Engaging Patients and Families to Improve Care Transitions


- Slides: 25
Engaging Patients and Families to Improve Care Transitions 1
Objective for the Session Discuss strategies for partnering with patients and families to improve their experience of discharge from the hospital and coordination of post-acute care.

Background: BIDMC’s Readmission Rates Publically Available Medicare Data:
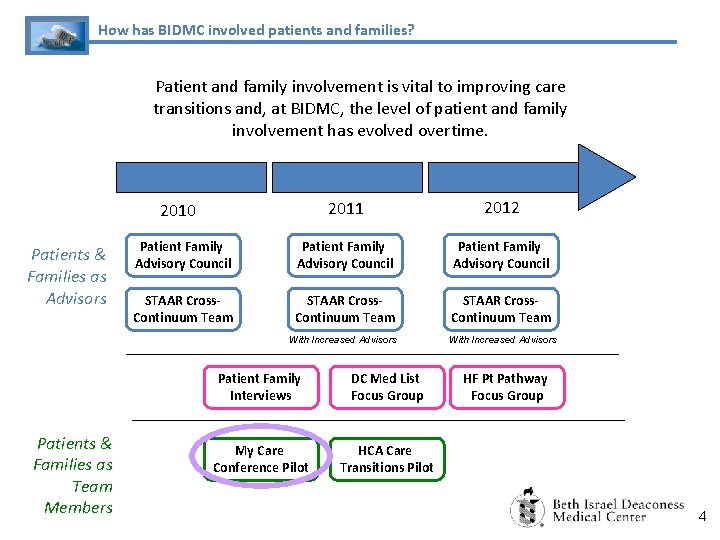
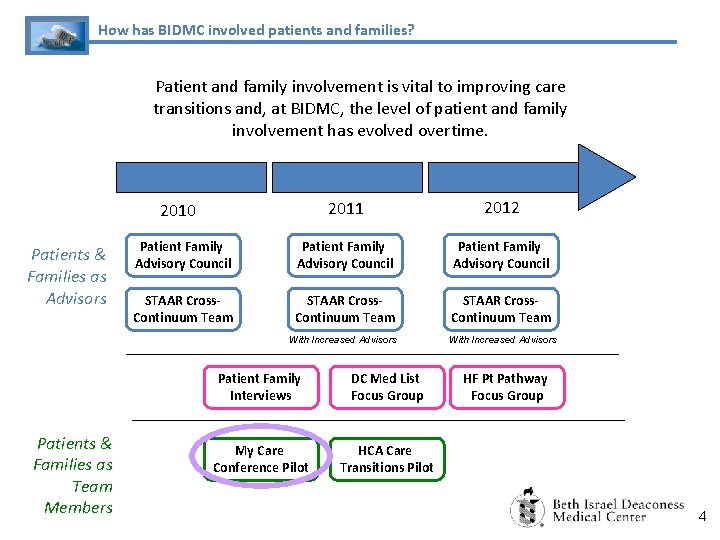
How has BIDMC involved patients and families? Patient and family involvement is vital to improving care transitions and, at BIDMC, the level of patient and family involvement has evolved overtime. 2011 2012 Patient Family Advisory Council STAAR Cross. Continuum Team With Increased Advisors 2010 Patients & Families as Advisors Patients & Families as Team Members Patient Family Interviews DC Med List Focus Group My Care Conference Pilot HCA Care Transitions Pilot HF Pt Pathway Focus Group 4
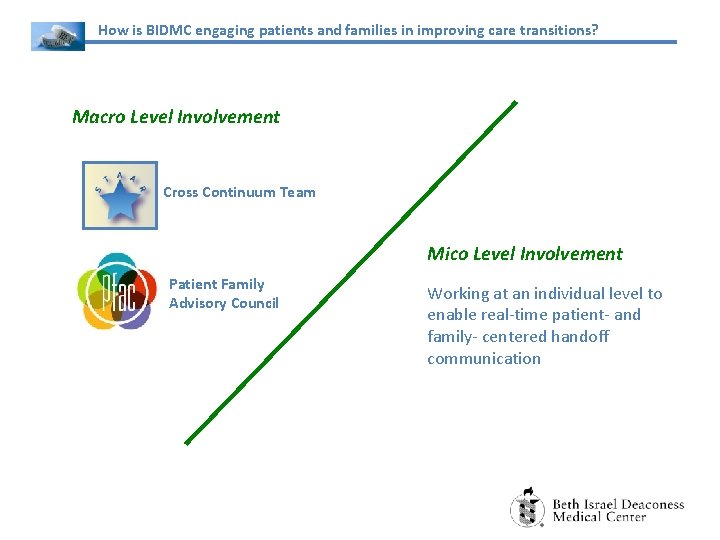
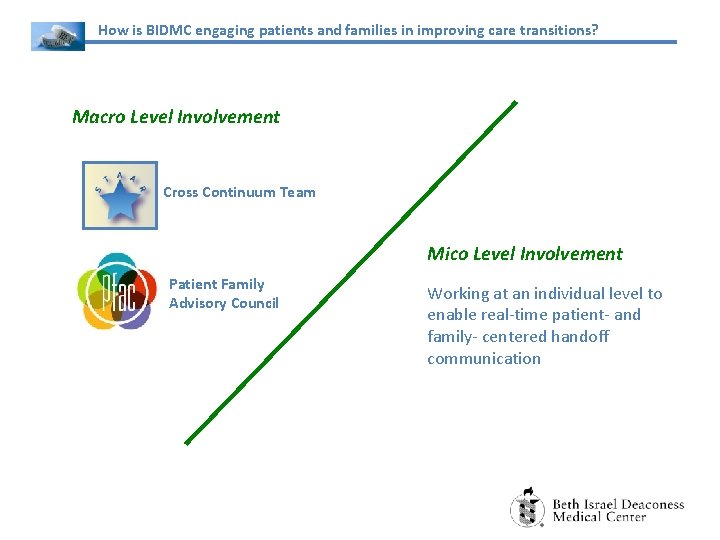
How is BIDMC engaging patients and families in improving care transitions? Macro Level Involvement Cross Continuum Team Mico Level Involvement Patient Family Advisory Council Working at an individual level to enable real-time patient- and family- centered handoff communication
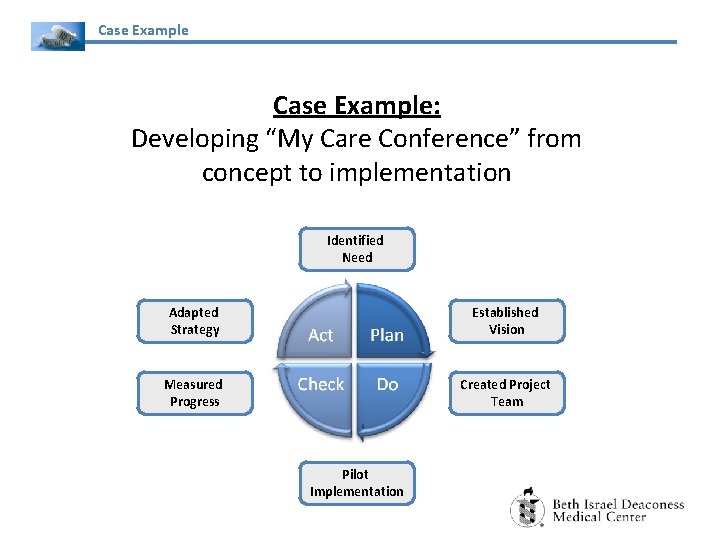
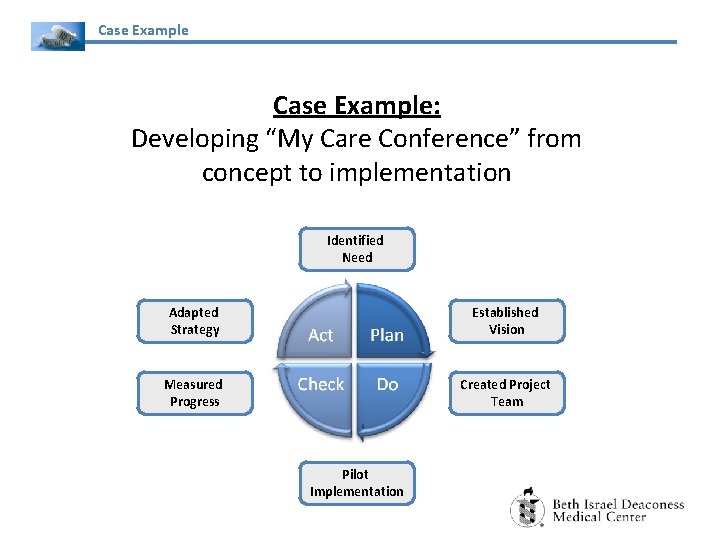
Case Example: Developing “My Care Conference” from concept to implementation Identified Need Adapted Strategy Established Vision Measured Progress Created Project Team Pilot Implementation
