Exercise Prescription for the Pulmonary Patient Chuck Kitchen

- Slides: 33
Exercise Prescription for the Pulmonary Patient Chuck Kitchen, MA, FAACVPR Chuck. kitchen@gmail. com
PULMONARY DISEASES OBSTRUCTIVE DISEASES COPD-Chronic airway obstruction Emphysema-Hyperinflation of the lungs, can’t get bad air out Chronic Bronchitis-Chronic sputum production and coughing Asthma-increased airway reactivity leading to narrowing of airways
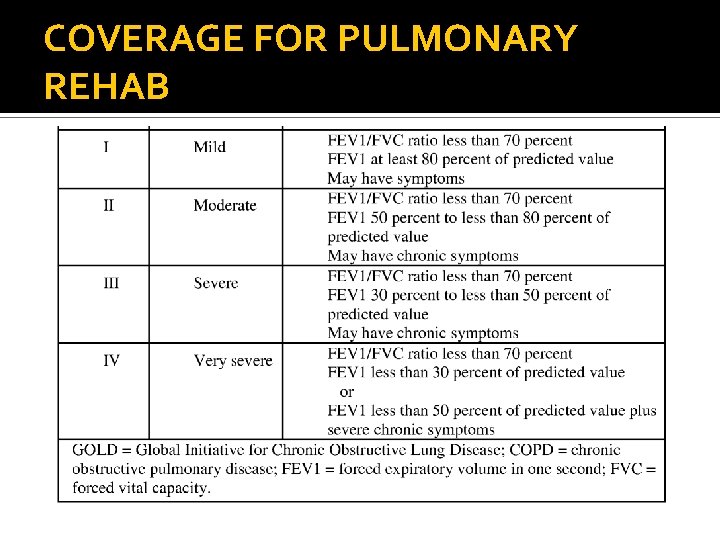
COVERAGE FOR PULMONARY REHAB PR only covered for Moderate, Severe, Very Severe COPD GOLD classification
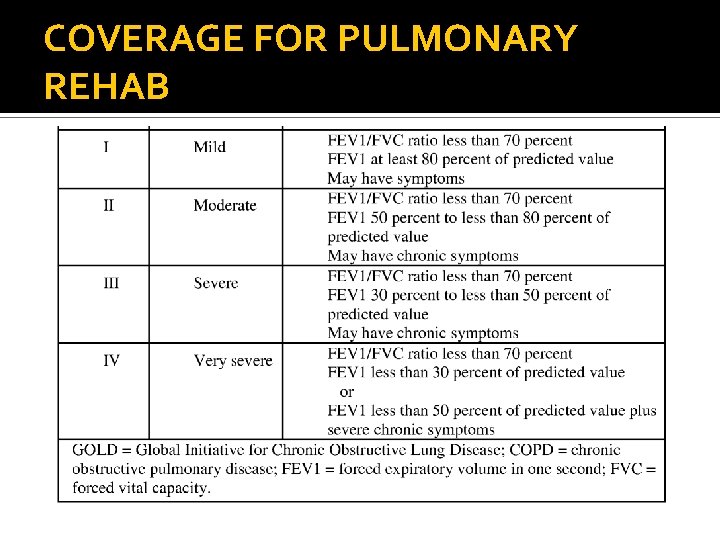
COVERAGE FOR PULMONARY REHAB
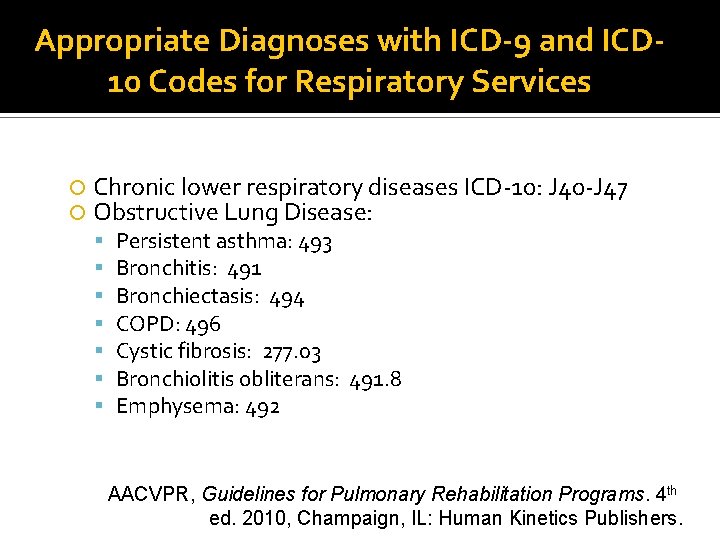
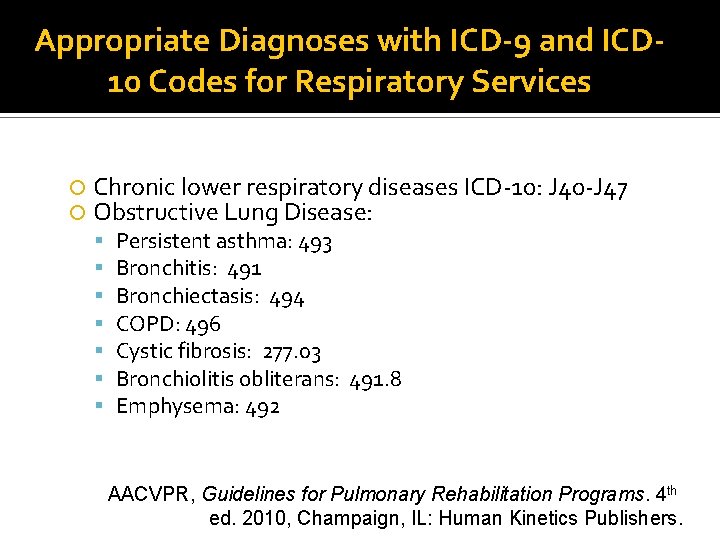
Appropriate Diagnoses with ICD-9 and ICD 10 Codes for Respiratory Services Chronic lower respiratory diseases ICD-10: J 40 -J 47 Obstructive Lung Disease: Persistent asthma: 493 Bronchitis: 491 Bronchiectasis: 494 COPD: 496 Cystic fibrosis: 277. 03 Bronchiolitis obliterans: 491. 8 Emphysema: 492 AACVPR, Guidelines for Pulmonary Rehabilitation Programs. 4 th ed. 2010, Champaign, IL: Human Kinetics Publishers.
