Chapter 23 Suicide Suicide Approximately 75 Americans commit

- Slides: 24
Chapter 23 Suicide
Suicide • Approximately 75 Americans commit suicide every day. • In 2001: – Eleventh leading cause of death – 30, 622 completed suicides – Third leading cause of death in 14 to 25 year olds – Highest risk age group: 65 years and older (risk increases as age increases)
Suicide Facts • Suicides outnumber homicides by 3: 2. • Suicide by firearm is the most common method for both men and women. • Occupations with the highest risk of suicide: – Physicians and dentists – Nursing and social work also with elevated risk
Suicide in the Elderly • ~75% of depressed older adults are not receiving treatment. • Two thirds of adults older than 60 years were in relatively good physical health when they died by suicide. • 66% to 90% of elderly suicide victims had at least one psychiatric diagnosis; two thirds of these diagnoses were lateonset, single-episode depression.
Suicide in Youth • Firearms are the most commonly used method. • The largest increase in suicide rates since 1980 has been among black males aged 10 to 19 years. • Self-report surveys show that nationwide, one in five high school students has seriously considered attempting suicide in the preceding 12 months.
Attempted Suicide • There an estimated 8 to 25 attempted suicides for each suicide death. • Women attempt suicide more than men. • Most adolescent suicide attempts are precipitated by interpersonal conflicts.
