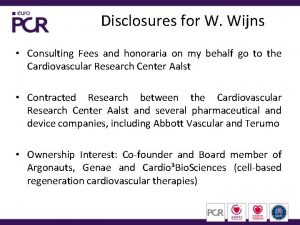
DISCLOSURES Lawrence A Garcia MD Consulting Fees ev
- Slides: 24
DISCLOSURES Lawrence A. Garcia, MD Consulting Fees – ev 3, Inc. , Spectranetics, Pathway Medical Technologies, Inc. , Boston Scientific Corporation Ownership Interest (Stocks, Stock Options or Other Ownership Interest) – Scion Cardio-Vascular, Arsenal Medical, Tissue. Gen, Inc.
Plaque excision: a critical review Lawrence A. Garcia, MD Chief, Section Interventional Cardiology Co-Director, Vascular Medicine Program Director, Interventional Cardiology Fellowship Program St. Elizabeth’s Medical Center Tuft’s University School of Medicine Boston, MA
Infra-inguinal Intervention
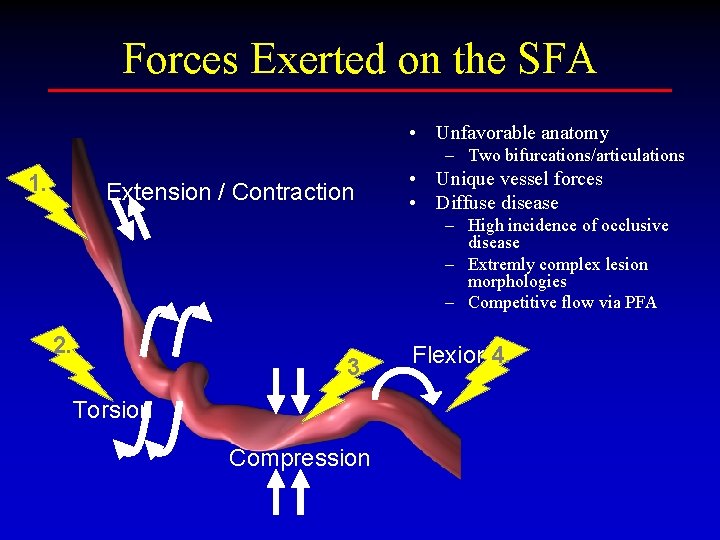
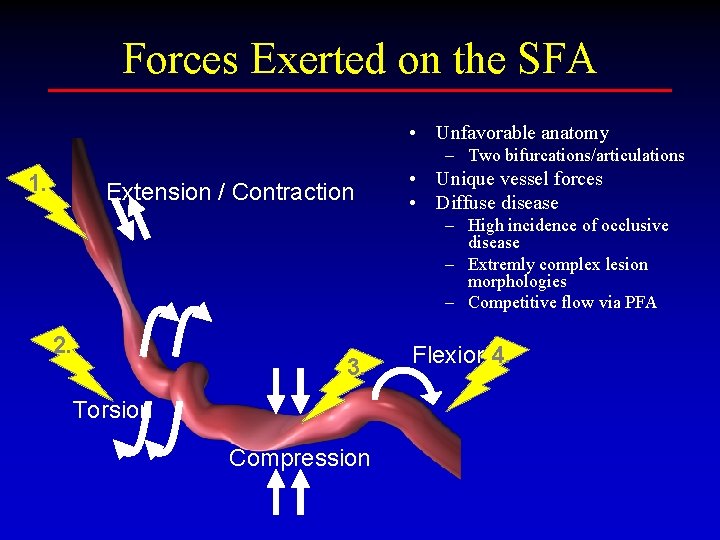
Forces Exerted on the SFA • Unfavorable anatomy – Two bifurcations/articulations 1. Extension / Contraction • Unique vessel forces • Diffuse disease – High incidence of occlusive disease – Extremly complex lesion morphologies – Competitive flow via PFA 2. 3. Torsion Compression Flexion 4.
Strategies to Improve Outcomes • Subintimal angioplasty • Cutting balloon • Nitinol self-expanding stent (SES) • (PTFE)-covered stent grafts • Biodegradable stents • Cutting balloon angioplasty • Cryoplasty • Atherectomy thrombectomy • Drug-eluting stents • Brachytherapy?
