoring Period of intervention n Period of maintenance n 7
Client choice n 6 months opt in period after assessment n Client takes final decision n Resource management n staggered opt in more manageable n ? ? Ensures intervention used by more motivated clients ? ? 8
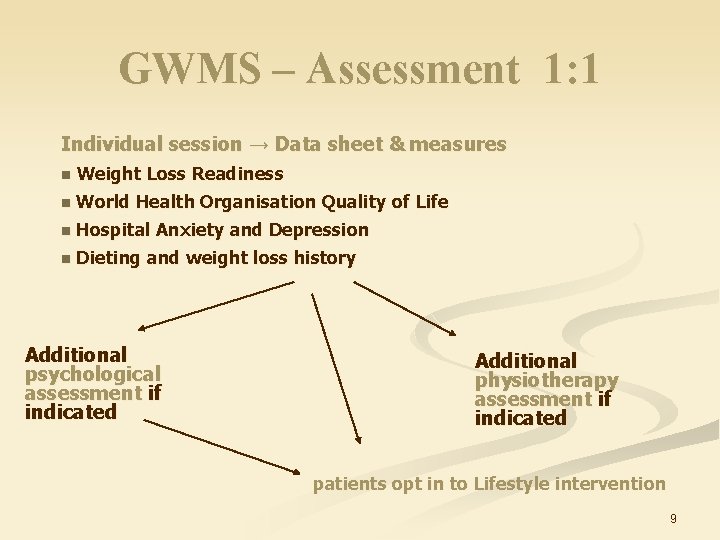
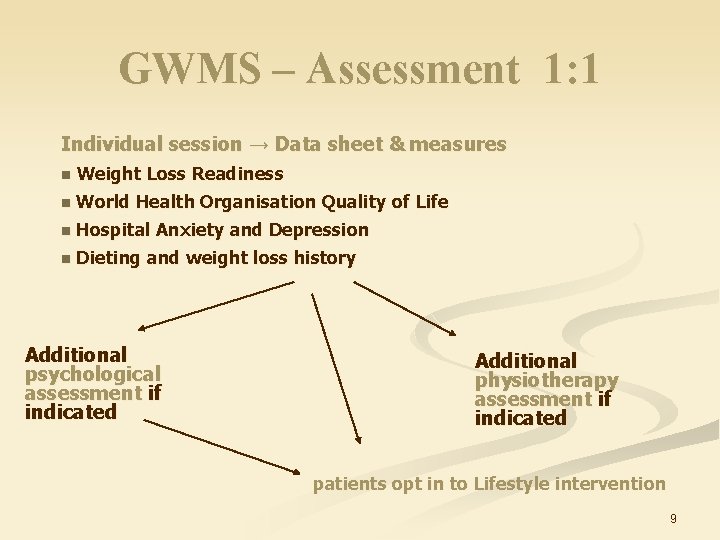
GWMS – Assessment 1: 1 Individual session → Data sheet & measures n Weight Loss Readiness n World Health Organisation Quality of Life n Hospital Anxiety and Depression n Dieting and weight loss history Additional psychological assessment if indicated Additional physiotherapy assessment if indicated patients opt in to Lifestyle intervention 9
GCWMS Assessment Questionnaires 10
Points to consider Intervention is part of the assessment – health behaviour change, but not formalised goal setting. n Generic assessment – carried out by MDT. n Assessing stage of change/readiness to change. n May have never been asked some of these questions about their weight before. n Allows patients consider the severity/the impact of their weight on their QOL. n 11
Points to consider cont. A lot of questions in questionnaire, some very personal – can bring up a lot of emotions. n Clinicians need to be skilled in dealing with emotional patients – frustrated/angry/depressed about their weight. n Patients previous weight loss attempts - their beliefs based on their experiences. n 12
Case study examples of using GCWMS assessment in practice 13
