Episodes of Care Tenn Care Episodes Market and
- Slides: 16
Episodes of Care Tenn. Care Episodes
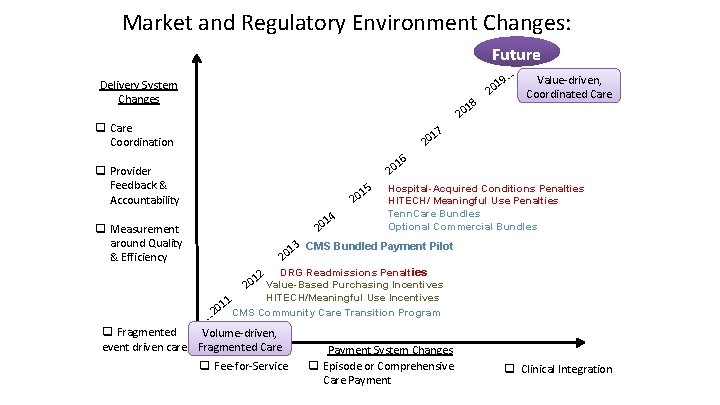
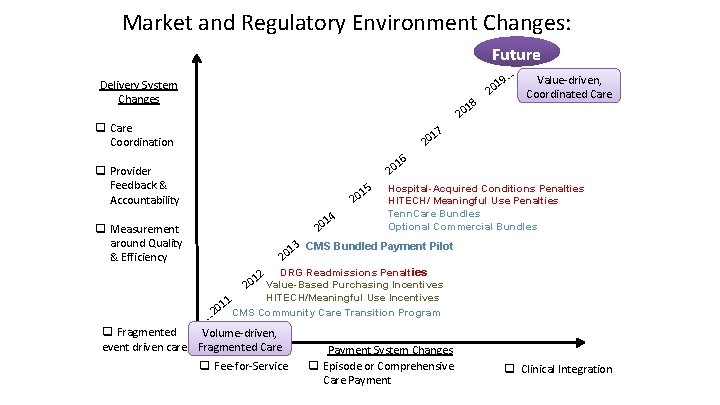
Market and Regulatory Environment Changes: Future 9… Delivery System Changes 18 Value-driven, Coordinated Care 20 q Care Coordination 17 20 20 q Provider Feedback & Accountability q Measurement around Quality & Efficiency 1 20 15 20 14 20 16 Hospital-Acquired Conditions Penalties HITECH/ Meaningful Use Penalties Tenn. Care Bundles Optional Commercial Bundles 13 CMS Bundled Payment Pilot 20 12 DRG Readmissions Penalties 20 Value-Based Purchasing Incentives HITECH/Meaningful Use Incentives 1 01 CMS Community Care Transition Program 2 … q Fragmented Volume-driven, event driven care Fragmented Care q Fee-for-Service Payment System Changes q Episode or Comprehensive Care Payment q Clinical Integration
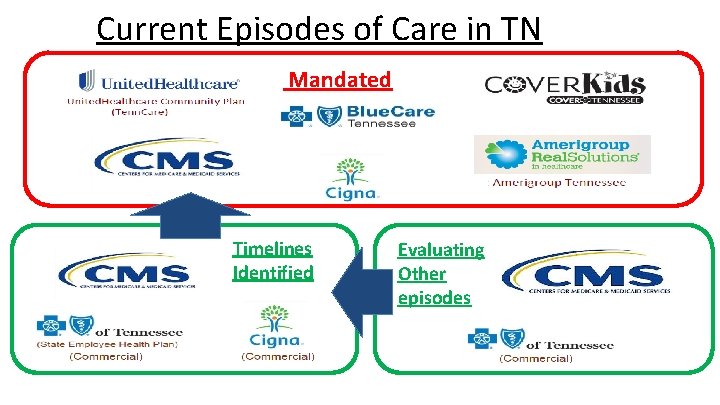
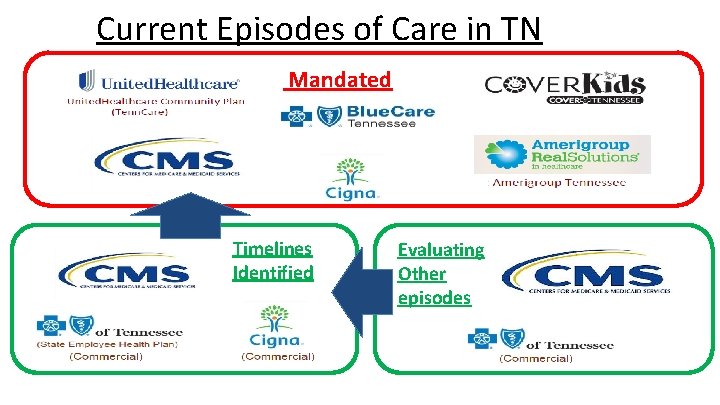
Current Episodes of Care in TN Mandated Timelines Identified Evaluating Other episodes
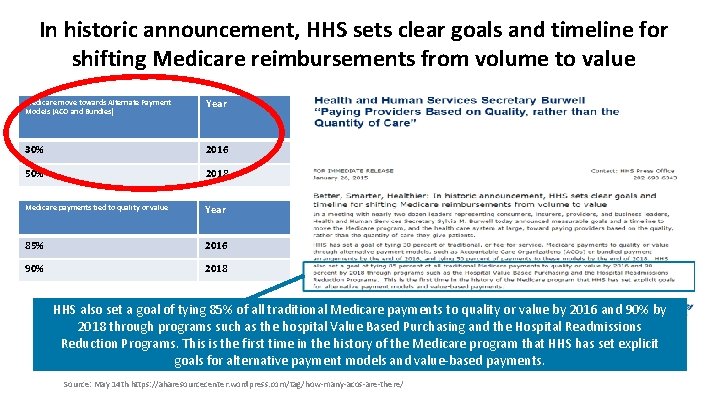
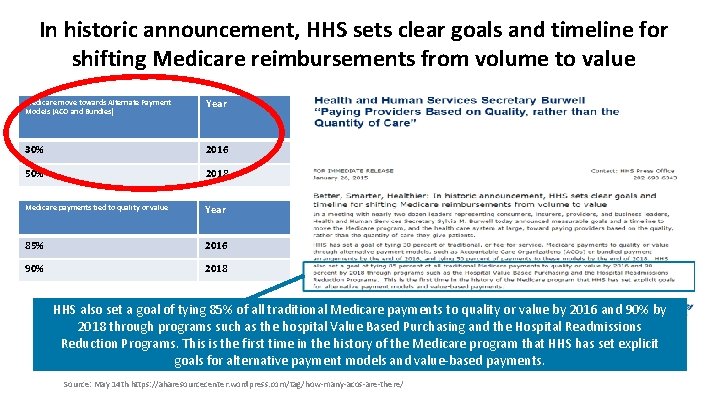
In historic announcement, HHS sets clear goals and timeline for shifting Medicare reimbursements from volume to value Medicare move towards Alternate Payment Models (ACO and Bundles) Year 30% 2016 50% 2018 Medicare payments tied to quality or value Year 85% 2016 90% 2018 HHS also set a goal of tying 85% of all