Strategies to Improve Outcomes • Angioplasty/subintimal angioplasty • Cutting balloon • Nitinol self-expanding stent (SES) • (PTFE)-covered stent grafts • Biodegradable stents • Cutting balloon angioplasty • Cryoplasty • Plaque modification – Directional atherectomy – Rotational systems • Drug-eluting stents • Brachytherapy? • DES alternatives
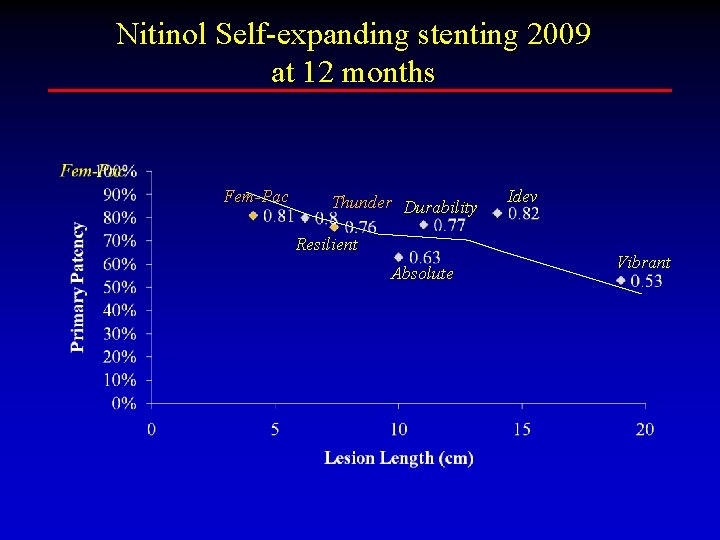
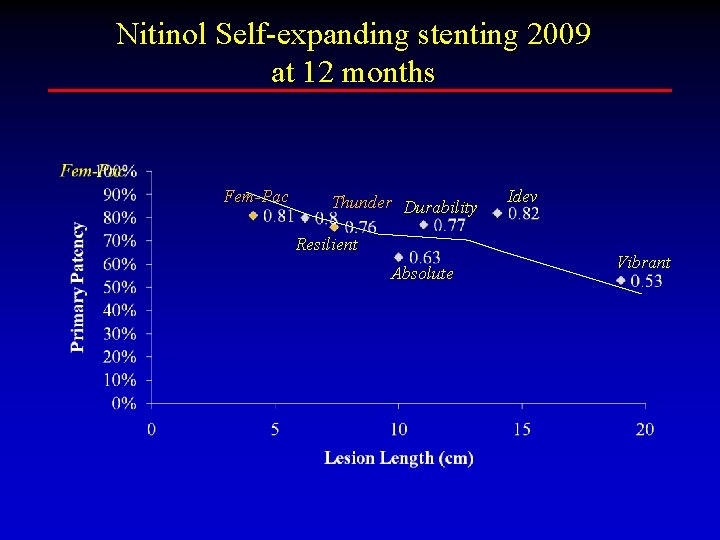
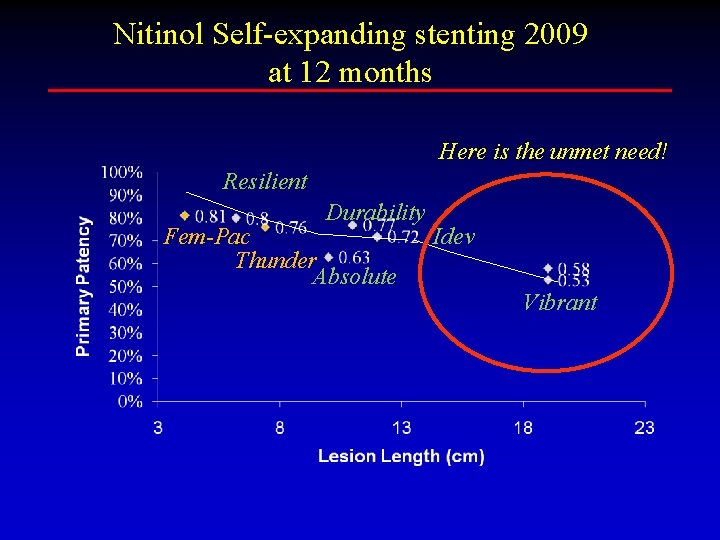
Nitinol Self-expanding stenting 2009 at 12 months Fem-Pac Thunder Durability Resilient Absolute Idev Vibrant
Plaque Modification Therapies • Laser • Directional atherectomy • Rotational devices
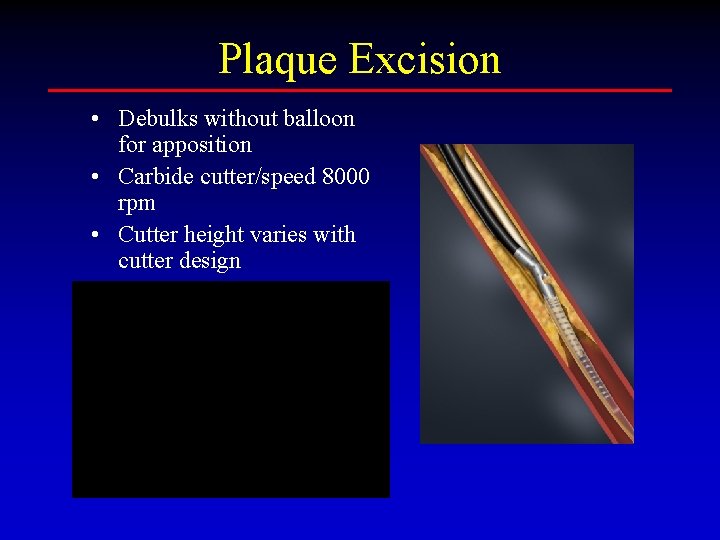
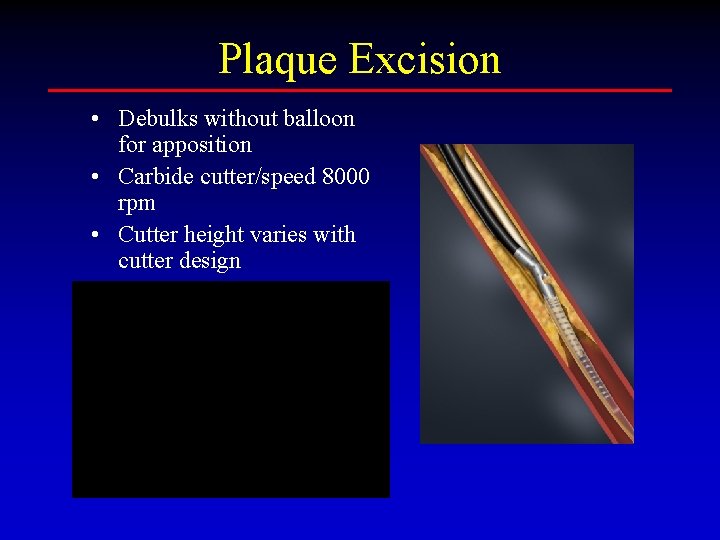
Plaque Excision • Debulks without balloon for apposition • Carbide cutter/speed 8000 rpm • Cutter height varies with cutter design
Plaque Excision • Registry Data • Numerous single center data registries or reports • To date no randomized trial of current technology
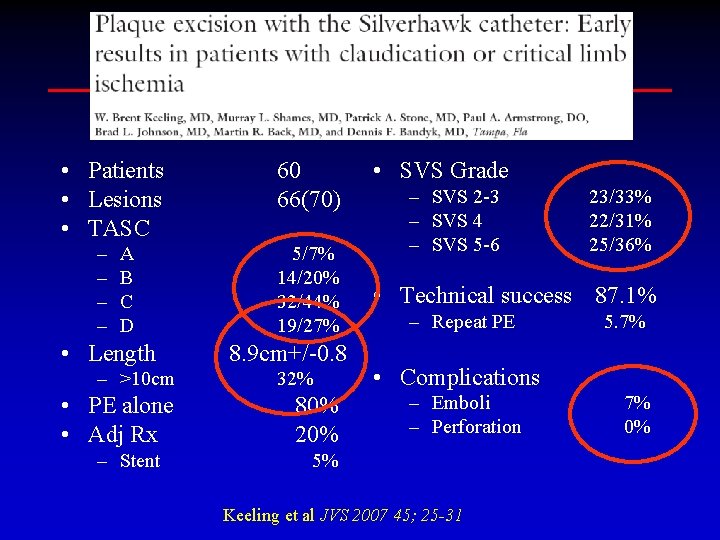
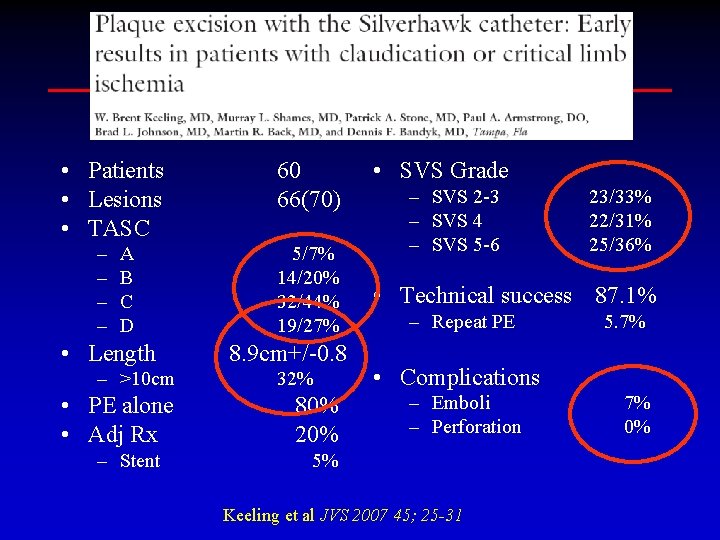
• Patients • Lesions • TASC – – A B C D • Length – >10 cm • PE alone • Adj Rx – Stent 60 66(70) 5/7% 14/20% 32/44% 19/27% 8. 9 cm+/-0. 8 32% 80% 20% • SVS Grade – SVS 2 -3 – SVS 4 – SVS 5 -6 23/33% 22/31% 25/36% • Technical success 87. 1% – Repeat PE 5. 7% • Complications – Emboli – Perforation 5% Keeling et al JVS 2007 45; 25 -31 7% 0%