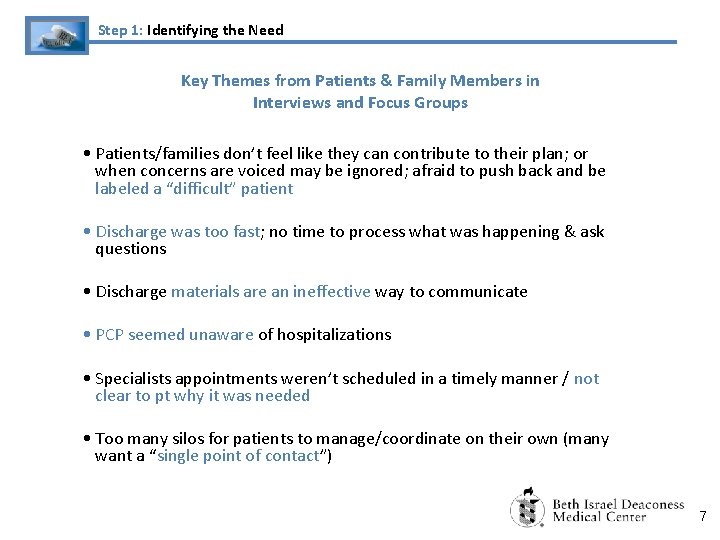
Step 1: Identifying the Need Key Themes from Patients & Family Members in Interviews and Focus Groups • Patients/families don’t feel like they can contribute to their plan; or when concerns are voiced may be ignored; afraid to push back and be labeled a “difficult” patient • Discharge was too fast; no time to process what was happening & ask questions • Discharge materials are an ineffective way to communicate • PCP seemed unaware of hospitalizations • Specialists appointments weren’t scheduled in a timely manner / not clear to pt why it was needed • Too many silos for patients to manage/coordinate on their own (many want a “single point of contact”) 7
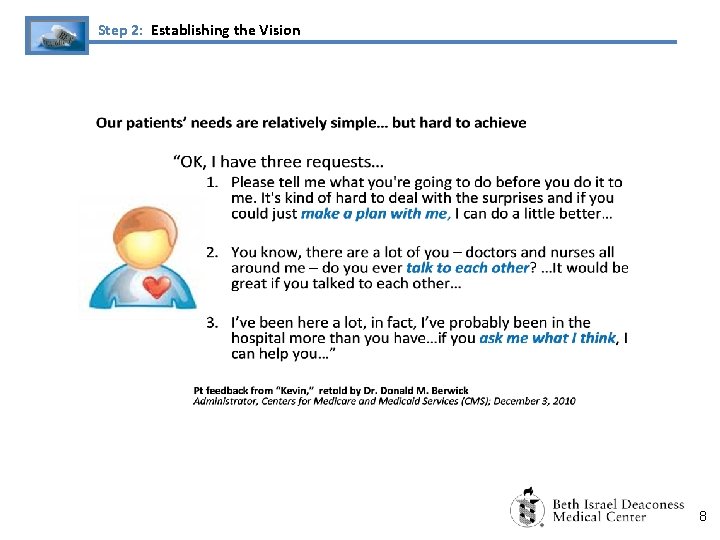
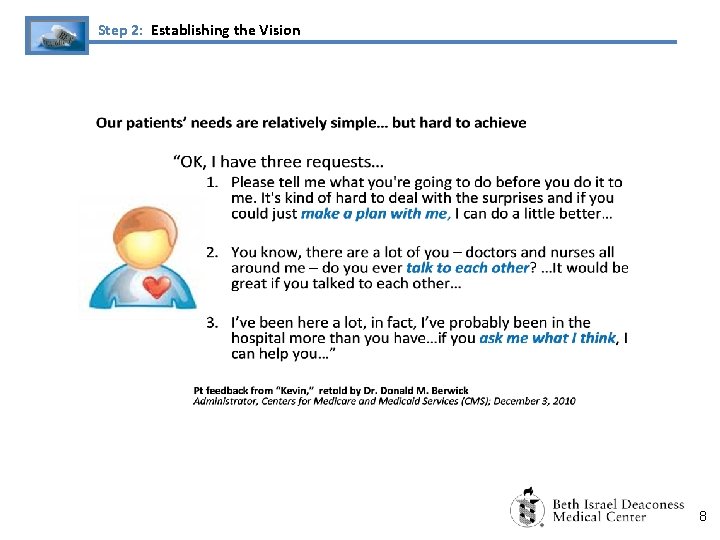
Step 2: Establishing the Vision 8
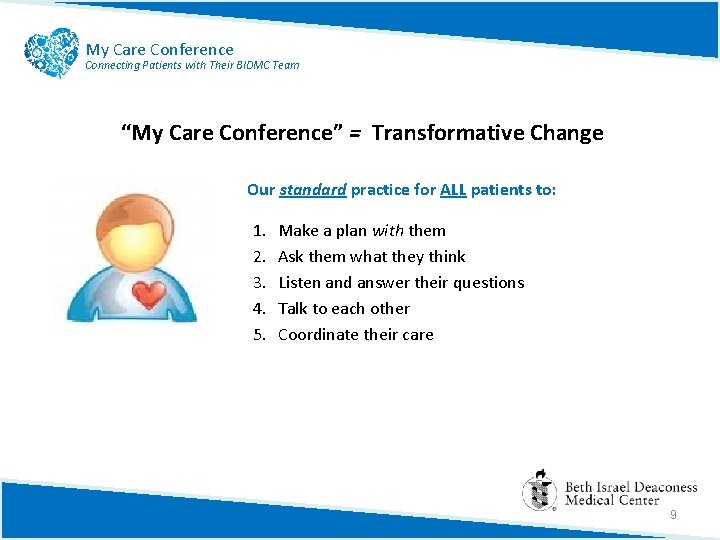
My Care Conference Connecting Patients with Their BIDMC Team “My Care Conference” = Transformative Change Our standard practice for ALL patients to: 1. 2. 3. 4. 5. Make a plan with them Ask them what they think Listen and answer their questions Talk to each other Coordinate their care 9
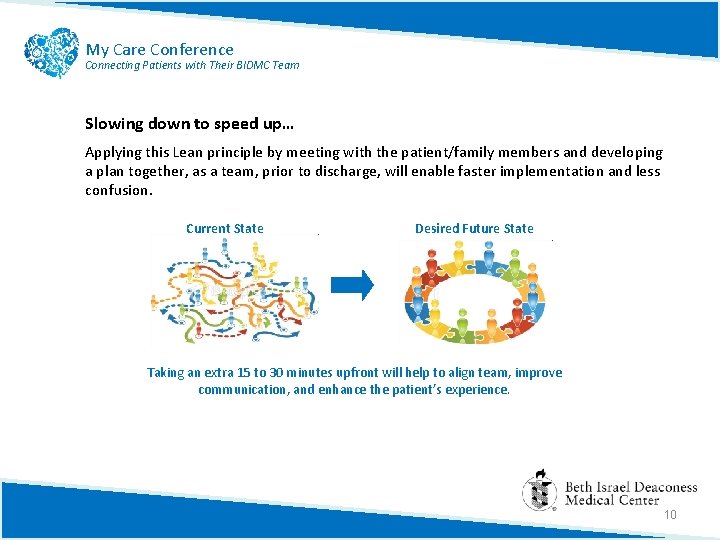
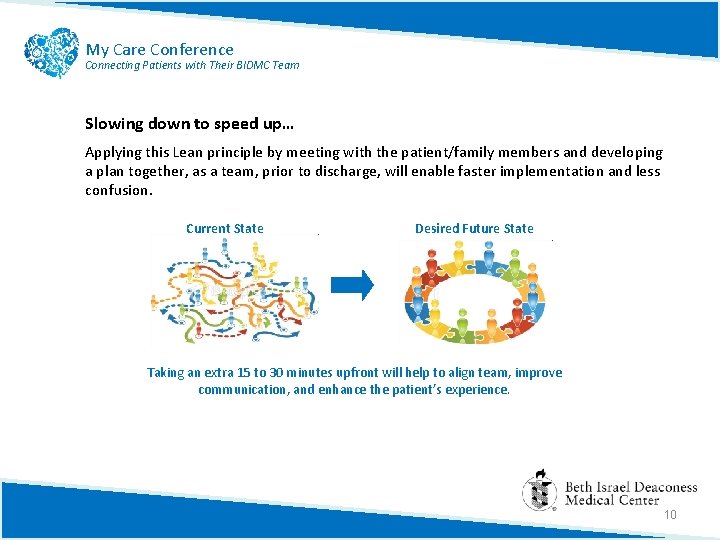
My Care Conference Connecting Patients with Their BIDMC Team Slowing down to speed up… Applying this Lean principle by meeting with the patient/family members and developing a plan together, as a team, prior to discharge, will enable faster implementation and less confusion. Current State Desired Future State Taking an extra 15 to 30 minutes upfront will help to align team, improve communication, and enhance the patient’s experience. 10