Patient 1: Mr M, 60 yr old male. n Height = 1. 68 m, Weight = 147 kg, BMI=52 kg/m 2 n GP stated on referral “for many years we have advised him to lose weight. . ” 14
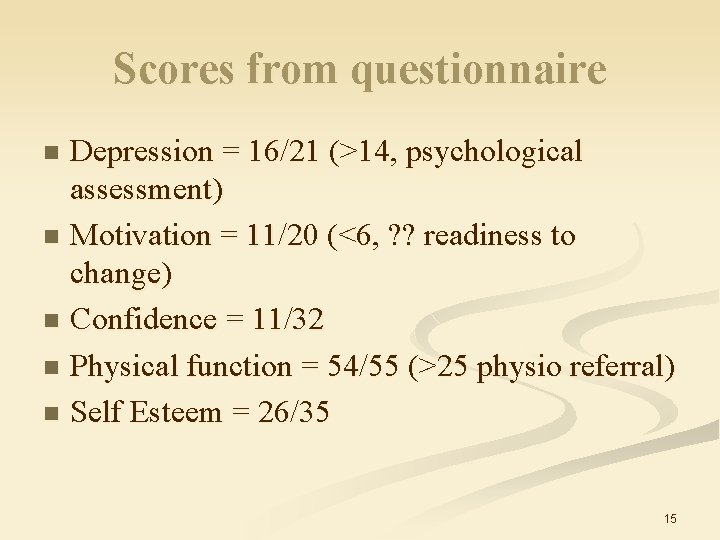
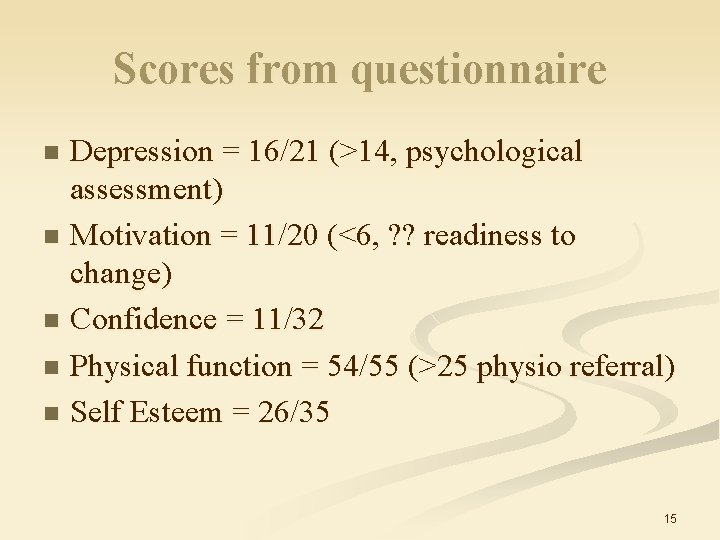
Scores from questionnaire Depression = 16/21 (>14, psychological assessment) n Motivation = 11/20 (<6, ? ? readiness to change) n Confidence = 11/32 n Physical function = 54/55 (>25 physio referral) n Self Esteem = 26/35 n 15
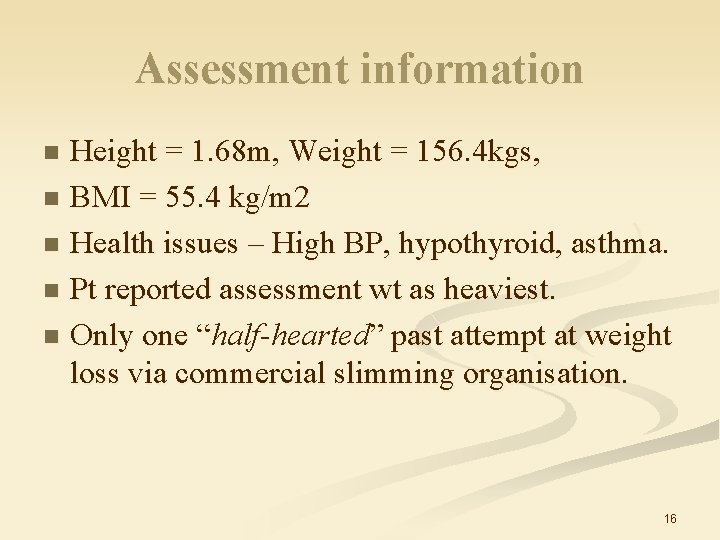
Assessment information Height = 1. 68 m, Weight = 156. 4 kgs, n BMI = 55. 4 kg/m 2 n Health issues – High BP, hypothyroid, asthma. n Pt reported assessment wt as heaviest. n Only one “half-hearted ” past attempt at weight “ loss via commercial slimming organisation. n 16
During assessment Patient presentation – body language, preconceived ideas of what would be involved n “I do this, but your going to want me to do this…” n “your going to tell me to stop having that and eat this…” n It was clear patient expected a didactic approach and to be given a diet sheet to follow. n 17
How I conducted the session Used questionnaire as a prompt. n Used reflective listening and open questions to respond to patient’s beliefs. n Used Motivational interviewing techniques eg rolling with resistance. n Aimed to illicit change talk from patient around his lifestyle. Where he identifies barriers trying to identify solutions also. n 18