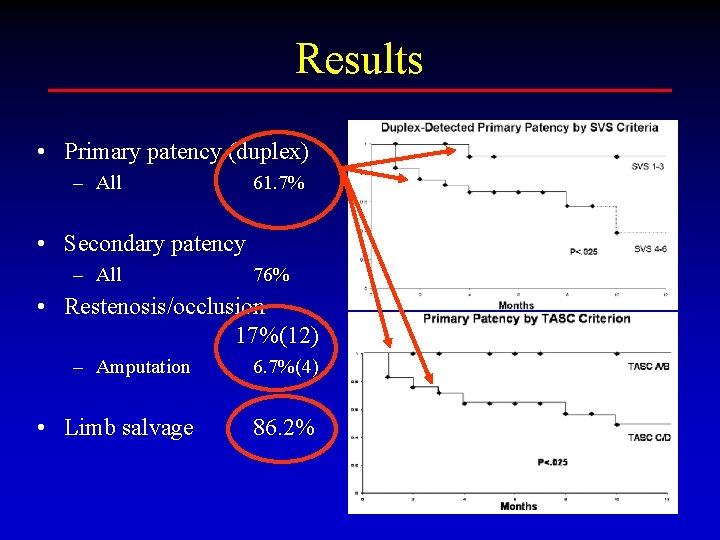
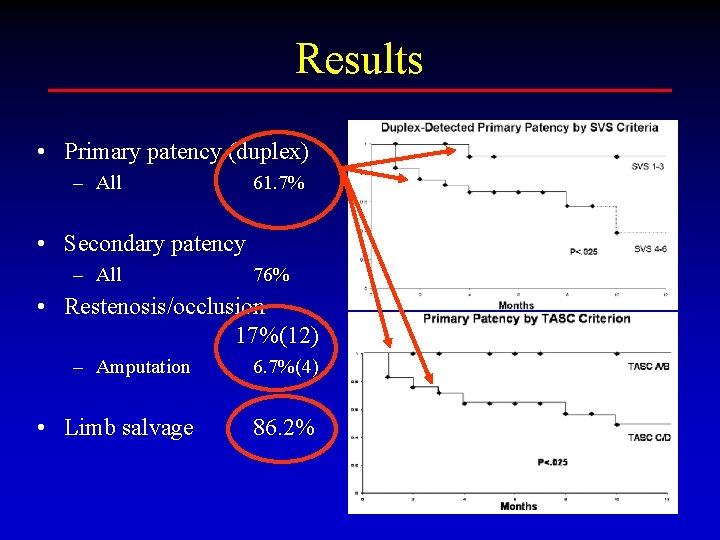
Results • Primary patency (duplex) – All 61. 7% • Secondary patency – All 76% • Restenosis/occlusion 17%(12) – Amputation 6. 7%(4) • Limb salvage 86. 2%
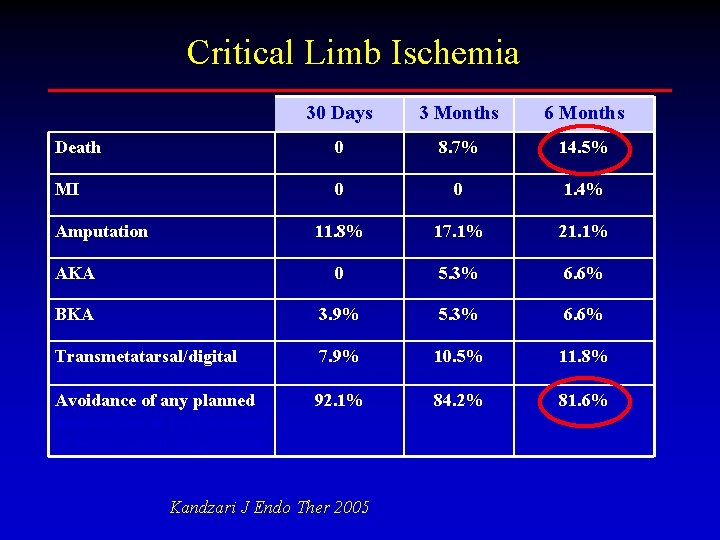
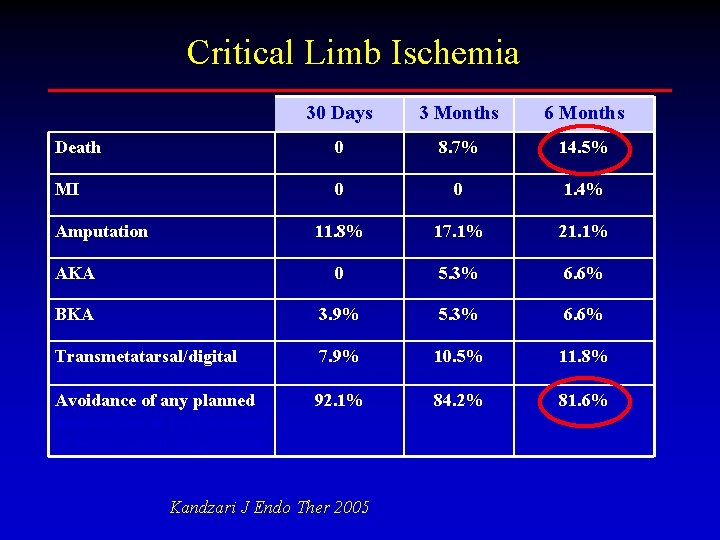
Critical Limb Ischemia 30 Days 3 Months 6 Months Death 0 8. 7% 14. 5% MI 0 0 1. 4% 11. 8% 17. 1% 21. 1% AKA 0 5. 3% 6. 6% BKA 3. 9% 5. 3% 6. 6% Transmetatarsal/digital 7. 9% 10. 5% 11. 8% Avoidance of any planned amputation or performance of lesser extent amputation 92. 1% 84. 2% 81. 6% Amputation Kandzari J Endo Ther 2005
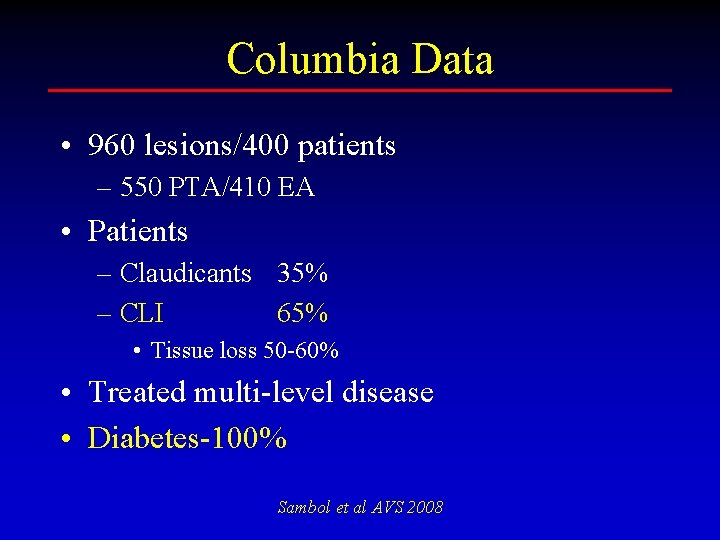
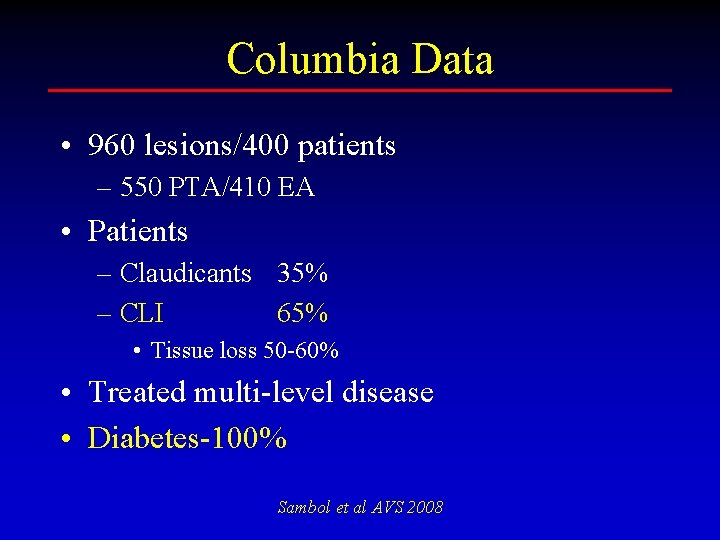
Columbia Data • 960 lesions/400 patients – 550 PTA/410 EA • Patients – Claudicants 35% – CLI 65% • Tissue loss 50 -60% • Treated multi-level disease • Diabetes-100% Sambol et al AVS 2008
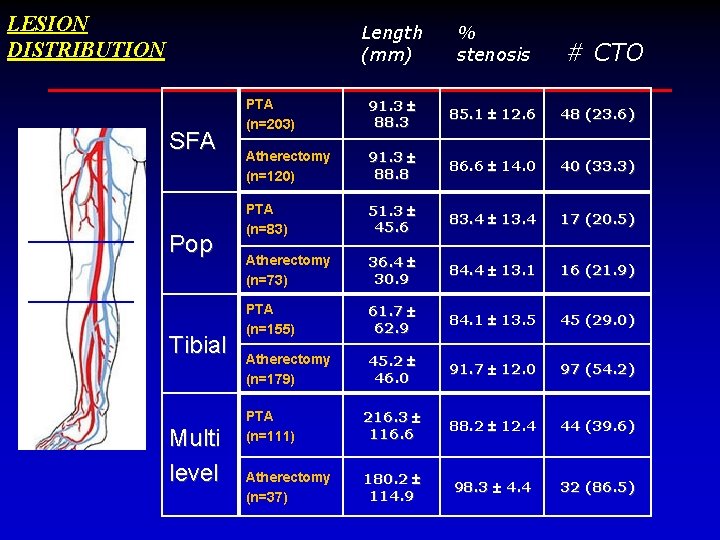
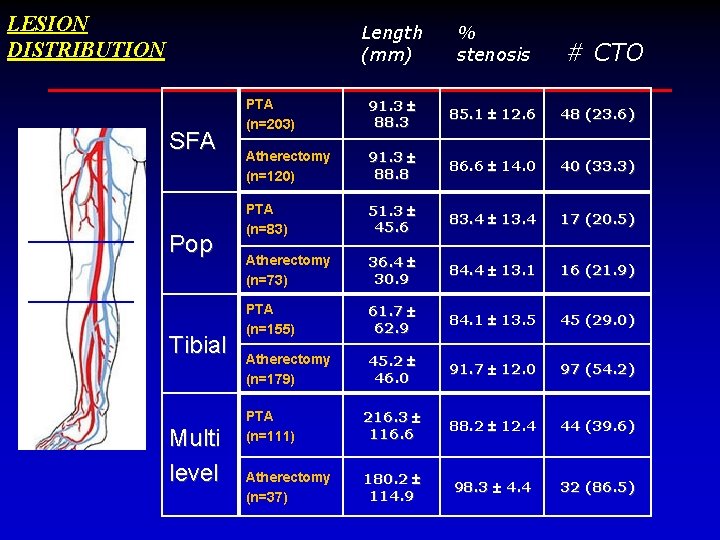