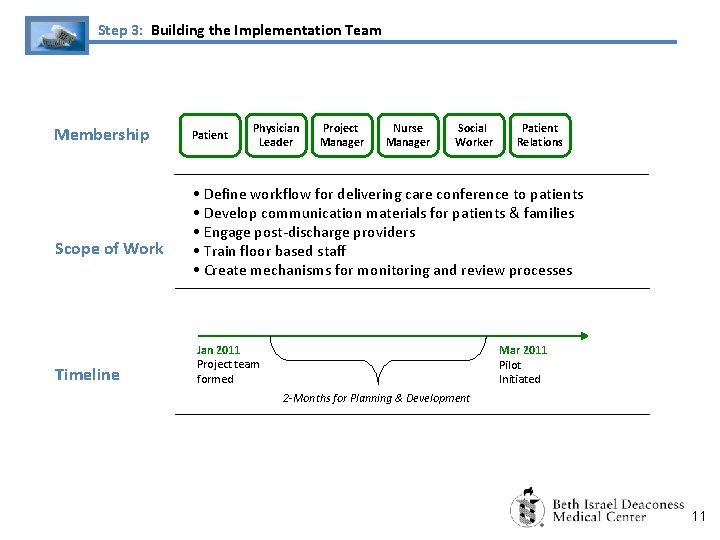
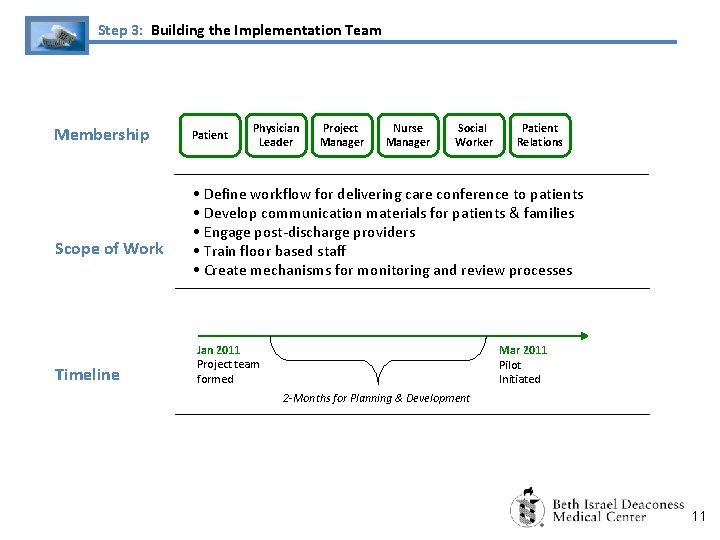
Step 3: Building the Implementation Team Membership Scope of Work Timeline Patient Physician Leader Project Manager Nurse Manager Social Worker Patient Relations • Define workflow for delivering care conference to patients • Develop communication materials for patients & families • Engage post-discharge providers • Train floor based staff • Create mechanisms for monitoring and review processes Jan 2011 Project team formed Mar 2011 Pilot Initiated 2 -Months for Planning & Development 11
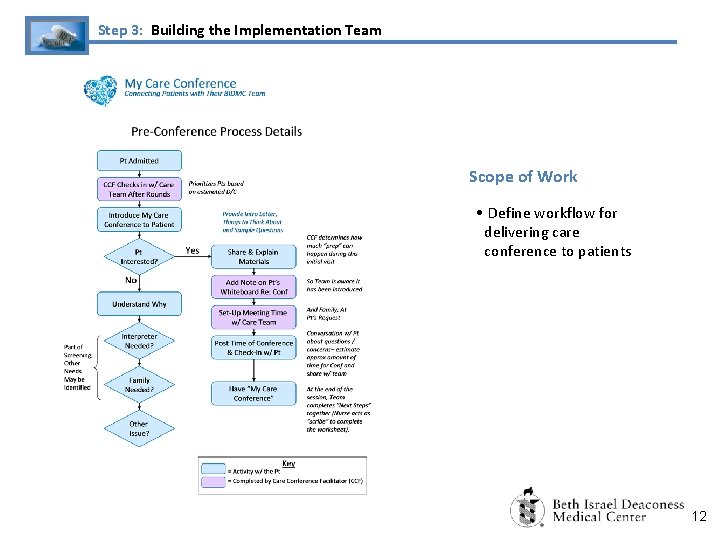
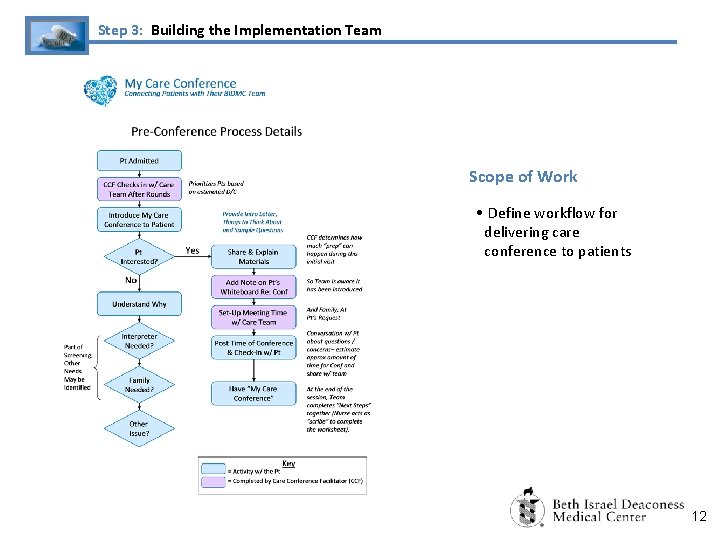
Step 3: Building the Implementation Team Scope of Work • Define workflow for delivering care conference to patients 12
My Care Conference Connecting Patients with Their BIDMC Team Making It Happen: Care Conference Facilitator A new role to help bring all the key participants together • Checks in with newly admitted patients to introduce “My Care Conference” • Identifies potential times for the conference, and coordinates with the patient, family members and BIDMC Team Care Conference Facilitator • Helps patient prepare questions and identify objectives for the conference • Facilitates the conference session to help patient achieve his/her objectives 13
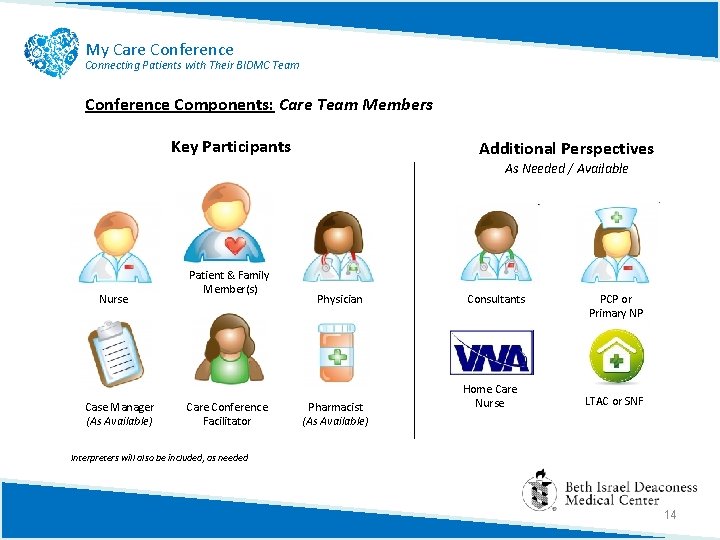
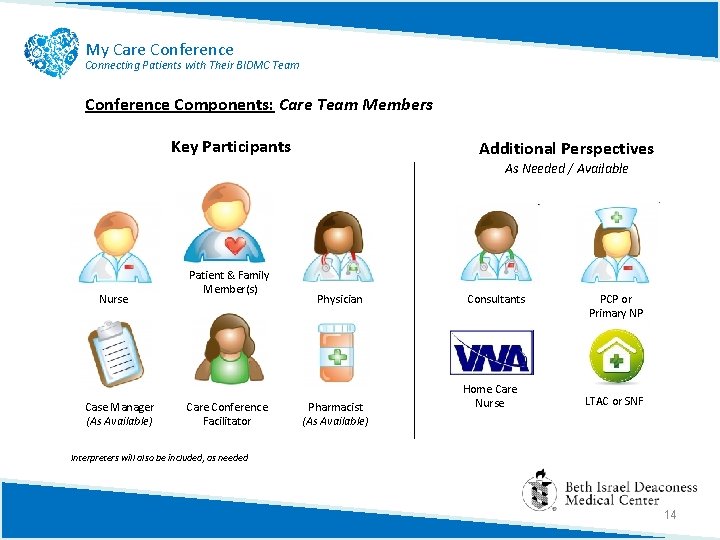
