Changing Nature of Managed Care OrganizationProvider Relationships WAMSS



- Slides: 15
Changing Nature of Managed Care Organization-Provider Relationships WAMSS Conference April 28, 2017 Andrew Nelson, Vice President, Provider Network Management Molina Healthcare of Washington
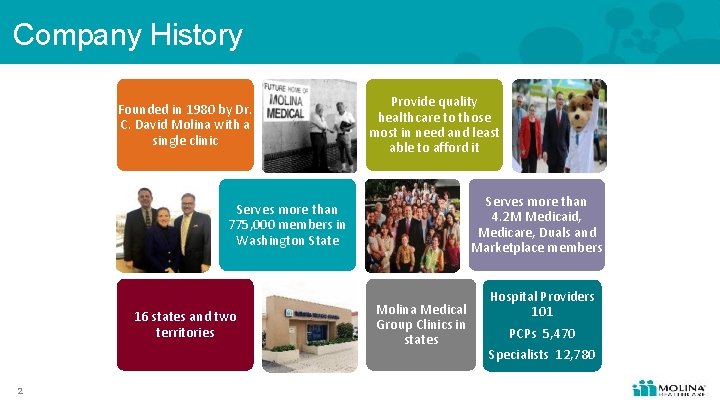
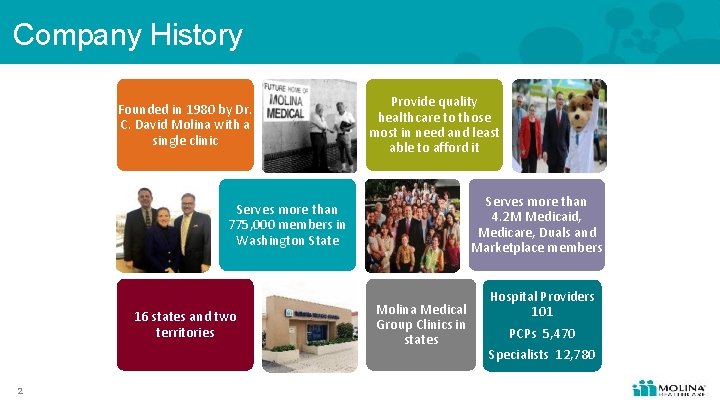
Company History Founded in 1980 by Dr. C. David Molina with a single clinic Provide quality healthcare to those most in need and least able to afford it Serves more than 4. 2 M Medicaid, Medicare, Duals and Marketplace members Serves more than 775, 000 members in Washington State 16 states and two territories 2 Molina Medical Group Clinics in states Hospital Providers 101 PCPs 5, 470 Specialists 12, 780

HCA’s “Value-Based Purchasing” goals 2021 90% state-financed 50% commercial In 2021, at least 90% of state-financed health care payments and 50% of commercial health care payments are linked to quality and value through Alternative Payment Mechanisms (APM) (Categories 2 c-4 b) Washington’s annual health care cost growth will be below the national health expenditure trend. Tools to accelerate VBP and health care transformation: • • • 3 2014 Legislation directing HCA to implement VBP strategies State Innovation Model (SIM) Round 2 grant, 2015 -2019 DSRIP Medicaid Transformation Demonstration Project, 2017 -2021
What is “Value”? What is “Paying for Value? ” 4 • • • Patient experience HEDIS Avoidable emergency room visits or readmissions • • Medical cost ratio Per member per month
Provider relationships focus on value • Emerging focus on specific populations – Share, not shed, risk with providers who manage populations with complex needs, AH Blind Disabled and Medicare (DSNP) • Evolution from volume to value-based relationships – Focus on long-term relationships, not just ‘contracts’ – Path-to-Value – Gain-sharing and risk-sharing on population –based outcomes performance. We have capitation arrangements with some integrated delivery systems – Not all providers are ready – Meet providers where they are at and start there • Increasing transparency into Provider Performance – Quality outcomes, cost, member satisfaction – Member self-direction & choice of provider and health plan • Aggregation of groups combine forces to create scale 5
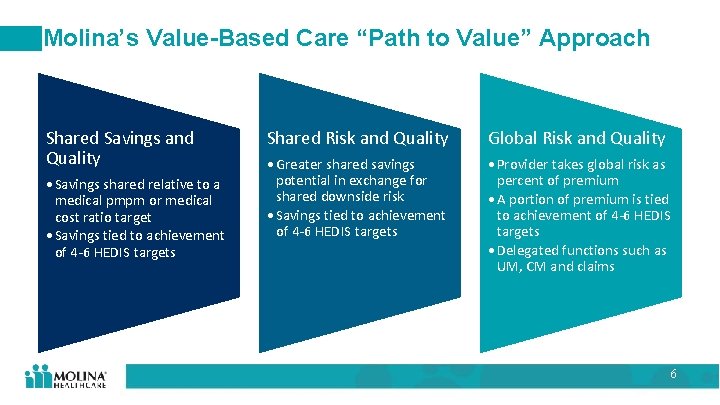
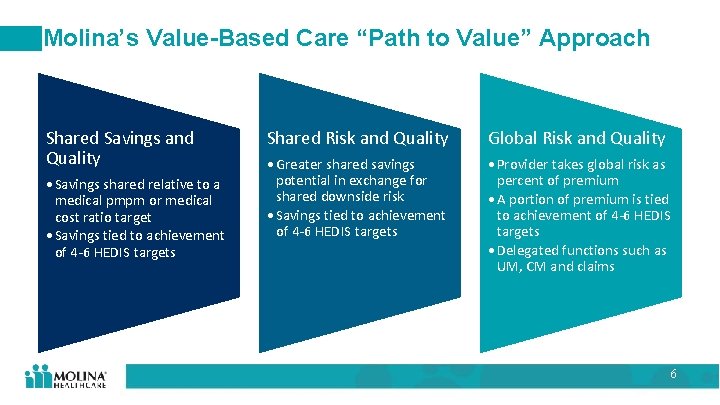
Molina’s Value-Based Care “Path to Value” Approach Shared Savings and Quality • Savings shared relative to a medical pmpm or medical cost ratio target • Savings tied to achievement of 4 -6 HEDIS targets Shared Risk and Quality Global Risk and Quality • Greater shared savings potential in exchange for shared downside risk • Savings tied to achievement of 4 -6 HEDIS targets • Provider takes global risk as percent of premium • A portion of premium is tied to achievement of 4 -6 HEDIS targets • Delegated functions such as UM, CM and claims 6

