Childrens Outcomes Research Program The Childrens Hospital Aurora

![Vaccine Financing “[Whether to participate in VFC] basically boiled down to again taking federal Vaccine Financing “[Whether to participate in VFC] basically boiled down to again taking federal](https://slidetodoc.com/presentation_image_h2/6e64ad1476e0076a1aed55aebe3662f0/image-15.jpg)
- Slides: 31
Children’s Outcomes Research Program The Children’s Hospital Aurora, CO Department of Pediatrics Univ. of Colorado Denver School of Medicine Feasibility of Adolescent Vaccination in Non. Traditional Settings: A Qualitative Study in Denver, Colorado, 2007 - 2008 Matthew F. Daley, MD
Disclosures No relevant financial relationships with any commercial interests are present No reference will be made to the use of medications in manners not licensed by the Food and Drug Administration
Background § 3 vaccines targeted at adolescents (MCV 4, Tdap, HPV) recently licensed § Renewed focus on addressing challenges to adolescent immunization delivery § One challenge: adolescent health care utilization • Most adolescents identify a source of primary care • No visits within year: 18% to 32% • Adolescents who are poor, uninsured, from racial/ethnic minority groups less likely to routinely access care Ref: Klein et al, Arch Pediatr Adolesc Med, 1998; Yu et al, J Adolesc Health, 2001; Newacheck et al, Health Serv Res, 2003

Non-Traditional Settings § Because adolescents underutilize primary care, increased attention to immunization in nontraditional settings § Non-traditional settings: • Working definition: settings that do not typically serve as comprehensive medical and vaccination homes for their patients • Broad: may include settings, such as school-based health centers, that do provide comprehensive care § Adolescent immunization delivery in non-traditional settings not extensively studied Ref: Schaffer et al, Pediatrics, 2008
Study Objectives In several different types of non-traditional settings, use standard qualitative techniques to explore: § Adolescent immunization delivery processes § Perceived advantages/disadvantages of adolescent immunization in these settings § Perceived advantages/disadvantages of HPV immunization
Study Setting § Conducted May 2007 -February 2008 § Key informant interviews of administrators and clinicians in 4 settings, metro Denver, CO: • • School-based health centers (SBHC) Public health departments (PH) Independent family planning clinics (FP) Emergency departments/urgent care clinics (ED) § Within public health, interviews in immunization, FP, sexually transmitted diseases (STD) clinics § FP/STD clinics typically combined in PH
Participant Recruitment § Potential study sites identified by a variety of means: • Local clinic listings (internet, telephone books) • Sites’ recommendation of other sites • Investigators’ knowledge and contacts in community § A key initial contact identified at each site § Initial contact referred study team to other key informants within institution
Analytic Methods § Interviews digitally recorded, transcribed, imported into ATLAS. ti qualitative software § Analyzed using standard qualitative techniques, including both template and editing approaches Ref: Crabtree and Miller, Sage Publications, 1999
Results: Settings for Interviews § 31 key informant interviews conducted: • 9 interviews in 4 school-based health centers • 14 interviews in 4 public health departments • 5 interviews in a large network of family planning clinics • 3 interviews in 2 emergency department/ urgent care clinics
Characteristics of Sites and Informants § Majority of patients served by study sites were publicly insured or uninsured § Key informants: • 27 of 31 female • Most either nurse practitioners or physician assistants • Most with >10 years clinical experience
Adolescent Immunization Delivery § All sites offered one or more immunizations to adolescents § SBHCs and PH immunization clinics offered all routinely recommended vaccines § Family planning and STD clinics within public health offered limited vaccines (e. g. Hep B) § Emergency/urgent care primarily provided tetanus-containing vaccines
Process of Immunization Delivery § Assessing vaccination status: • Written records • Immunization information systems (registries) § Parental consent: required in all settings except some family planning and STD settings