traditional Medicare payments to quality or value by 2016 and 90% by 2018 through programs such as the hospital Value Based Purchasing and the Hospital Readmissions Reduction Programs. This is the first time in the history of the Medicare program that HHS has set explicit goals for alternative payment models and value-based payments. Source: May 14 th https: //aharesourcecenter. wordpress. com/tag/how-many-acos-are-there/
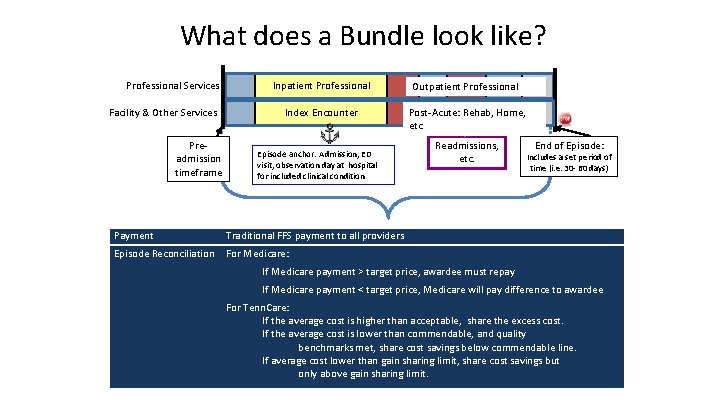
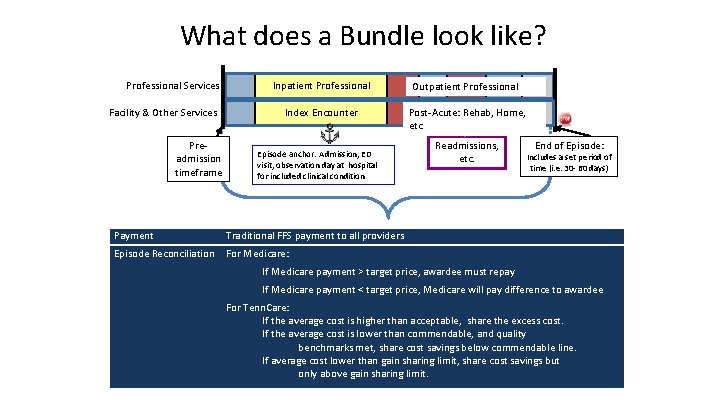
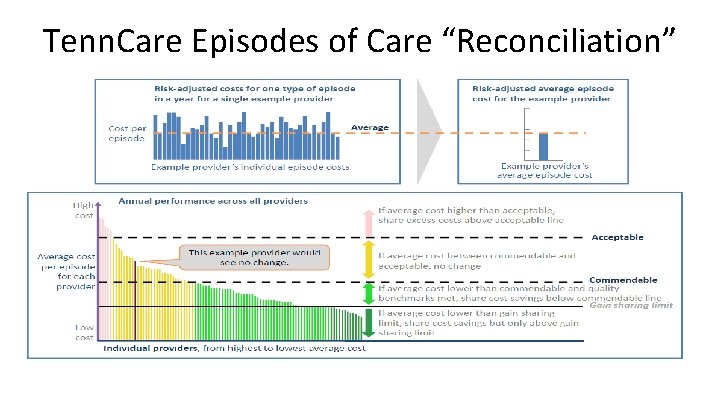
What does a Bundle look like? Professional Services Facility & Other Services Preadmission timeframe Inpatient Professional Outpatient Professional Index Encounter Post-Acute: Rehab, Home, etc Episode anchor: Admission, ED visit, observation day at hospital for included clinical condition Payment Traditional FFS payment to all providers Episode Reconciliation For Medicare: Readmissions, etc. End of Episode: Includes a set period of time (i. e. 30 - 60 days) If Medicare payment > target price, awardee must repay If Medicare payment < target price, Medicare will pay difference to awardee For Tenn. Care: If the average cost is higher than acceptable, share the excess cost. If the average cost is lower than commendable, and quality benchmarks met, share cost savings below commendable line. If average cost lower than gain sharing limit, share cost savings but only above gain sharing limit.