My Care Conference Connecting Patients with Their BIDMC Team Conference Components: Care Team Members Key Participants Additional Perspectives As Needed / Available Nurse Case Manager (As Available) Patient & Family Member(s) Care Conference Facilitator Physician Pharmacist (As Available) Consultants Home Care Nurse PCP or Primary NP LTAC or SNF Interpreters will also be included, as needed 14

My Care Conference Connecting Patients with Their BIDMC Team Conference Components: Environment of Care To foster dignity and respect Location Ideally, the conference would occur outside the patient’s room in a dedicated family meeting space. 15
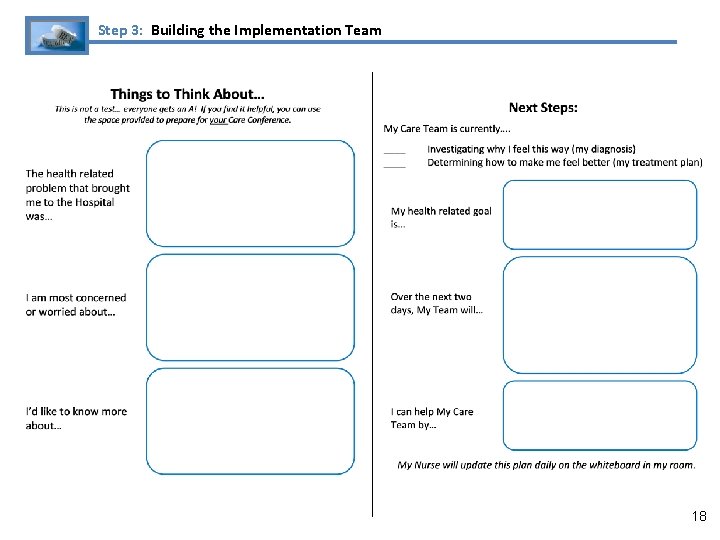
My Care Conference Connecting Patients with Their BIDMC Team Conference Components: Post Meeting Follow-Up Develop a standard planning document for the Patient and the Care Team to complete during the conference • All participants will leave the conference with a copy of the plan • Care Conference Facilitator will use a template to document the meeting and include a copy of the plan in OMR 16
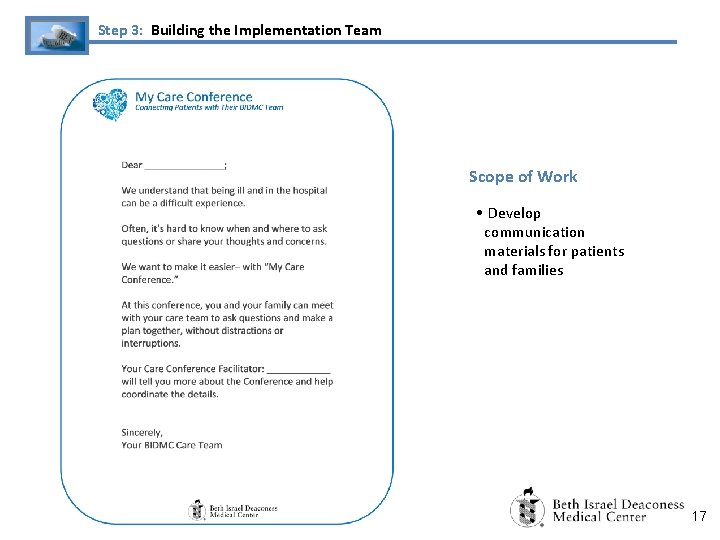
Step 3: Building the Implementation Team Scope of Work • Develop communication materials for patients and families 17
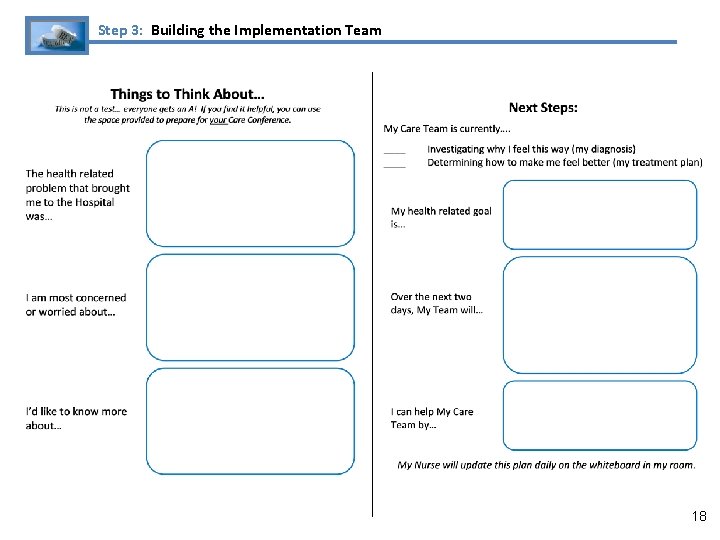
Step 3: Building the Implementation Team 18
My Care Conference Connecting Patients with Their BIDMC Team Pilot: Outcome Measures to Monitor (Quarterly) Primary Metrics: Patient Satisfaction Scores: • The hypothesis is that this drastically different intervention will enable us to better meet inpatients’ needs, and show a consistent improvement in