Coordination of Care and Integrated Care New York

- Slides: 13
Coordination of Care and Integrated Care New York State Perspective Association Greater New York Hospital Association Peggy Elmer, LCSW Health Home Director, Department of Health, Office of Health Insurance Programs Nicole Haggerty, LMHC Director for the Bureau of Rehabilitation Services and Care Coordination, OMH Adult Services Office of Mental Health

2 THANK YOU
3 MRT Waivers New York’s Medicaid program is largely governed by our Medicaid Waiver with CMS New York is continuing to monitor and assess the development of priorities, policies and procedures of the new Federal Administration and how its approach may impact New York’s current Medicaid Program and other important MRT Initiatives that require CMS approval Until uncertainties are resolved, New York will continue to take a prudent and cautious approach to submitting amendments to its Medicaid Waiver, including: • Children’s Health and Behavioral Health Waiver Amendment • Criminal Justice Waiver Amendment • Ending the AIDS Epidemic
4 Health Home Successes • • Implementation of temporary billing processes (Emed. NY to HH to CMA) to ensure timely payments while Managed Care plans make system changes to process claims through their All Payer Database (Plan to HH to CMA) Expansion of HH+ to include: • • State Psychiatric Center Discharges and; Central New York/NYS Prison releases for individuals with SMI. *Assisted Outpatient Treatment (AOT) since 2014 Looking at additional populations that would benefit from increased care management support Successful launch of Health Homes Serving Children ü As of April 2017 • 8, 218 children enrolled in Health Home • 3, 494 in outreach ü Northwell is continuing its readiness activities to become designated to serve children ü Conversion of OMH TCM providers to Health Home nearing completion ü Other operational issues being addressed through guidance documents
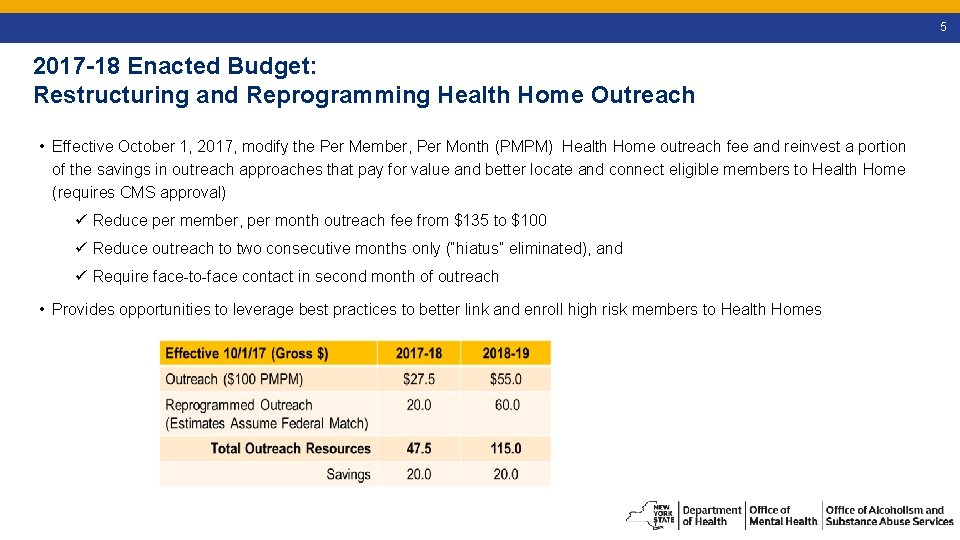
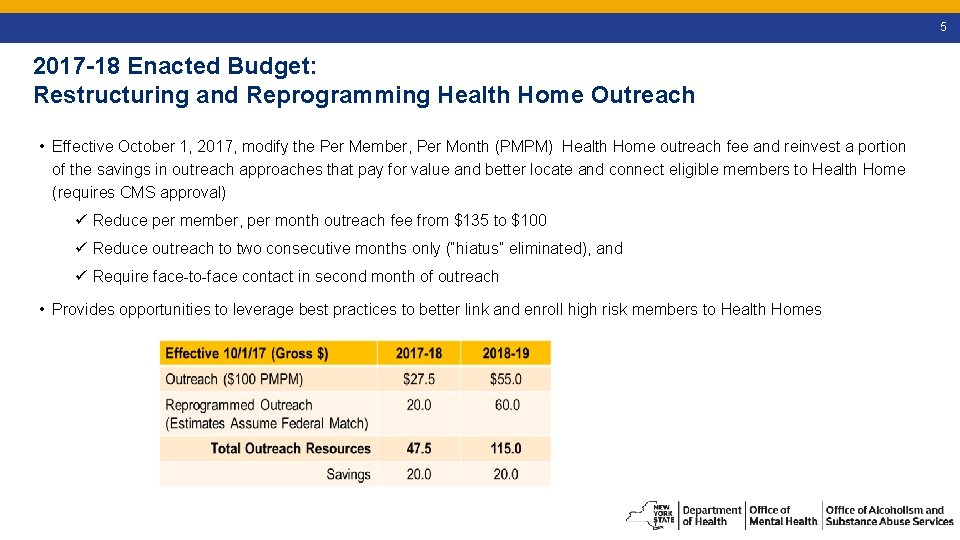
5 2017 -18 Enacted Budget: Restructuring and Reprogramming Health Home Outreach • Effective October 1, 2017, modify the Per Member, Per Month (PMPM) Health Home outreach fee and reinvest a portion of the savings in outreach approaches that pay for value and better locate and connect eligible members to Health Home (requires CMS approval) ü Reduce per member, per month outreach fee from $135 to $100 ü Reduce outreach to two consecutive months only (“hiatus” eliminated), and ü Require face-to-face contact in second month of outreach • Provides opportunities to leverage best practices to better link and enroll high risk members to Health Homes