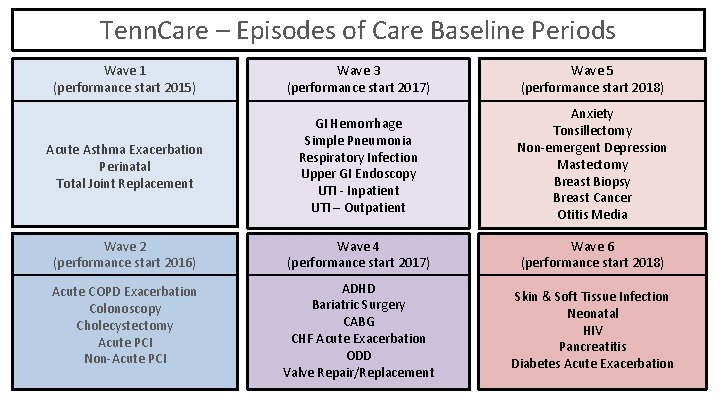
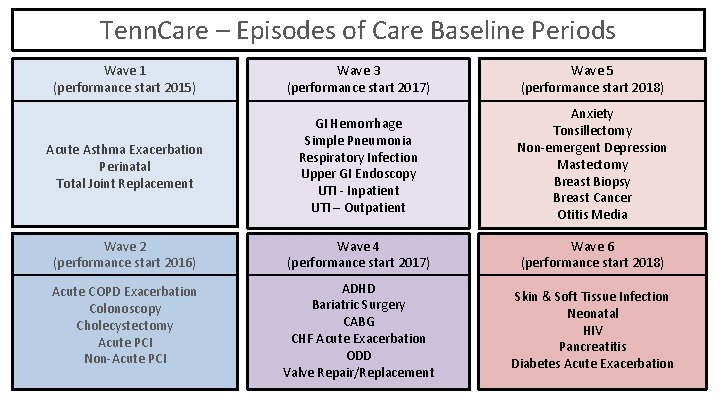
Tenn. Care – Episodes of Care Baseline Periods Wave 1 (performance start 2015) Wave 3 (performance start 2017) Wave 5 (performance start 2018) Acute Asthma Exacerbation Perinatal Total Joint Replacement GI Hemorrhage Simple Pneumonia Respiratory Infection Upper GI Endoscopy UTI - Inpatient UTI – Outpatient Anxiety Tonsillectomy Non-emergent Depression Mastectomy Breast Biopsy Breast Cancer Otitis Media Wave 2 (performance start 2016) Wave 4 (performance start 2017) Wave 6 (performance start 2018) Acute COPD Exacerbation Colonoscopy Cholecystectomy Acute PCI Non-Acute PCI ADHD Bariatric Surgery CABG CHF Acute Exacerbation ODD Valve Repair/Replacement Skin & Soft Tissue Infection Neonatal HIV Pancreatitis Diabetes Acute Exacerbation
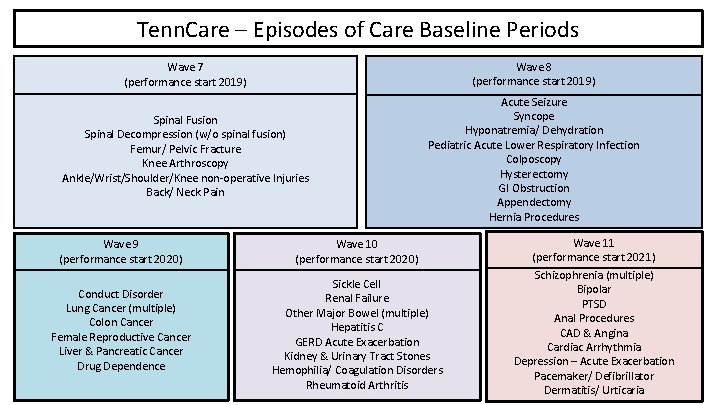
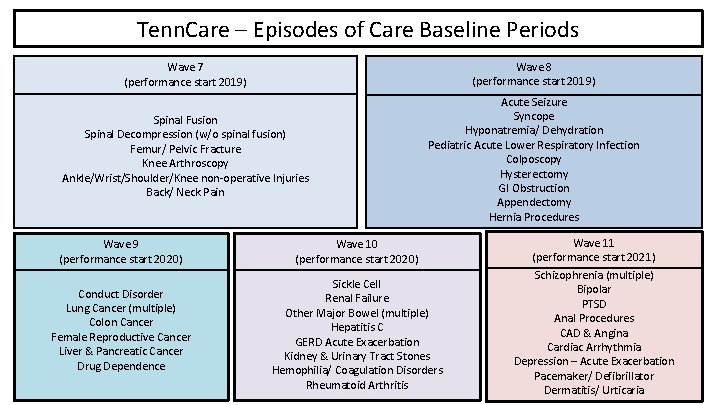
Tenn. Care – Episodes of Care Baseline Periods Wave 7 (performance start 2019) Wave 8 (performance start 2019) Spinal Fusion Spinal Decompression (w/o spinal fusion) Femur/ Pelvic Fracture Knee Arthroscopy Ankle/Wrist/Shoulder/Knee non-operative Injuries Back/ Neck Pain Acute Seizure Syncope Hyponatremia/ Dehydration Pediatric Acute Lower Respiratory Infection Colposcopy Hysterectomy GI Obstruction Appendectomy Hernia Procedures Wave 9 (performance start 2020) Wave 10 (performance start 2020) Wave 11 (performance start 2021) Conduct Disorder Lung Cancer (multiple) Colon Cancer Female Reproductive Cancer Liver & Pancreatic Cancer Drug Dependence Sickle Cell Renal Failure Other Major Bowel (multiple) Hepatitis C GERD Acute Exacerbation Kidney & Urinary Tract Stones Hemophilia/ Coagulation Disorders Rheumatoid Arthritis Schizophrenia (multiple) Bipolar PTSD Anal Procedures CAD & Angina Cardiac Arrhythmia Depression – Acute Exacerbation Pacemaker/ Defibrillator Dermatitis/ Urticaria
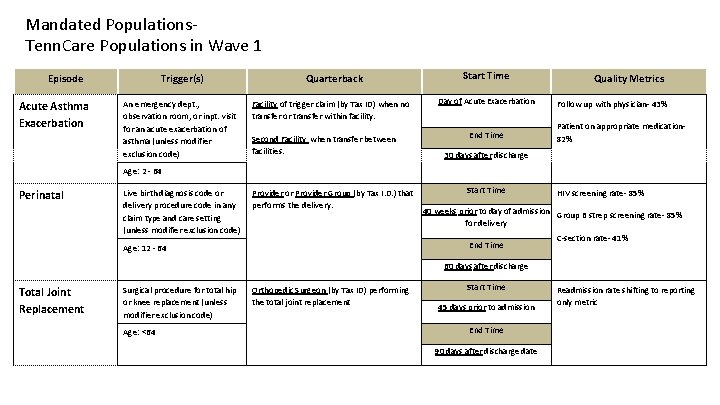
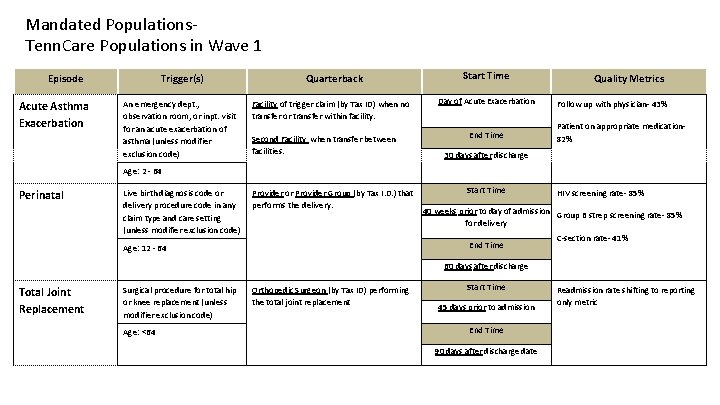
