CONSUMER PROTECTION ACT CPACOPRA Who is a Consumer


- Slides: 35
CONSUMER PROTECTION ACT (CPA/COPRA)
Who is a Consumer? According to Websters 1913 dictionary – “A consumer is a person who uses goods or services”
The consumer protection act is a welfare organization tilting towards the consumer just as the industrial act is in favour of the workers. The consumer protection act 1986 came into force on 15 th April 1987.
AIMS & OBJECTIVES Ø Ø Better protection of the interest of the consumer and for settlement of consumer disputes. It provides speedy and inexpensive settlement of disputes within a limited timeframe as against civil action which are expensive and take years in coming to a settlement.
WHO IS LIABLE? Ø Ø Doctors with independent practice Private hospitals charging all All hospitals having free as well as paying patients are liable to both. Doctors/Hospitals paid by insurance firms for treatment of the client or an employer for the treatment of an employee
WHO IS NOT LIABLE? Ø Ø Doctors in hospitals who do not charge their patients. Hospitals offering only free services to all patients.
THE ACT ENVISAGES A 3 TIER QUASI JUDICIAL MACHINERY 1. The District Consumer Disputes Redressal Forum at the district level. 2. State Consumer Disputes Redressal Commission at the state level. 3. National Consumer Disputes Redressal Commission at the national level.
PROCEDURE FOR LODGING A COMPLAINT Ø Ø An Individual can lodge a complaint at any centre with or without a lawyer and by paying a nominal fees. At the district level – At this forum a person can claim for compensation towards damages upto a maximum limit of Rs 5 Lakh. A district judge and two other members chair this.
n n At the state level – At this level the claim for compensation is enhanced to Rs 5 -20 lakh. A High court judge and two other members chair this. At the National level – Here the compensation is more than 20 lakh. This forum constitutes of a supreme court judge and four other members.
PREVENTIVE STEPS AGAINST LITIGATION Complaints have been lodged with the state medical council and medical council of india and there have been instances of action taken against doctors. The doctors have been prosecuted at the civil & criminal courts. The medical professionals have been excising due caution while dealing with patients due to the existence of compensation oriented forum.
When the doctor feels that the patient is suffering from some major illness in which complications are pre existing or are likely to occur, then the precautions which the doctor must take to avoid consumer protection forums are summarized as DO’s or DONT’s.
SOME DO’S Ø Ø Mention the qualification on the prescription as regulated by the Indian Medical Degrees Act 1916. Always mention date & timing of consultation. Mention age, sex & weight of a child. In case of complicated cases precisely record history of illness and substantial physical findings about the patients.
Ø Ø If the patient/attendants are erring on any accounts(history not reliable, refusing investigation, refusing admission)make a note of it or seek written refusal preferably in local language Mention the condition of patient in specific/objective term.
Ø Ø Record history of drug allergy. Mention additional precautions like avoidance of certain drugs, smoking etc if indicated. Mention whether prognosis is explained. Mention reason for deviations from standard care.
Ø Ø Mention review or follow up schedule. Mention if patient/attendants is under effect of alcohol/drugs. Mention where the patient should contact in case of the doctors non availability/emergency. In case of a particular drug/equipment is not available, make a note.
Ø Ø Routinely advise x-rays in case of injury to bones/joints. The doctors should routinely update their knowledge.
SOME DON’T’s Ø Ø Ø Do not hesitate to discuss the case with your colleagues. Do not hesitate to discuss the case with the patient/attendants. Do not write ayurvedic formulations. Do not allow substitution. Never talk ill about your colleagues despite intense professional rivalry.

