Documentation Standards 2009 Agenda Goals of documentation training
- Slides: 37
Documentation Standards 2009
Agenda Goals of documentation training Iowa Administrative Code SURS Reviews Questions & answers 2
Documentation Standards Training Goals: To discuss IAC as it pertains to documentation To emphasize compliance with doc standards in relation to SURS review To educate providers about requirements, but not to provide specific documentation wording 3
Iowa Administrative Code http: //www. dhs. state. ia. us/policyanalysis/Policy. M anual. Pages/Manual_Documents/Rules/441 -79. pdf 4
Discussion of 441 - 79. 3(249 A) 5
441 - 79. 3(249 A) Maintenance of records by providers of service Providers shall maintain complete and legible records as required in this rule. Failure to maintain records or to make records available to the department or its representative may result in claim denial or recoupment. 6
Medical (clinical) records 79. 3(2) Medical (clinical) records Provider shall maintain complete and legible medical records for each service Required records will include records required to maintain license in good standing 7
Definition of Medical Records 79. 3(2)a Definition. Medical record means a tangible history that provides evidence of: (1) The provision of each service and each billed to the program activity (2) First and last name of the member receiving service 8
Purpose of Medical Record 79. 3(2)b Purpose The Medical record shall provide evidence that the service provided is: (1) Medically necessary; (2) Consistent with the diagnosis… (3) Consistent with professionally recognized standards of care 9
Components of Medical Records 79. 3(2)c(1 -4) Components (1) Identification (2) Basis for coverage (3) Service documentation (4) Outcome of service Each will be discussed in greater detail in following slides. 10
Medical Records Component #1 - Identification 79. 3(2)c(1) Identification Each page or separate electronic document: - Member’s first and last name Associated within the medical record: - Medical assistance id number - Date of birth 11
Medical Records Component #2– Basis for Service 79. 3(2)c(2) Basis for Service Medical record shall reflect: - the reason for performing the service - substantiate medical necessity - demonstrate level of care 13 Bullets to follow on several slides 12
Basis for Service 1. Complaint, symptoms, and diagnosis 2. Medical or social history 3. Examination finding 4. Diagnostic, lab, X-ray reports 5. Goals or needs identified in Plan of Care 13
Basis for Service 6. Physician orders and required Prior Authorizations 7. Medication & pharmacy records, provider’s orders 8. Professional consultation reports 9. Progress or status notes 14
Basis for Service 10. Forms required by the department as condition of payment 11. Treatment plans, care plans, service plans, etc. 12. Provider’s assessment, clinical impression, etc 13. Any additional documentation to demonstrate medical necessity 15
Medical Records Component #3 –Service Documentation 79. 3(2)c(3) Service documentation Record shall include information necessary to substantiate the provided service. 1. Specific procedures or treatments 2. Complete date of service with begin and end dates 16
Service Documentation 3. Complete time of service with begin and end time (unless time-defined CPT code is used) 4. Location 5. Name, dosage, and route of medication administration 17