Mandated Populations. Tenn. Care Populations in Wave 1 Episode Acute Asthma Exacerbation Trigger(s) An emergency dept. , observation room, or inpt. visit for an acute exacerbation of asthma (unless modifier exclusion code) Quarterback Facility of trigger claim (by Tax ID) when no transfer or transfer within facility. Second Facility when transfer between facilities. Start Time Day of Acute Exacerbation End Time Quality Metrics Follow up with physician- 43% Patient on appropriate medication 82% 30 days after discharge Age: 2 - 64 Perinatal Live birth diagnosis code or delivery procedure code in any claim type and care setting (unless modifier exclusion code) Provider or Provider Group (by Tax I. D. ) that performs the delivery. Start Time 40 weeks prior to day of admission Group B strep screening rate- 85% for delivery End Time Age: 12 - 64 HIV screening rate- 85% C-section rate- 41% 60 days after discharge Total Joint Replacement Surgical procedure for total hip or knee replacement (unless modifier exclusion code) Age: <64 Orthopedic Surgeon (by Tax ID) performing the total joint replacement Start Time 45 days prior to admission End Time 90 days after discharge date Readmission rate shifting to reporting only metric
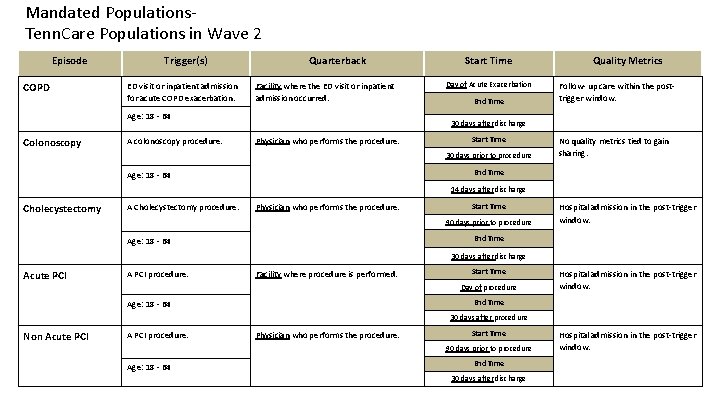
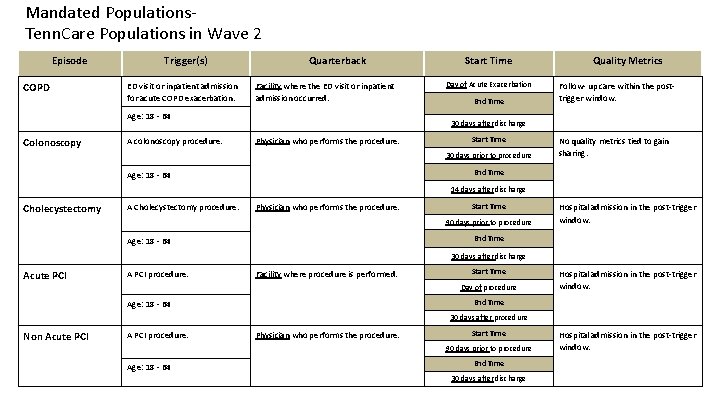
Mandated Populations. Tenn. Care Populations in Wave 2 Episode COPD Trigger(s) ED visit or inpatient admission for acute COPD exacerbation. Quarterback Facility where the ED visit or inpatient admission occurred. Age: 18 - 64 Colonoscopy A colonoscopy procedure. Start Time Day of Acute Exacerbation End Time Quality Metrics Follow- up care within the posttrigger window. 30 days after discharge Physician who performs the procedure. Start Time 30 days prior to procedure No quality metrics tied to gain sharing. End Time Age: 18 - 64 14 days after discharge Cholecystectomy A Cholecystectomy procedure. Physician who performs the procedure. Start Time 90 days prior to procedure Hospital admission in the post-trigger window. End Time Age: 18 - 64 30 days after discharge Acute PCI A PCI procedure. Facility where procedure is performed. Start Time Day of procedure Hospital admission in the post-trigger window. End Time Age: 18 - 64 30 days after procedure Non Acute PCI A PCI procedure. Physician who performs the procedure. Start Time 90 days prior to procedure Age: 18 - 64 End Time 30 days after discharge Hospital admission in the post-trigger window.
