Fast and expensive or cheap and slow A






- Slides: 57
Fast and expensive or cheap and slow? A mathematical modelling study to explore screening for carbapenem resistant Enterobacteriaceae in UK hospitals Gwenan M Knight, Eleonora Dyakova, Siddharth Mookerjee, Frances Davies, Eimear T Brannigan, Jonathan A Otter, Alison H Holmes
Fast and expensive or cheap and slow? Gwen (modeller), Elie, Sid (ICHNT data within…) Frances, Eimear, Jon, Alison (IPC team)
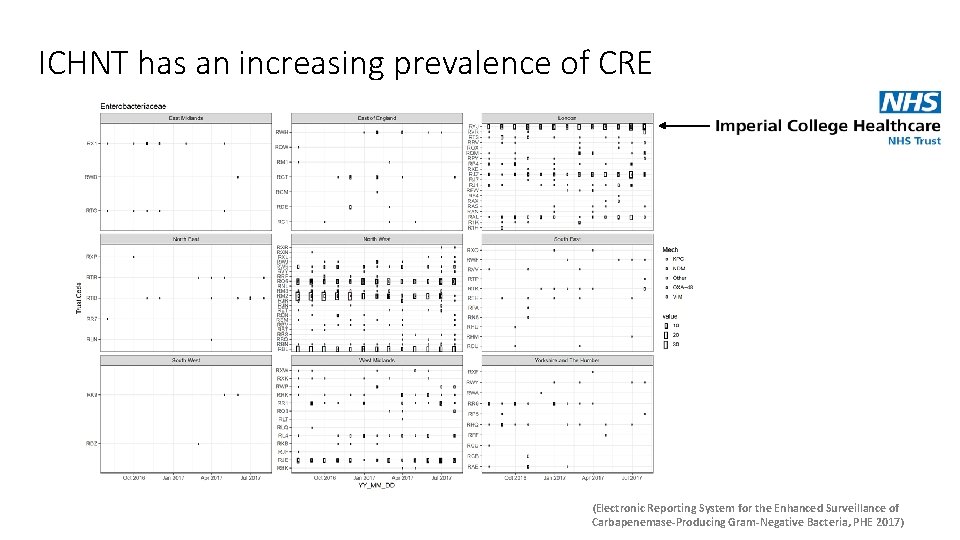
ICHNT has an increasing prevalence of CRE

Acronyms…
Acronyms… ICHNT = PHE =
Acronyms… ICHNT = PHE = CRE = carbapenem-resistant Enterobacteriaceae • Resistant by any mechanism CRE

Acronyms… ICHNT = PHE = CRE = carbapenem-resistant Enterobacteriaceae • Resistant by any mechanism CP-CRE = carbapenemase-producing CRE • Resistant to carbapenems by the production of carbapenemases CRE CP-CRE
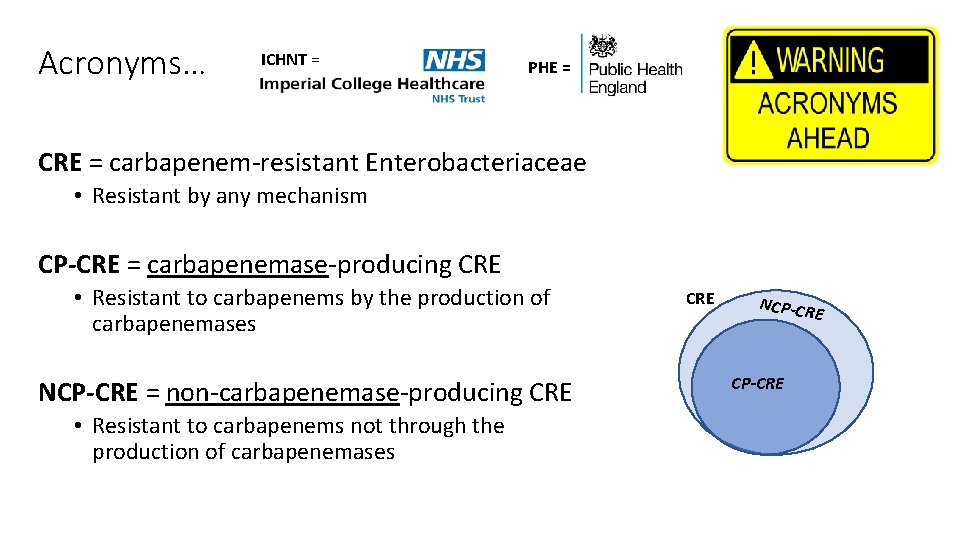
Acronyms… ICHNT = PHE = CRE = carbapenem-resistant Enterobacteriaceae • Resistant by any mechanism CP-CRE = carbapenemase-producing CRE • Resistant to carbapenems by the production of carbapenemases NCP-CRE = non-carbapenemase-producing CRE • Resistant to carbapenems not through the production of carbapenemases CRE NCP-CR E CP-CRE
How can we tackle CP-CRE?
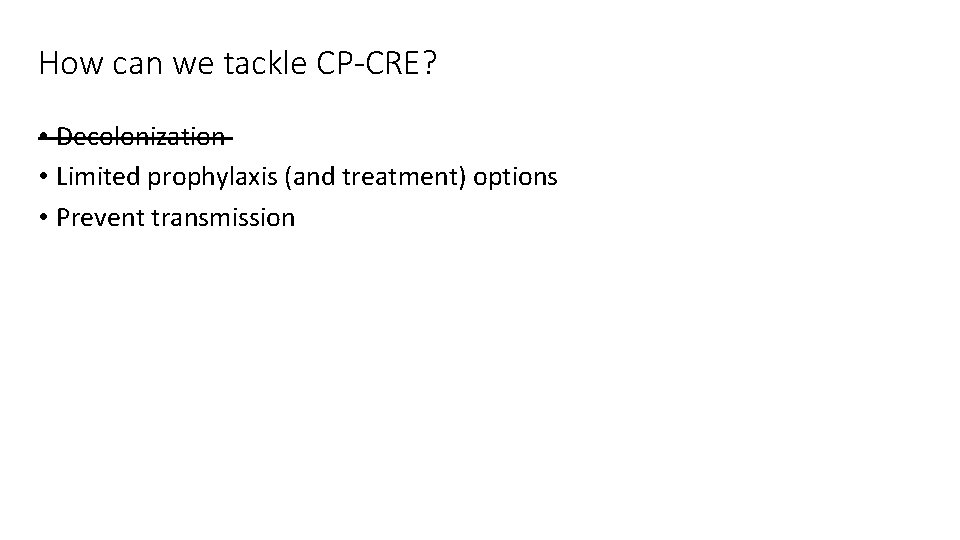
How can we tackle CP-CRE? • Decolonization • Limited prophylaxis (and treatment) options • Prevent transmission
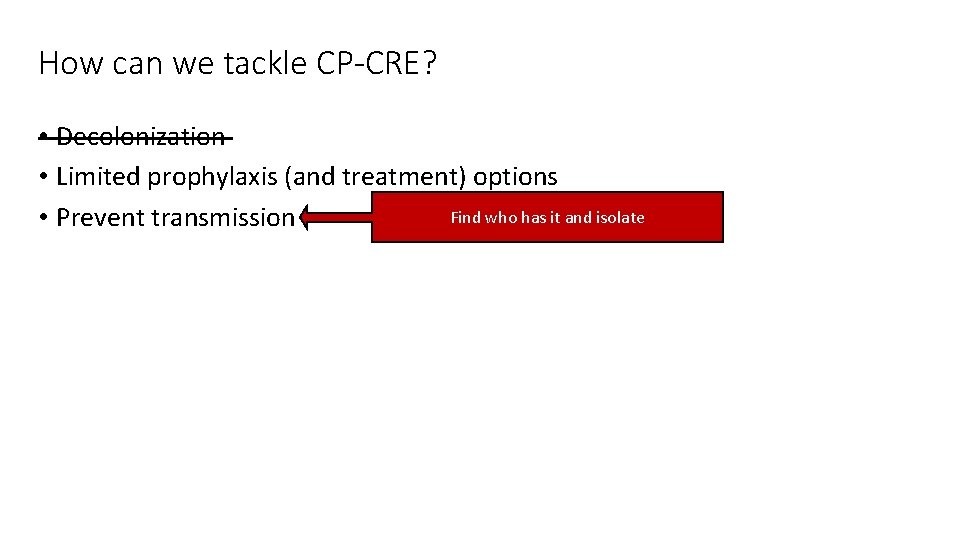
How can we tackle CP-CRE? • Decolonization • Limited prophylaxis (and treatment) options Find who has it and isolate • Prevent transmission
How can we tackle CP-CRE? • Decolonization • Limited prophylaxis (and treatment) options Find who has it and isolate • Prevent transmission ICHNT = universal screening for high-risk specialties since 2015 BUT various screening methods available