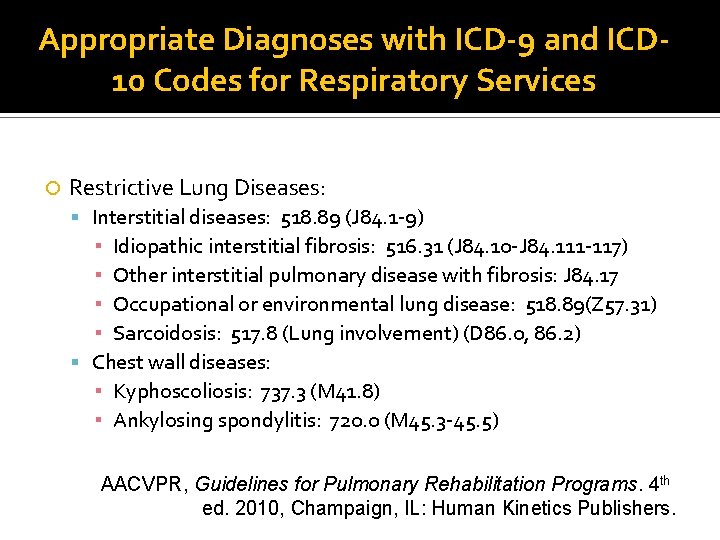
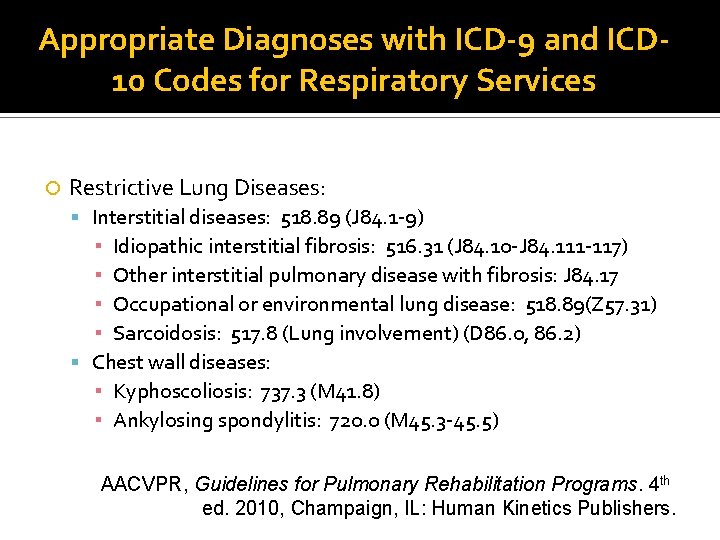
Appropriate Diagnoses with ICD-9 and ICD 10 Codes for Respiratory Services Restrictive Lung Diseases: Interstitial diseases: 518. 89 (J 84. 1 -9) ▪ Idiopathic interstitial fibrosis: 516. 31 (J 84. 10 -J 84. 111 -117) ▪ Other interstitial pulmonary disease with fibrosis: J 84. 17 ▪ Occupational or environmental lung disease: 518. 89(Z 57. 31) ▪ Sarcoidosis: 517. 8 (Lung involvement) (D 86. 0, 86. 2) Chest wall diseases: ▪ Kyphoscoliosis: 737. 3 (M 41. 8) ▪ Ankylosing spondylitis: 720. 0 (M 45. 3 -45. 5) AACVPR, Guidelines for Pulmonary Rehabilitation Programs. 4 th ed. 2010, Champaign, IL: Human Kinetics Publishers.
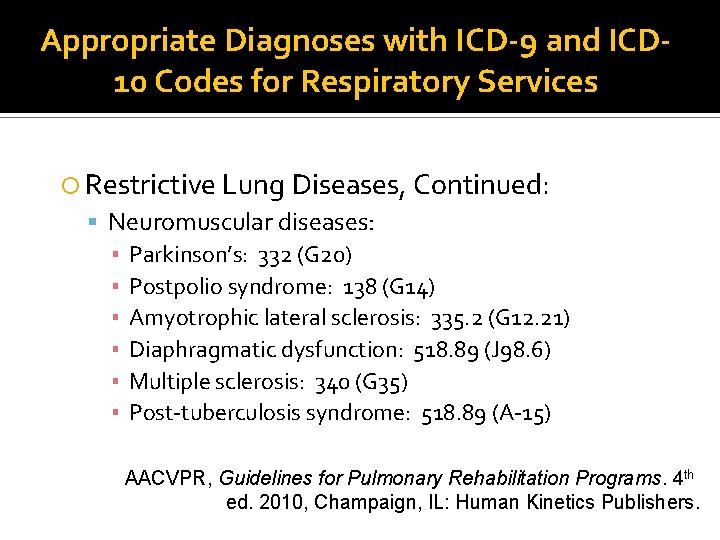
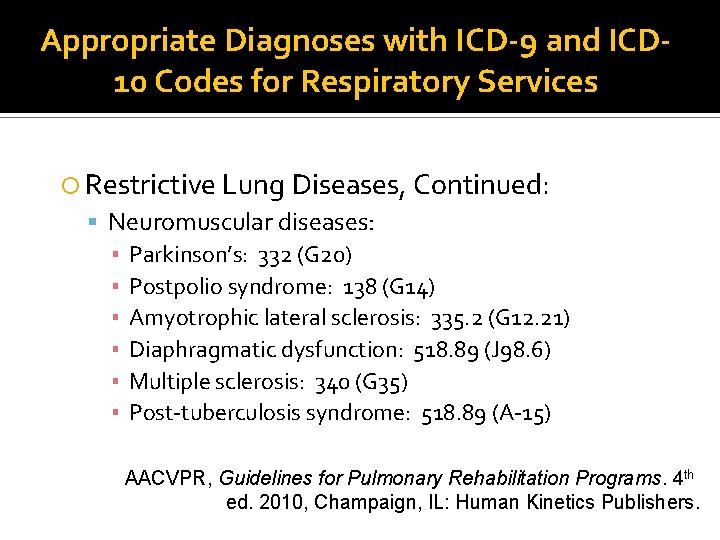
Appropriate Diagnoses with ICD-9 and ICD 10 Codes for Respiratory Services Restrictive Lung Diseases, Continued: Neuromuscular diseases: ▪ Parkinson’s: 332 (G 20) ▪ Postpolio syndrome: 138 (G 14) ▪ Amyotrophic lateral sclerosis: 335. 2 (G 12. 21) ▪ Diaphragmatic dysfunction: 518. 89 (J 98. 6) ▪ Multiple sclerosis: 340 (G 35) ▪ Post-tuberculosis syndrome: 518. 89 (A-15) AACVPR, Guidelines for Pulmonary Rehabilitation Programs. 4 th ed. 2010, Champaign, IL: Human Kinetics Publishers.