6 2017 -18 Enacted Budget: Opportunities to Reprogram Outreach to Pay for Value, Increase Health Home Enrollment Options for reprogramming outreach include: ü Provide higher PMPMs for first three months of enrollment for high risk members (e. g. , HARP) not previously enrolled by Health Home ü Make performance based payments to be shared by Care Managers and their lead Health Homes • Payments for retention and active engagement (provision of billable services) for six consecutive months • Establish Health Home Peer Program - work with Health Homes to strategically resource and locate peers in Hospitals, Emergency Rooms, clinics, shelters and PPS projects ü Work with Health Homes and Managed Care Plans to expand use of best practices/current and proven outreach approaches
7 2017 -18 Enacted Budget Facilitation Transition of VFCA Population to Managed Care – VFCA License The Enacted Budget (Part N of the ELFA Bill) includes language to authorize and implement a specialized licensed for voluntary foster care agencies (VFCAs) that provide medical services to children enrolled in foster care • The VFCA License facilitates the transition of the VFCA population to Managed Care by providing Managed Care plans the ability to contract with VFCAs consistent with the State’s Corporate Practice of Medicine Requirements
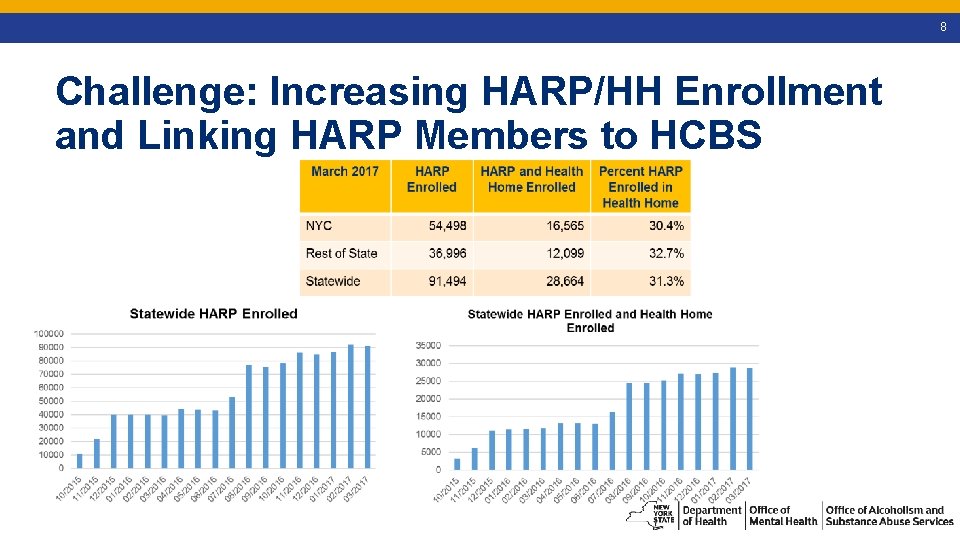
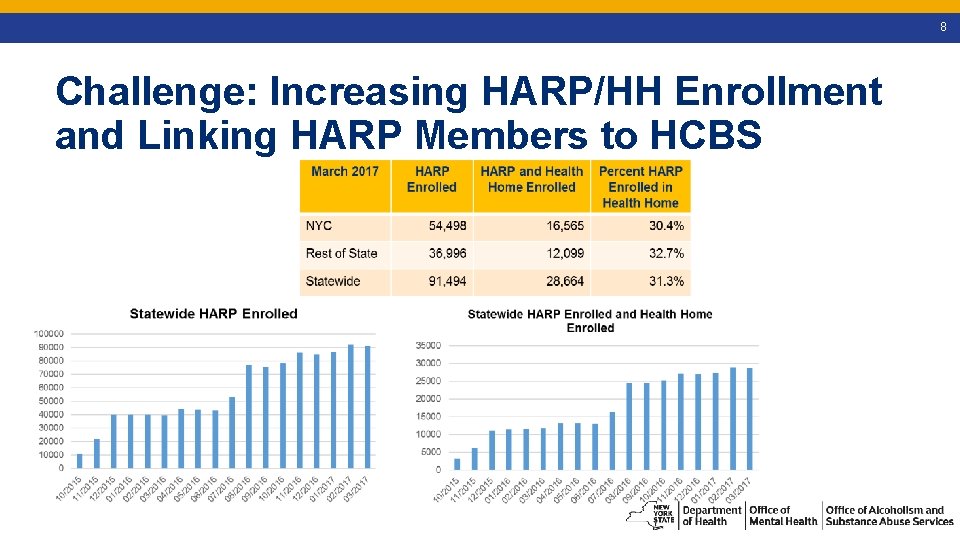
8 Challenge: Increasing HARP/HH Enrollment and Linking HARP Members to HCBS
9 Focus on Health Home Performance • State is continuing focus on Health Home performance management – ownership and accountability that is measured by performance and health outcomes • By end of June 2017 site Redesignation Visits completed for all 32 Health Homes • Includes implementation of Technical Assistance and Quality Monitoring based on outcomes • Performance Improvement Plans – Development, Implementation and Monitoring • Policy Revision and standardization • Rollout of Performance Management Program – May 2017
10 Health Home and Health and Recovery Plan (HARP)/Adult Behavioral Health (BH) Home and Community Based Services (HCBS) • Major focus on access to HCBS and for all HARP members • Emphasis on quality of care for all Health Home enrollees, including the high need/high risk behavioral health population (HARP, HH+): engagement and relationships • Increase Person-Centered Care planning, moving rehab and recovery movement forward • Streamlining and simplifying from the perspective of the individuals we serve
