CPPD DEPOSITION DISEASE z Calcium Pyrophosphate Dihydrate Epidemiology



- Slides: 34
CPPD DEPOSITION DISEASE z. Calcium Pyrophosphate Dihydrate
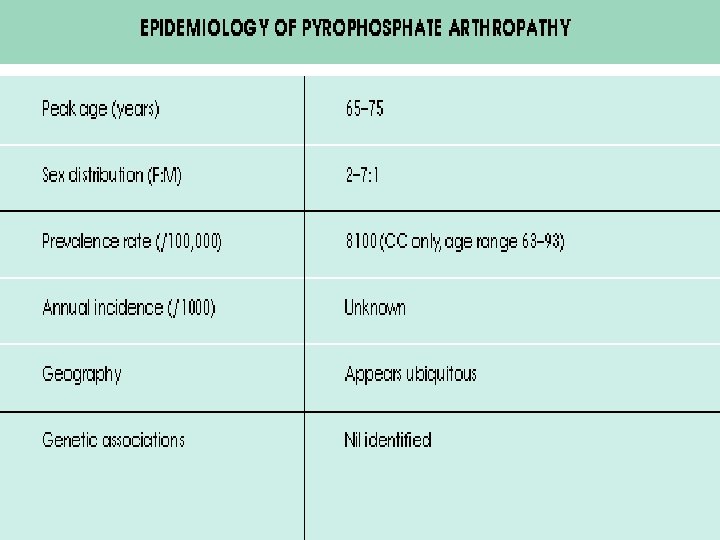
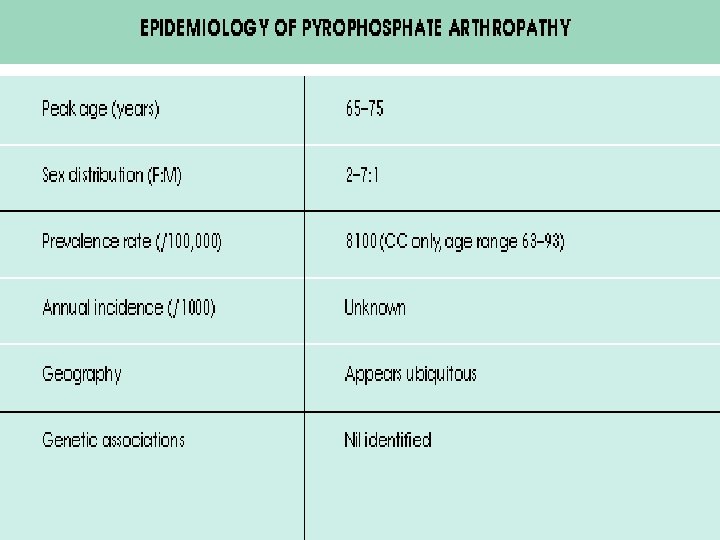
Epidemiology z. Most common in the elderly z 10 to 15% of persons 65 to 75 years old and 30 to 60% of those more than 85 years old z. In most cases this process is asymptomatic
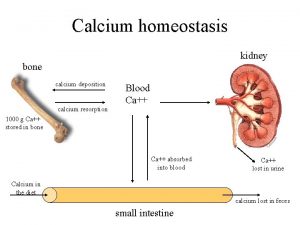
What is CPPD Ca 2 P 2 O 2. 2 H 2 O
Etiology z Cause of CPPD deposition is uncertain z Because over 80% of patients are more than 60 years old and 70% have preexisting joint damage from other conditions, it is likely that biochemical changes in aging cartilage favor crystal nucleation z There is an increased production of inorganic pyrophosphate and decreased levels of pyrophosphatases in cartilage extracts from patients