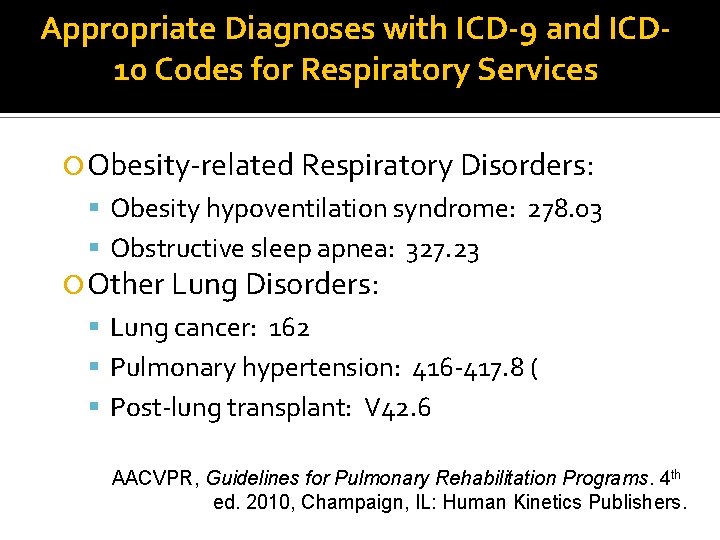
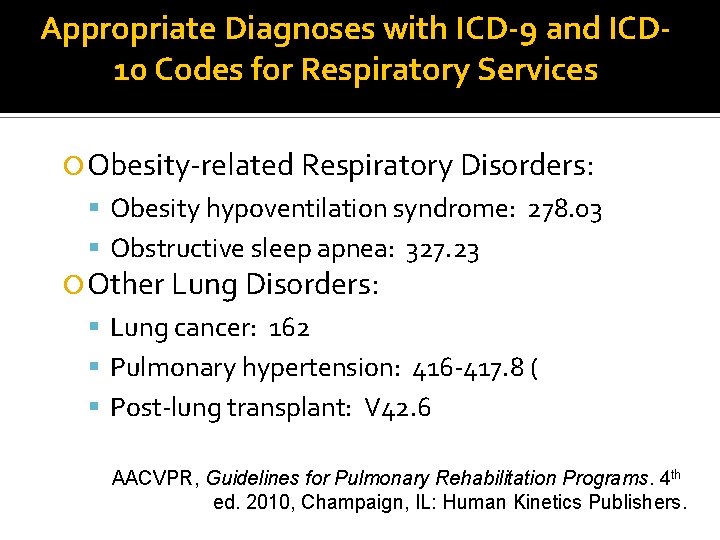
Appropriate Diagnoses with ICD-9 and ICD 10 Codes for Respiratory Services Obesity-related Respiratory Disorders: Obesity hypoventilation syndrome: 278. 03 Obstructive sleep apnea: 327. 23 Other Lung Disorders: Lung cancer: 162 Pulmonary hypertension: 416 -417. 8 ( Post-lung transplant: V 42. 6 AACVPR, Guidelines for Pulmonary Rehabilitation Programs. 4 th ed. 2010, Champaign, IL: Human Kinetics Publishers.