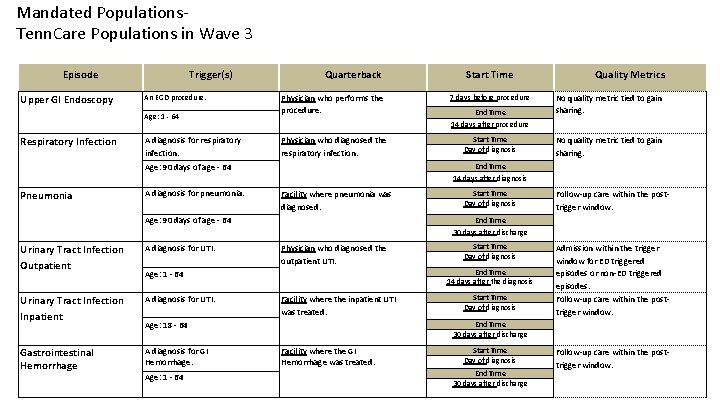
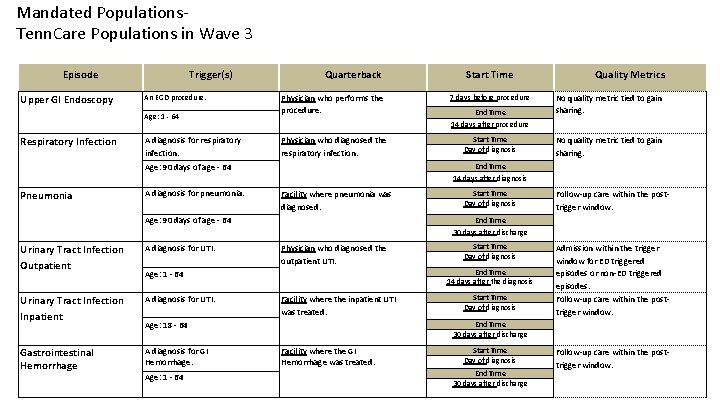
Mandated Populations. Tenn. Care Populations in Wave 3 Episode Upper GI Endoscopy Trigger(s) An EGD procedure. Age: 1 - 64 Respiratory Infection A diagnosis for respiratory infection. Quarterback Physician who performs the procedure. 7 days before procedure Physician who diagnosed the respiratory infection. Start Time Day of diagnosis A diagnosis for pneumonia. Facility where pneumonia was diagnosed. Age: 90 days of age - 64 Urinary Tract Infection Outpatient A diagnosis for UTI. Urinary Tract Infection Inpatient A diagnosis for UTI. Gastrointestinal Hemorrhage A diagnosis for GI Hemorrhage. No quality metric tied to gain sharing. Start Time Day of diagnosis Follow-up care within the posttrigger window. End Time 30 days after discharge Physician who diagnosed the outpatient UTI. Start Time Day of diagnosis End Time 14 days after the diagnosis Age: 1 - 64 Facility where the inpatient UTI was treated. Age: 18 - 64 Age: 1 - 64 End Time 14 days after procedure Quality Metrics End Time 14 days after diagnosis Age: 90 days of age - 64 Pneumonia Start Time Day of diagnosis Admission within the trigger window for ED triggered episodes or non-ED triggered episodes. Follow-up care within the posttrigger window. End Time 30 days after discharge Facility where the GI Hemorrhage was treated. Start Time Day of diagnosis End Time 30 days after discharge Follow-up care within the posttrigger window.