11 Health Home and HARP/Adult BH HBCS Implementation Challenge: Complex and Layered Assessment Process and Completing Plans of Care ü Solution: Eliminate Full CMHA as of March 7, 2017 Challenge: Low HARP/HH enrollment (30%) ü Solutions: Implementation of PSYCKES flag for HARP members not enrolled in Health Home – encourage and provide education materials to providers, including clinics, to link and enroll members in Health Home Challenge: Delayed payment for assessments, system crashes ü Solution: CMAs directly bill for CMHA fee Challenge: Link HARP members to HCBS and HCBS Provider readiness, ramp-up ü Solutions: Consumer Education initiatives (HARP, HCBS, and HH), Procedures for improving access to HCBS for members not enrolled in Health Home; development of HCBS Roadmap as training resource for CMAs and HCBS providers ; A simplified Plan of Care driven by the member’s goals, that is also integrated (coming soon)
12 Best Practices for HARP and Health Home/HCBS Linkage ü Use of Peers to engage in Health Home and the Adult BH HCBS process ü Getting to know your partners: HH Care Manager, MCO, HCBS provider ü Dedicated HARP teams (at MCO and HH Care Management Agency) ü Standardized processes (Plan Of Care, MCO, HCBS referrals) ü Care Managers that help individuals understand what HCBS can do to assist in their recovery
13 Resources Health Homes by County, Department of Health website https: //www. health. ny. gov/health_care/medicaid/program/medicaid_health_hom es/contact_information/ Behavioral Health Managed Care, Office of Mental Health website https: //www. omh. ny. gov/omhweb/bho/
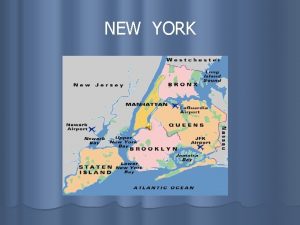
 New york, new jersey, pennsylvania, and delaware
New york, new jersey, pennsylvania, and delaware Articles of confederation strengths
Articles of confederation strengths Leanne keene french ambassador arrives from paris
Leanne keene french ambassador arrives from paris Slidetodoc.com
Slidetodoc.com Orchard 14 new hartford
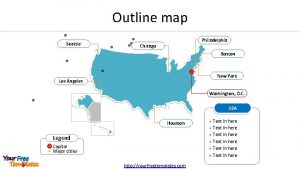
Orchard 14 new hartford Map boston to philadelphia
Map boston to philadelphia West egg and east egg
West egg and east egg Brainpop 13 colonies
Brainpop 13 colonies Nyc youth and community development
Nyc youth and community development Pathways community hub model
Pathways community hub model Isbarq
Isbarq Elements of primary health care
Elements of primary health care Care coordination ring
Care coordination ring Care coordination models
Care coordination models