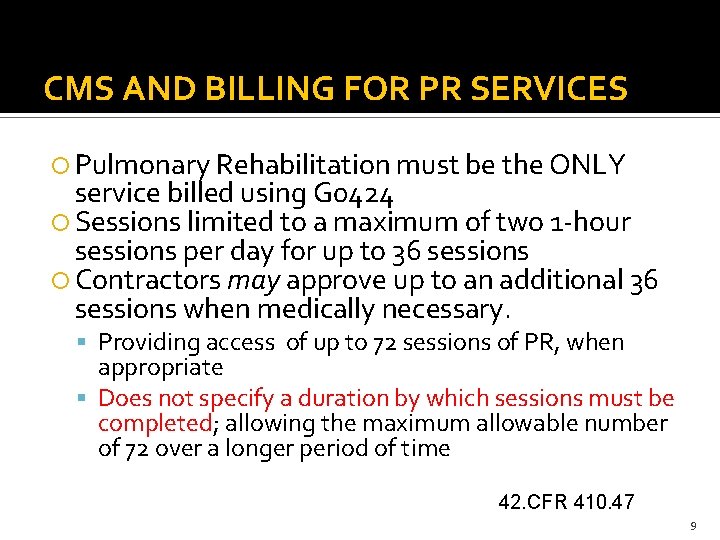
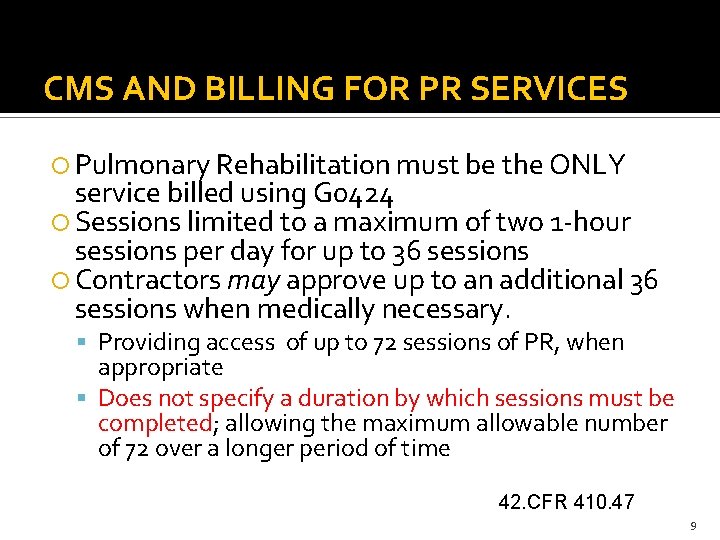
CMS AND BILLING FOR PR SERVICES Pulmonary Rehabilitation must be the ONLY service billed using G 0424 Sessions limited to a maximum of two 1 -hour sessions per day for up to 36 sessions Contractors may approve up to an additional 36 sessions when medically necessary. Providing access of up to 72 sessions of PR, when appropriate Does not specify a duration by which sessions must be completed; allowing the maximum allowable number of 72 over a longer period of time 42. CFR 410. 47 9
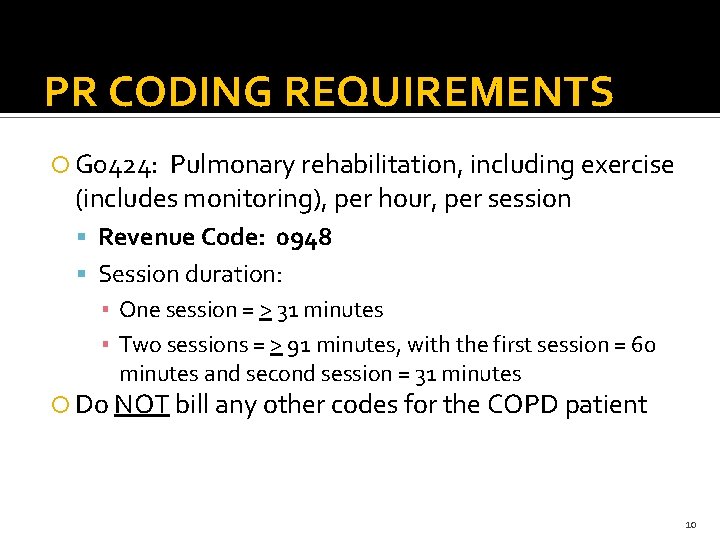
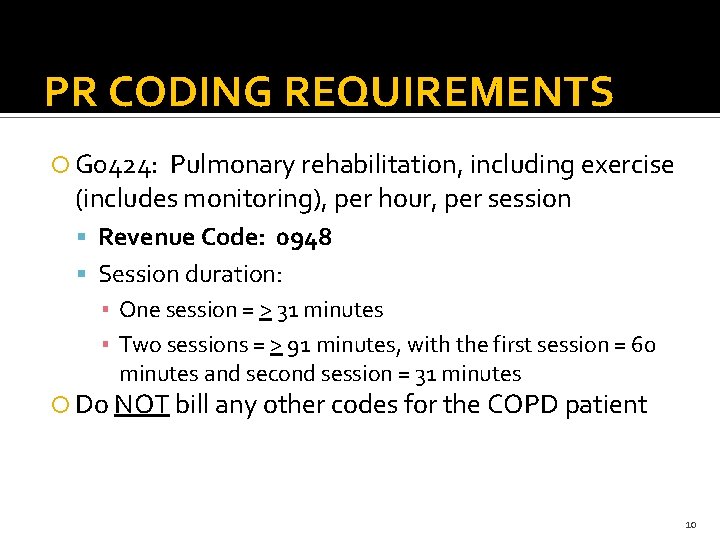
PR CODING REQUIREMENTS G 0424: Pulmonary rehabilitation, including exercise (includes monitoring), per hour, per session Revenue Code: 0948 Session duration: ▪ One session = > 31 minutes ▪ Two sessions = > 91 minutes, with the first session = 60 minutes and second session = 31 minutes Do NOT bill any other codes for the COPD patient 10
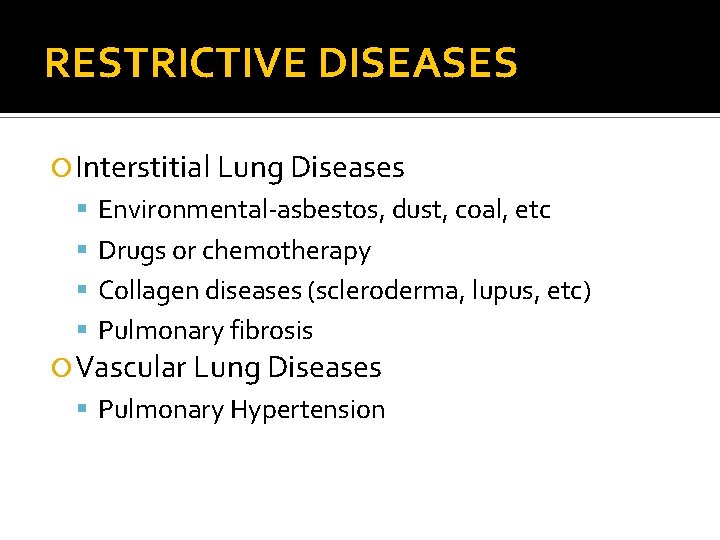
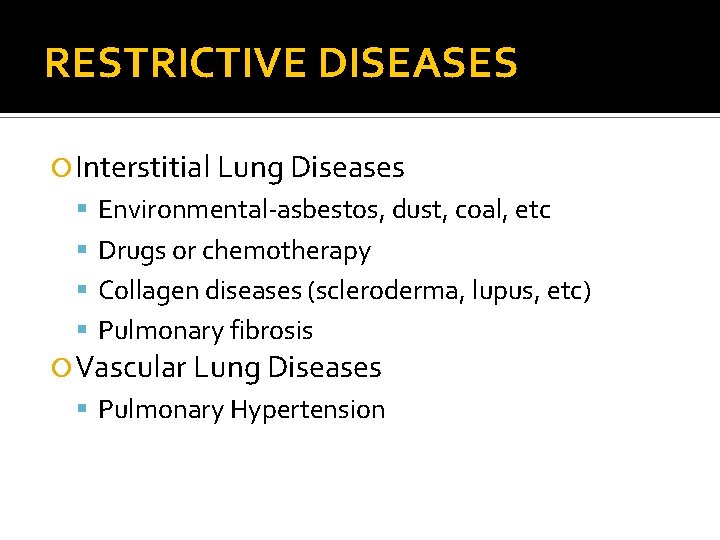
RESTRICTIVE DISEASES Interstitial Lung Diseases Environmental-asbestos, dust, coal, etc Drugs or chemotherapy Collagen diseases (scleroderma, lupus, etc) Pulmonary fibrosis Vascular Lung Diseases Pulmonary Hypertension
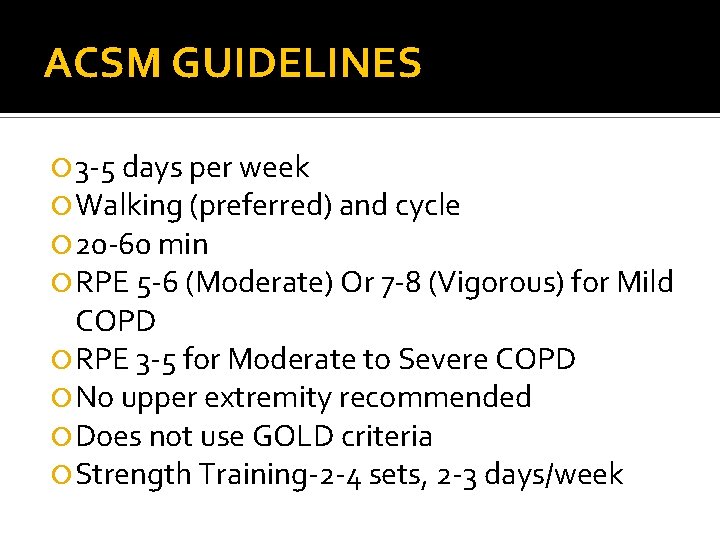
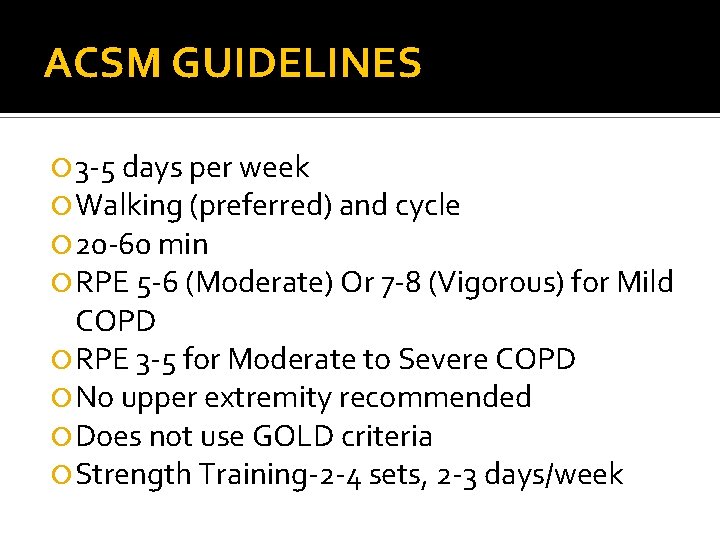