Comorbidity • Suicide occurs more frequently among those with: – Major depression – Bipolar disorder – Schizophrenia – Alcohol and substance use disorders – Borderline and antisocial personality disorders – Panic disorder
• Suicide is not necessarily synonymous with a mental disorder. • The act of purposeful self-destruction represented by taking one's own life is usually accompanied by intense feelings of pain and hopelessness, coupled with the belief that no solutions exist.
Biological Theory • Low levels of serotonin – Low serotonin levels are related to depressed mood. • Suicidal behavior seems to run in families. • Physical illness is considered a factor in 11% to 51% of suicides.
Psychosocial Factors • Freud: Aggression turned inward • Menninger: – The wish to kill – The wish to be killed – The wish to die • Aaron Beck: Hopelessness as central emotional factor
Psychosocial Factors • Experiences in which people are more likely to act out suicidal fantasies: – Loss of love – Narcissistic injury (humiliation, loss of job, threat of incarceration) – Overwhelming moods such as rage or guilt – Identification with a suicide victim (copycat suicide)

Cultural Factors • European Americans with twice the suicide rate of minorities • Protective factors for minorities – African Americans • Religion, role of the extended family – Hispanic Americans • Roman Catholic religion, importance of extended family – Asian Americans • Adherence to cultural beliefs that tend to emphasize interdependence between the individual and society