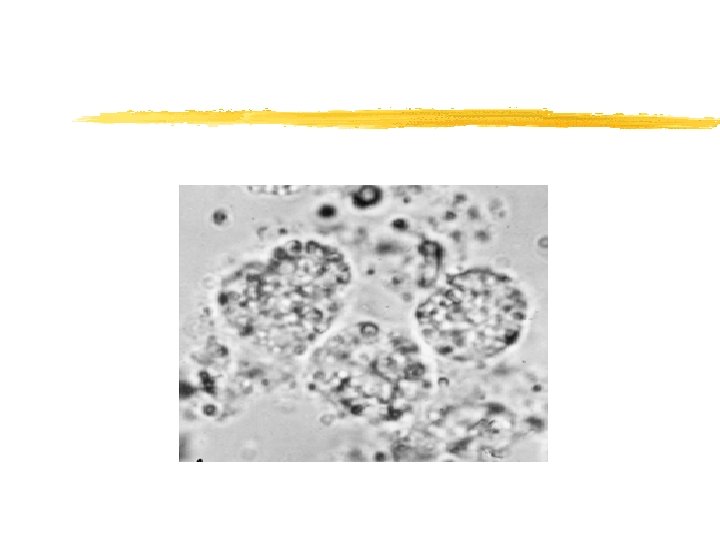
Pathophysioloy z. The release of CPPD crystals into the joint space is followed by the phagocytosis of these crystals by neutrophils, which respond by releasing inflammatory substances. In addition, neutrophils release a glycopeptide that is chemotactic for other neutrophils, thus augmenting the inflammatory events
Pathophysioloy z. A minority of patients with CPPD arthropathy have metabolic abnormalities or hereditary CPPD disease
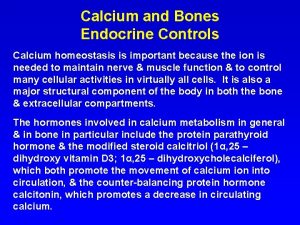
Conditions associated with CPPD z. Aging z. Hyperparathyroidism z Hemochromatosis z Hypophosphatasia z. Hypomagnesemia z. Chronic thophaceous gout z. Hereditary
Clinical Manifestations z. CPPD arthropathy may be asymptomatic, acute, subacute, or chronic or cause acute synovitis superimposed on chronically involved joints
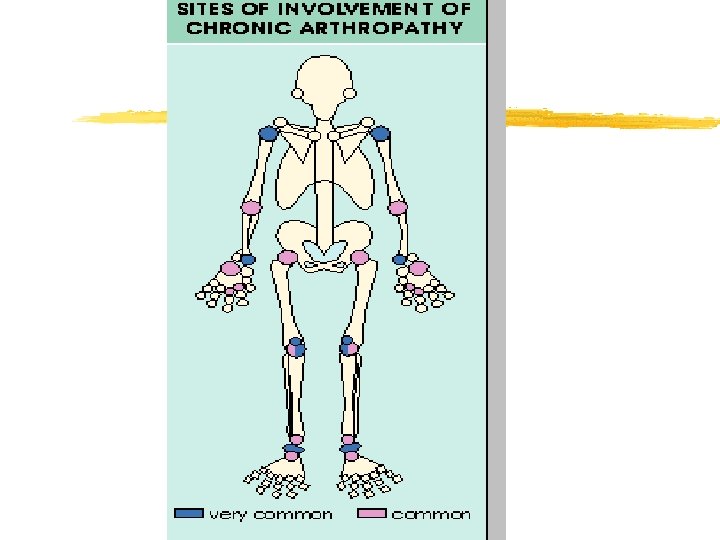