H-CAHPS scores for the floor (when compared to Farr 2 or CC 7). Secondary Metrics: Operational Efficiencies: • • • Increased coordination will potentially decrease wasted or duplicated effort (measured through work sampling) Planning with the patient from the first day of their visit will help the Team better understand the goals of care and decrease length of stay or improve discharge times Ultimately, over the long term, this strategy may improve transitions in care and reduce readmissions. Staff Satisfaction: • Although this intervention will require a time commitment from the Care Team, it will enable staff to more effectively connect with their patients, potentially increasing staff satisfaction. 19
Step 4: Pilot Implementation & Learning / Adaptation Challenges Observed at 3 -Months - Staff still perceive Care Conferences as only for the most complex patients - Because conferences have been held primarily for highly complex patients, they typically last longer than the estimated 20 minutes - Time staff is available doesn’t correlate with when family members can easily attend - Patients sometimes decline– they don’t want to disrupt their busy doctors 20
Step 4: Pilot Implementation & Learning / Adaptation Questions Presented to PFAC 1) Timing: Based on your perspective, when during a patient’s stay would this type of conference be most beneficial? 2) Participation: Some patients have expressed a reluctance to participate in the conferences, how can we better present this option to them? 3) Triggers: Are there any factors that should automatically "trigger" a Care Conference? 21