Ø Do not examine the patient if the doctor is sick, exhausted or under the effect of alcohol.
CONSENT Definition – “When two or more persons agree upon a same thing in the same sense they are said to consent” as given under section 13 of Indian Contract Act of 1872.
WHO CAN GIVE CONSENT? Ø Ø For the purpose of clinical examination diagnosis and treatment, consent can be given by any person who is conscious, mentally sound above 12 years. The consent of the patient should be written from parents or guardian for a patient below 18 years.
WHEN CONSENT IS NOT VALID Ø Ø Ø Consent under fear, fraud or misinterpretation of facts. Consent given by a person who is ignorant of implications of consent. Consent given by a person under 12 years of age.
TYPES OF CONSENT 1. Implied Consent – This is used for General Practice and hospital practice like palpation, percussion, auscultation and routine sonography. But for examinations like withdrawal of blood, endoscopy, CT scan express written consent should be obtained.
2. Express Consent – Express consent may be oral or written. Oral Consent is for minor examination or theraupetic procedures, preferably in the presence of a third party. Written consent is used for all the four major diagnostic procedures -
FOUR MAJOR DIAGNOTIC PROCEDURES Ø Ø General anesthesia Surgical operations Intimate examination Examination for determining age, potency, virginity and medico legal cases.
3. Informed Consent – The patients who alleged that they did not understand the nature of medical procedure to which they gave consent have brought many actions. The information given to the patient must be explained in comprehensible non-medical terms preferably in local language.
Informed consent must be given about – a. Diagnosis b. Nature of treatment c. Risk involved d. Prospect of success e. Prognosis if procedure is not performed f. Alternative methods of treatment
WHEN INFORMED CONSENT MAY NOT BE GIVEN Ø Ø If the patient prefers not to be informed If the doctor believes it could cause significant psychological harm to the patient.
4. Proxy Consent (Substitute Consent) – All the above type of consent can take the shape of Proxy Consent, for. eg. • Parent for child • Close relative for mentally unsound/unconscious patients
SITUATIONS WHERE CONSENT MAY NOT BE OBTAINED Ø Ø Ø Medical Emergencies Notifiable disease such as AIDS/HIV Immigrants Members of armed forces New admissions to prisons In case of a person where a court may order for psychiatric examination/treatment
Ø Patient to be examined at the request of the police
SITUATIONS REQUIRING EXTRA CAUTION Ø Ø Accident and emergency department Anesthesia High risk specialties like orthopedics, gynecology etc In the field of operation
Therapeutic hazards can be avoided by – • Administration of the right drug, right dose, right route etc. • Informing patients about the potential risk of treatment.

Failure of Communication – • A doctor should inform the patient’s condition in a comprehensible language. In case of reference to another doctor, the doctor should directly communicate with the second doctor.
IN CASE OF MISHAP Ø Ø Ø Be frank and inform clearly about the mishap. Answer all queries of patient/relative and do not mind their repeated questioning. Harsh attitude and abusive language must be tolerated.
Ø After these initial responses the doctor should contact some protective organization like medical practitioners society etc.
 District forum in consumer protection act
District forum in consumer protection act Right to be heard
Right to be heard Conclusion of consumer protection act
Conclusion of consumer protection act Consumer rights objectives
Consumer rights objectives Aedilitian
Aedilitian Interpret a food chain or food web.
Interpret a food chain or food web. Introduction of consumer protection
Introduction of consumer protection Consumer protection manitoba
Consumer protection manitoba Who is consumer
Who is consumer Consumer purchasing strategies and legal protection
Consumer purchasing strategies and legal protection Chapter 6 consumer purchasing and protection
Chapter 6 consumer purchasing and protection Act 1 act 2 act 3
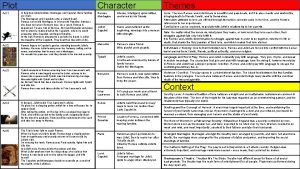
Act 1 act 2 act 3 Domestic and family violence protection act 2012
Domestic and family violence protection act 2012 Child protection reform amendment act 2017
Child protection reform amendment act 2017 Data protection act in health and social care settings
Data protection act in health and social care settings Data protection act 1998 ict
Data protection act 1998 ict Child protection and toy safety act
Child protection and toy safety act Child care and protection act 3 of 2015
Child care and protection act 3 of 2015 Bbc bitesize data protection act
Bbc bitesize data protection act Florida information protection act of 2014
Florida information protection act of 2014 Cncp and ccl
Cncp and ccl Archaeological resources protection act of 1979
Archaeological resources protection act of 1979 Omnibus adult protection act
Omnibus adult protection act Paul d coverdell teacher protection act
Paul d coverdell teacher protection act Teach ict data protection act
Teach ict data protection act Wildlife protection act
Wildlife protection act Domestic and family violence protection act 2012
Domestic and family violence protection act 2012 Decomposer in the sahara desert
Decomposer in the sahara desert Characteristics of consumer behavior
Characteristics of consumer behavior Cengage
Cengage Consumer markets and consumer buyer behavior
Consumer markets and consumer buyer behavior Consumer behaviour research process
Consumer behaviour research process Ra no. 9344
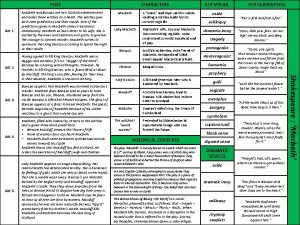
Ra no. 9344 Act 6 act 5
Act 6 act 5 Modifier of human act
Modifier of human act Title act interior design
Title act interior design