LESION DISTRIBUTION SFA Pop Tibial Multi level Length (mm) % stenosis PTA (n=203) 91. 3 88. 3 85. 1 12. 6 48 (23. 6) Atherectomy (n=120) 91. 3 88. 8 86. 6 14. 0 40 (33. 3) PTA (n=83) 51. 3 45. 6 83. 4 13. 4 17 (20. 5) Atherectomy (n=73) 36. 4 30. 9 84. 4 13. 1 16 (21. 9) PTA (n=155) 61. 7 62. 9 84. 1 13. 5 45 (29. 0) Atherectomy (n=179) 45. 2 46. 0 91. 7 12. 0 97 (54. 2) PTA (n=111) 216. 3 116. 6 88. 2 12. 4 44 (39. 6) Atherectomy (n=37) 180. 2 114. 9 98. 3 4. 4 32 (86. 5) # CTO
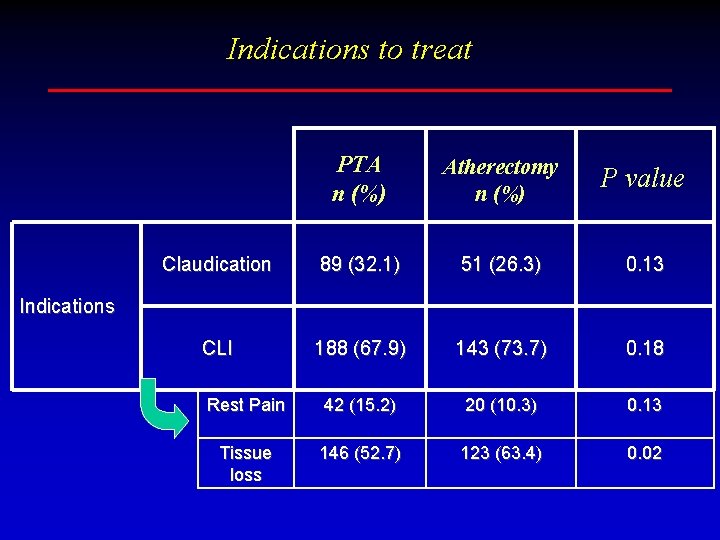
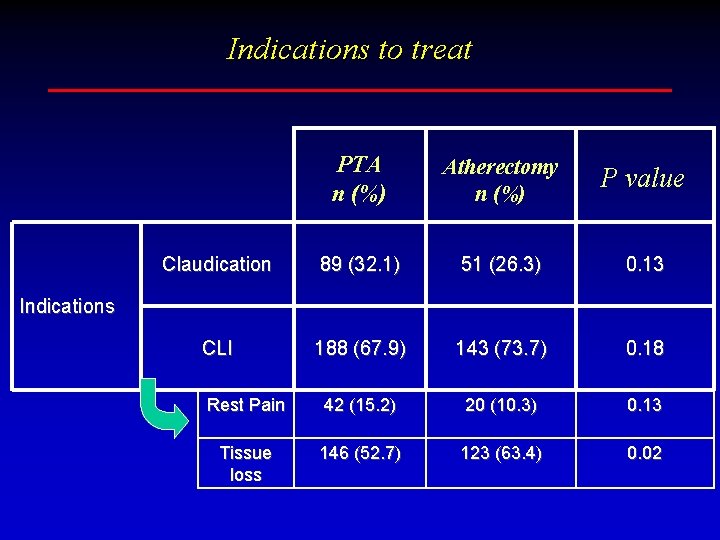
Indications to treat PTA n (%) Atherectomy n (%) P value Claudication 89 (32. 1) 51 (26. 3) 0. 13 CLI 188 (67. 9) 143 (73. 7) 0. 18 Rest Pain 42 (15. 2) 20 (10. 3) 0. 13 Tissue loss 146 (52. 7) 123 (63. 4) 0. 02 Indications
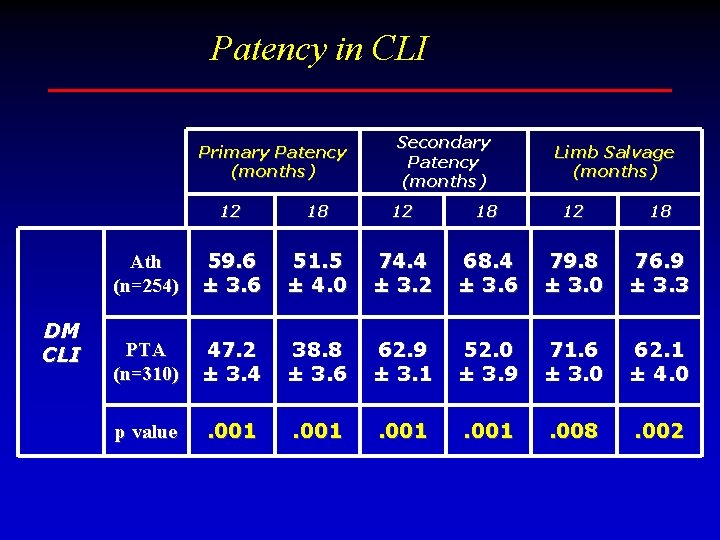
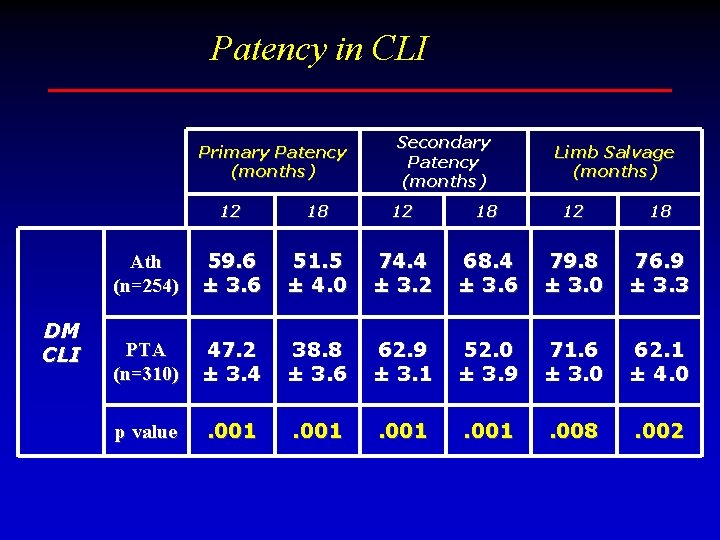
Patency in CLI Primary Patency (months) DM CLI Secondary Patency (months) Limb Salvage (months) 12 18 Ath (n=254) 59. 6 ± 3. 6 51. 5 ± 4. 0 74. 4 ± 3. 2 68. 4 ± 3. 6 79. 8 ± 3. 0 76. 9 ± 3. 3 PTA (n=310) 47. 2 ± 3. 4 38. 8 ± 3. 6 62. 9 ± 3. 1 52. 0 ± 3. 9 71. 6 ± 3. 0 62. 1 ± 4. 0 p value . 001 . 008 . 002
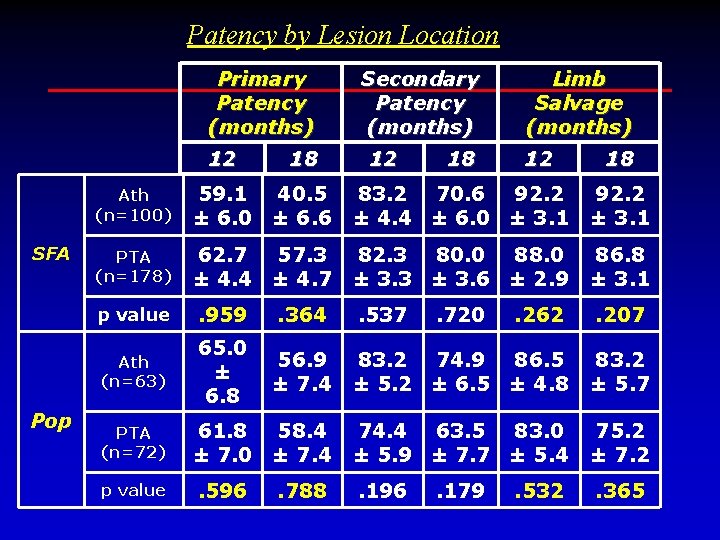
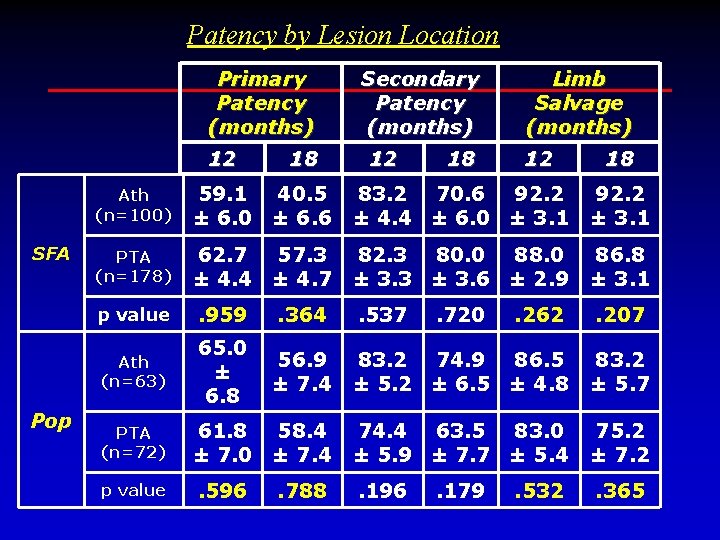
Patency by Lesion Location Primary Patency (months) 12 SFA Pop 18 Secondary Patency (months) 12 18 Limb Salvage (months) 12 18 Ath (n=100) 59. 1 40. 5 ± 6. 0 ± 6. 6 83. 2 70. 6 92. 2 ± 4. 4 ± 6. 0 ± 3. 1 92. 2 ± 3. 