Clinical Manifestations z. Pseudogout z. Pseudo-osteoarthritis z. Pseudo-Rheumatoid z. Destructive arthropathy z. Bursitis, tendinitis, enthesitis
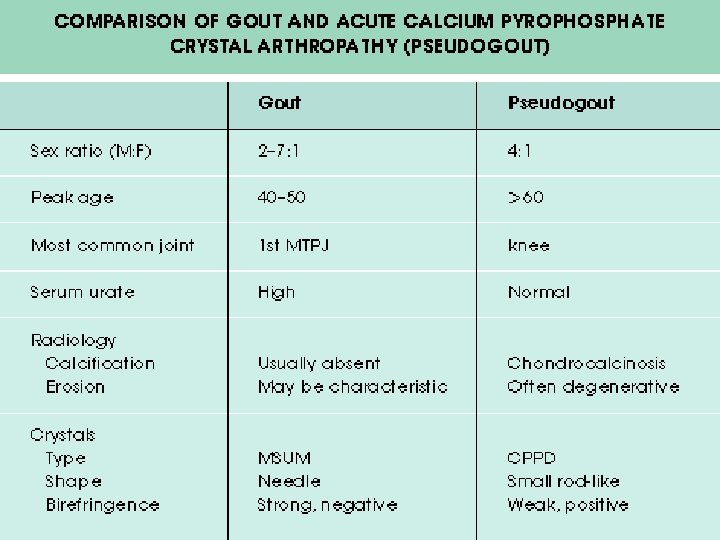
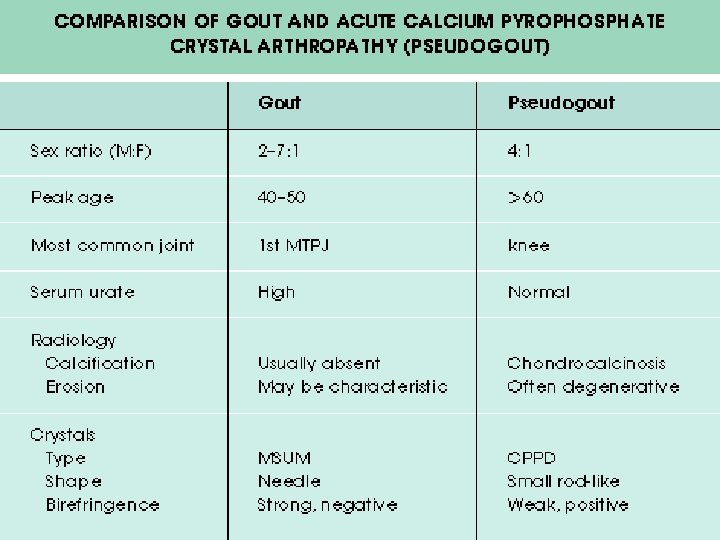
Acute Arthritis(Pseudogout) z May be precipitated by trauma z Knee, wrist, shoulder, ankle, elbow, and hands z Symptoms are the same as any acute arthritis z Occasionally systemic symptoms: Fever z Self limited z Patients are asymptomatic between attacks

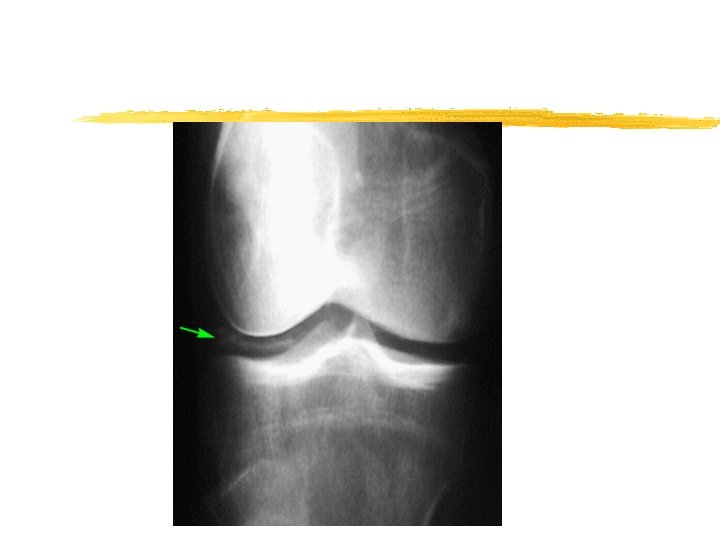
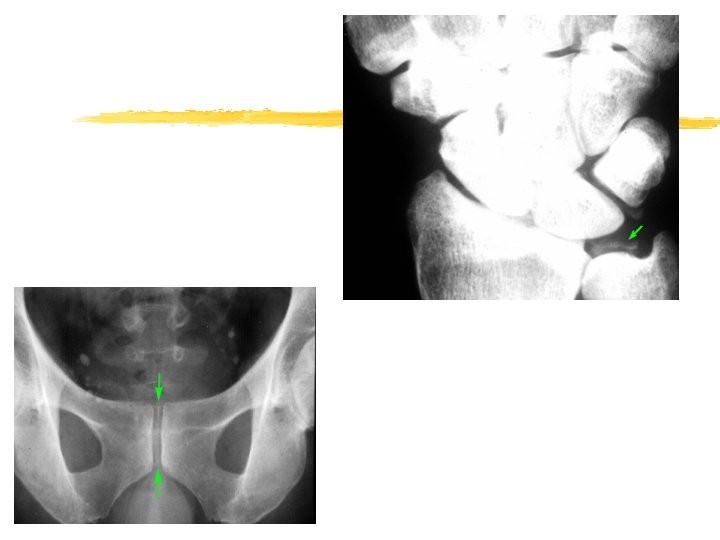
Imaging z Chondrocalcinosis
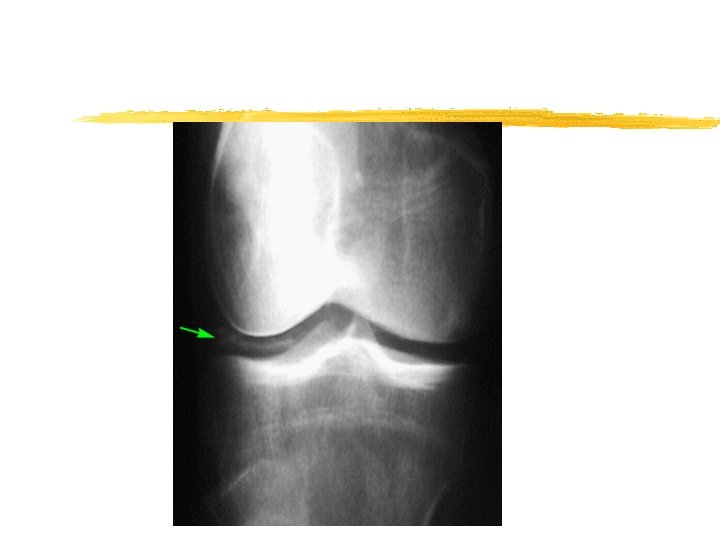
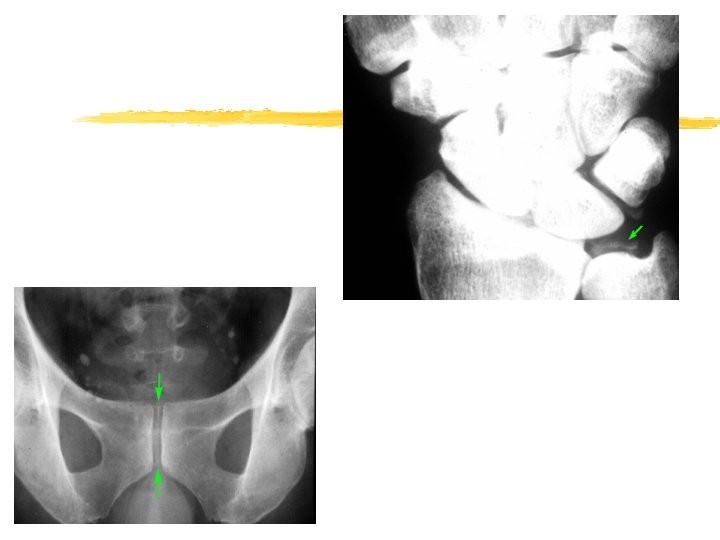

IS all chondrocaclnosis caused by CPPD z. No z. Other calcium salts such as calcium hydroxyapatite z. Ochronosis