How can we tackle CP-CRE? • Decolonization • Limited prophylaxis (and treatment) options Find who has it and isolate • Prevent transmission ICHNT = universal screening for high-risk specialties since 2015 BUT various screening methods available QN: What algorithm should ICHNT use for CP-CRE screening?

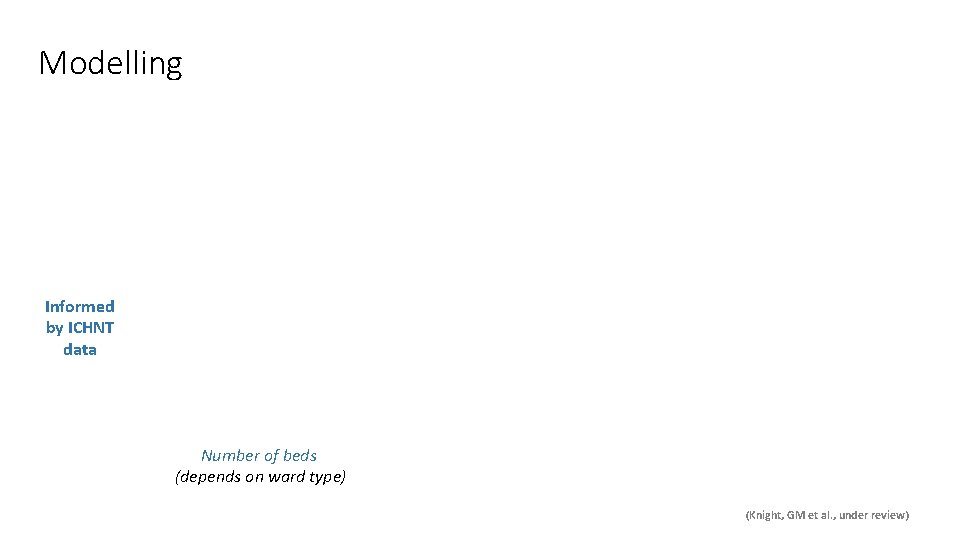
Modelling

Modelling Informed by ICHNT data
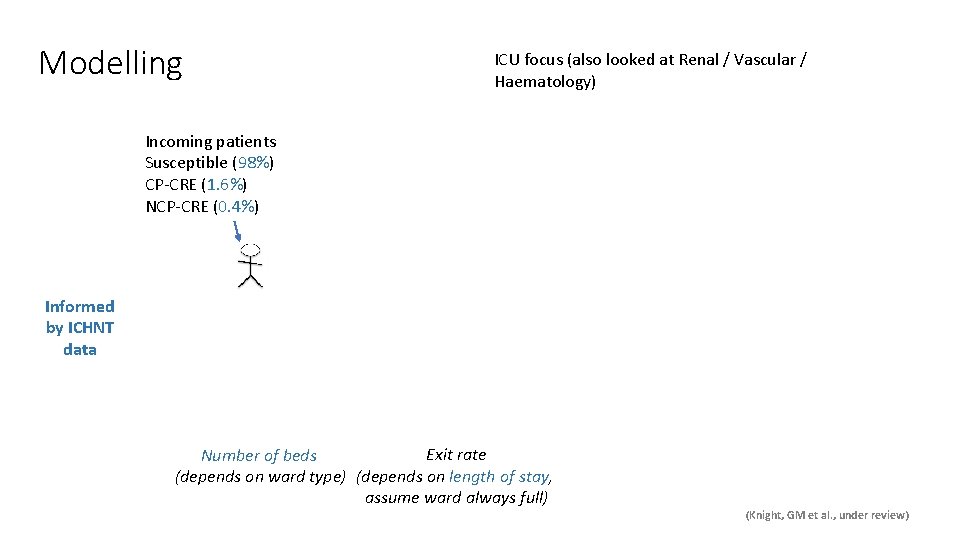
Modelling Informed by ICHNT data Exit rate Number of beds (depends on ward type) (depends on length of stay, assume ward always full) (Knight, GM et al. , under review)
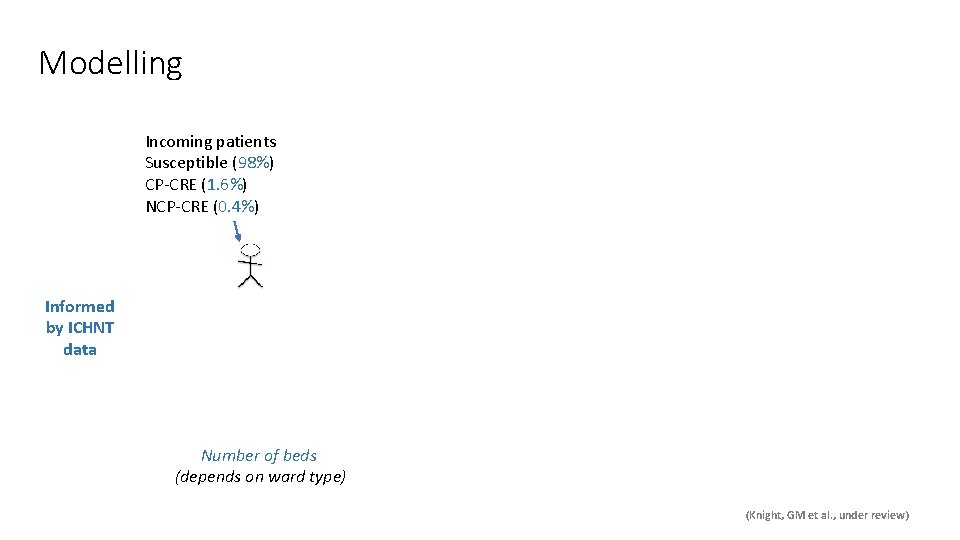
Modelling Incoming patients Susceptible (98%) CP-CRE (1. 6%) NCP-CRE (0. 4%) Informed by ICHNT data Exit rate Number of beds (depends on ward type) (depends on length of stay, assume ward always full) (Knight, GM et al. , under review)
Modelling Incoming patients Susceptible (98%) CP-CRE (1. 6%) NCP-CRE (0. 4%) Informed by ICHNT data Exit rate Number of beds (depends on ward type) (depends on length of stay, assume ward always full) (Knight, GM et al. , under review)
Modelling Incoming patients Susceptible (98%) CP-CRE (1. 6%) NCP-CRE (0. 4%) Informed by ICHNT data Exit rate Number of beds (depends on ward type) (depends on length of stay, assume ward always full) (Knight, GM et al. , under review)
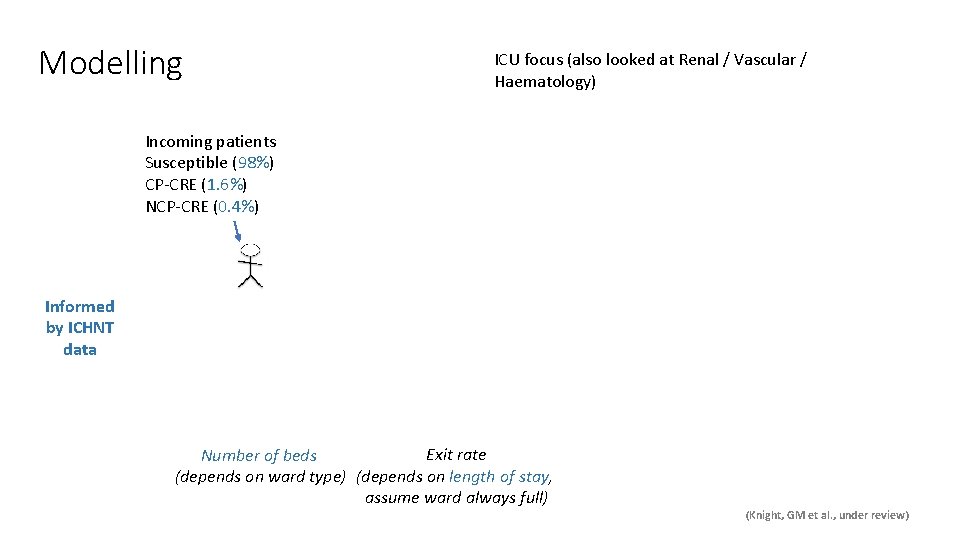
Modelling ICU focus (also looked at Renal / Vascular / Haematology) Incoming patients Susceptible (98%) CP-CRE (1. 6%) NCP-CRE (0. 4%) Informed by ICHNT data Exit rate Number of beds (depends on ward type) (depends on length of stay, assume ward always full) (Knight, GM et al. , under review)
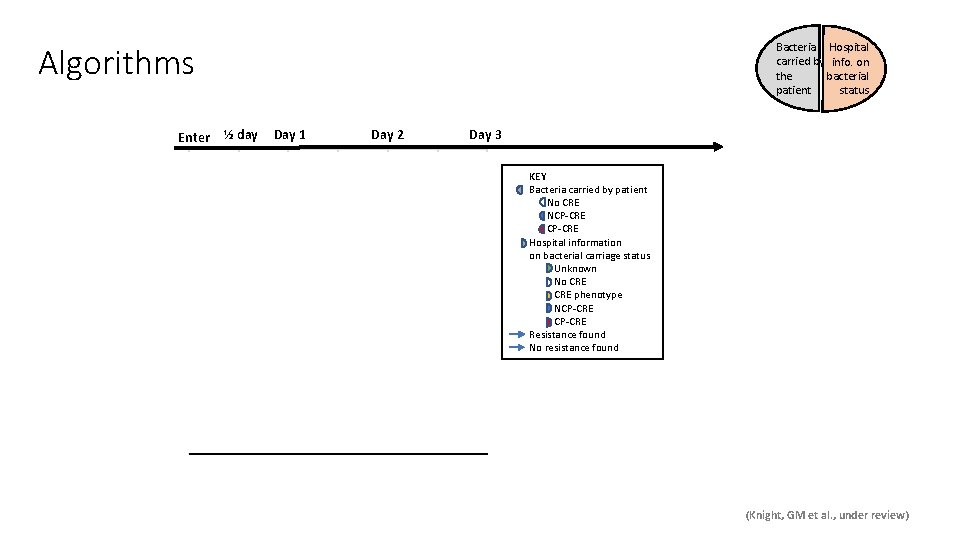
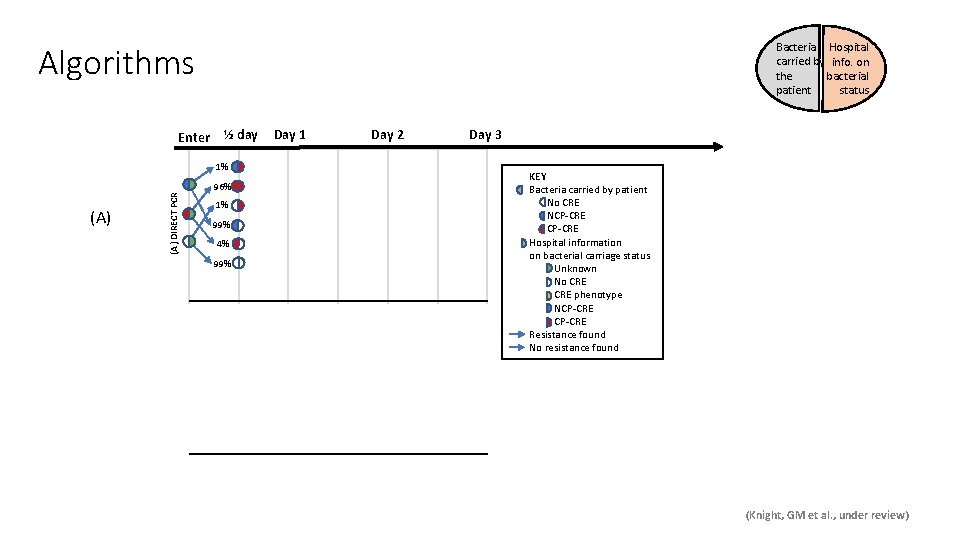
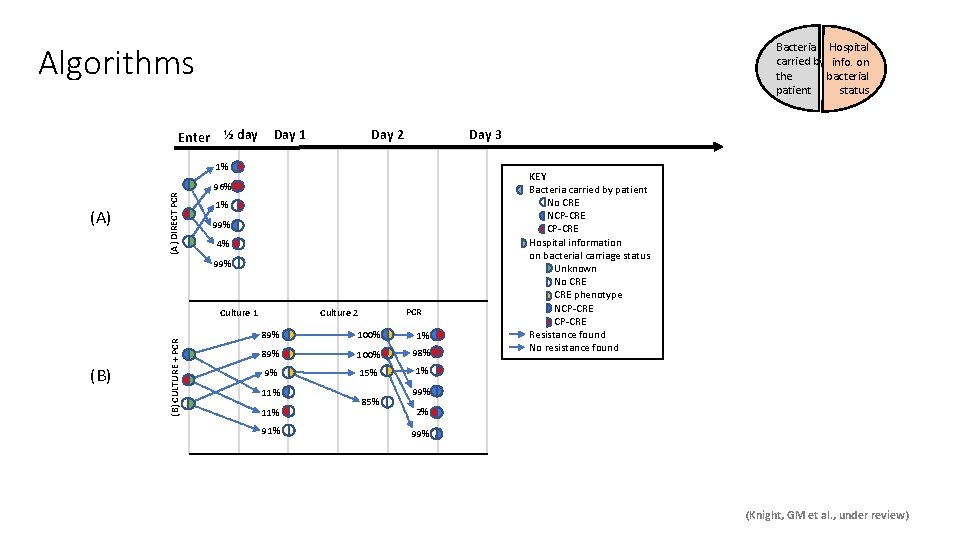
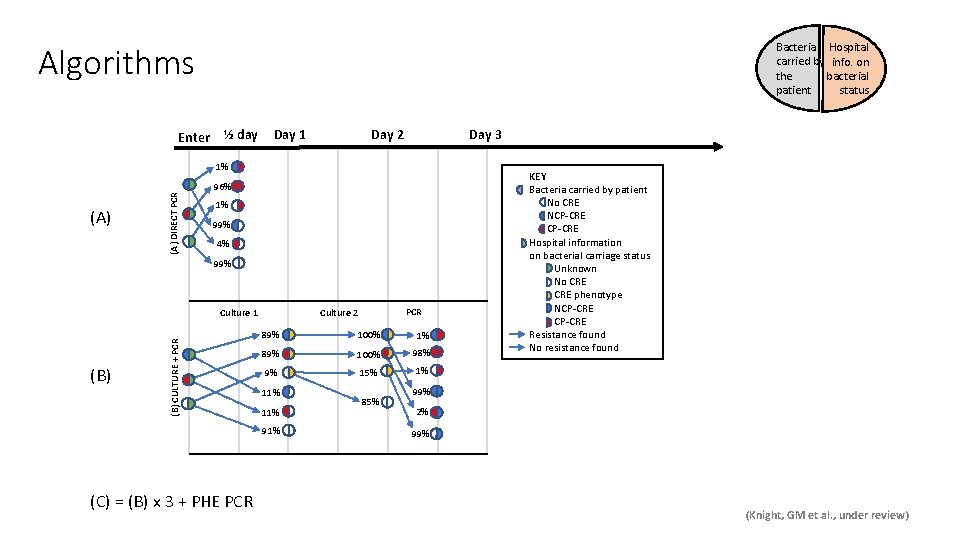
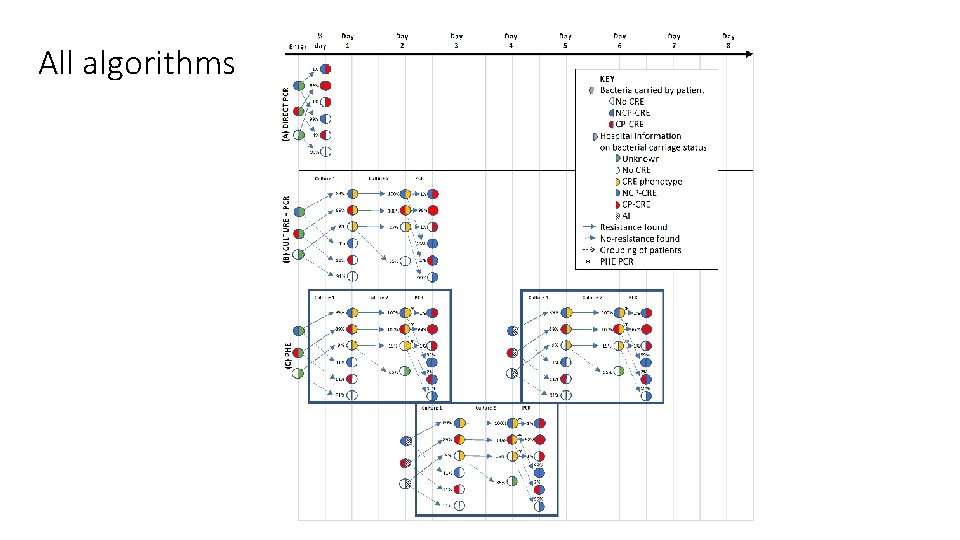