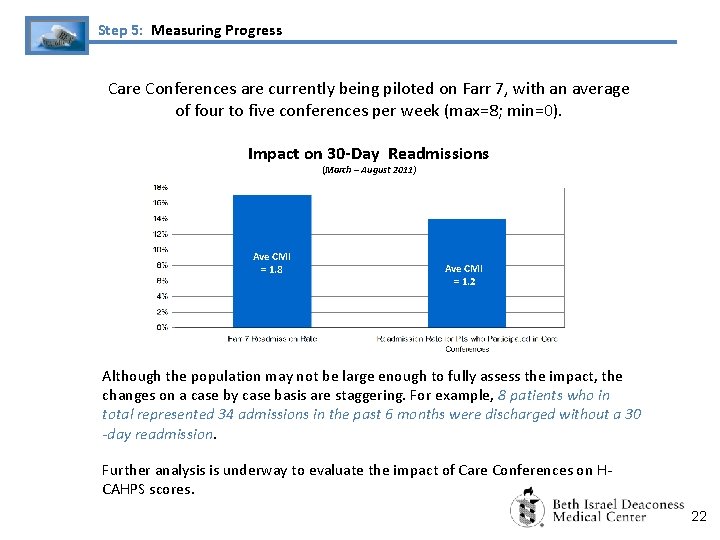
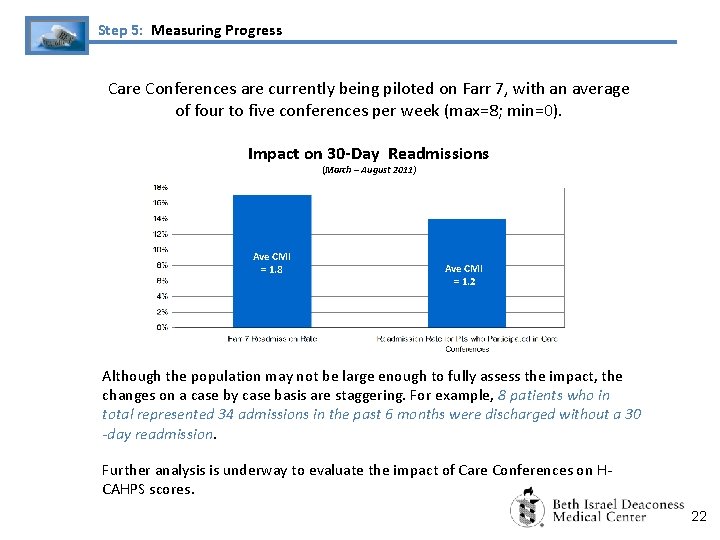
Step 5: Measuring Progress Care Conferences are currently being piloted on Farr 7, with an average of four to five conferences per week (max=8; min=0). Impact on 30 -Day Readmissions (March – August 2011) Ave CMI = 1. 8 Ave CMI = 1. 2 Although the population may not be large enough to fully assess the impact, the changes on a case by case basis are staggering. For example, 8 patients who in total represented 34 admissions in the past 6 months were discharged without a 30 -day readmission. Further analysis is underway to evaluate the impact of Care Conferences on HCAHPS scores. 22
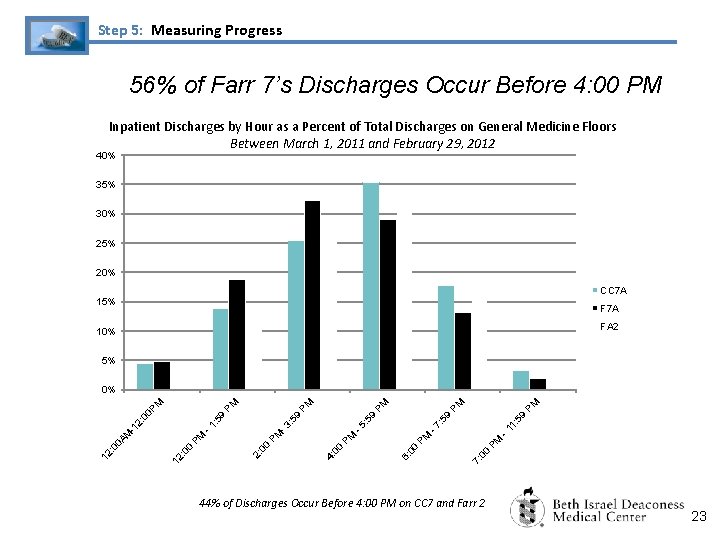
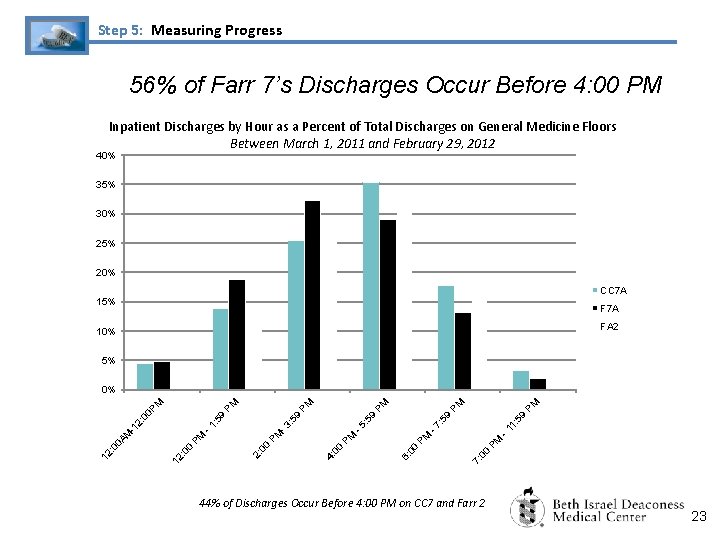
Step 5: Measuring Progress 56% of Farr 7’s Discharges Occur Before 4: 00 PM Inpatient Discharges by Hour as a Percent of Total Discharges on General Medicine Floors Between March 1, 2011 and February 29, 2012 40% 35% 30% 25% 20% CC 7 A 15% F 7 A FA 2 10% 5% PM -1 1: : 5 9 7: 0 0 PM -7 6: 00 PM PM 00 4: 59 PM PM -5 -3 PM 2: 0 0 PM 0 : 0 12 : 5 9 PM : 5 -1 2: -1 M 0 A 12 : 0 : 5 9 9 00 P M PM 0% 44% of Discharges Occur Before 4: 00 PM on CC 7 and Farr 2 23
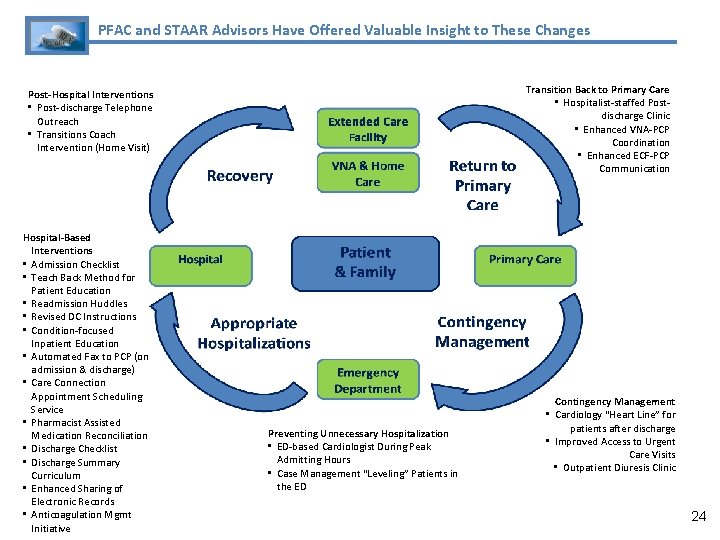
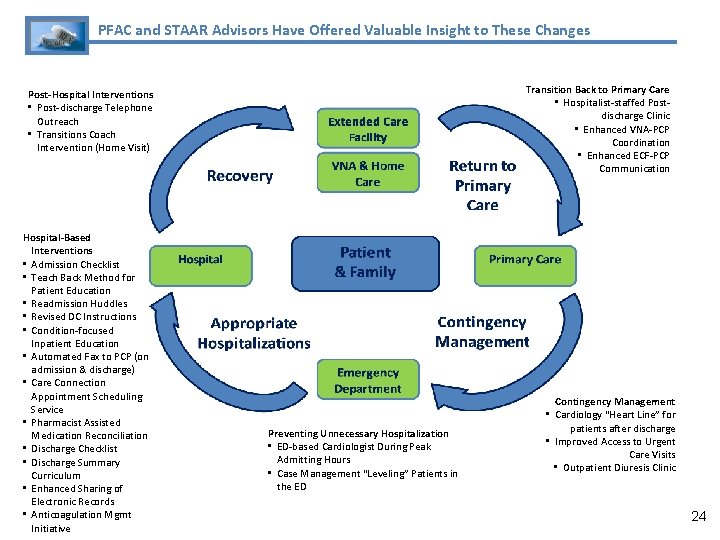
PFAC and STAAR Advisors Have Offered Valuable Insight to These Changes Transition Back to Primary Care • Hospitalist-staffed Postdischarge Clinic • Enhanced VNA-PCP Coordination • Enhanced ECF-PCP Communication Post-Hospital Interventions • Post-discharge