Synovial fluid z. Several thousand cells to 100, 000 cells/u. L z. Mean being about 24, 000 cells/u. L z. Predominant cell being the PMN
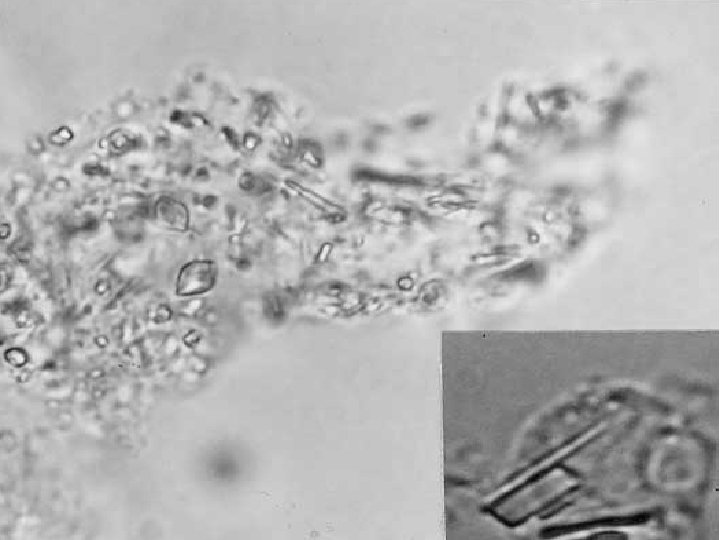
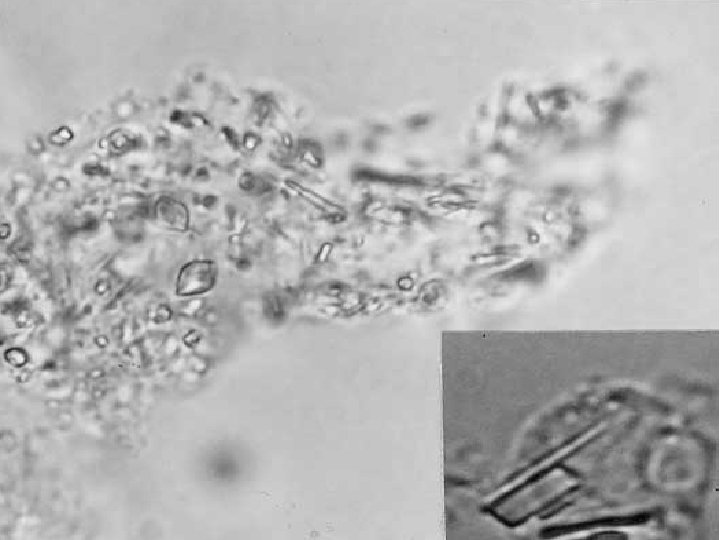
Diagnosis z Polarization microscopy usually reveals rod - shape or rhomboid crystals inside fibrin and in PMN
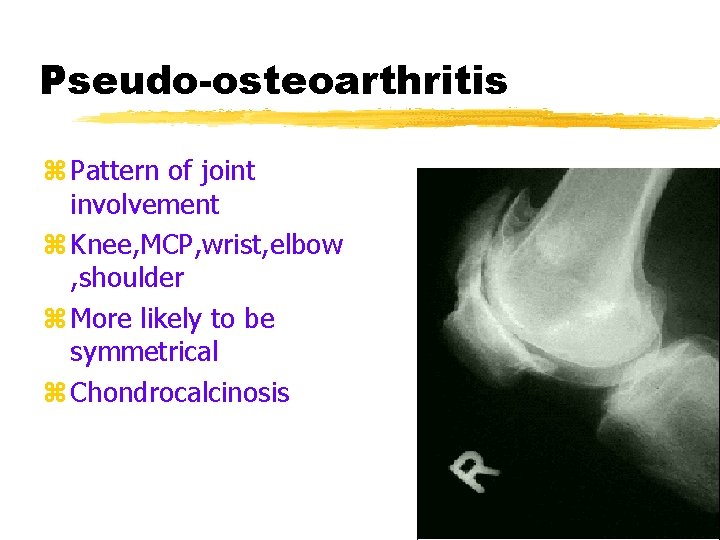
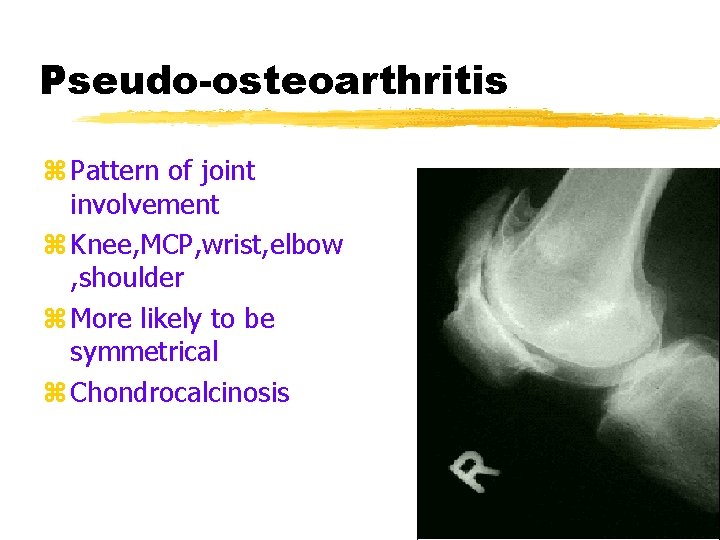
Pseudo-osteoarthritis z Pattern of joint involvement z Knee, MCP, wrist, elbow , shoulder z More likely to be symmetrical z Chondrocalcinosis
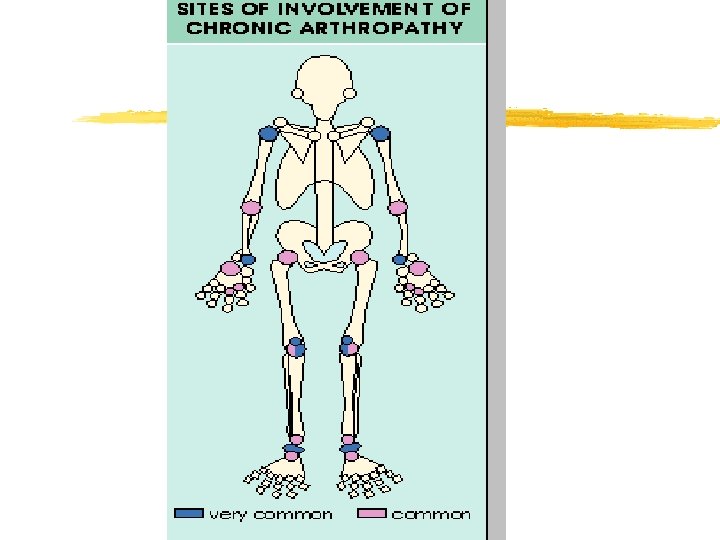
Pseudo-Rheumatoid z. RF 10% z. Involvement of hands z. CPPD Crystals z. X-ray

Treatment z. NSAIDS z. Colchicin z. Corticosteroids
CALCIUM HYDROXYAPATITE DEPOSITION DISEASE
Pathogenesis z HA is the primary mineral of bone z HA may be released from exposed bone and cause the acute synovitis z Most patients with HA arthropathy are