Algorithms Enter Bacteria Hospital carried by info. on the bacterial patient status ½ day Day 1 Day 2 Day 3 (A) DIRECT PCR 1% 96% 1% 99% 4% 99% (B) CULTURE + PCR (B) PCR Culture 2 Culture 1 89% 100% 1% 89% 100% 98% 9% 15% 1% 11% 91% 85% KEY Bacteria carried by patient No CRE NCP-CRE Hospital information on bacterial carriage status Unknown No CRE phenotype NCP-CRE Resistance found No resistance found 99% 2% 99% (Knight, GM et al. , under review)
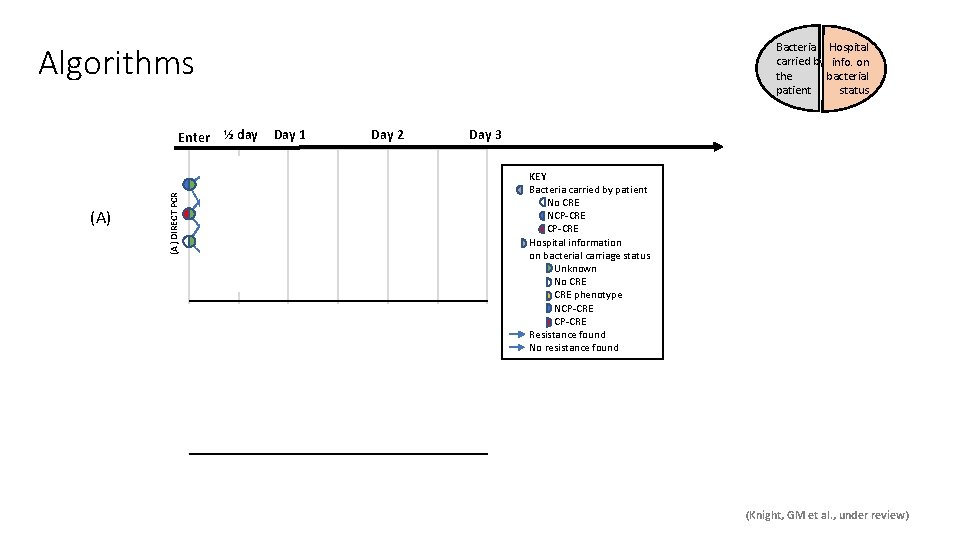
Algorithms Enter Bacteria Hospital carried by info. on the bacterial patient status ½ day Day 1 Day 2 Day 3 (A) DIRECT PCR 1% 96% 1% 99% 4% 99% (B) CULTURE + PCR (B) PCR Culture 2 Culture 1 89% 100% 1% 89% 100% 98% 9% 15% 1% 11% 91% 85% KEY Bacteria carried by patient No CRE NCP-CRE Hospital information on bacterial carriage status Unknown No CRE phenotype NCP-CRE Resistance found No resistance found 99% 2% 99% (Knight, GM et al. , under review)
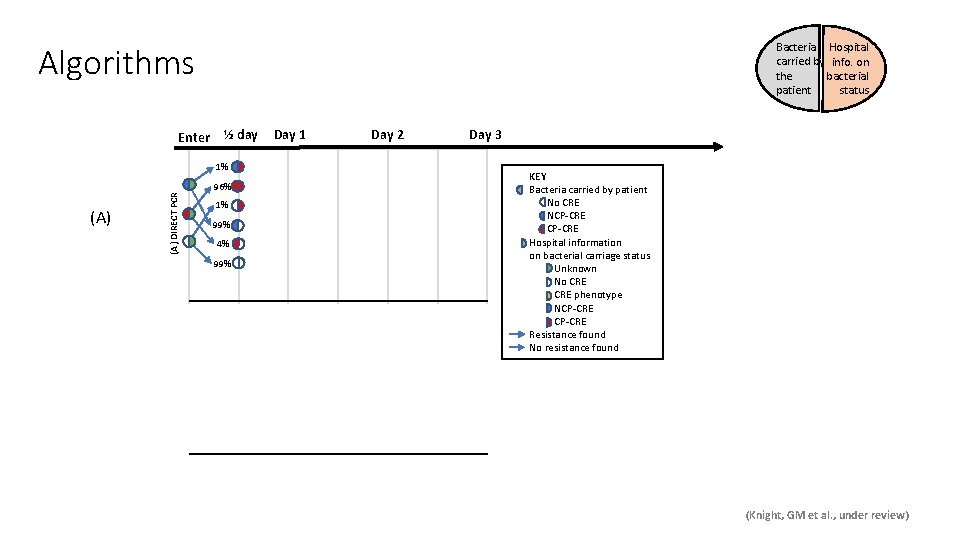
Algorithms Enter Bacteria Hospital carried by info. on the bacterial patient status ½ day Day 1 Day 2 Day 3 (A) DIRECT PCR 1% 96% 1% 99% 4% 99% (B) CULTURE + PCR (B) PCR Culture 2 Culture 1 89% 100% 1% 89% 100% 98% 9% 15% 1% 11% 91% 85% KEY Bacteria carried by patient No CRE NCP-CRE Hospital information on bacterial carriage status Unknown No CRE phenotype NCP-CRE Resistance found No resistance found 99% 2% 99% (Knight, GM et al. , under review)
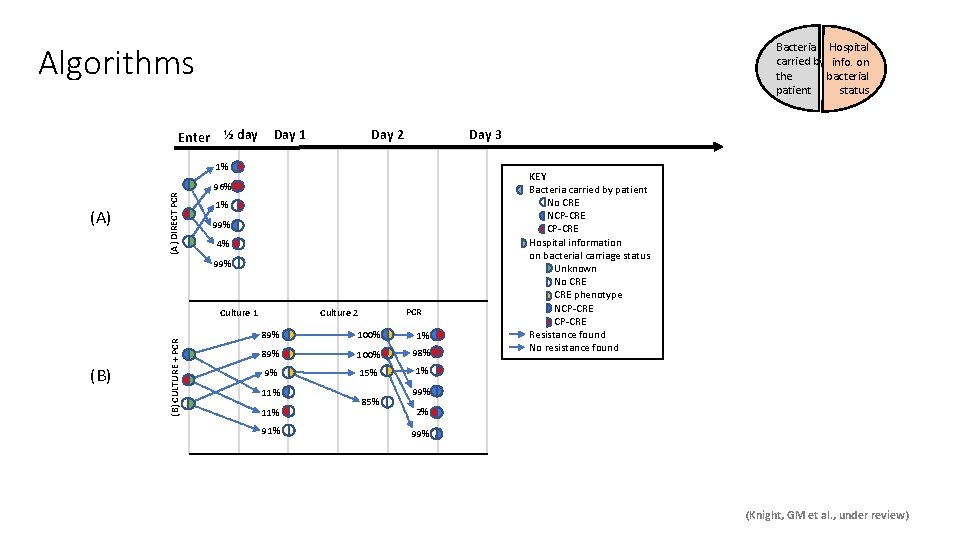
Algorithms Enter Bacteria Hospital carried by info. on the bacterial patient status ½ day Day 1 Day 2 Day 3 (A) DIRECT PCR 1% 96% 1% 99% 4% 99% (B) CULTURE + PCR (B) PCR Culture 2 Culture 1 89% 100% 1% 89% 100% 98% 9% 15% 1% 11% 91% 85% KEY Bacteria carried by patient No CRE NCP-CRE Hospital information on bacterial carriage status Unknown No CRE phenotype NCP-CRE Resistance found No resistance found 99% 2% 99% (Knight, GM et al. , under review)
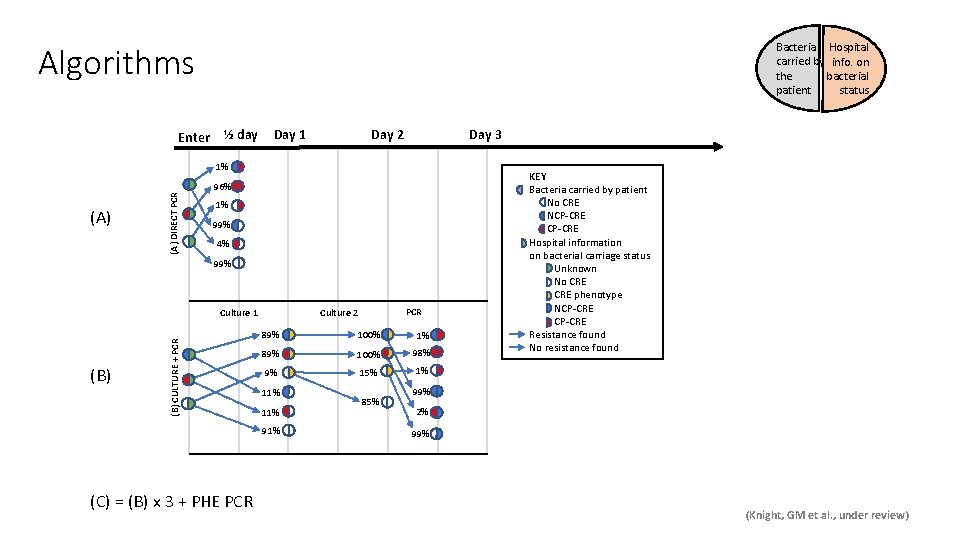