1 PTA (n=178) 62. 7 57. 3 ± 4. 4 ± 4. 7 82. 3 80. 0 88. 0 ± 3. 3 ± 3. 6 ± 2. 9 86. 8 ± 3. 1 p value . 959 . 364 . 537 . 262 . 207 Ath (n=63) 65. 0 ± 6. 8 56. 9 ± 7. 4 83. 2 74. 9 86. 5 ± 5. 2 ± 6. 5 ± 4. 8 83. 2 ± 5. 7 61. 8 58. 4 ± 7. 0 ± 7. 4 74. 4 63. 5 83. 0 ± 5. 9 ± 7. 7 ± 5. 4 75. 2 ± 7. 2 . 596 . 196 . 365 PTA (n=72) p value . 788 . 720 . 179 . 532
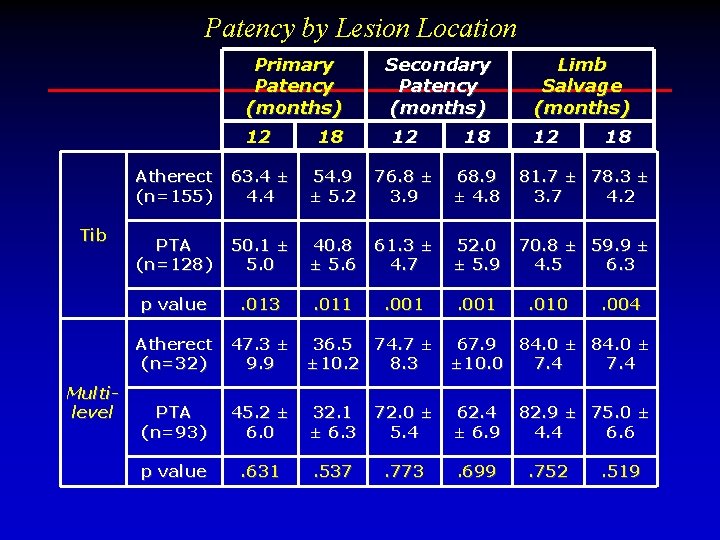
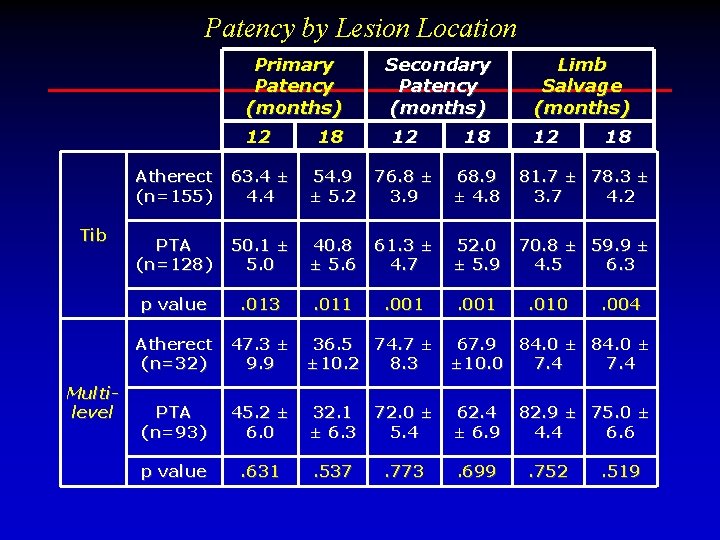
Patency by Lesion Location Primary Patency (months) Tib Limb Salvage (months) 12 18 Atherect (n=155) 63. 4 ± 4. 4 54. 9 ± 5. 2 76. 8 ± 3. 9 68. 9 ± 4. 8 81. 7 ± 78. 3 ± 3. 7 4. 2 PTA (n=128) 50. 1 ± 5. 0 40. 8 ± 5. 6 61. 3 ± 4. 7 52. 0 ± 5. 9 70. 8 ± 59. 9 ± 4. 5 6. 3 p value . 013 . 011 . 001 Atherect (n=32) Multilevel Secondary Patency (months) 12 . 010 18 . 004 47. 3 ± 36. 5 74. 7 ± 67. 9 84. 0 ± 9. 9 ± 10. 2 8. 3 ± 10. 0 7. 4 PTA (n=93) 45. 2 ± 6. 0 32. 1 ± 6. 3 72. 0 ± 5. 4 62. 4 ± 6. 9 p value . 631 . 537 . 773 . 699 82. 9 ± 75. 0 ± 4. 4 6. 6. 752 . 519
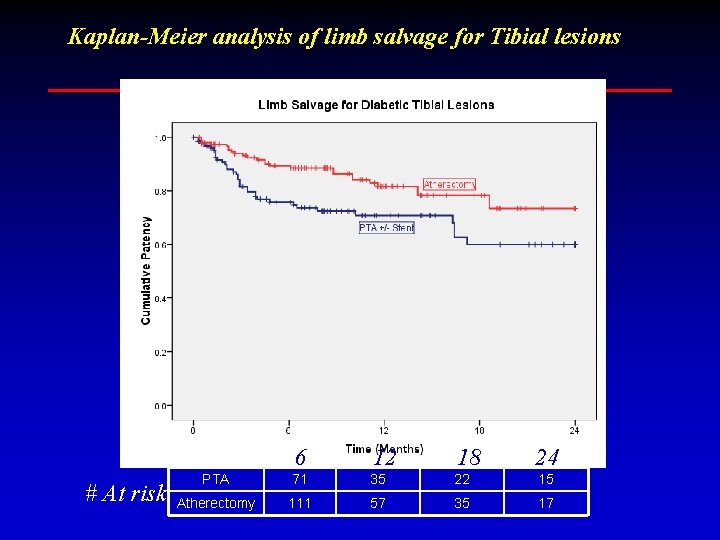
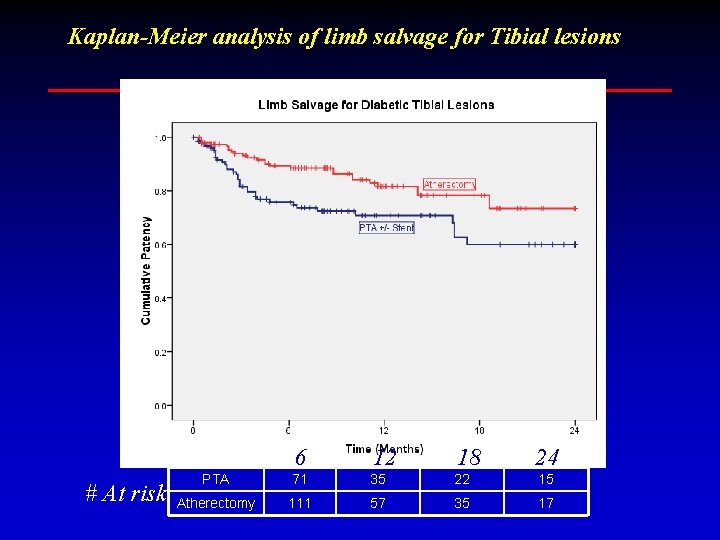
Kaplan-Meier analysis of limb salvage for Tibial lesions PTA # At risk: Atherectomy 6 12 18 24 71 35 22 15 111 57 35 17
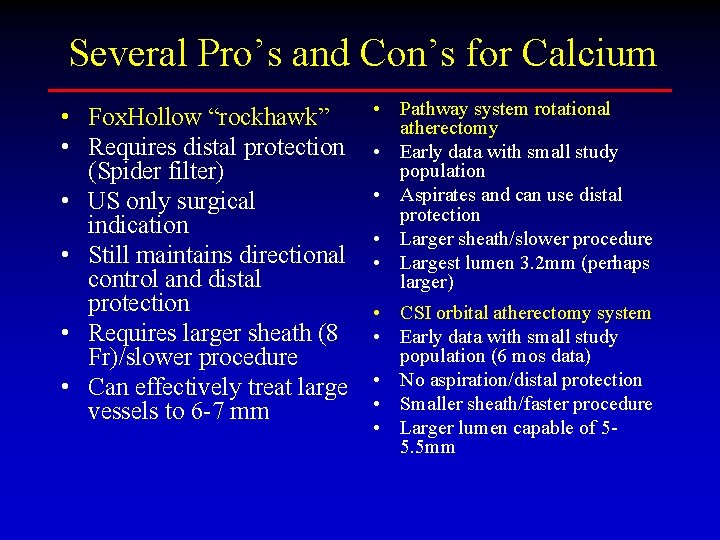
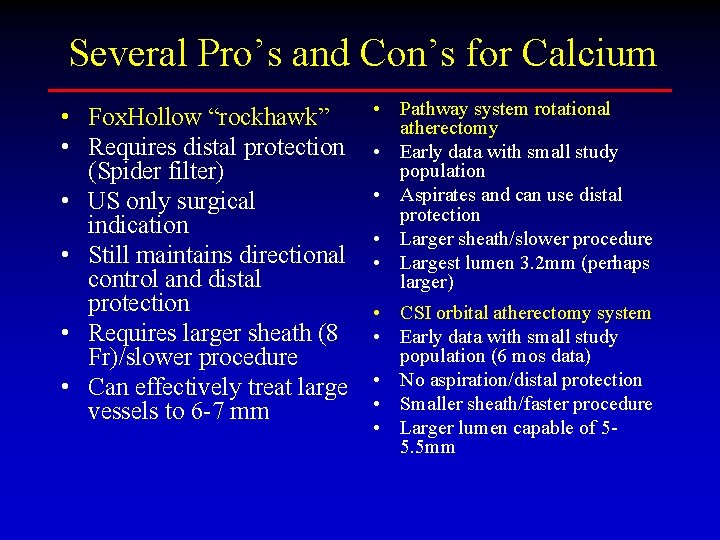