ACSM GUIDELINES 3 -5 days per week Walking (preferred) and cycle 20 -60 min RPE 5 -6 (Moderate) Or 7 -8 (Vigorous) for Mild COPD RPE 3 -5 for Moderate to Severe COPD No upper extremity recommended Does not use GOLD criteria Strength Training-2 -4 sets, 2 -3 days/week
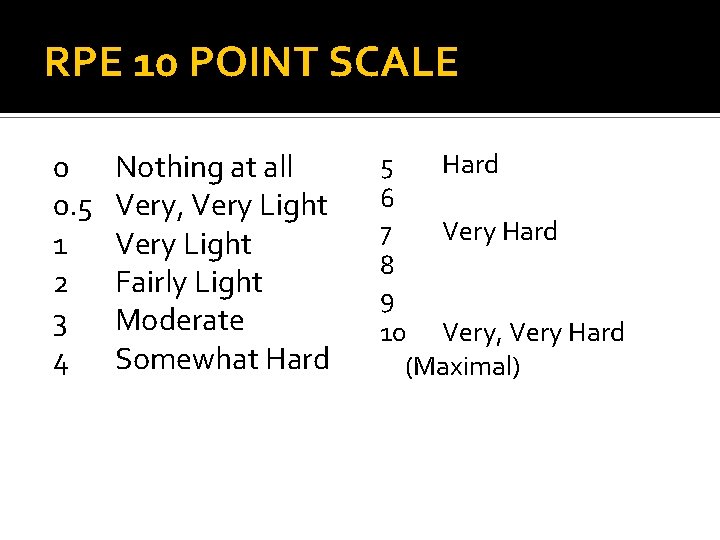
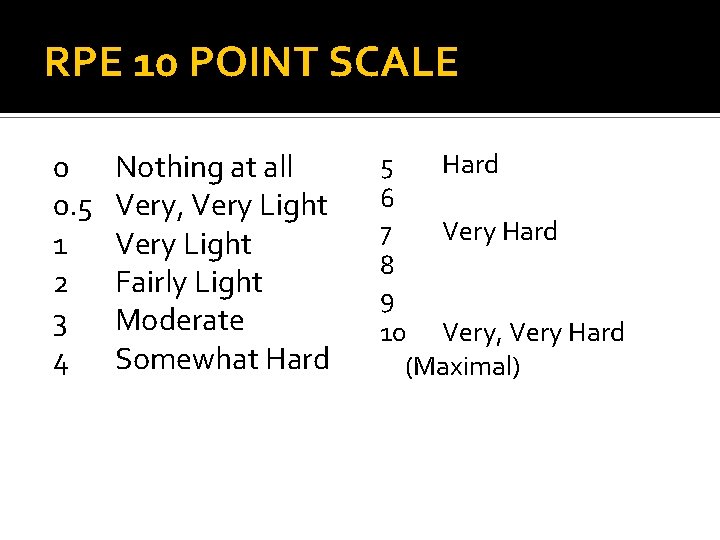
RPE 10 POINT SCALE 0 0. 5 1 2 3 4 Nothing at all Very, Very Light Fairly Light Moderate Somewhat Hard 5 Hard 6 7 Very Hard 8 9 10 Very, Very Hard (Maximal)
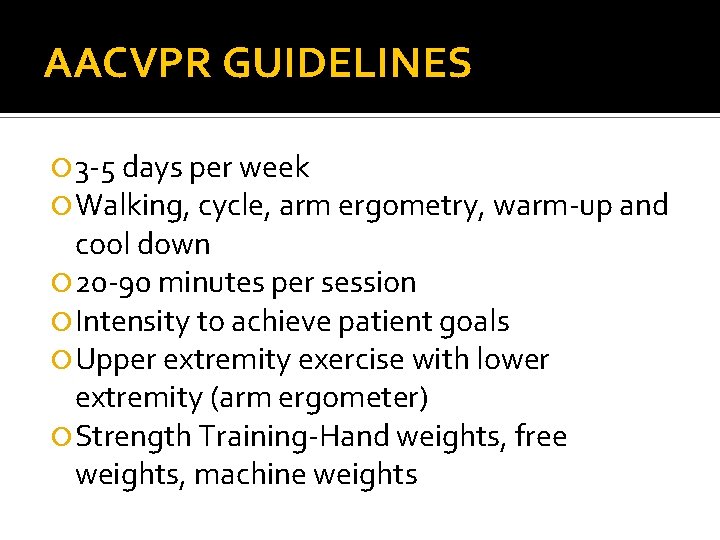
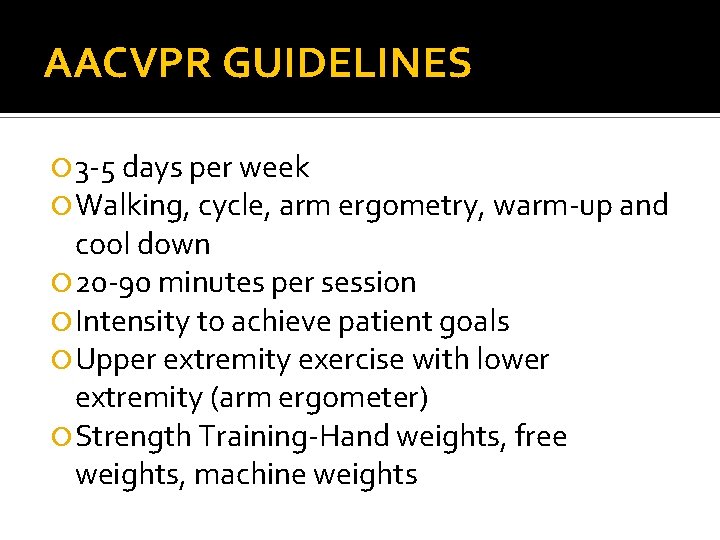
AACVPR GUIDELINES 3 -5 days per week Walking, cycle, arm ergometry, warm-up and cool down 20 -90 minutes per session Intensity to achieve patient goals Upper extremity exercise with lower extremity (arm ergometer) Strength Training-Hand weights, free weights, machine weights
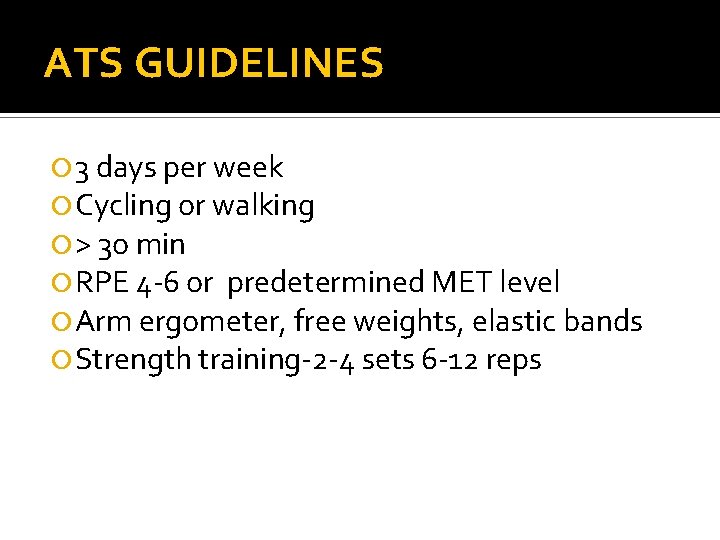
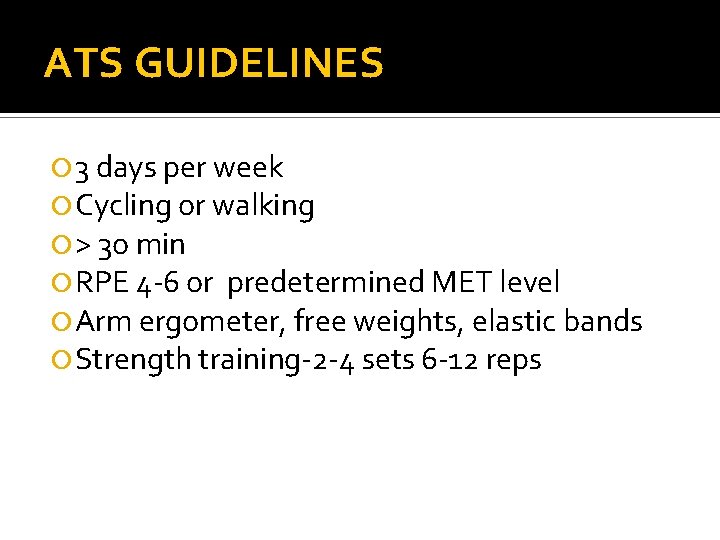
ATS GUIDELINES 3 days per week Cycling or walking > 3 o min RPE 4 -6 or predetermined MET level Arm ergometer, free weights, elastic bands Strength training-2 -4 sets 6 -12 reps
EXERCISE PRESCRIPTION 6 Min Walk Test-Widely used tool to determine exercise prescription Determine initial exercise intensity
EXERCISE PRESCRIPTION Frequency Intensity Time Type F. I. T. T PRINCIPLE
EXERCISE PRESCRIPTION FREQUENCY 3 to 5 times per week
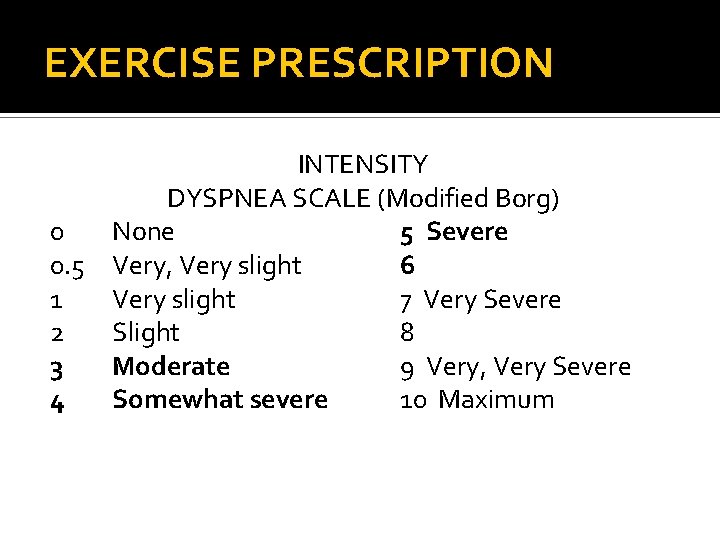
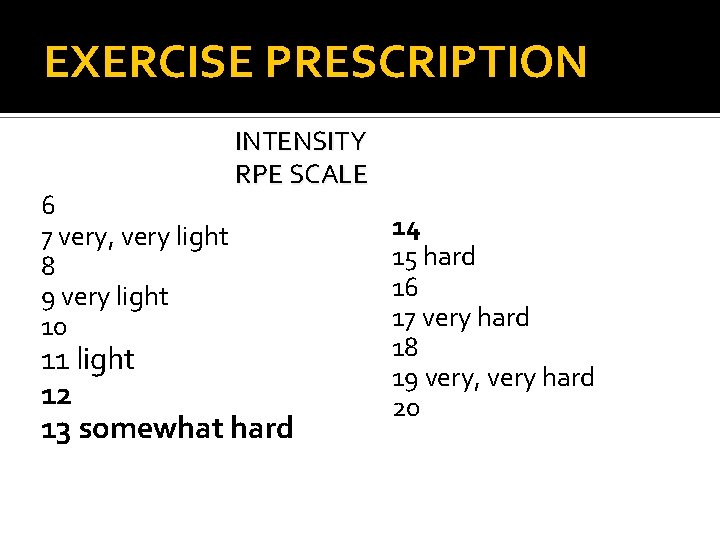
EXERCISE PRESCRIPTION INTENSITY 4 -6 Borg Dyspnea scale 12 -14 RPE scale
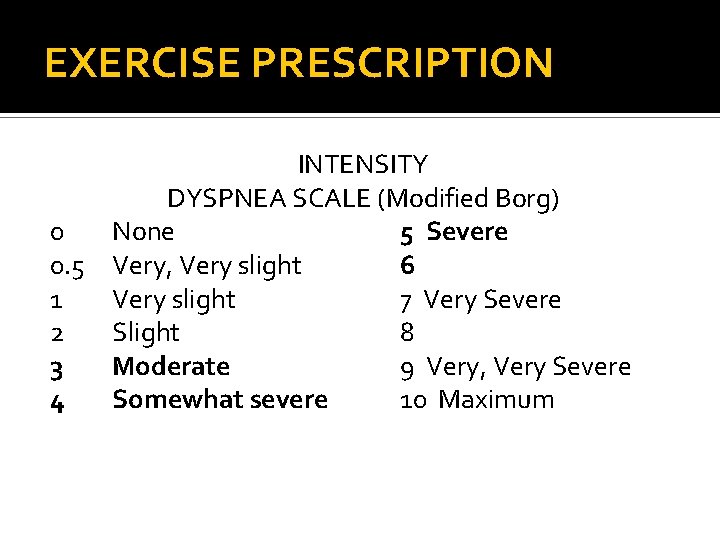