elderly. z Periarticular and articular deposits may coexist and be associated with acute and/or chronic damage to the joint capsule, tendons, bursa, or articular surfaces.
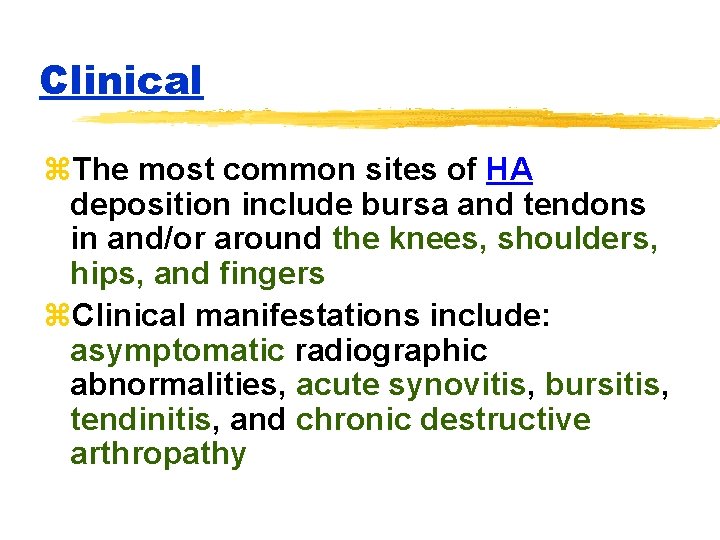
Clinical z. The most common sites of HA deposition include bursa and tendons in and/or around the knees, shoulders, hips, and fingers z. Clinical manifestations include: asymptomatic radiographic abnormalities, acute synovitis, bursitis, tendinitis, and chronic destructive arthropathy
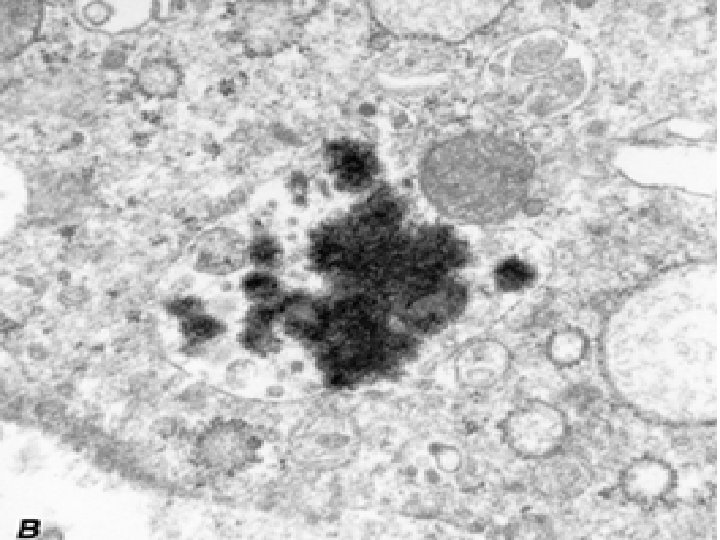
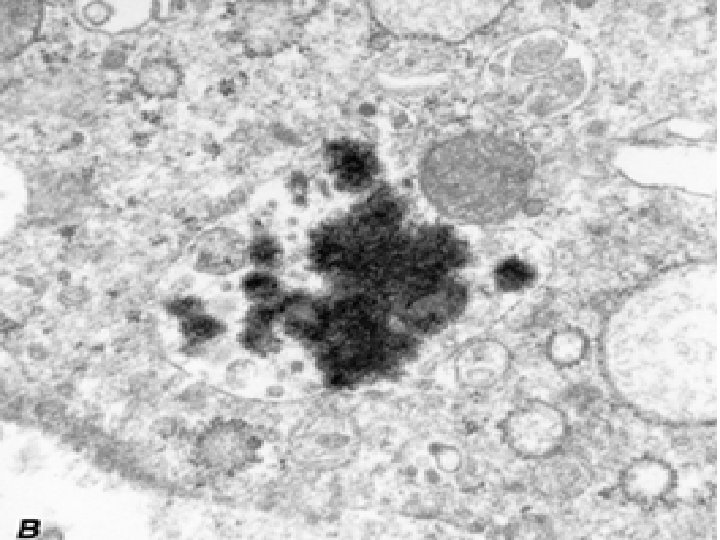
Diagnosis z. Intra- and/or periarticular calcifications zcrystals are very small, and can only be seen by electron microscopy.
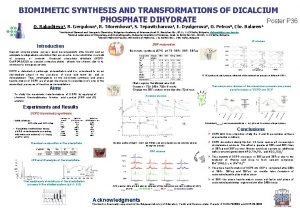
 Gypsum bonded investment composition
Gypsum bonded investment composition Thiamine pyrophosphate