Several Pro’s and Con’s for Calcium • Fox. Hollow “rockhawk” • Requires distal protection (Spider filter) • US only surgical indication • Still maintains directional control and distal protection • Requires larger sheath (8 Fr)/slower procedure • Can effectively treat large vessels to 6 -7 mm • Pathway system rotational atherectomy • Early data with small study population • Aspirates and can use distal protection • Larger sheath/slower procedure • Largest lumen 3. 2 mm (perhaps larger) • CSI orbital atherectomy system • Early data with small study population (6 mos data) • No aspiration/distal protection • Smaller sheath/faster procedure • Larger lumen capable of 55. 5 mm
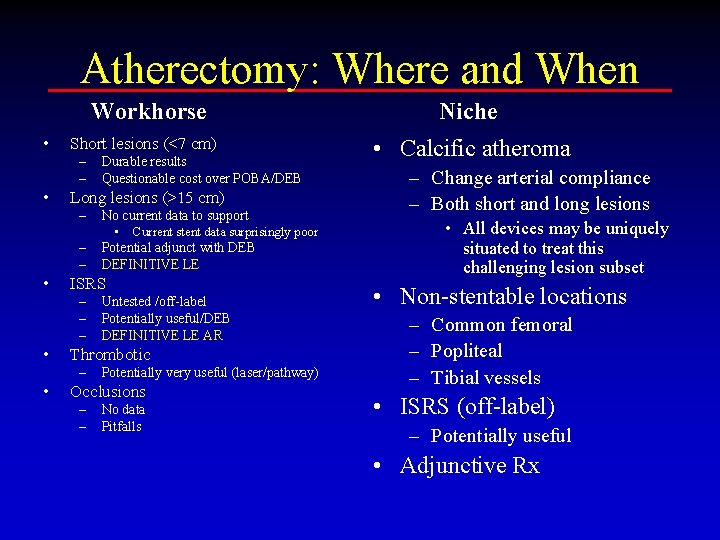
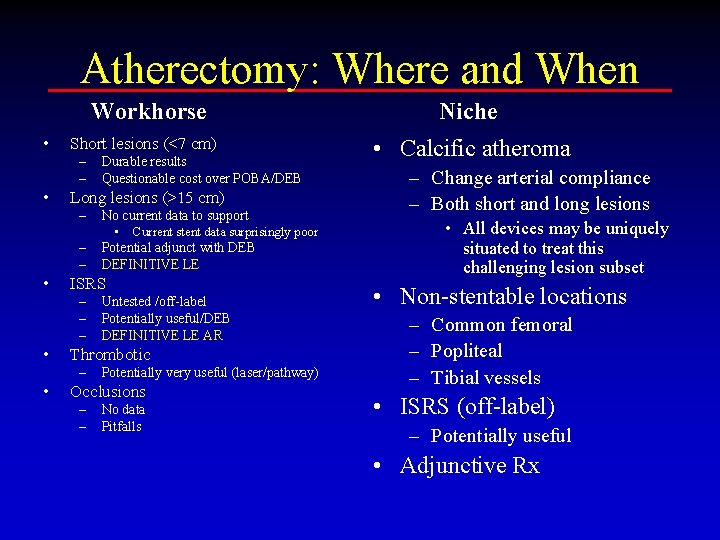
Atherectomy: Where and When Workhorse • Short lesions (<7 cm) – – • Long lesions (>15 cm) – – – • Untested /off-label Potentially useful/DEB DEFINITIVE LE AR Thrombotic – • No current data to support • Current stent data surprisingly poor Potential adjunct with DEB DEFINITIVE LE ISRS – – – • Durable results Questionable cost over POBA/DEB Potentially very useful (laser/pathway) Occlusions – – No data Pitfalls Niche • Calcific atheroma – Change arterial compliance – Both short and long lesions • All devices may be uniquely situated to treat this challenging lesion subset • Non-stentable locations – Common femoral – Popliteal – Tibial vessels • ISRS (off-label) – Potentially useful • Adjunctive Rx