Assessment: Overt Statements • “I can't take it anymore. ” • “Life isn't worth living anymore. ” • “I wish I were dead. ” • “Everyone would be better off if I died. ”
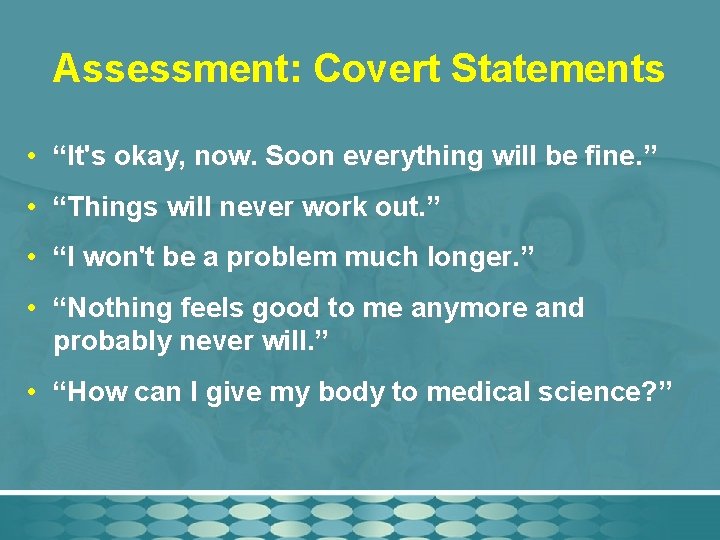
Assessment: Covert Statements • “It's okay, now. Soon everything will be fine. ” • “Things will never work out. ” • “I won't be a problem much longer. ” • “Nothing feels good to me anymore and probably never will. ” • “How can I give my body to medical science? ”
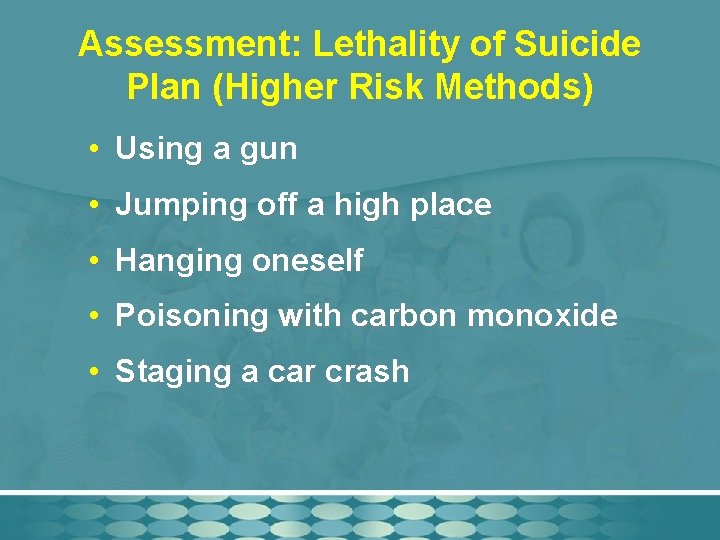
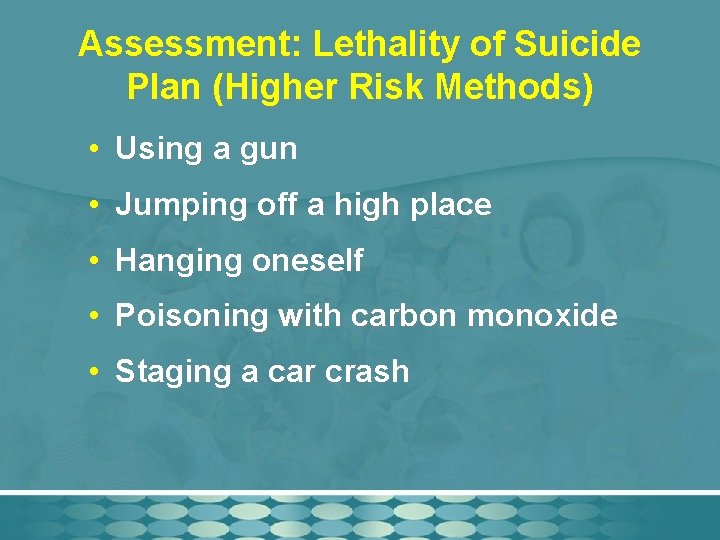
Assessment: Lethality of Suicide Plan (Higher Risk Methods) • Using a gun • Jumping off a high place • Hanging oneself • Poisoning with carbon monoxide • Staging a car crash
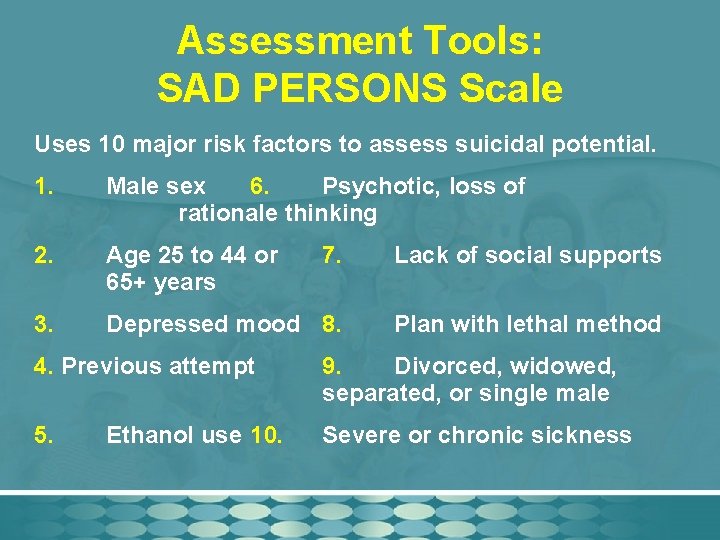
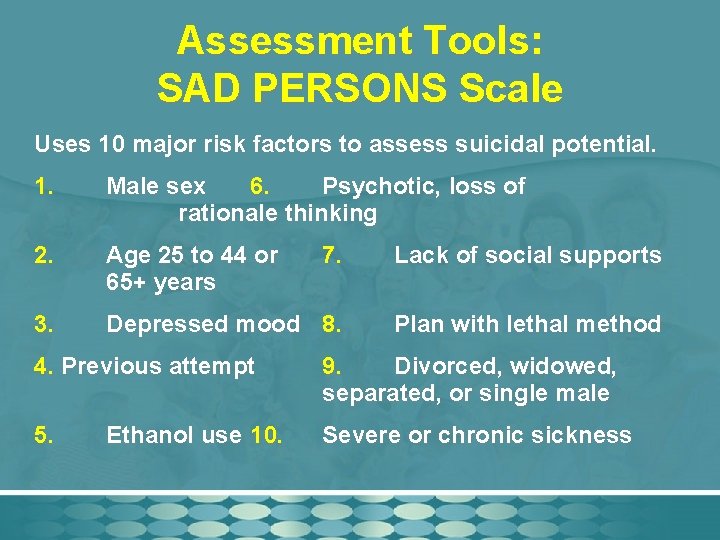
Assessment Tools: SAD PERSONS Scale Uses 10 major risk factors to assess suicidal potential. 1. Male sex 6. Psychotic, loss of rationale thinking 2. Age 25 to 44 or 65+ years 7. Lack of social supports 3. Depressed mood 8. Plan with lethal method 4. Previous attempt 9. Divorced, widowed, separated, or single male 5. Severe or chronic sickness Ethanol use 10.
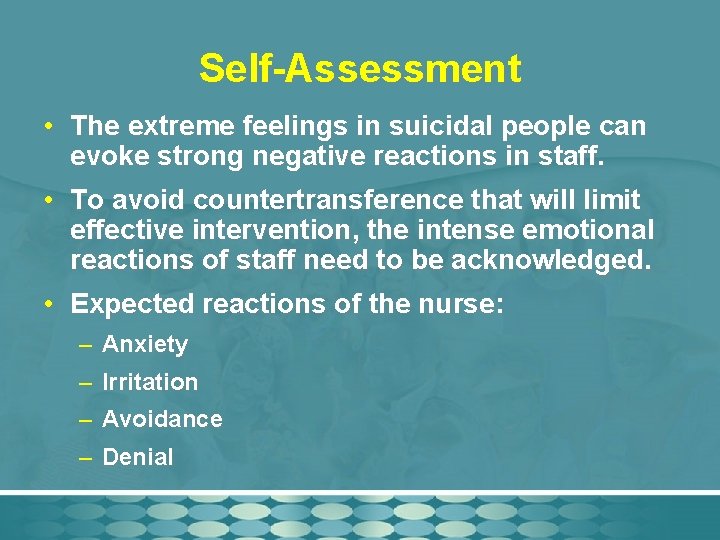
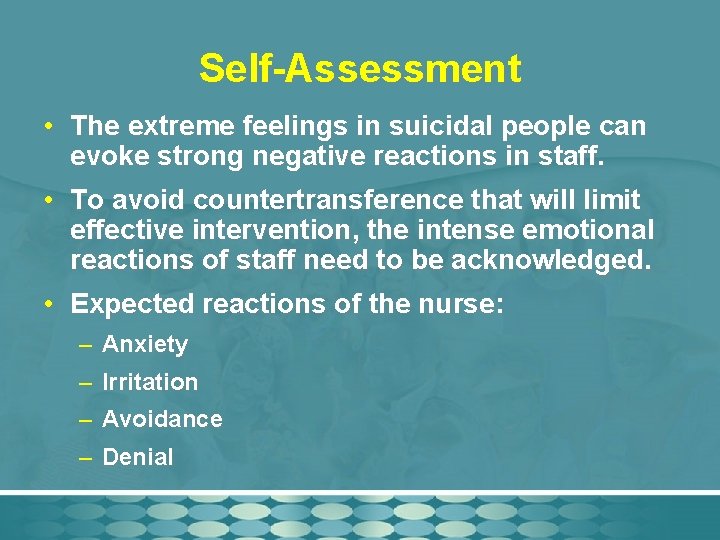