Parental Consent “We get the parents to sign for all vaccines at the time of registration for the school year” (SBHC) “[Adolescents] are able to consent for testing and treatment of STDs and hepatitis B is an STD. They are able to consent on their own” (Combined FP/STD clinic within public health)
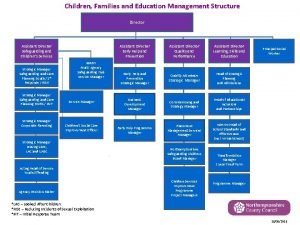
Financing of Vaccines Given § Majority of sites participated in Vaccines for Children (VFC) program § Not participating in VFC: • Emergency department • Independent family planning clinic network • Some FP/STD clinics within public health § Many sites did not have processes for billing private insurance for vaccines given
![Vaccine Financing Whether to participate in VFC basically boiled down to again taking federal Vaccine Financing “[Whether to participate in VFC] basically boiled down to again taking federal](https://slidetodoc.com/presentation_image_h2/6e64ad1476e0076a1aed55aebe3662f0/image-15.jpg)
Vaccine Financing “[Whether to participate in VFC] basically boiled down to again taking federal or state dollars and then being accountable for everything else that comes with that” (Independent FP clinic network) “We are not set up, we are not capable, we do not have the feasibility to bill for anything we do for anybody” (FP/STD clinic within public health)
Advantages of Adolescent Vaccination in These Settings § Most sites described benefits such as convenience, saving parents’ time, easy access to adolescents in schools § Some sites described potential to reach adolescents who might not otherwise be seen for vaccination
Perceived Advantages “I could see us being a benefit to the patients in terms of getting them immunized because this may be the only time they come in and a lot of patients do use us only” (ED) “It’s easier. Parents don’t have to take time off from work. We chase [the students] around!” (SBHC) “Providing them with the whole gamut of preventive health services is very important because for many of them we are their only provider” (SBHC)
Disadvantages of Adolescent Vaccination in These Settings § Challenges across multiple types of settings: • • Competing clinical priorities Staff knowledge and demands on staff time Infrastructure issues such as vaccine storage Vaccine tracking and potential for overimmunization § In ED settings only: perception that offering vaccines other than tetanus did not fit with overall clinical mission
Perceived Challenges with Vaccine Knowledge and Tracking “If you don’t keep updated on your vaccines…it is going to take you twice as long to draw them up and figure out what you are actually giving than it would be for anybody else. And I think your chance of error would be greater” (ED) “The STD clinic doesn’t have access to [the state registry] and it takes time to [check the registry]. You know, you are giving somebody a tetanus and maybe they got it before and so you can be overimmunizing people” (FP/STD clinic within public health)
Perceived Lack of Fit with Mission “We are an Emergency Department. Our mission is to deal with emergent issues and visits. Concern about that type of preventive care is really outside our scope. ” (ED) “We tell them you have to go to your doctor [for routine vaccines] and that’s probably the way it is going to be. ” (ED)
HPV Vaccination: Advantages in These Settings § Some sites described potential benefits such as synergy with mission, convenience, providing an opportunity for additional education § FP/STD clinics, in particular, described benefits related to expertise in sexually transmitted infections and anonymity
Perceived Advantages (HPV) “If they have a reaction, they just have to walk down to the clinic and say, ‘my arm is red and swollen. ’ It is not a matter of calling the doctor and waiting [to be seen. ]” (SBHC) “Maybe there is a certain amount of anonymity about coming to a clinic that is not your normal primary care clinic. ” (FP/STD clinic in public health) “It is easy to talk to them about cervical cancer because cervical cancer is really our forté. We understand it. It would be easy to counsel an adolescent about that. ” (FP/STD clinic in public health)
HPV Vaccination: Perceived Barriers in These Settings § § Vaccine financing Parental consent issues Vaccine tracking and the need for 3 doses Need for additional staff training and infrastructure