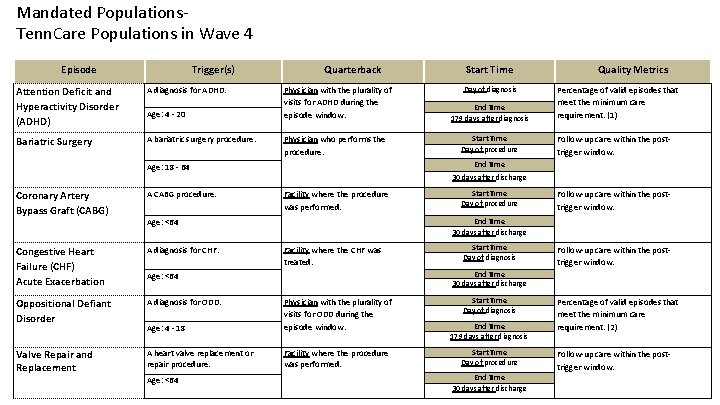
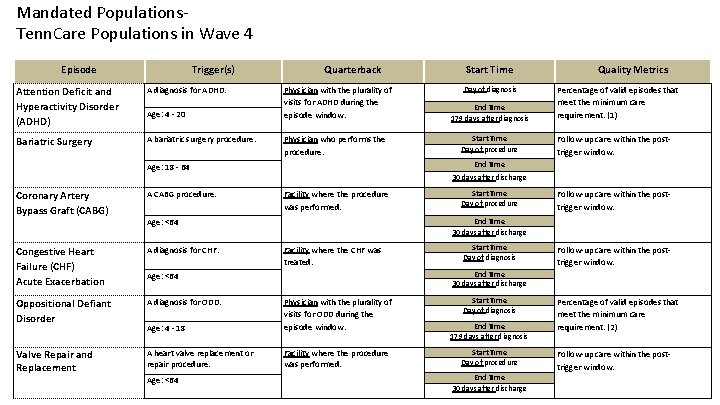
Mandated Populations. Tenn. Care Populations in Wave 4 Episode Trigger(s) Attention Deficit and Hyperactivity Disorder (ADHD) A diagnosis for ADHD. Bariatric Surgery A bariatric surgery procedure. Age: 4 - 20 Quarterback Physician with the plurality of visits for ADHD during the episode window. Physician who performs the procedure. Day of diagnosis End Time 179 days after diagnosis Start Time Day of procedure Quality Metrics Percentage of valid episodes that meet the minimum care requirement. (1) Follow-up care within the posttrigger window. End Time Age: 18 - 64 30 days after discharge Coronary Artery Bypass Graft (CABG) A CABG procedure. Facility where the procedure was performed. Congestive Heart Failure (CHF) Acute Exacerbation A diagnosis for CHF. Oppositional Defiant Disorder A diagnosis for ODD. Age: 4 - 18 Physician with the plurality of visits for ODD during the episode window. Valve Repair and Replacement A heart valve replacement or repair procedure. Facility where the procedure was performed. Start Time Day of procedure Follow-up care within the posttrigger window. End Time 30 days after discharge Age: <64 Facility where the CHF was treated. Start Time Day of diagnosis Follow-up care within the posttrigger window. End Time 30 days after discharge Age: <64 Start Time Day of diagnosis End Time 179 days after diagnosis Start Time Day of procedure End Time 30 days after discharge Percentage of valid episodes that meet the minimum care requirement. (2) Follow-up care within the posttrigger window.
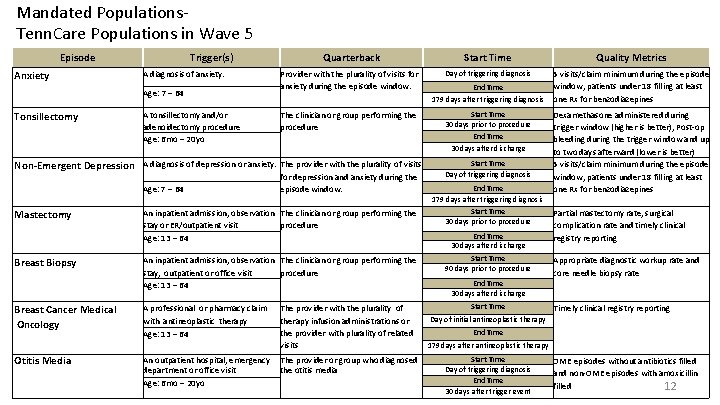
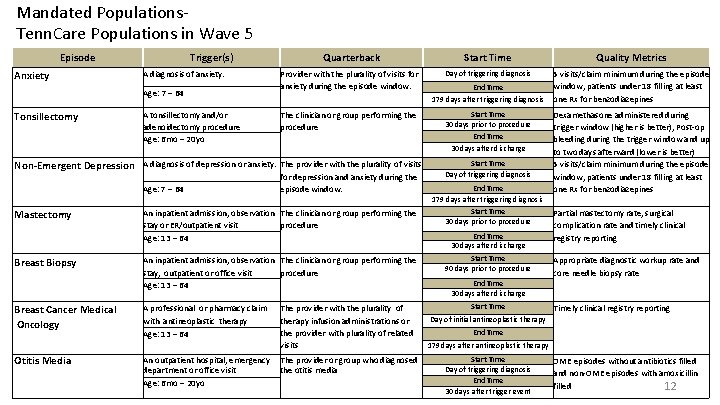
Mandated Populations. Tenn. Care Populations in Wave 5 Episode Anxiety Trigger(s) A diagnosis of anxiety. Age: 7 – 64 Tonsillectomy A tonsillectomy and/or adenoidectomy procedure Age: 6 mo – 20 yo Quarterback Start Time Quality Metrics Provider with the plurality of visits for anxiety during the episode window. Day of triggering diagnosis 5 visits/claim minimum during the episode window, patients under 18 filling at least one Rx for benzodiazepines The clinician or group performing the procedure Non-Emergent Depression A diagnosis of depression or anxiety. The provider with the plurality of visits Age: 7 – 64 Mastectomy Breast Biopsy Breast Cancer Medical Oncology Otitis Media for depression and anxiety during the episode window. An inpatient admission, observation The clinician or group performing the