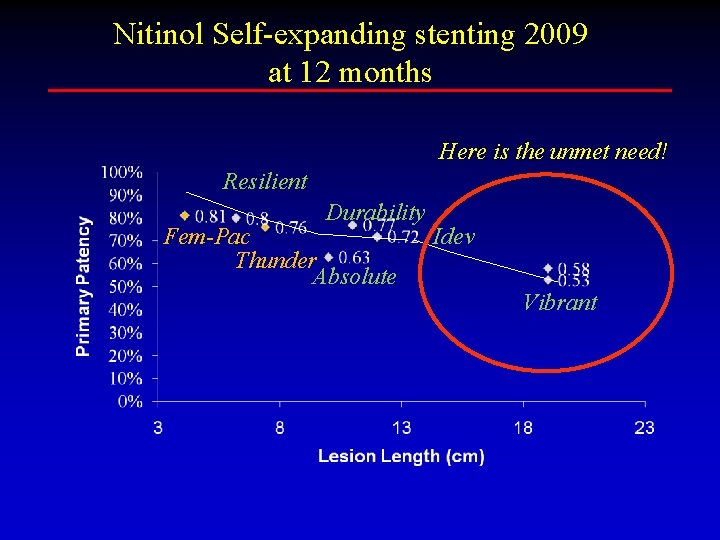
Nitinol Self-expanding stenting 2009 at 12 months Here is the unmet need! Resilient Durability Fem-Pac Thunder Absolute Idev Vibrant
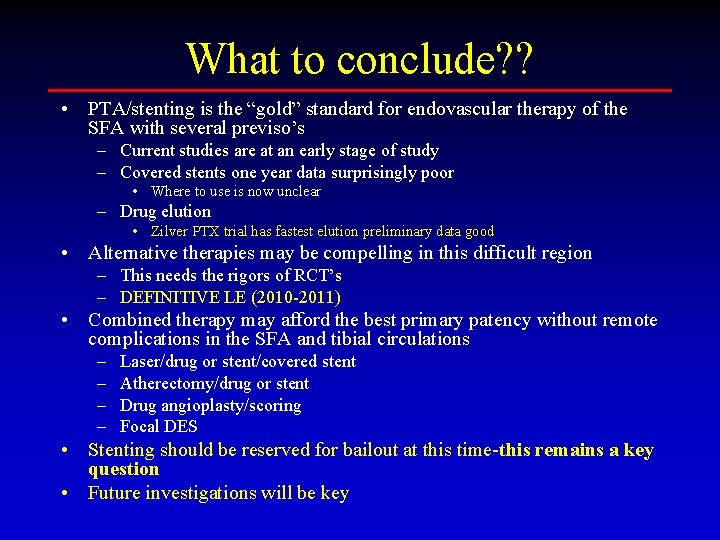
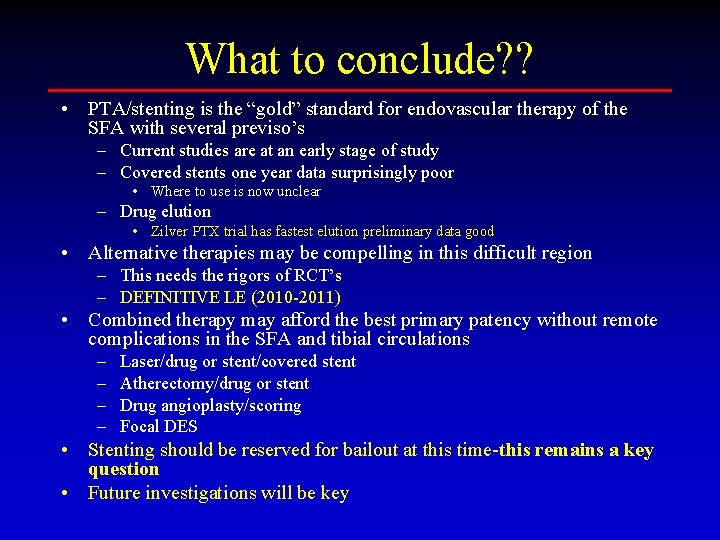
What to conclude? ? • PTA/stenting is the “gold” standard for endovascular therapy of the SFA with several previso’s – Current studies are at an early stage of study – Covered stents one year data surprisingly poor • Where to use is now unclear – Drug elution • Zilver PTX trial has fastest elution preliminary data good • Alternative therapies may be compelling in this difficult region – This needs the rigors of RCT’s – DEFINITIVE LE (2010 -2011) • Combined therapy may afford the best primary patency without remote complications in the SFA and tibial circulations – – Laser/drug or stent/covered stent Atherectomy/drug or stent Drug angioplasty/scoring Focal DES • Stenting should be reserved for bailout at this time-this remains a key question • Future investigations will be key
 Lawrence garcia md
Lawrence garcia md No financial interest disclosure statement
No financial interest disclosure statement Voluntary disclosures meaning