Algorithms Enter Bacteria Hospital carried by info. on the bacterial patient status ½ day Day 1 Day 2 Day 3 (A) DIRECT PCR 1% 96% 1% 99% 4% 99% (B) CULTURE + PCR (B) 89% 100% 1% 89% 100% 98% 9% 15% 1% 11% 91% (C) = (B) x 3 + PHE PCR Culture 2 Culture 1 85% KEY Bacteria carried by patient No CRE NCP-CRE Hospital information on bacterial carriage status Unknown No CRE phenotype NCP-CRE Resistance found No resistance found 99% 2% 99% (Knight, GM et al. , under review)
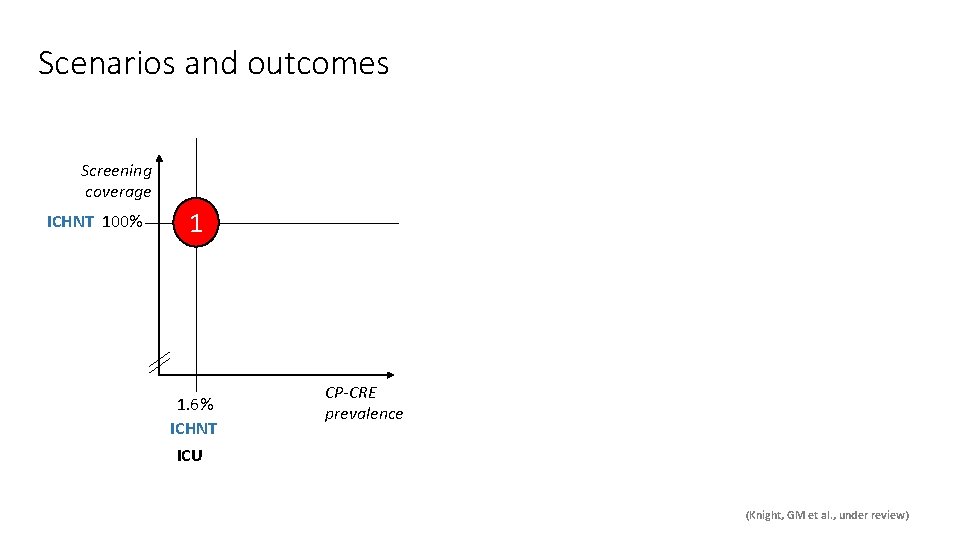
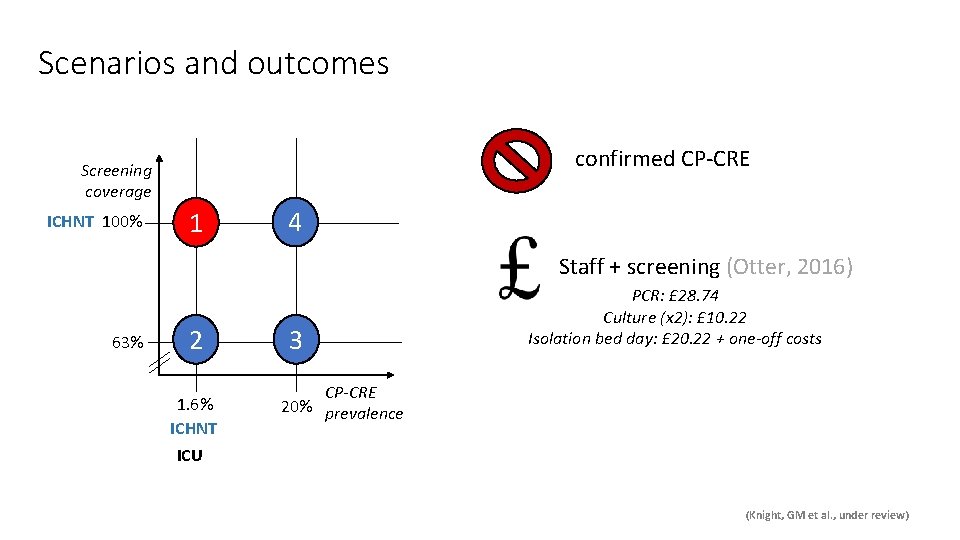
Scenarios and outcomes Screening coverage CP-CRE prevalence (Knight, GM et al. , under review)
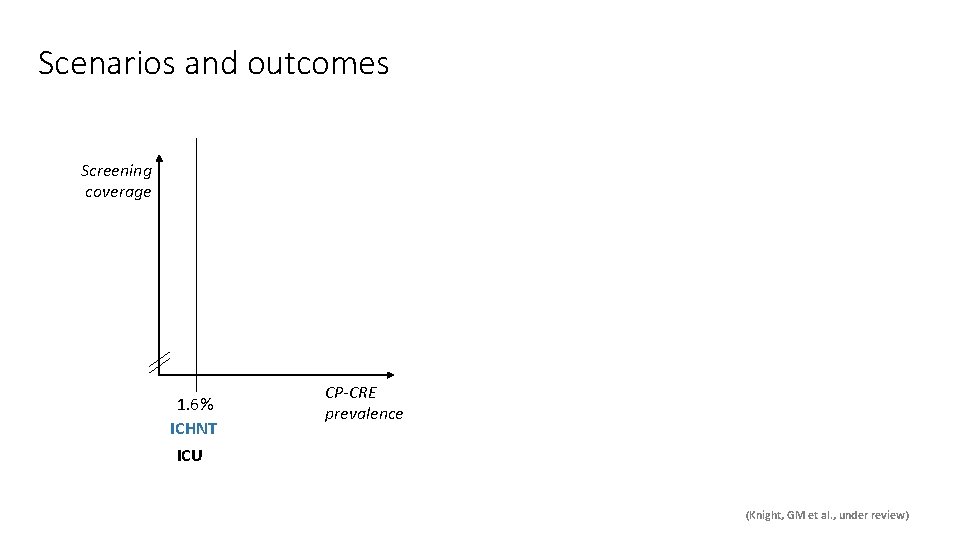
Scenarios and outcomes Screening coverage 1. 6% ICHNT CP-CRE prevalence ICU (Knight, GM et al. , under review)
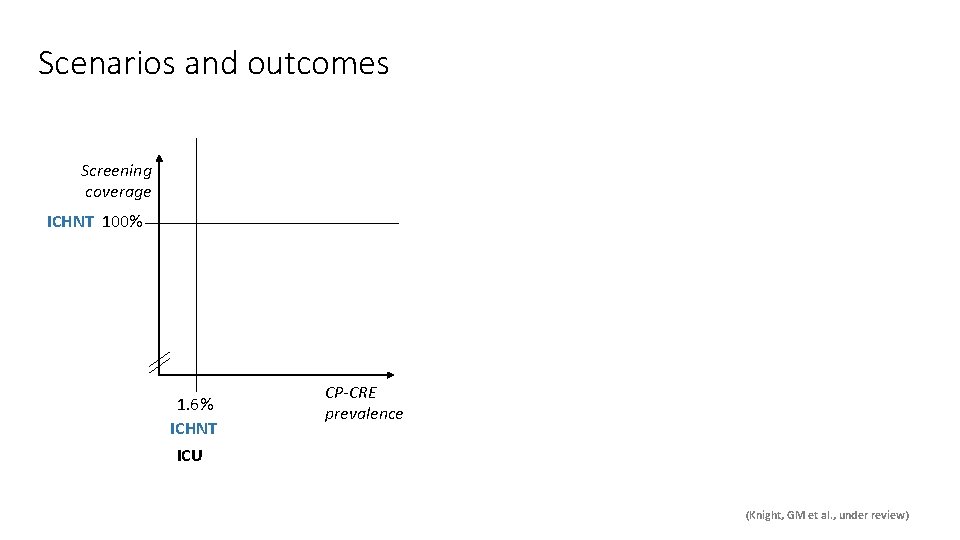
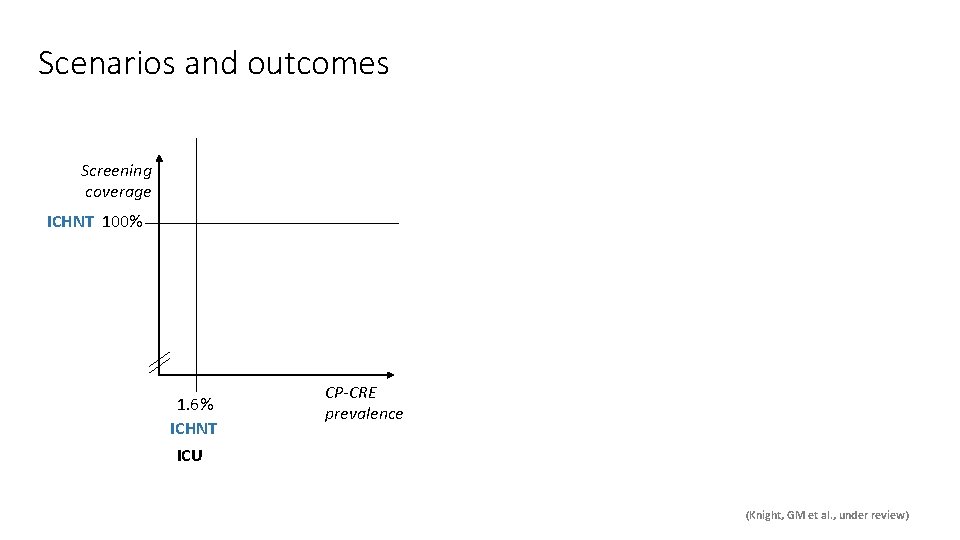
Scenarios and outcomes Screening coverage ICHNT 100% 1. 6% ICHNT CP-CRE prevalence ICU (Knight, GM et al. , under review)
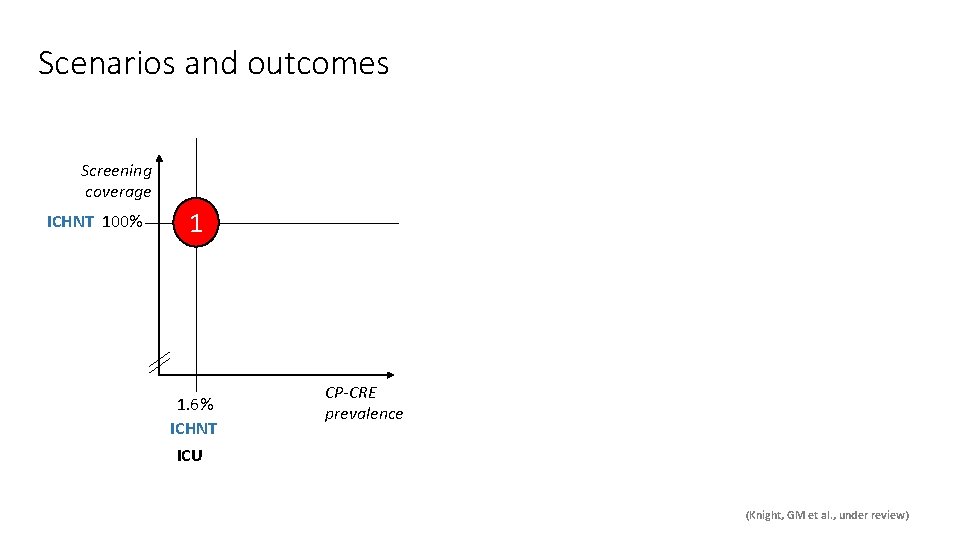
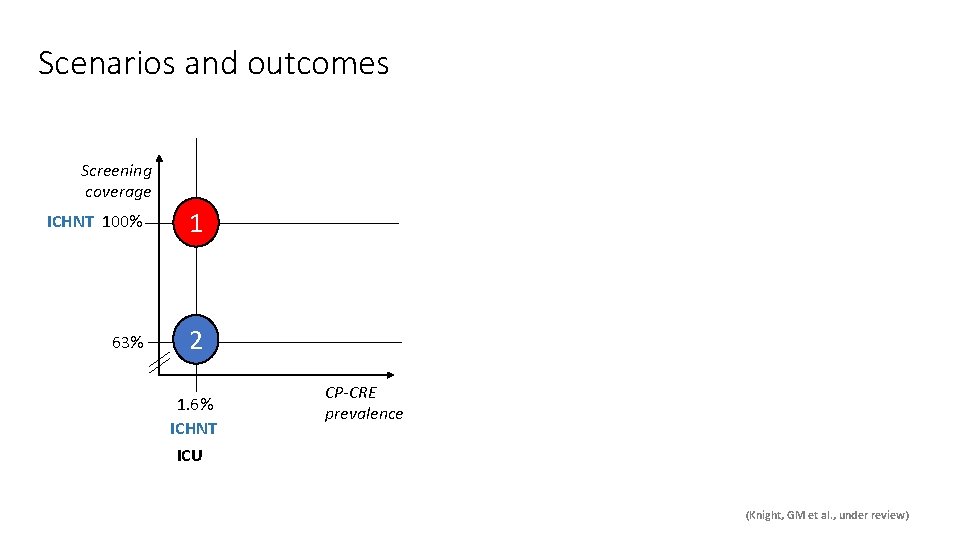
Scenarios and outcomes Screening coverage ICHNT 100% 1 1. 6% ICHNT CP-CRE prevalence ICU (Knight, GM et al. , under review)
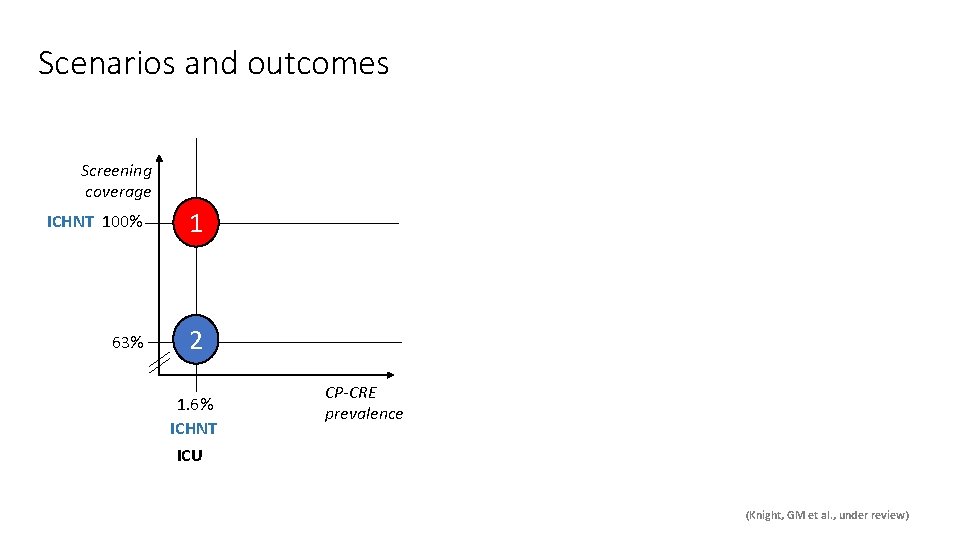
Scenarios and outcomes Screening coverage ICHNT 100% 1 63% 2 1. 6% ICHNT CP-CRE prevalence ICU (Knight, GM et al. , under review)
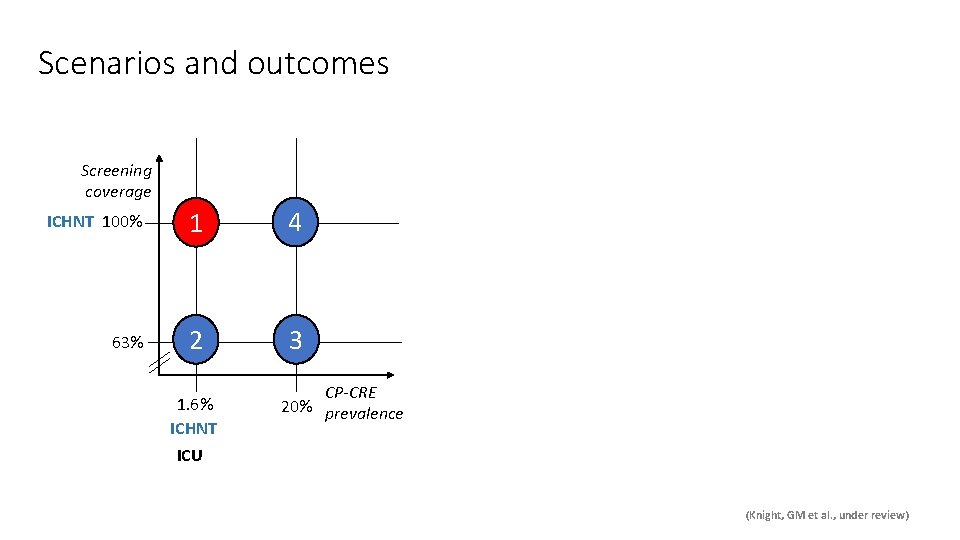
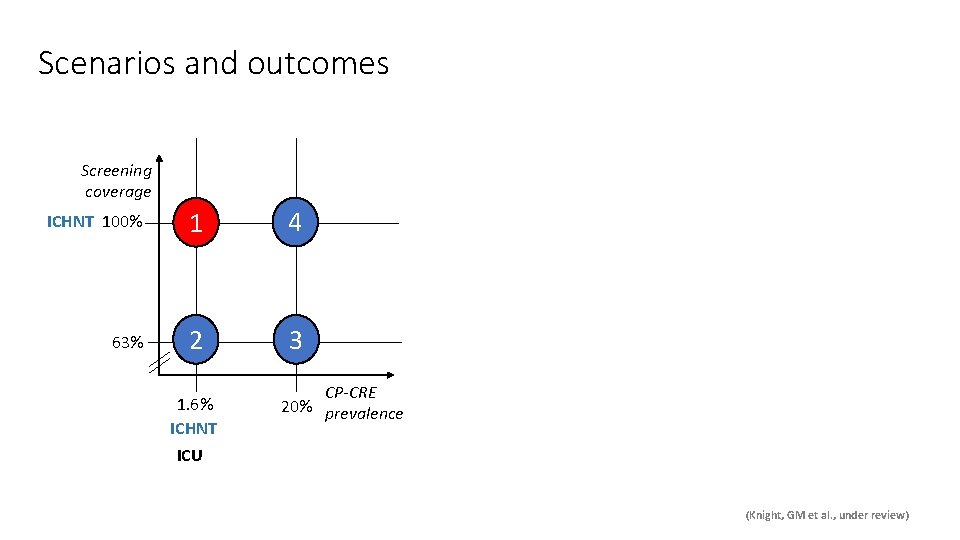
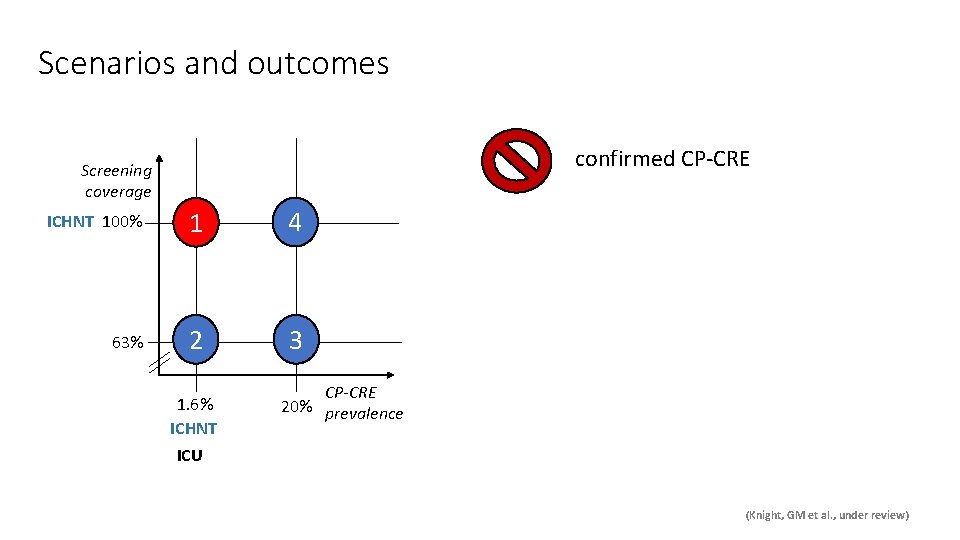
Scenarios and outcomes Screening coverage ICHNT 100% 1 4 63% 2 3 1. 6% ICHNT CP-CRE 20% prevalence ICU (Knight, GM et al. , under review)
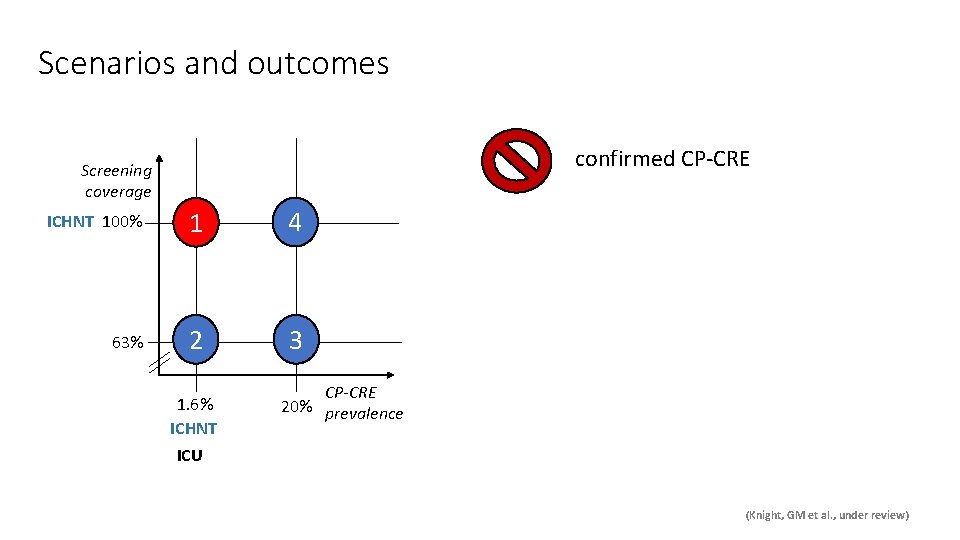
Scenarios and outcomes confirmed CP-CRE Screening coverage ICHNT 100% 1 4 63% 2 3 1. 6% ICHNT CP-CRE 20% prevalence ICU (Knight, GM et al. , under review)
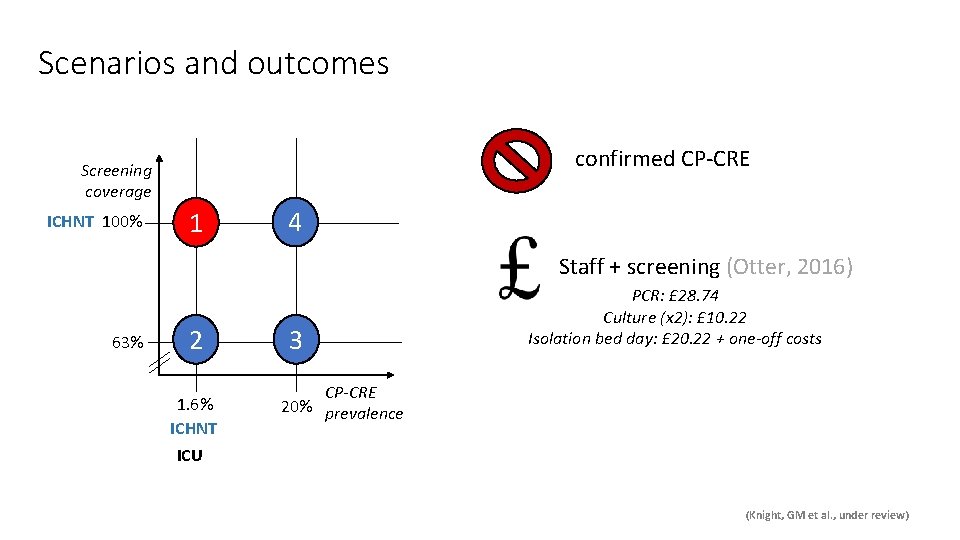