Service Documentation 6. Supplies dispensed 7. First name, last name & credential of provider 8. Signature of provider or initials if signature log used 9. 24 -hour care needs documentation, member’s response, provider’s name for each shift 18
Medical Records Component #4 – Outcome of Service 79. 3(2)c(4) Outcome of Service Medical record shall indicate: member’s progress in response to services including: changes in treatment alteration of plan of care revision of diagnosis 19
Basis for Service Requirements 79. 3(2)d Basis for service requirements for specific services New as of 4/1/08 specific requirements for more than 40 provider types Outlines documents needed by provider type for SURS review 20
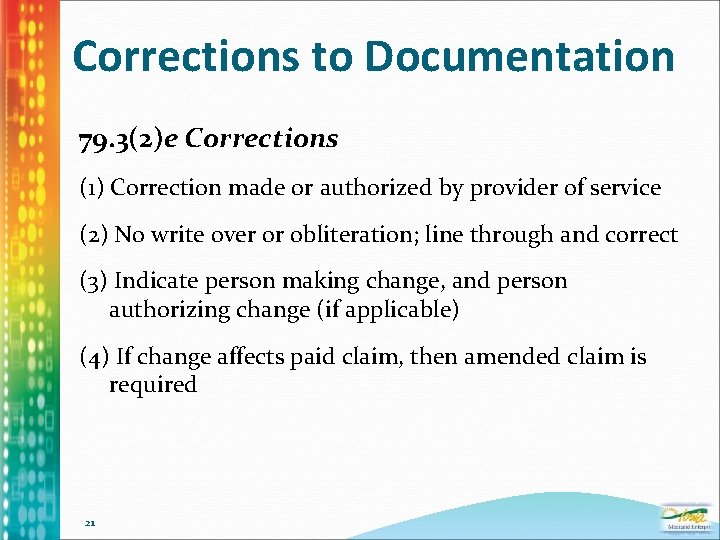
Corrections to Documentation 79. 3(2)e Corrections (1) Correction made or authorized by provider of service (2) No write over or obliteration; line through and correct (3) Indicate person making change, and person authorizing change (if applicable) (4) If change affects paid claim, then amended claim is required 21
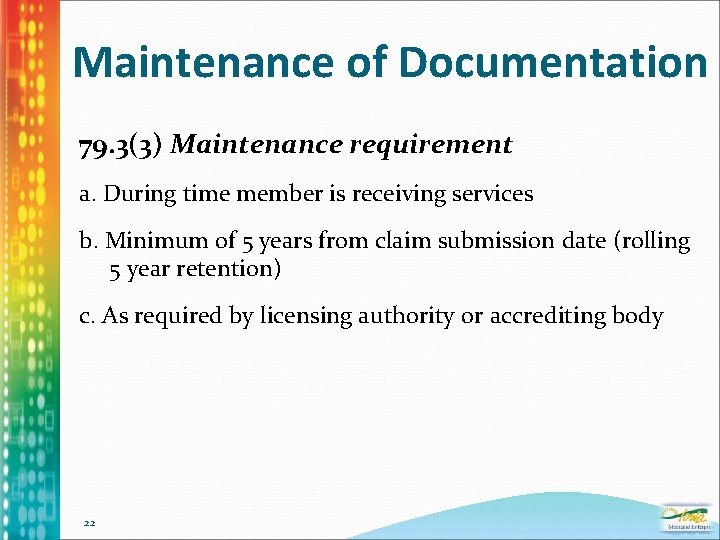
Maintenance of Documentation 79. 3(3) Maintenance requirement a. During time member is receiving services b. Minimum of 5 years from claim submission date (rolling 5 year retention) c. As required by licensing authority or accrediting body 22
Discussion of 441 -79. 4(249 A) 23
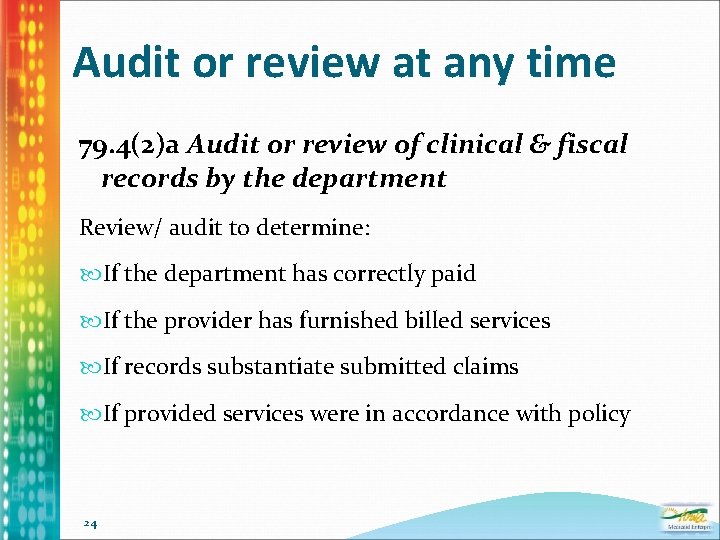
Audit or review at any time 79. 4(2)a Audit or review of clinical & fiscal records by the department Review/ audit to determine: If the department has correctly paid If the provider has furnished billed services If records substantiate submitted claims If provided services were in accordance with policy 24
Documentation Checklist 79. 4(2)b Audit or review of clinical & fiscal records by the department Form 470 -4479 Documentation Checklist Lists specific documents to be requested for SURS review 25
Audit/Review Procedures 79. 4(3) Audit or review procedures a. Records must be submitted within 30 days of written notification b. Extension of time limits: (1) for up to 15 days when: Established good cause Request received before deadline 26
Audit/Review Procedures (2) For another 15 days when: Established exceptional circumstances Received before 15 day extension deadline 27
Audit/Review Procedures c. Announced or unannounced on-site reviews or audits are possible d. Procedures Comparing clinical record against claim Interviewing members & staff Examining TPL records Comparing usual & customary fees 28
Preliminary Report of findings 79. 4(4) Preliminary report of audit or review findings If overpayment has occurred, a preliminary finding of a tentative overpayment letter is issued Provider has opportunity to request reevaluation. 29
Disagreement with Findings 79. 4(5) Disagreement with review findings. Written reevaluation request received within 15 calendar days of notice date Provider can submit clarifying information or supplemental documentation within 30 days 30
Order for Repayment 79. 4(6) Finding and order for repayment. When reevaluation or expiration of deadlines has passed Order for repayment of over payment IME may withhold payments from other claims. 31