Perceived Barriers to Offering HPV “It makes perfect sense to us [to offer HPV. ] To our attorney, he just didn’t feel like that was covered under the role of a Title X clinic. ” (FP/STD clinic in public health) “We don’t offer [HPV vaccine] because we don’t have funds to pay for it. So we refer kids to the immunization clinic or community health centers” (FP/STD clinic in public health)
Perceived Barriers to Offering HPV “We have to kind of wrestle with…do we require parental consent [for HPV vaccine. ] A lot of parents wouldn’t want their children coming to family planning to begin with and then also receiving a vaccine they didn’t consent to…so it’s really a philosophical and policy decision that we have yet to make. ” (FP/STD clinic in public health) “It is not practical to provide 3 doses of anything. We are not the medical home. ” (ED)
Limitations § Standard qualitative approach is to conduct interviews until saturation of ideas reached § While saturation reached for SBHCs, PH clinics, may not have been reached for: • Independent FP clinics: only one large network in Colorado from which to sample • EDs: few agreed to participate (more interviews planned) § Other types of non-traditional settings (pharmacies, teen clinics, retail-based clinics) not examined
Summary of Findings § Many non-traditional settings already providing at least some immunizations to adolescents § SBHCs reported providing comprehensive vaccination services § Challenges around vaccine financing common: • Most sites participated in VFC • Non-VFC sites reported barriers to funding vaccines for VFC-eligible patients • Many sites did not bill private insurance, limiting ability to vaccinate privately insured
Summary of Findings § For some sites, perceived lack of fit of routine adolescent vaccination with mission § However, many sites recognized opportunities to immunize high-risk adolescents, such as those without medical homes, those who only seek care in non-traditional settings
Implications § Non-traditional settings are diverse; some may have greater barriers to comprehensive adolescent vaccination § Additional quantitative work needed to better define immunization delivery capacity in nontraditional settings with high potential (e. g. SBHCs) § Non-traditional settings may serve as an immunization “safety-net” for high-risk adolescents, particularly if issues of vaccine financing resolved
Research Collaborators University of Colorado Denver § § § Allison Kempe, MD, MPH Deborah Main, Ph. D Lori A. Crane, Ph. D, MPH Carolyn Nowels, MSPH Jennifer Barrow, MSPH Jennifer L. Pyrzanowski, BA Centers for Disease Control and Prevention § C. Robinette Curtis, MD, MPH
Acknowledgments This investigation was funded by the Centers for Disease Control and Prevention
 Aurora eap
Aurora eap Program specific outcomes nba
Program specific outcomes nba Diabetes prevention program outcomes study
Diabetes prevention program outcomes study Expected results research proposal example
Expected results research proposal example Expected results research proposal example
Expected results research proposal example Objectives of hospital pharmacy
Objectives of hospital pharmacy Moli texas childrens
Moli texas childrens Christian children's fund inc
Christian children's fund inc Childrens services
Childrens services Childrens services walsall
Childrens services walsall Levine childrens
Levine childrens 23 april international children's day turkey
23 april international children's day turkey Multi agency assessment
Multi agency assessment Childrens literature quiz
Childrens literature quiz Manchester childrens university
Manchester childrens university Longman picture dictionary
Longman picture dictionary Black childrens memorial
Black childrens memorial Baby temperature chart
Baby temperature chart History of childrens literature
History of childrens literature Colorado children's book award
Colorado children's book award Aurora and cephalus story
Aurora and cephalus story Nihilismo
Nihilismo Aurora multi master
Aurora multi master Aurora espinosa
Aurora espinosa Reflexia totala in natura
Reflexia totala in natura Kelemen auróra
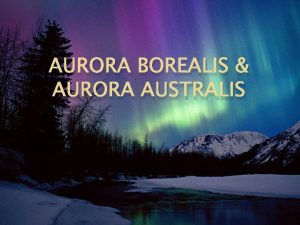
Kelemen auróra Aurora borealis kada se javlja
Aurora borealis kada se javlja Driveway installation east aurora, ny
Driveway installation east aurora, ny Sugars aurora
Sugars aurora Oh que saudades que tenho
Oh que saudades que tenho Aurora boreal letra
Aurora boreal letra Isccupra
Isccupra