Scenarios and outcomes confirmed CP-CRE Screening coverage ICHNT 100% 1 4 Staff + screening (Otter, 2016) 63% 2 1. 6% ICHNT 3 PCR: £ 28. 74 Culture (x 2): £ 10. 22 Isolation bed day: £ 20. 22 + one-off costs CP-CRE 20% prevalence ICU (Knight, GM et al. , under review)

Scenarios and outcomes confirmed CP-CRE Screening coverage ICHNT 100% 1 4 Staff + screening (Otter, 2016) 63% 2 1. 6% ICHNT ICU 3 CP-CRE 20% prevalence PCR: £ 28. 74 Culture (x 2): £ 10. 22 Isolation bed day: £ 20. 22 + one-off costs Outcomes: (1) Number of “days at risk” (2) Cost per averted risk day (Knight, GM et al. , under review)
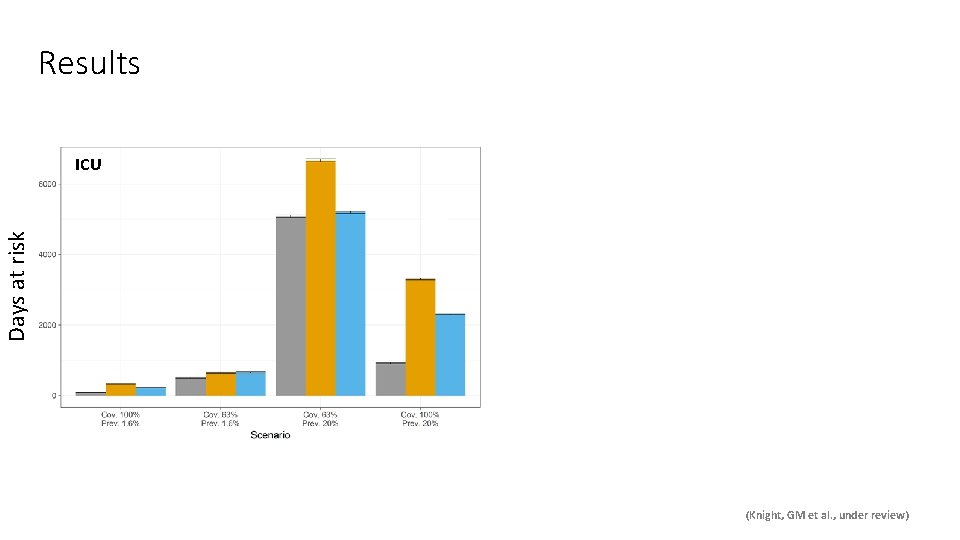
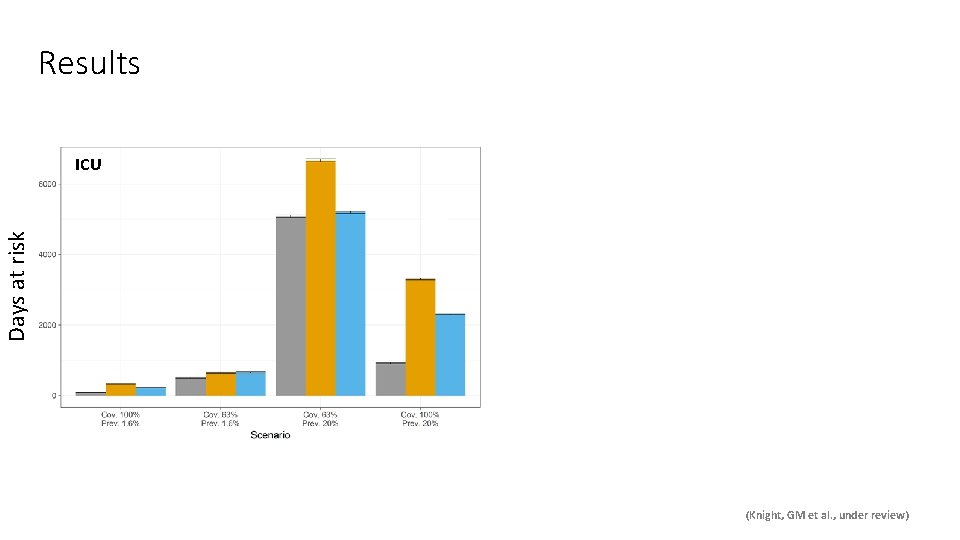
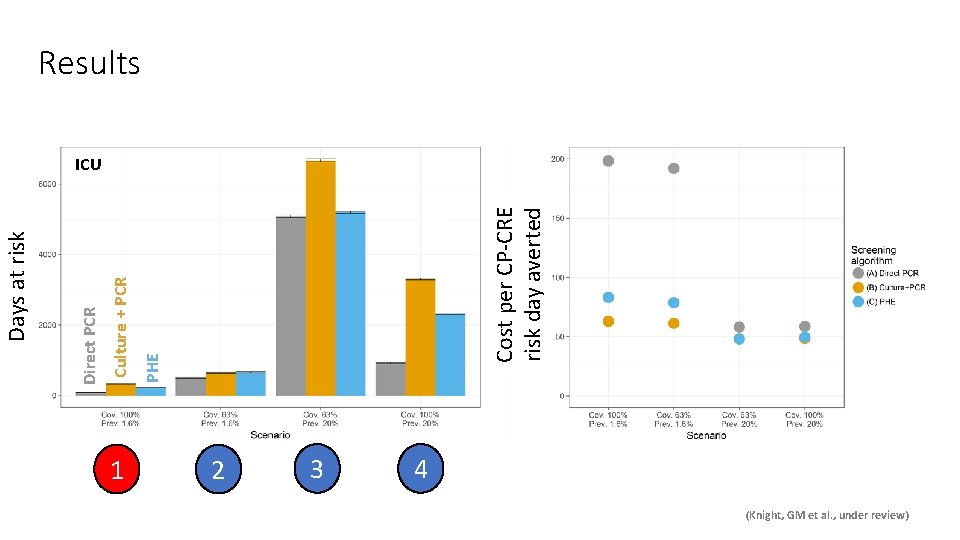
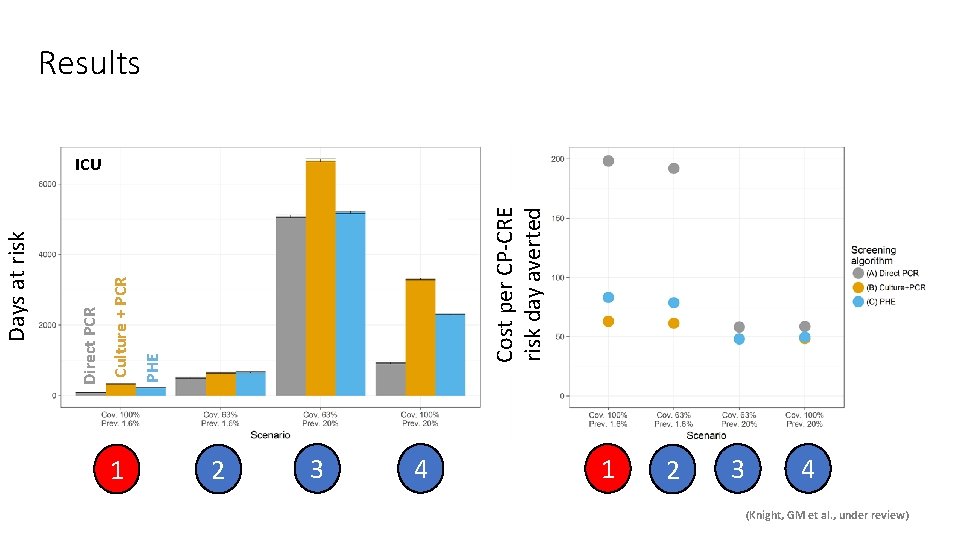
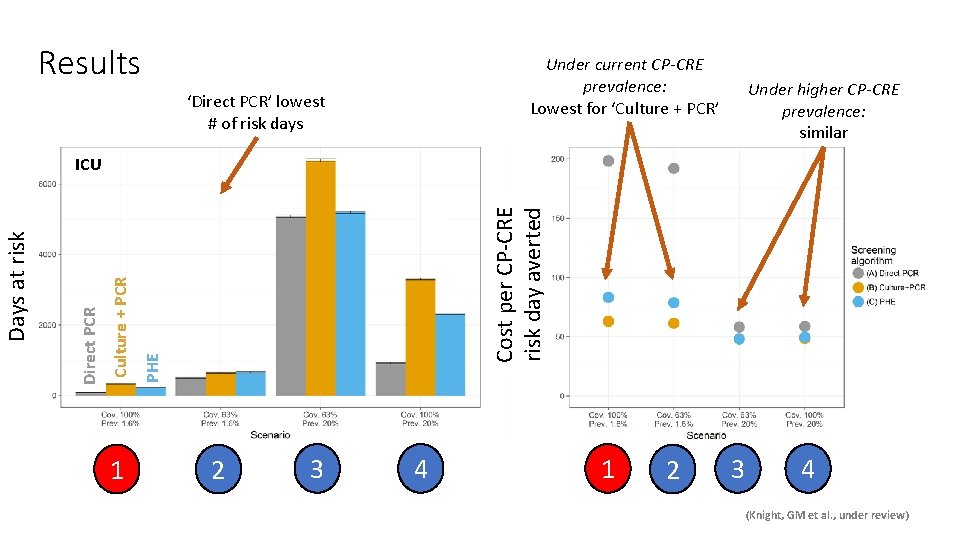
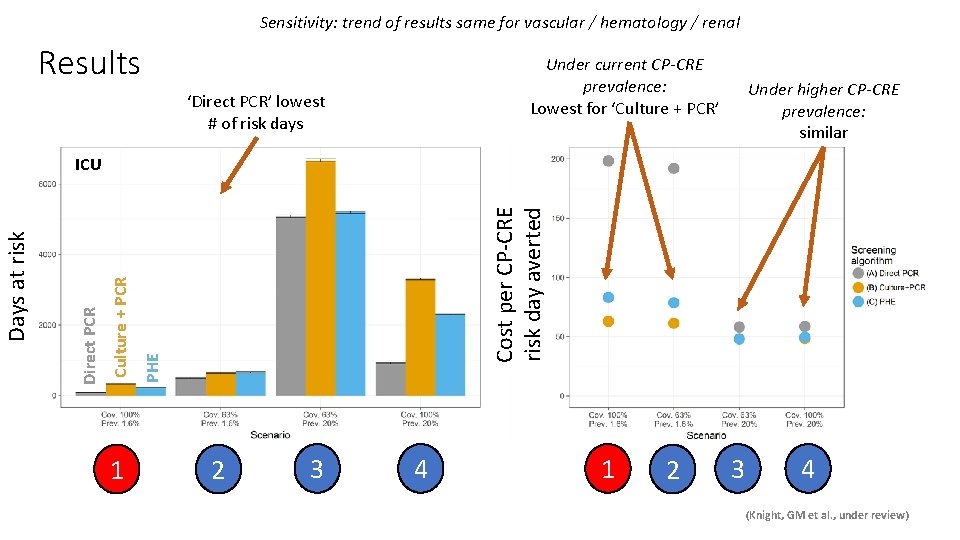
Results Days at risk ICU (Knight, GM et al. , under review)
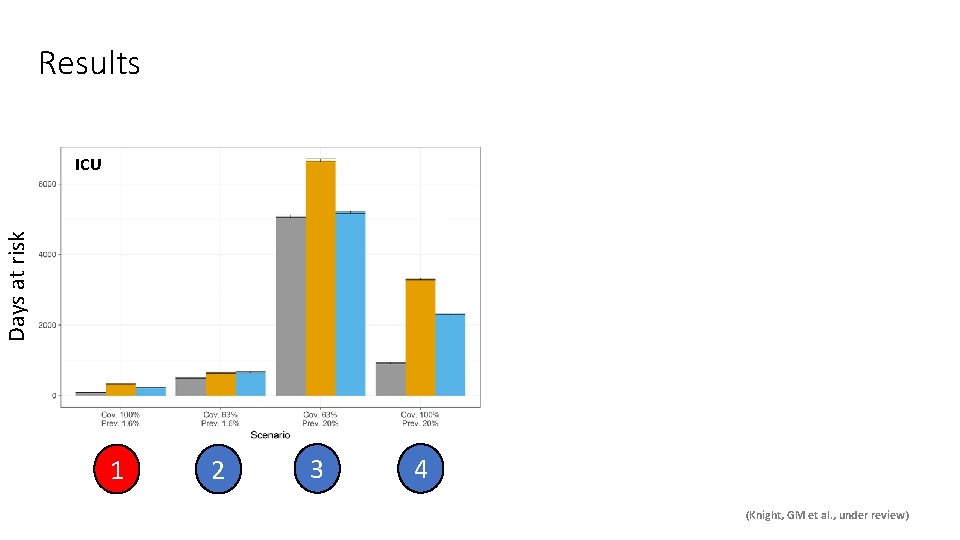
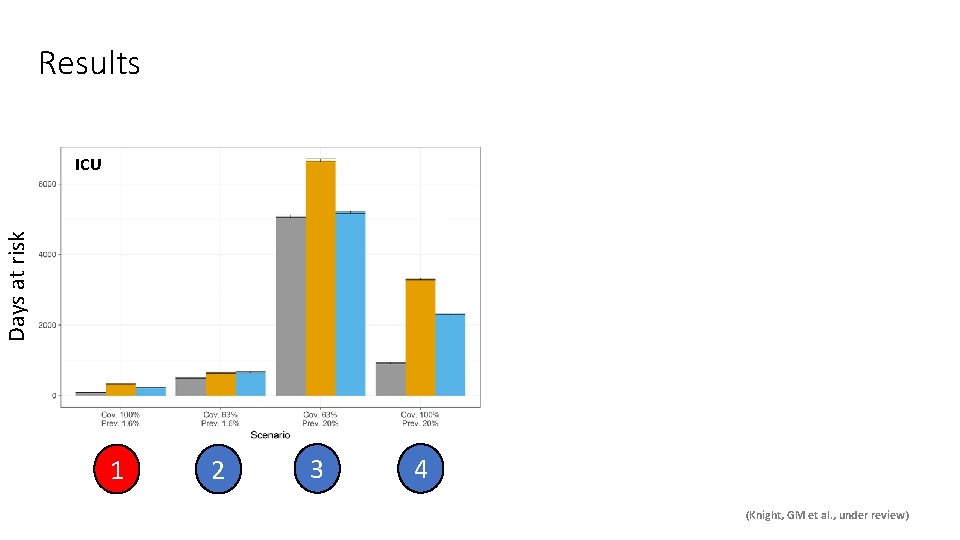
Results Days at risk ICU 1 2 3 4 (Knight, GM et al. , under review)
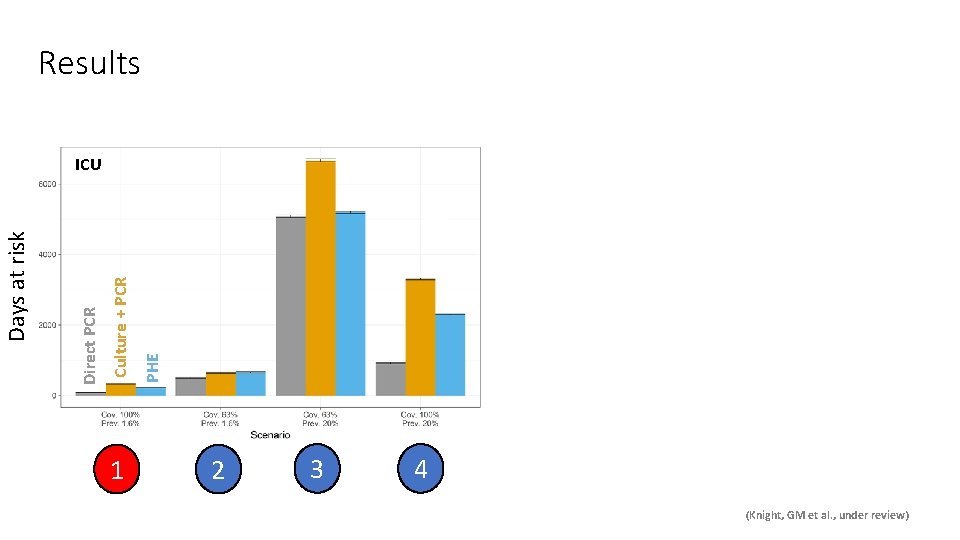
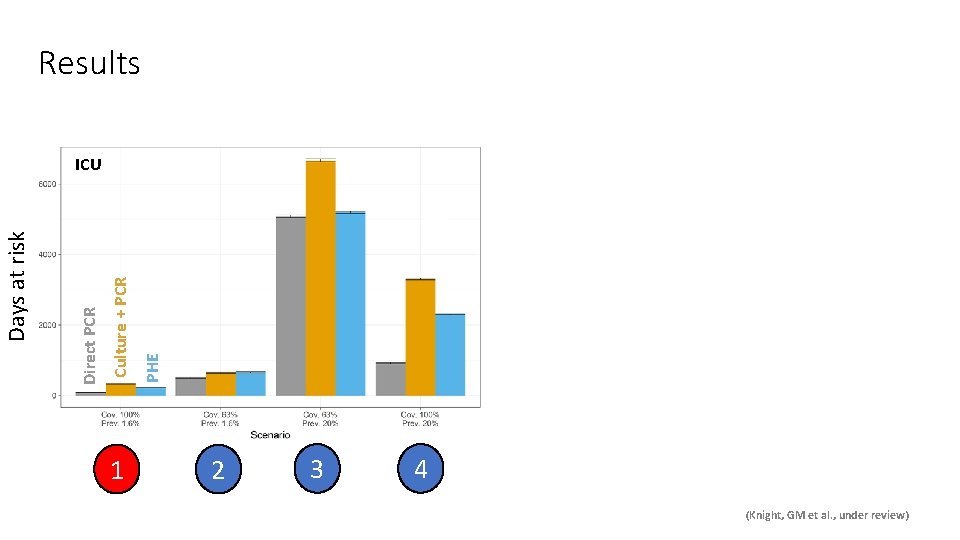
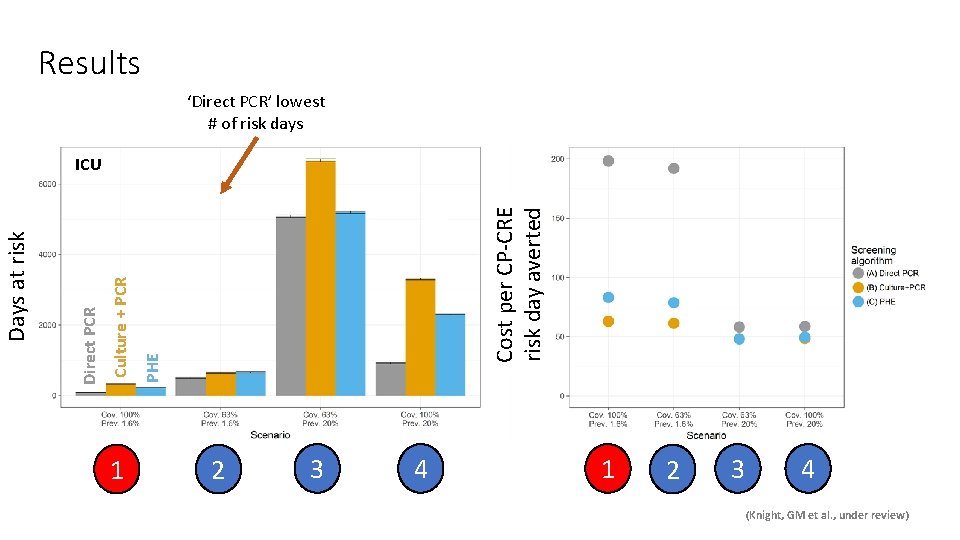
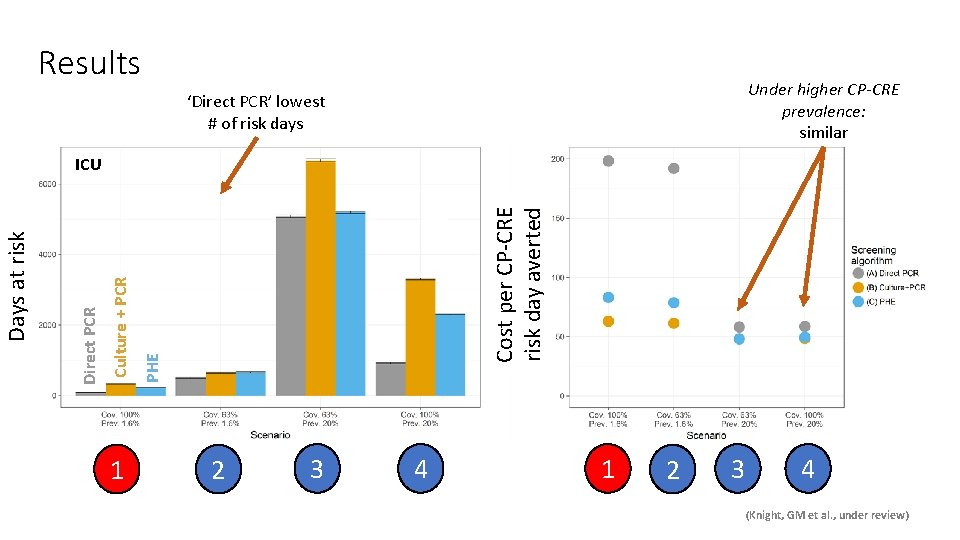
Results 1 PHE Culture + PCR Direct PCR Days at risk ICU 2 3 4 (Knight, GM et al. , under review)
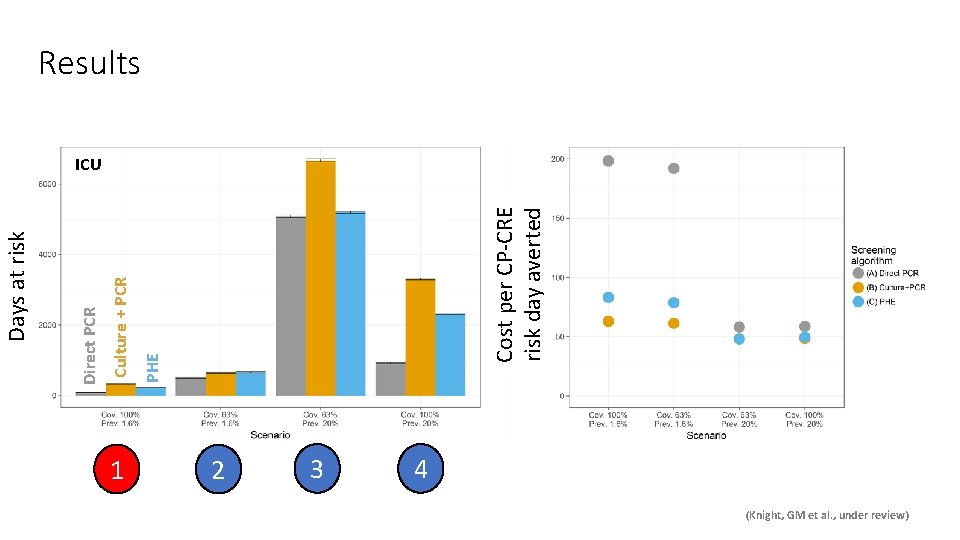
1 Cost per CP-CRE risk day averted PHE Culture + PCR Direct PCR Days at risk Results ICU 2 3 4 (Knight, GM et al. , under review)
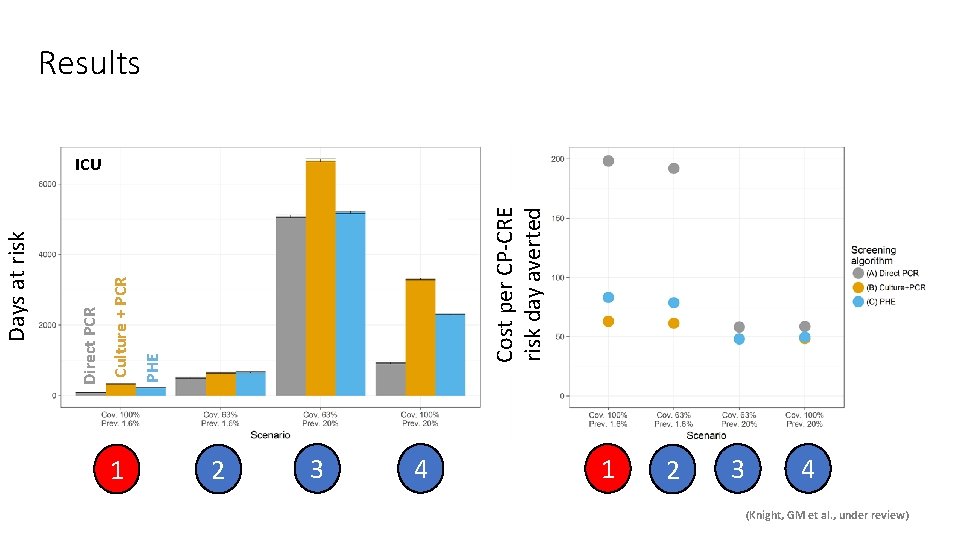
1 Cost per CP-CRE risk day averted PHE Culture + PCR Direct PCR Days at risk Results ICU 2 3 4 1 2 3 4 (Knight, GM et al. , under review)
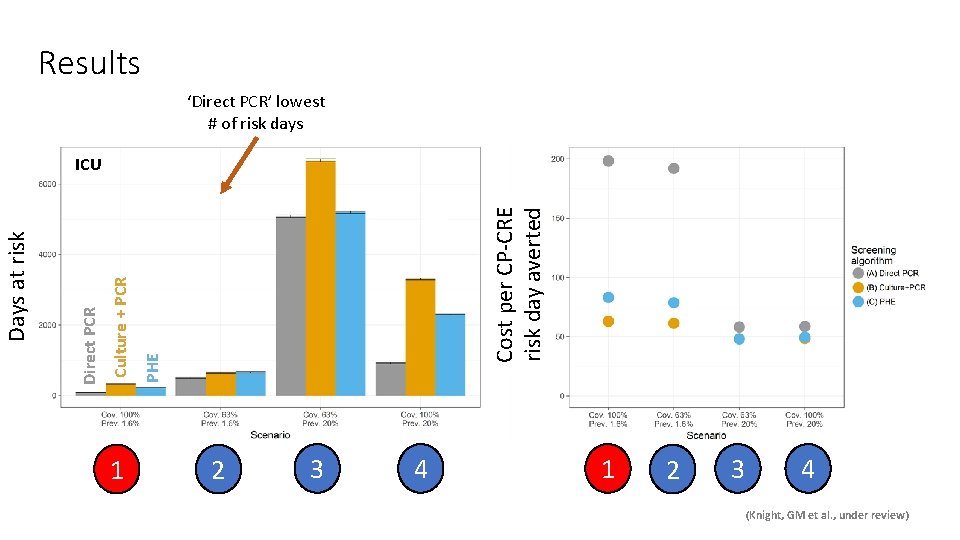
Results ‘Direct PCR’ lowest # of risk days 1 Cost per CP-CRE risk day averted PHE Culture + PCR Direct PCR Days at risk ICU 2 3 4 1 2 3 4 (Knight, GM et al. , under review)
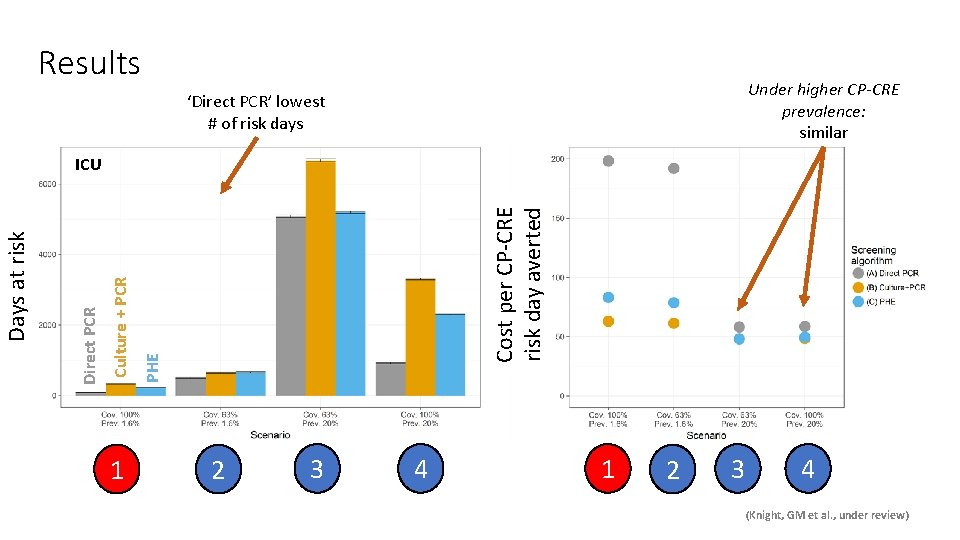