Explored motivation- importance and confidence in relation to patient’s weight loss expectations. n By end of assessment he had stated changes he felt he could make and was aware which areas he needs to work on and how the service could support him with this. n He also challenged his own reported barriers “I’m just making excuses, aren’t I? . . . ” n 19
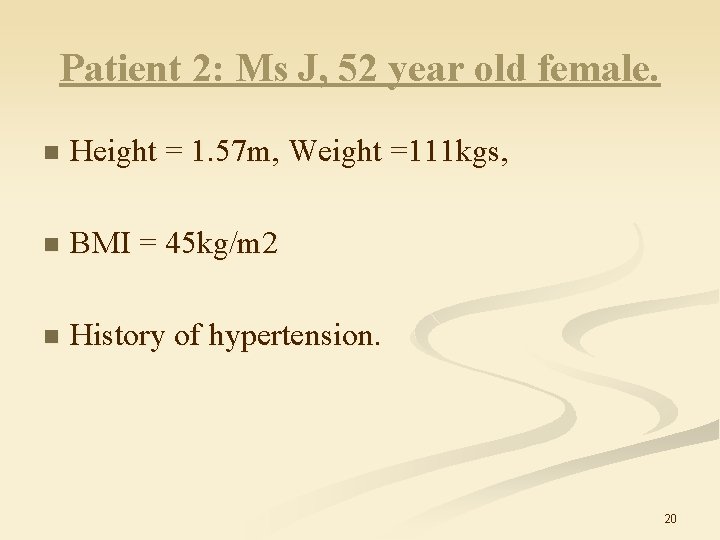
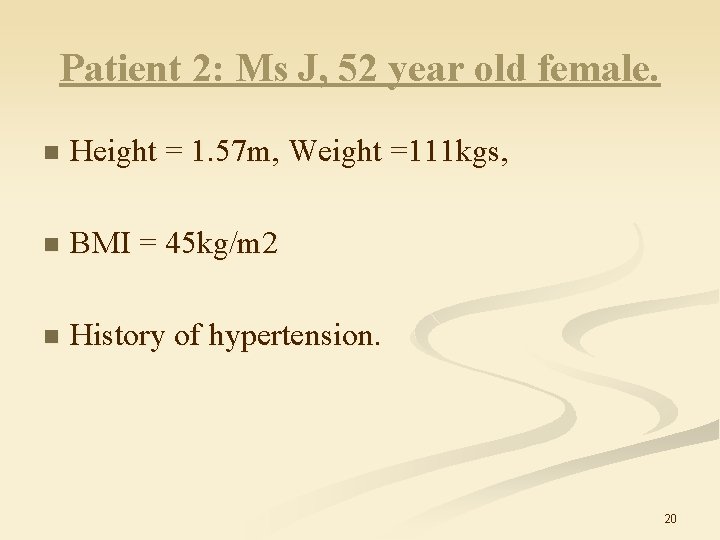
Patient 2: Ms J, 52 year old female. n Height = 1. 57 m, Weight =111 kgs, n BMI = 45 kg/m 2 n History of hypertension. 20
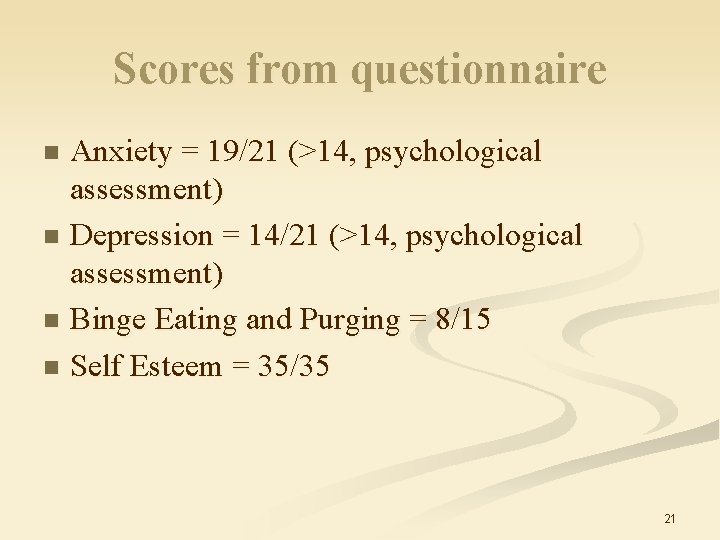
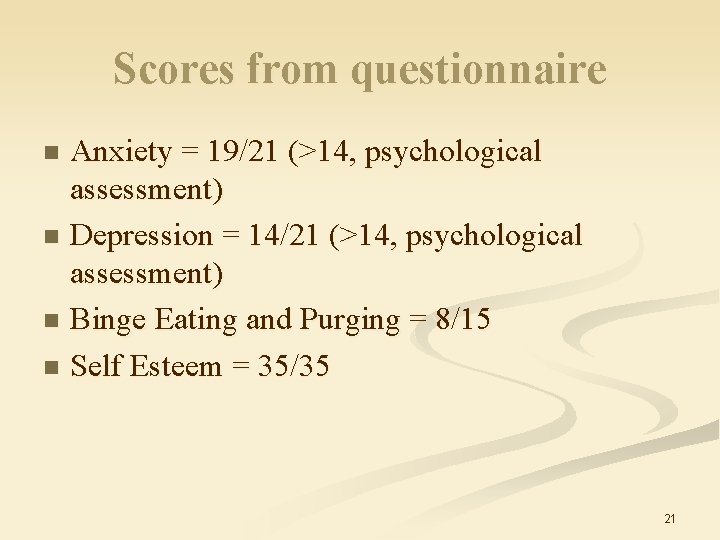
Scores from questionnaire Anxiety = 19/21 (>14, psychological assessment) n Depression = 14/21 (>14, psychological assessment) n Binge Eating and Purging = 8/15 n Self Esteem = 35/35 n 21
During assessment n Patient reported a long history of binge eating and purging behaviour. Explored further with patient. n Patient felt she would be able to control her bingeing and purging when on the programme. n However, currently was attending slimming club and had binge eaten twice that week. n Patient apprehensive about attending psychology assessment. Keen to start programme. 22
Recognising the issue – currently not under control and seeking specialist support for her weight. Patient had never disclosed this to anyone before. n Impact on her weight/self-esteem if not dealt with. n Highlighting skills of clinical psychologists and treatment options potentially available eg disordered eating group. n 23