Self-Assessment • The extreme feelings in suicidal people can evoke strong negative reactions in staff. • To avoid countertransference that will limit effective intervention, the intense emotional reactions of staff need to be acknowledged. • Expected reactions of the nurse: – Anxiety – Irritation – Avoidance – Denial
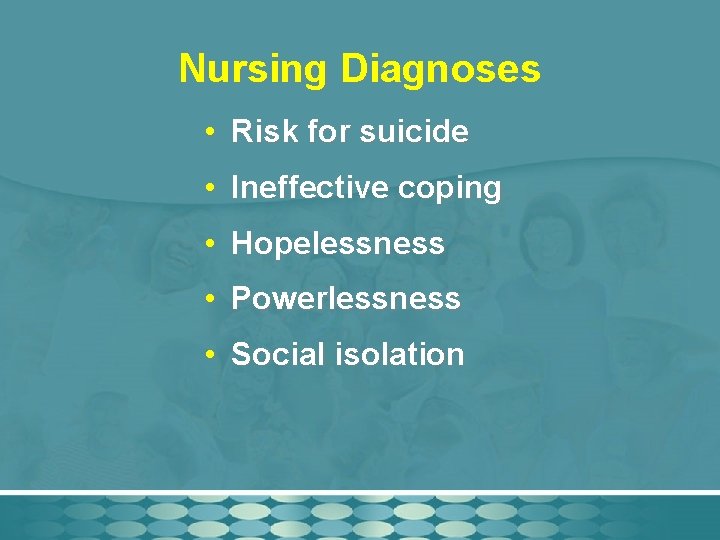
Nursing Diagnoses • Risk for suicide • Ineffective coping • Hopelessness • Powerlessness • Social isolation
Levels of Intervention • Primary: activities that provide support, information, and education to prevent suicide • Secondary: treatment of the actual suicidal crisis • Tertiary: interventions with the family and friends of a person who has committed suicide to reduce the traumatic aftereffects
Basic Level Interventions • Milieu therapy with suicidal precautions • Counseling: Establish an alliance • Health teaching: Include family • Case management: Community services • Psychobiological interventions: Meds
Advanced Practice Interventions • Psychotherapy • Clinical supervision • Consultation
Survivors of Completed Suicide: Postintervention • Surviving friends and family – Refer to support groups. – Show empathy. • Staff – Conduct a psychological postmortem assessment.
Evaluation • Evaluation of a suicidal client is an ongoing part of assessment. • Be alert for sudden behavioral/mood changes – Increased cheerfulness and energy – Worsening depression or anger • Assess for improved communication of thoughts and feelings as well as increased social network.
Take all suicidal ideation and gestures seriously.