Results Under higher CP-CRE prevalence: similar ‘Direct PCR’ lowest # of risk days 1 Cost per CP-CRE risk day averted PHE Culture + PCR Direct PCR Days at risk ICU 2 3 4 1 2 3 4 (Knight, GM et al. , under review)
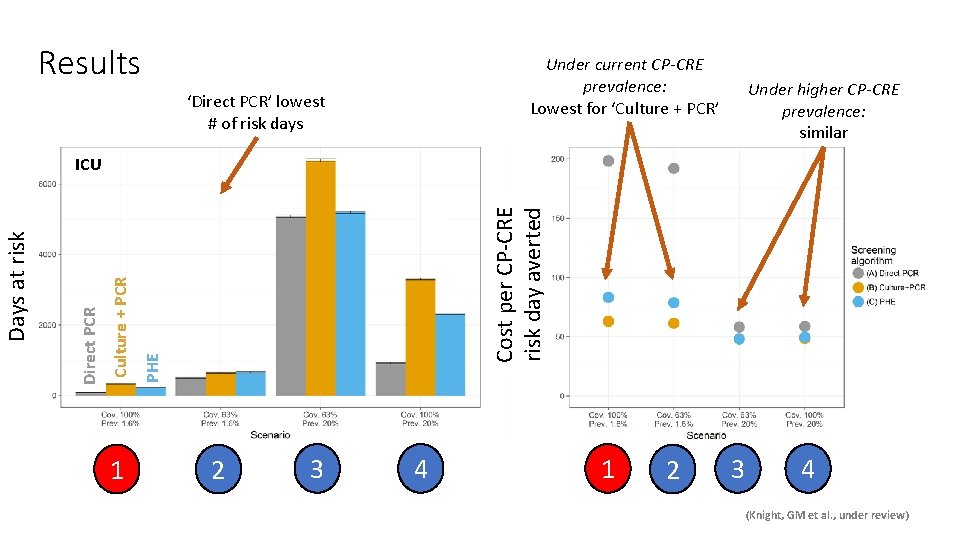
Results Under current CP-CRE prevalence: Lowest for ‘Culture + PCR’ ‘Direct PCR’ lowest # of risk days Under higher CP-CRE prevalence: similar 1 Cost per CP-CRE risk day averted PHE Culture + PCR Direct PCR Days at risk ICU 2 3 4 1 2 3 4 (Knight, GM et al. , under review)
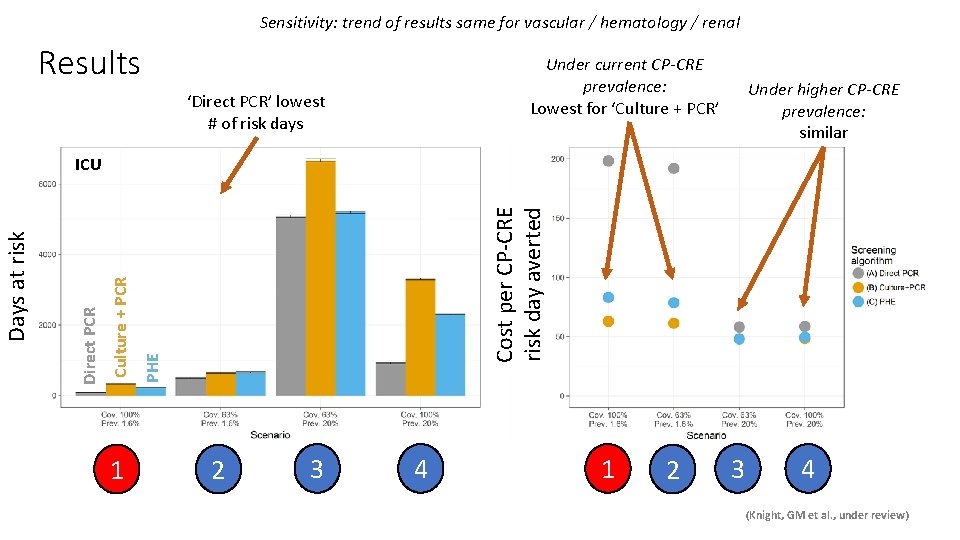
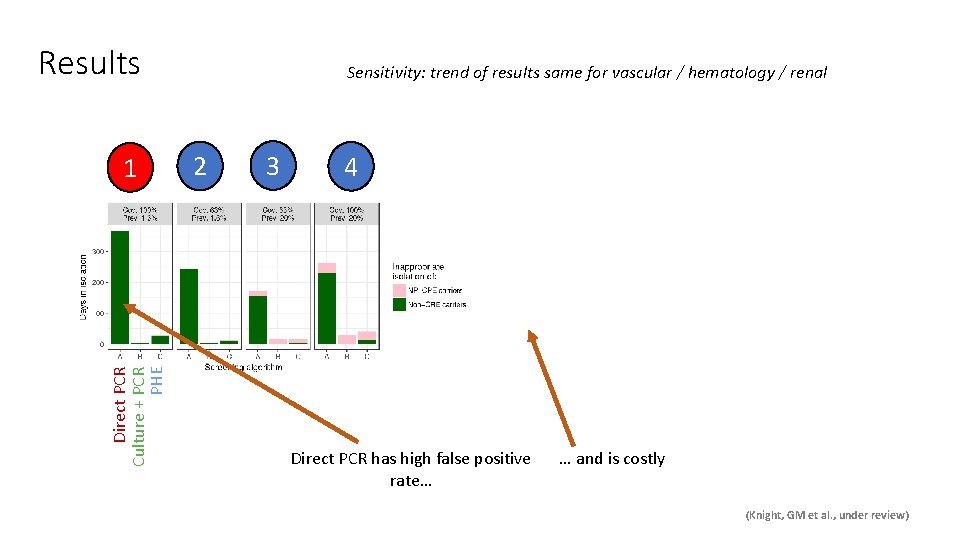
Sensitivity: trend of results same for vascular / hematology / renal Results Under current CP-CRE prevalence: Lowest for ‘Culture + PCR’ ‘Direct PCR’ lowest # of risk days Under higher CP-CRE prevalence: similar 1 Cost per CP-CRE risk day averted PHE Culture + PCR Direct PCR Days at risk ICU 2 3 4 1 2 3 4 (Knight, GM et al. , under review)
Conclusions Link to data Missing complexity: transmission / heterogeneity / implementation
Conclusions Link to data Missing complexity: transmission / heterogeneity / implementation • “Fast and expensive” too costly, unless higher prevalence • “Cheap and slow” best for ICHNT now • Next steps: PCR after first culture?
Conclusions Link to data Model available Inputs required: prevalence / length of stay / ward size / costs Missing complexity: transmission / heterogeneity / implementation • “Fast and expensive” too costly, unless higher prevalence • “Cheap and slow” best for ICHNT now • Next steps: PCR after first culture?
Conclusions Link to data Model available Inputs required: prevalence / length of stay / ward size / costs Missing complexity: transmission / heterogeneity / implementation • “Fast and expensive” too costly, unless higher prevalence • “Cheap and slow” best for ICHNT now • Next steps: PCR after first culture? X-AMR New cross-disciplinary pop-up journal from Microbiology society