Voluntary disclosures meaning Disclosure slide example
Disclosure slide example Website disclosures under companies act 2013
Website disclosures under companies act 2013 Disclosures slide
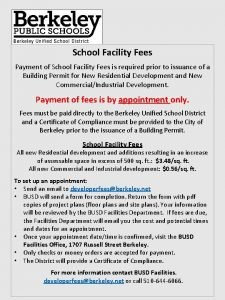
Disclosures slide Application for fees delay
Application for fees delay Leo club membership fees
Leo club membership fees Wells fargo credit card machine
Wells fargo credit card machine What is considered immediate family
What is considered immediate family Slotting fees ethical
Slotting fees ethical Atys international school
Atys international school Lmaa fees
Lmaa fees Vsas fees
Vsas fees What's the best strategy for avoiding atm fees?
What's the best strategy for avoiding atm fees? Hmda dpms land use
Hmda dpms land use Donation in income and expenditure account
Donation in income and expenditure account Student financial services uwaterloo
Student financial services uwaterloo Computer society of india logo
Computer society of india logo Withdraw cash for personal use journal entry
Withdraw cash for personal use journal entry Toomanagement auction list
Toomanagement auction list Zed scheme
Zed scheme Ssp naat
Ssp naat Finance mathematical literacy grade 12
Finance mathematical literacy grade 12 Flower of may site fees
Flower of may site fees