Thiamine pyrophosphate Communicable disease and non communicable disease
Communicable disease and non communicable disease Gate frame epidemiology
Gate frame epidemiology Distribution in epidemiology
Distribution in epidemiology Spurious association in epidemiology
Spurious association in epidemiology Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Attack rate epidemiology formula
Attack rate epidemiology formula Logistic regression epidemiology
Logistic regression epidemiology John snow epidemiology
John snow epidemiology Nutritional epidemiology
Nutritional epidemiology Gordon epidemiology
Gordon epidemiology Defination of epidemiology
Defination of epidemiology Thesourceagents
Thesourceagents Epidemiology definition
Epidemiology definition Define epidemiology
Define epidemiology Field epidemiology ppt
Field epidemiology ppt Gate frame epidemiology
Gate frame epidemiology Pros and cons of cross sectional study
Pros and cons of cross sectional study Formula for attack rate
Formula for attack rate Orlies
Orlies Malaria parasites under microscope
Malaria parasites under microscope Effect modification epidemiology
Effect modification epidemiology Epidemiology kept simple
Epidemiology kept simple Epornithic
Epornithic Descriptive epidemiology
Descriptive epidemiology Perbedaan or dan rr
Perbedaan or dan rr Define epidemiology
Define epidemiology Prevalence definition epidemiology
Prevalence definition epidemiology Aims of epidemiology
Aims of epidemiology Wheel causation model
Wheel causation model Causal vs association
Causal vs association Classification of epidemiological studies
Classification of epidemiological studies Attack rate epidemiology
Attack rate epidemiology Distribution in epidemiology
Distribution in epidemiology