Model available Inputs required: prevalence / length of stay / ward size / costs Conclusions Link to data Missing complexity: transmission / heterogeneity / implementation • “Fast and expensive” too costly, unless higher prevalence • “Cheap and slow” best for ICHNT now • Next steps: PCR after first culture? X-AMR New cross-disciplinary pop-up journal from Microbiology society Thanks to: - Elie Dyakova, Sid Mookerjee, Frances Davies, Eimear Brannigan, Jon Otter & Alison Holmes - ICHNT laboratory staff: Preetha Shibu and Jyothsna Dronavalli - The team at NIHR HPRU in HCAI and AMR at Imperial College London gwen. knight@lshtm. ac. uk

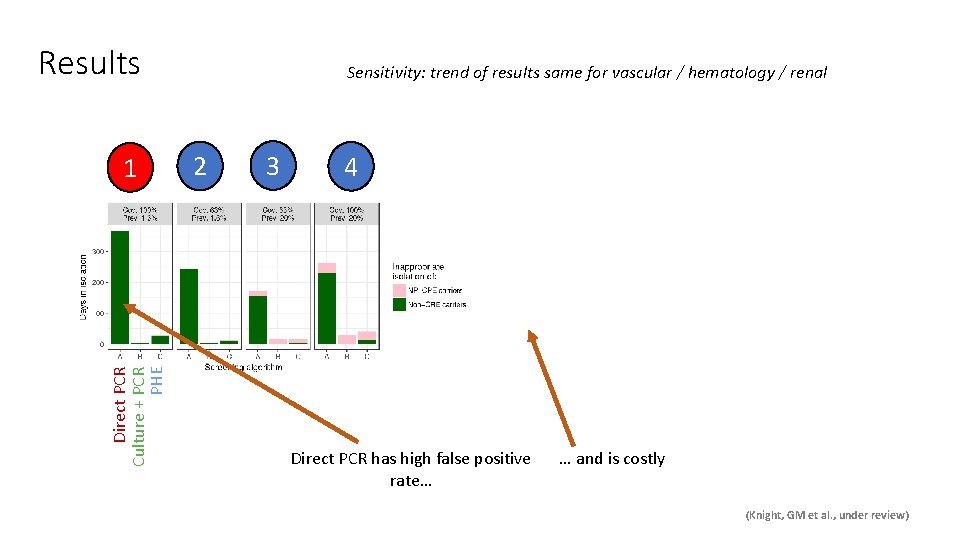
Results Direct PCR Culture + PCR PHE 1 Sensitivity: trend of results same for vascular / hematology / renal 2 3 4 Direct PCR has high false positive rate… … and is costly (Knight, GM et al. , under review)
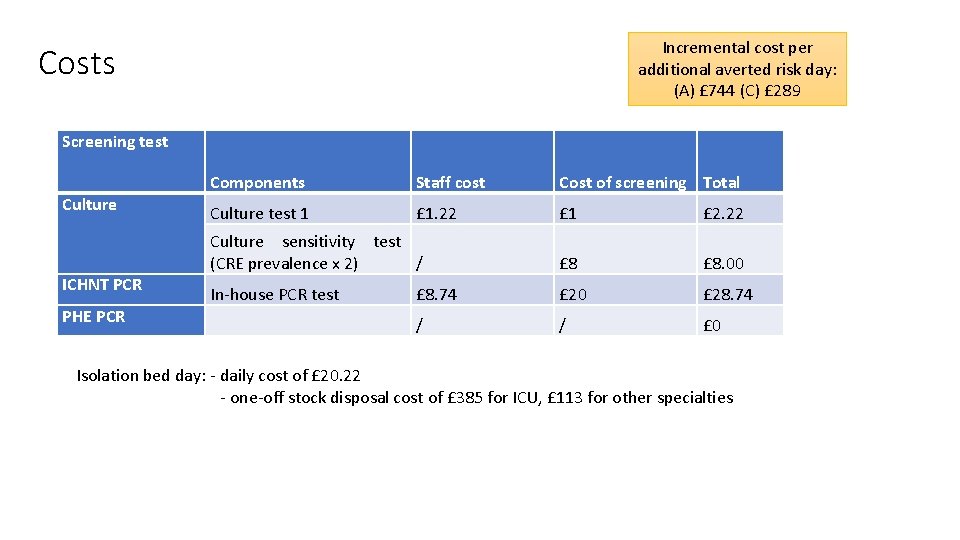
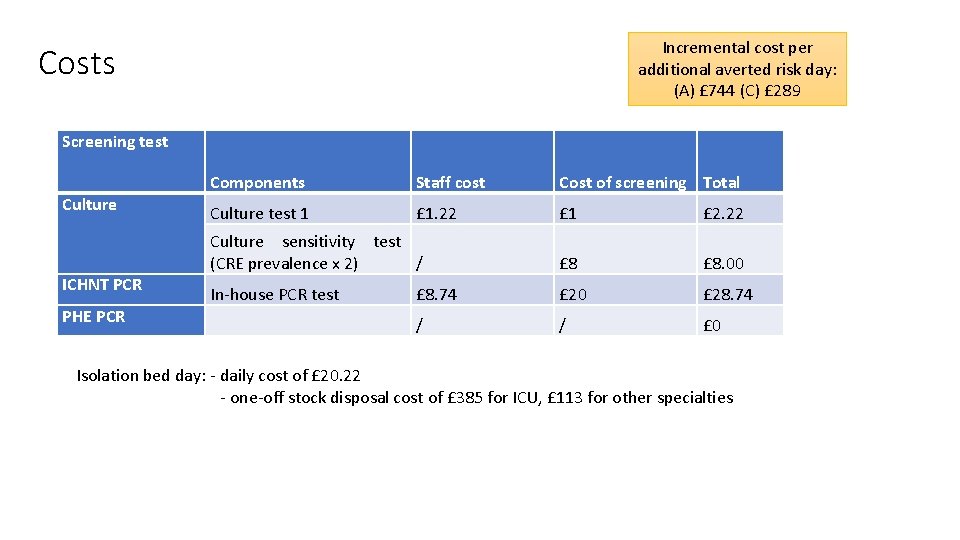
Incremental cost per additional averted risk day: (A) £ 744 (C) £ 289 Costs Screening test Culture ICHNT PCR PHE PCR Components Staff cost Cost of screening Total Culture test 1 £ 1. 22 £ 1 £ 2. 22 Culture sensitivity test (CRE prevalence x 2) / £ 8. 00 In-house PCR test £ 8. 74 £ 20 £ 28. 74 / / £ 0 Isolation bed day: - daily cost of £ 20. 22 - one-off stock disposal cost of £ 385 for ICU, £ 113 for other specialties
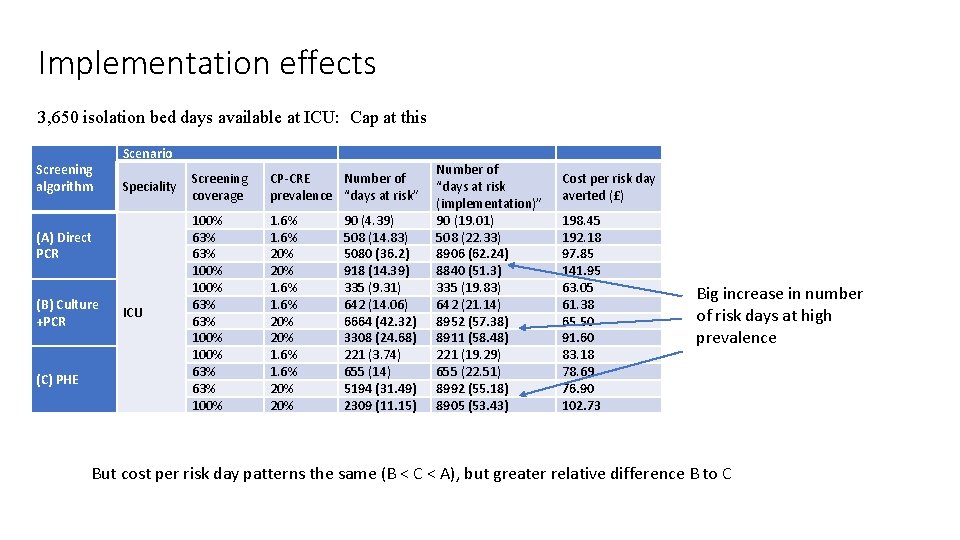
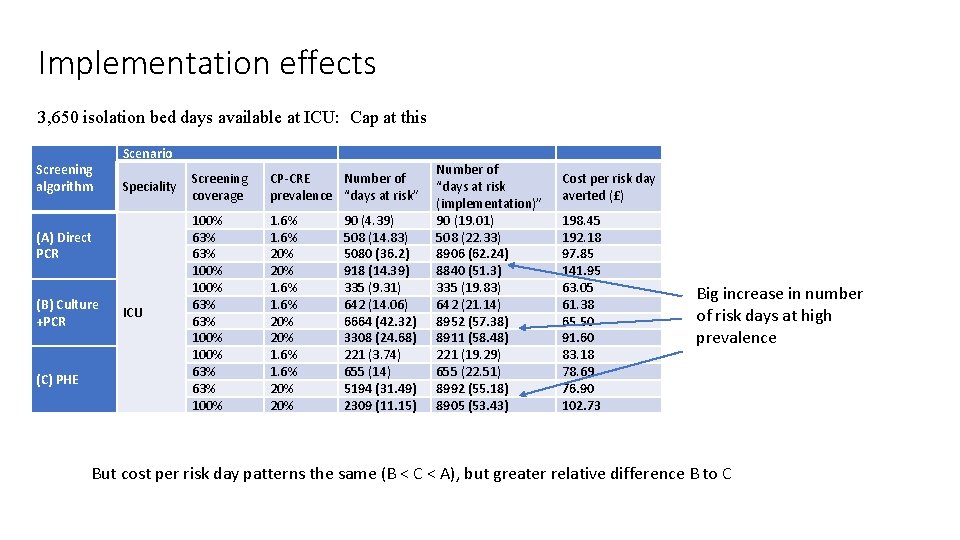
Implementation effects 3, 650 isolation bed days available at ICU: Cap at this Screening algorithm Scenario Speciality Screening coverage CP-CRE Number of prevalence “days at risk” ICU 100% 63% 63% 100% 63% 100% 1. 6% 20% 20% 1. 6% 20% (A) Direct PCR (B) Culture +PCR (C) PHE 90 (4. 39) 508 (14. 83) 5080 (36. 2) 918 (14. 39) 335 (9. 31) 642 (14. 06) 6664 (42. 32) 3308 (24. 