Stressing purpose of assessment and questions asked to screen for disordered eating behaviours. n Also understanding group programme focus is on wt loss – could potentially make disordered eating worse. n Recognising that this is not my area of expertise but highlights the benefits of MDT working. n 24
 Ross shearer
Ross shearer Bandura ross and ross
Bandura ross and ross Amy shearer lingo
Amy shearer lingo Erik shearer
Erik shearer Penilaian klinis
Penilaian klinis Cas clinical assessment
Cas clinical assessment Nutrition assessment abcd
Nutrition assessment abcd Clinical assessment protocols
Clinical assessment protocols National clinical assessment service
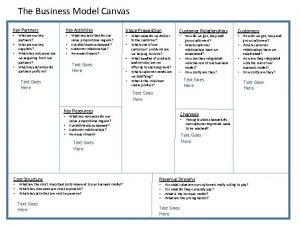
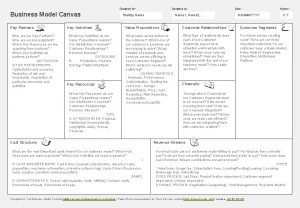
National clinical assessment service Key activities business model
Key activities business model Key partners key activities key resources
Key partners key activities key resources Clinicalkey for nurses
Clinicalkey for nurses Clinical key
Clinical key Elsevier clinical solutions
Elsevier clinical solutions Site versus situation
Site versus situation Deer population
Deer population Abiotic vs biotic factors
Abiotic vs biotic factors Aboitic environment
Aboitic environment Is a car abiotic or biotic
Is a car abiotic or biotic Site and situation factors
Site and situation factors Greatest common factor of monomials
Greatest common factor of monomials Highest common factor
Highest common factor Factors of 56
Factors of 56 Macbeth's best friend
Macbeth's best friend Wd ross theory
Wd ross theory