EXERCISE PRESCRIPTION INTENSITY DYSPNEA SCALE (Modified Borg) 0 None 5 Severe 0. 5 Very, Very slight 6 1 Very slight 7 Very Severe 2 Slight 8 3 Moderate 9 Very, Very Severe 4 Somewhat severe 10 Maximum
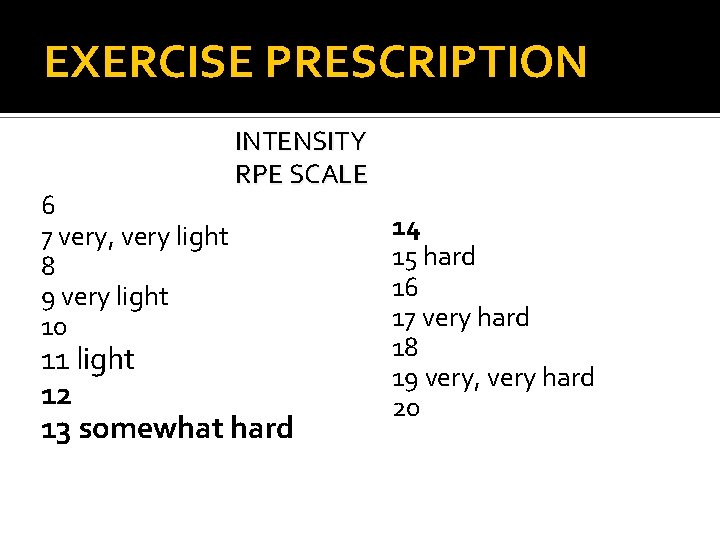
EXERCISE PRESCRIPTION 6 7 very, very light 8 9 very light 10 INTENSITY RPE SCALE 11 light 12 13 somewhat hard 14 15 hard 16 17 very hard 18 19 very, very hard 20
EXERCISE PRESCRIPTION TIME 20 to 6 o minutes Can use interval training especially for beginners or low level patients Total exercise time is most important
EXERCISE PRESCRIPTION TYPE Continuous Aerobic High Intensity Interval Training not found to have same benefits as with Cardiac Population (CHF, etc) Possibly due to Dyspnea Low to moderate intensity interval training can be used Resistance Training
STRENGTH TRAINING No data for “optimal” resistance training program Important to help maintain muscle mass (muscle wasting) 1 -3 sets 8 -12 repetitions 2 -3 days per week
SPECIAL CONSIDERATIONS Exercise capacity often limited by dyspnea, not MET level or RPE, etc Sa. O 2 Monitoring Supplemental O 2 to maintain 88%-90% Generally, cycle or other non weight bearing equipment has higher O 2 sats Consider continuous exercise on cycle, recumbent stepper, etc. Interval on TM
SPECIAL CONSIDERATIONS Take bronchodilators prior to exercise
RESTRICTIVE DISEASES Short term benefits from PR Smaller improvements and shorter lasting Typically more dyspnea than obstructive disease Generally more reliant on supplemental O 2