Errors in Responding to Reviews - Failure to submit docs timely per IAC 79. 4 - Documentation submitted for wrong dates - Submitted documentation not detailed - Failure to submit: Individual Service Plans Individual comprehensive plans CDAC agreements 32
Documentation Errors Illegible writing No in/ out times (where required) Wrong code vs. service Documentation does not match services Invalid correction No signature or signature sheet 33
More Documentation Errors No dates of service Missing member response to interventions Physician orders not followed Chiro not indicating area of treatment Vision not stating replacement reason DME incorrectly using UE modifier 34
Self Assessments - Quality assurance is in best interest of providers - Value to providers of their own QA assessments Quickly ID narratives that are not adequate Corrections can be made before claim submission Quickly identify staff who need additional training 35
Summary of IAC Discussion Providers can develop a process or system of their own design Chosen system must demonstrate that Medicaid rules are met Providers should proactively review their current system to ensure IAC requirements are met 36
You Have Now Completed Documentation Standards Thank you!
 Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals 2009 mathematics standards of learning answers
2009 mathematics standards of learning answers Agenda sistemica y agenda institucional
Agenda sistemica y agenda institucional General goals and specific goals
General goals and specific goals Motivation in consumer behaviour
Motivation in consumer behaviour User documentation standards
User documentation standards Golden thread clinical documentation
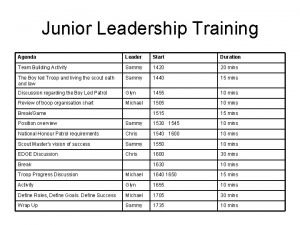
Golden thread clinical documentation Leadership training agenda
Leadership training agenda Hard customer defined standards
Hard customer defined standards Training is expensive without training it is more expensive
Training is expensive without training it is more expensive Perbedaan on the job training dan off the job training
Perbedaan on the job training dan off the job training Aggression replacement training facilitator training
Aggression replacement training facilitator training 2008-2009 school year
2008-2009 school year Servicio social uabc
Servicio social uabc Saresp 2009 uma maquina fotografica
Saresp 2009 uma maquina fotografica Record keeping nmc
Record keeping nmc Ssdt boc
Ssdt boc Plan nacional del buen vivir 2009 al 2013
Plan nacional del buen vivir 2009 al 2013 Permenkes 51 tahun 2009
Permenkes 51 tahun 2009 R.t.t. 2009
R.t.t. 2009 January 2018 chemistry regents
January 2018 chemistry regents Calendar april 2009
Calendar april 2009 Rcfce
Rcfce Impaact 2009
Impaact 2009 In 2009 there were 1570 bears
In 2009 there were 1570 bears Rosa catania 2009
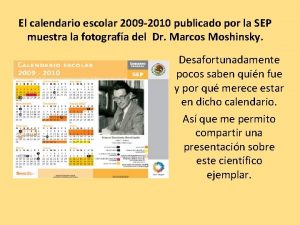
Rosa catania 2009 Calendario escolar 2009
Calendario escolar 2009 Nice 2009
Nice 2009 Decreto 1290 de 2009
Decreto 1290 de 2009 Dpr 89/2009
Dpr 89/2009 Microsoft word 2009
Microsoft word 2009 2009 pearson education inc
2009 pearson education inc Delmar cengage learning medical terminology
Delmar cengage learning medical terminology 2009 delmar cengage learning
2009 delmar cengage learning Chapter 1 learning exercises medical terminology
Chapter 1 learning exercises medical terminology Iso 9004 2009
Iso 9004 2009 Contoh laporan perubahan laba kotor
Contoh laporan perubahan laba kotor