Telephone Outreach • Transitions Coach Intervention (Home Visit) Hospital-Based Interventions • Admission Checklist • Teach Back Method for Patient Education • Readmission Huddles • Revised DC Instructions • Condition-focused Inpatient Education • Automated Fax to PCP (on admission & discharge) • Care Connection Appointment Scheduling Service • Pharmacist Assisted Medication Reconciliation • Discharge Checklist • Discharge Summary Curriculum • Enhanced Sharing of Electronic Records • Anticoagulation Mgmt Initiative Preventing Unnecessary Hospitalization • ED-based Cardiologist During Peak Admitting Hours • Case Management “Leveling” Patients in the ED Contingency Management • Cardiology “Heart Line” for patients after discharge • Improved Access to Urgent Care Visits • Outpatient Diuresis Clinic 24
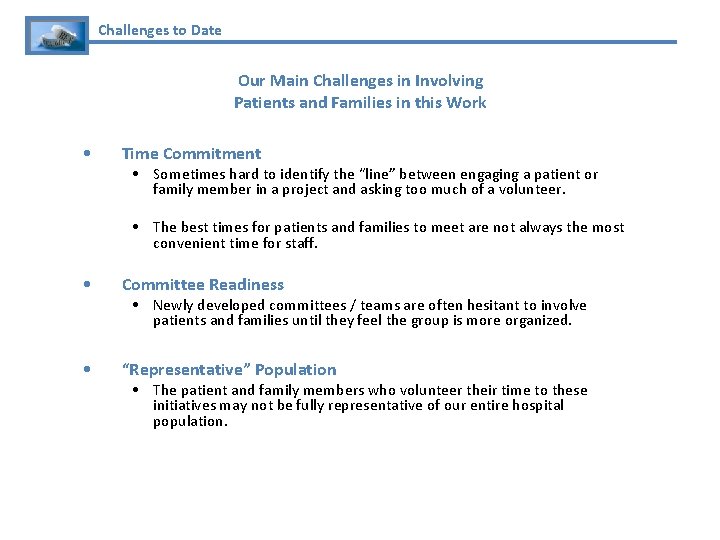
Challenges to Date Our Main Challenges in Involving Patients and Families in this Work • Time Commitment • Sometimes hard to identify the “line” between engaging a patient or family member in a project and asking too much of a volunteer. • The best times for patients and families to meet are not always the most convenient time for staff. • Committee Readiness • “Representative” Population • Newly developed committees / teams are often hesitant to involve patients and families until they feel the group is more organized. • The patient and family members who volunteer their time to these initiatives may not be fully representative of our entire hospital population.
 Big families vs small families
Big families vs small families National transitions of care coalition
National transitions of care coalition Fundal level
Fundal level Dynamisch verbinden
Dynamisch verbinden Marketing involve engaging directly with carefully targeted
Marketing involve engaging directly with carefully targeted Marketing involve engaging directly with carefully targeted
Marketing involve engaging directly with carefully targeted Factors of care patients can expect to receive
Factors of care patients can expect to receive Nursing diagnosis for cataracts
Nursing diagnosis for cataracts Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Nursing care plan for breast cancer ppt
Nursing care plan for breast cancer ppt Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Health care levels primary secondary tertiary
Health care levels primary secondary tertiary Filters and transitions in dhtml
Filters and transitions in dhtml Transitional devices
Transitional devices Unity and coherence شرح
Unity and coherence شرح Windows live movie make
Windows live movie make What holds paper together
What holds paper together Transition thesis statements
Transition thesis statements Elements of script writing
Elements of script writing Modern process transitions in spm
Modern process transitions in spm Transitions for rhetorical analysis
Transitions for rhetorical analysis Melcon transition words
Melcon transition words Mel con format
Mel con format Effects of transitions in early years
Effects of transitions in early years Gregory is my beautiful gray persian cat
Gregory is my beautiful gray persian cat