PULMONARY HYPERTENSION Careful to maintain O 2 sats above 88%-90% Monitor BP and HR Consider telemetry monitoring Exercise Intensity should be light to moderate ONLY Monitor for lightheadedness, chest pain, etc

INSPIRATORY MUSCLE TRAINERS
INSPIRATORY MUSCLE TRAINING AACVPR and ACCP do not recognize IMT as part of Pulmonary Rehab Devices used to impose resistance or load Patients increase inspiratory muscle strength Significant decreases in dyspnea Increased walking distance However, no increase in peak power Increased quality of life measures
EXERCISE PRESCRIPTION Exercise Prescription is an Art!! Every patient is different 31
REFERENCES American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs, 4 th ed. Champaign, IL; Human Kinetics, 2010. Garvey C, Fullwood MD, Rigler J. Pulmonary Rehabilitation Exercise Prescription in Chronic Obstructive Lung Disease. JCRP 2013; 33: 314 -322 Johnson-Warrington V, Harrison S, Mitchell K, et al. Exercise Capacity and Physical Activity in Patients With COPD and Healthy Subjects Classified as Medical Research Council Dyspnea Scale Grade 2. JCRP 2014; 34(2): 150 -154
REFERENCES Ryerson CJ, Cayou C, Toop F, et al. Pulmonary rehabilitation improves long-term outcomes in interstitial lung disease: A prospective cohort study. Respir Med 2014; 108(1): 203 -210 Spruit MA, Singh SJ, Garvey C, et al. An Official American Thoracic Society/European Respiratory Society Statement: Key Concepts and Advances in Pulmonary Rehabilitation. Am J Respir Crit Care Med 2013; 188(8): e 13 -e 64