stay or ER/outpatient visit procedure Age: 13 – 64 An inpatient admission, observation The clinician or group performing the stay, outpatient or office visit procedure Age: 13 – 64 A professional or pharmacy claim with antineoplastic therapy Age: 13 – 64 An outpatient hospital, emergency department or office visit Age: 6 mo – 20 yo The provider with the plurality of therapy infusion administrations or the provider with plurality of related visits The provider or group who diagnosed the otitis media End Time 179 days after triggering diagnosis Start Time 30 days prior to procedure End Time 30 days after discharge Start Time Day of triggering diagnosis End Time 179 days after triggering diagnosis Start Time 30 days prior to procedure End Time 30 days after discharge Start Time 90 days prior to procedure Dexamethasone administered during trigger window (higher is better), Post-op bleeding during the trigger window and up to two days afterward (lower is better) 5 visits/claim minimum during the episode window, patients under 18 filling at least one Rx for benzodiazepines Partial mastectomy rate, surgical complication rate and timely clinical registry reporting Appropriate diagnostic workup rate and core needle biopsy rate End Time 30 days after discharge Start Timely clinical registry reporting Day of initial antineoplastic therapy End Time 179 days after antineoplastic therapy Start Time Day of triggering diagnosis End Time 30 days after trigger event OME episodes without antibiotics filled and non-OME episodes with amoxicillin filled 12
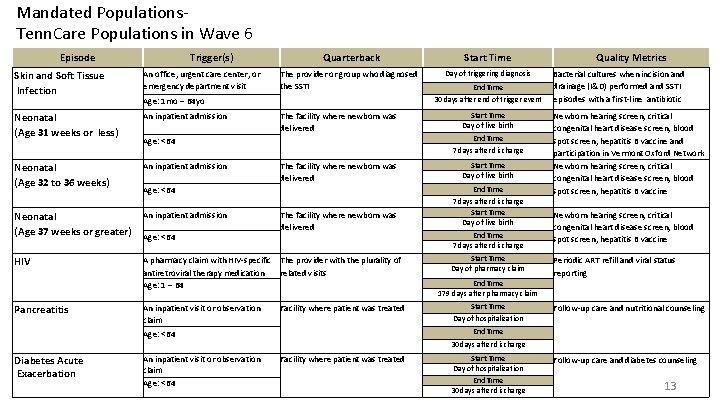
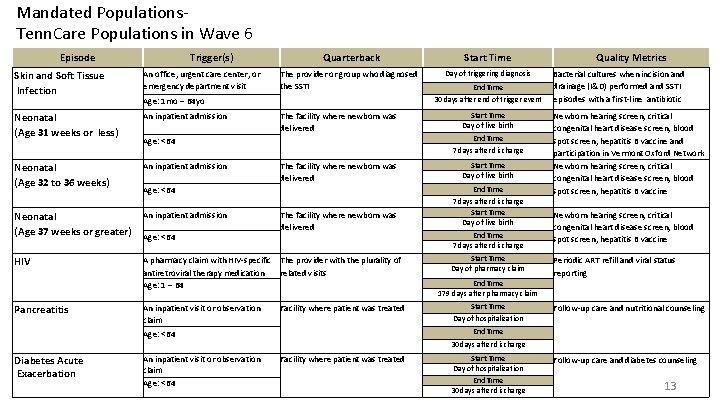
Mandated Populations. Tenn. Care Populations in Wave 6 Episode Trigger(s) Quarterback Skin and Soft Tissue Infection An office, urgent care center, or emergency department visit Neonatal (Age 31 weeks or less) An inpatient admission Neonatal (Age 32 to 36 weeks) An inpatient admission Neonatal (Age 37 weeks or greater) An inpatient admission HIV A pharmacy claim with HIV-specific The provider with the plurality of antiretroviral therapy medication related visits Age: 1 – 64 Pancreatitis The provider or group who diagnosed the SSTI Age: 1 mo – 64 yo The facility where newborn was delivered Age: <64 An inpatient visit or observation claim Age: <64 The facility where newborn was delivered Facility where patient was treated Start Time Day of triggering diagnosis End Time 30 days after end of trigger event Start Time Day of live birth End Time 7 days after discharge