68) 221 (3. 74) 655 (14) 5194 (31. 49) 2309 (11. 15) Number of “days at risk (implementation)” 90 (19. 01) 508 (22. 33) 8906 (62. 24) 8840 (51. 3) 335 (19. 83) 642 (21. 14) 8952 (57. 38) 8911 (58. 48) 221 (19. 29) 655 (22. 51) 8992 (55. 18) 8905 (53. 43) Cost per risk day averted (£) 198. 45 192. 18 97. 85 141. 95 63. 05 61. 38 65. 50 91. 60 83. 18 78. 69 76. 90 102. 73 Big increase in number of risk days at high prevalence But cost per risk day patterns the same (B < C < A), but greater relative difference B to C
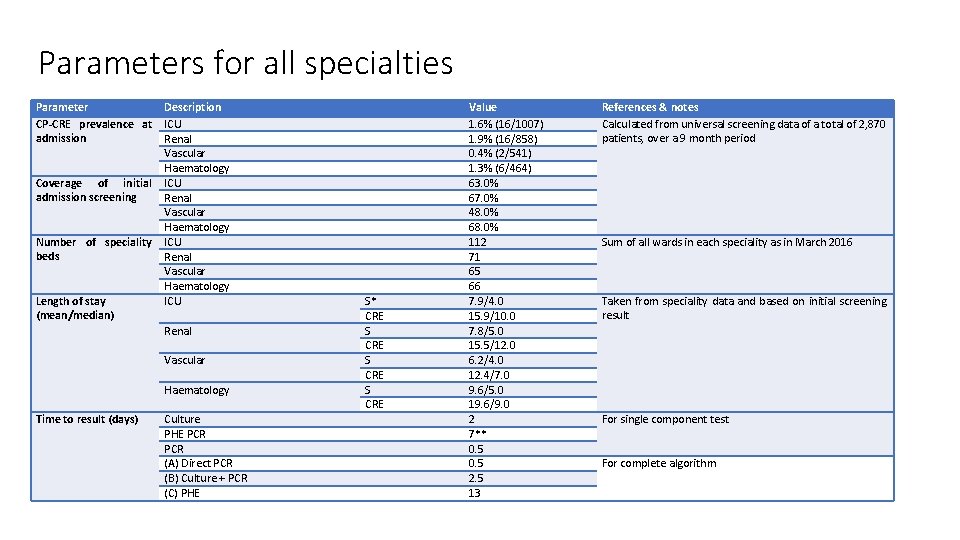
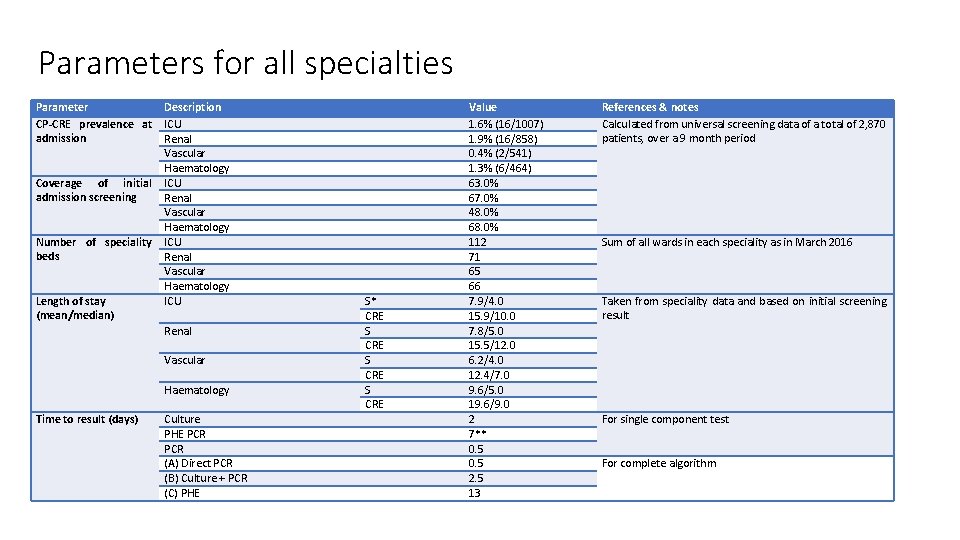
Parameters for all specialties Parameter CP-CRE prevalence at admission Coverage of initial admission screening Number of speciality beds Length of stay (mean/median) Description ICU Renal Vascular Haematology Time to result (days) Culture PHE PCR (A) Direct PCR (B) Culture + PCR (C) PHE S* CRE S CRE Value 1. 6% (16/1007) 1. 9% (16/858) 0. 4% (2/541) 1. 3% (6/464) 63. 0% 67. 0% 48. 0% 68. 0% 112 71 65 66 7. 9/4. 0 15. 9/10. 0 7. 8/5. 0 15. 5/12. 0 6. 2/4. 0 12. 4/7. 0 9. 6/5. 0 19. 6/9. 0 2 7** 0. 5 2. 5 13 References & notes Calculated from universal screening data of a total of 2, 870 patients, over a 9 month period Sum of all wards in each speciality as in March 2016 Taken from speciality data and based on initial screening result For single component test For complete algorithm
Outcomes for all four specialties 0. 4% CP-CRE prev 1 Baseline prevalence 100% screening coverage
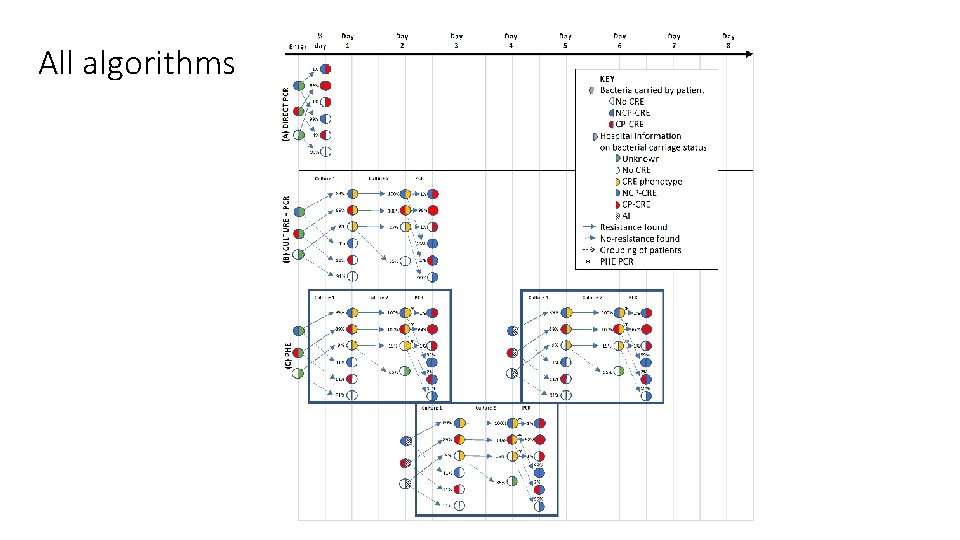
All algorithms
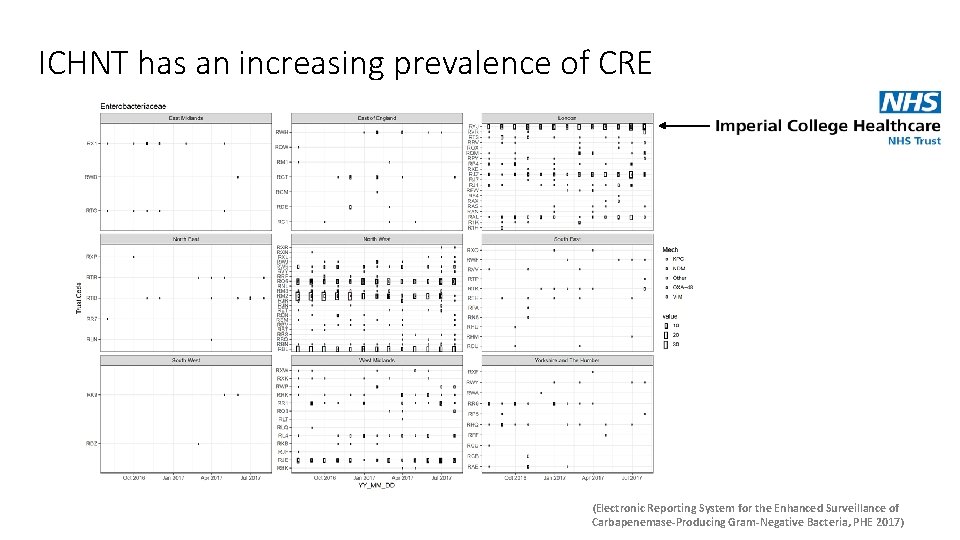
ICHNT has an increasing prevalence of CRE (Electronic Reporting System for the Enhanced Surveillance of Carbapenemase-Producing Gram-Negative Bacteria, PHE 2017)
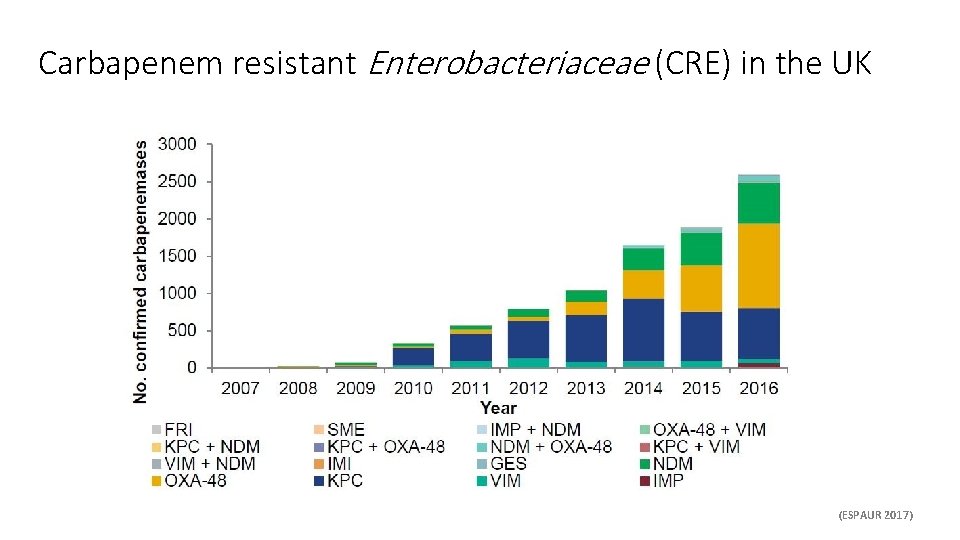
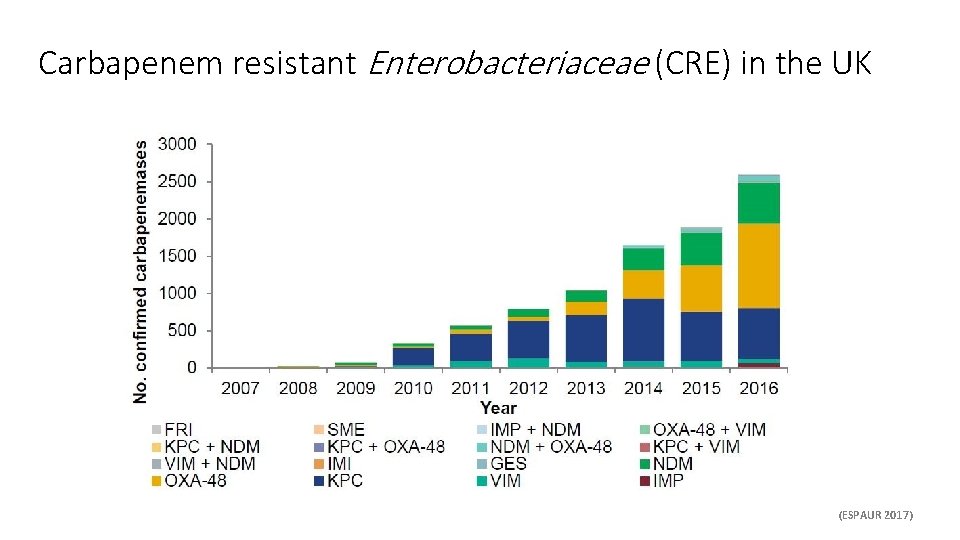
Carbapenem resistant Enterobacteriaceae (CRE) in the UK (ESPAUR 2017)