 Chuck kitchen
Chuck kitchen Specially constructed stainless steel truck
Specially constructed stainless steel truck How to write an exercise prescription
How to write an exercise prescription Principles of therapeutic exercise
Principles of therapeutic exercise Exercise prescription example
Exercise prescription example In the kitchen or at the kitchen grammar
In the kitchen or at the kitchen grammar Prepositions of place
Prepositions of place Patient 2 patient
Patient 2 patient Chuck bartel
Chuck bartel Kovar tine weeder
Kovar tine weeder Management by chuck williams
Management by chuck williams What is swing over carriage mcq
What is swing over carriage mcq Chuck close childhood
Chuck close childhood Chuck cusack
Chuck cusack Meanbp
Meanbp Chuck allison
Chuck allison Chuck thacker
Chuck thacker Transportation
Transportation Chuck moran skillsoft
Chuck moran skillsoft Eqdfa
Eqdfa Sculpture in asl
Sculpture in asl Chuck huber stata
Chuck huber stata Chuck mohler cornell
Chuck mohler cornell Lca stata
Lca stata Castaway character
Castaway character Chuck cagle
Chuck cagle Chuck grimm
Chuck grimm Drill press tray
Drill press tray Telus work styles
Telus work styles Chuck hauck
Chuck hauck Chuck connell
Chuck connell Pitot tube bernoulli equation
Pitot tube bernoulli equation Chuck close self portrait 1997
Chuck close self portrait 1997 Chuck tolbert
Chuck tolbert