Start Time Day of pharmacy claim Quality Metrics Bacterial cultures when incision and drainage (I&D) performed and SSTI episodes with a first-line antibiotic Newborn hearing screen, critical congenital heart disease screen, blood spot screen, hepatitis B vaccine and participation in Vermont Oxford Network Newborn hearing screen, critical congenital heart disease screen, blood spot screen, hepatitis B vaccine Periodic ART refill and viral status reporting End Time 179 days after pharmacy claim Start Time Follow-up care and nutritional counseling Day of hospitalization End Time 30 days after discharge Diabetes Acute Exacerbation An inpatient visit or observation claim Age: <64 Facility where patient was treated Start Time Day of hospitalization End Time 30 days after discharge Follow-up care and diabetes counseling 13
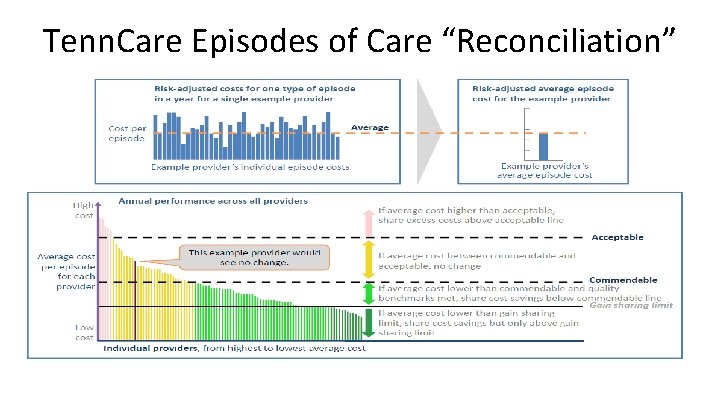
Tenn. Care Episodes of Care “Reconciliation”
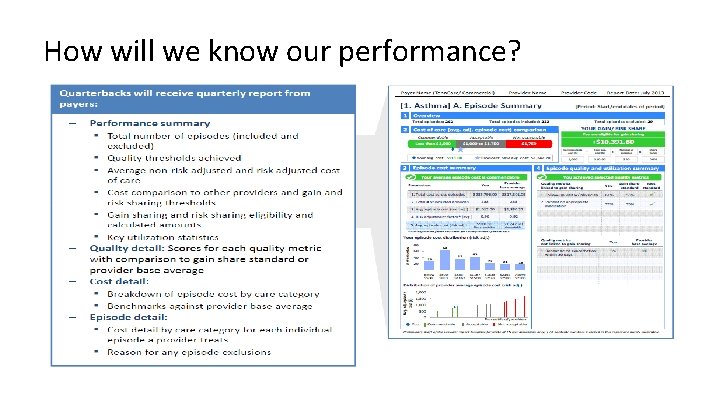
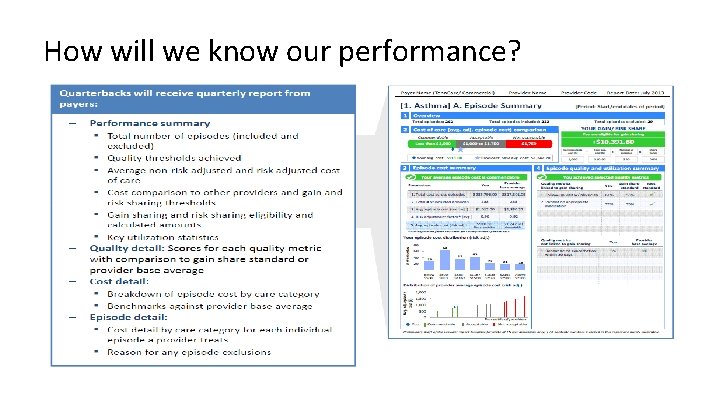
How will we know our performance?
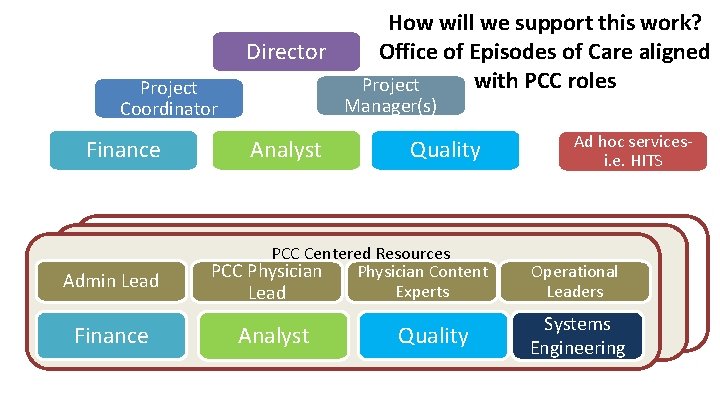
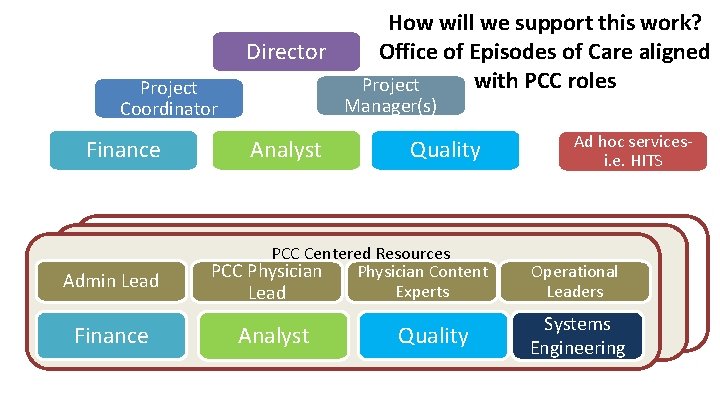
Director Project Coordinator Finance Admin Lead Finance How will we support this work? Office of Episodes of Care aligned with PCC roles Project Manager(s) Analyst Quality PCC Centered Resources PCC Physician Content Experts Lead Analyst Quality Ad hoc servicesi. e. HITS Operational Leaders Systems Engineering
 Tenn. code ann. § 67-4-708(3)(c)(i-xvi)
Tenn. code ann. § 67-4-708(3)(c)(i-xvi) Tenn. code ann. § 67-4-708(3)(c)(i-xvi)
Tenn. code ann. § 67-4-708(3)(c)(i-xvi) Tenn lys et lys skal brenne
Tenn lys et lys skal brenne Steps in market segmentation targeting and positioning
Steps in market segmentation targeting and positioning Market leader challenger follower nicher examples
Market leader challenger follower nicher examples Parallel episodes
Parallel episodes Social episodes are
Social episodes are Jonathan schultz jenny jones
Jonathan schultz jenny jones Quavers marvellous world of music theme song
Quavers marvellous world of music theme song Anorexia vs bulimia usmle
Anorexia vs bulimia usmle Parade's end episodes
Parade's end episodes The daily episodes from
The daily episodes from Genic balance theory in drosophila
Genic balance theory in drosophila Symbols in the kite runner
Symbols in the kite runner Big bang theory episodes
Big bang theory episodes Severe episodes of spasmodic choking
Severe episodes of spasmodic choking Algernon definition
Algernon definition