Challenges and opportunities in achieving a successful Value -Based Care relationship 7
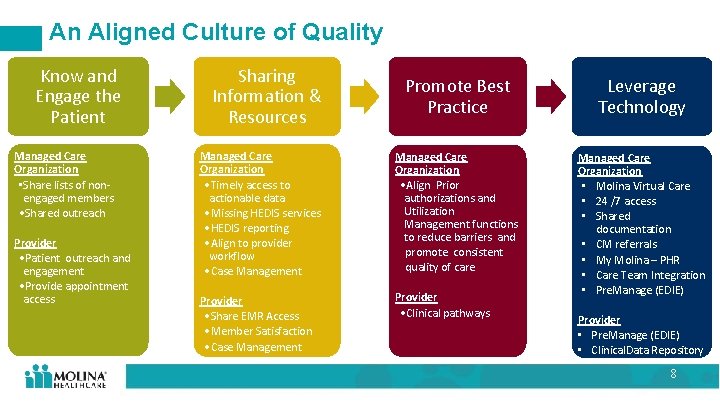
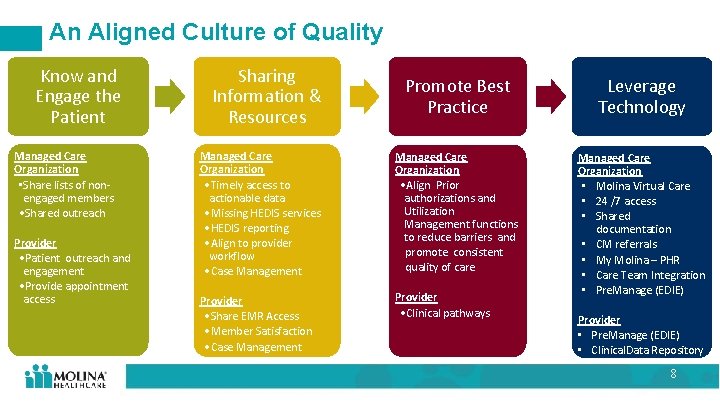
An Aligned Culture of Quality Know and Engage the Patient Managed Care Organization • Share lists of nonengaged members • Shared outreach Provider • Patient outreach and engagement • Provide appointment access Sharing Information & Resources Promote Best Practice Leverage Technology Managed Care Organization • Timely access to actionable data • Missing HEDIS services • HEDIS reporting • Align to provider workflow • Case Management Managed Care Organization • Align Prior authorizations and Utilization Management functions to reduce barriers and promote consistent quality of care Provider • Share EMR Access • Member Satisfaction • Case Management Provider • Clinical pathways Managed Care Organization • Molina Virtual Care • 24 /7 access • Shared documentation • CM referrals • My Molina – PHR • Care Team Integration • Pre. Manage (EDIE) Provider • Pre. Manage (EDIE) • Clinical. Data Repository 8
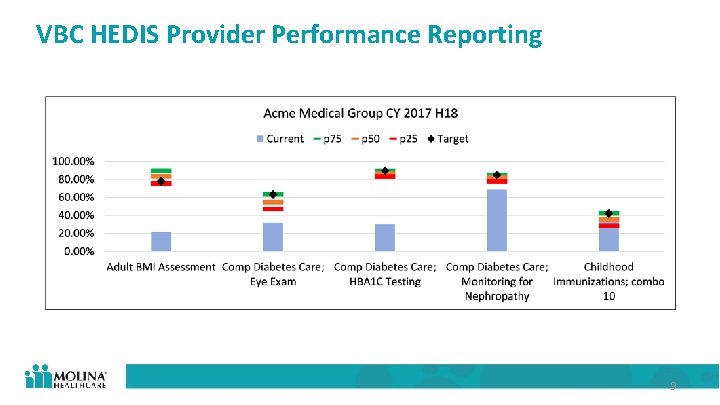
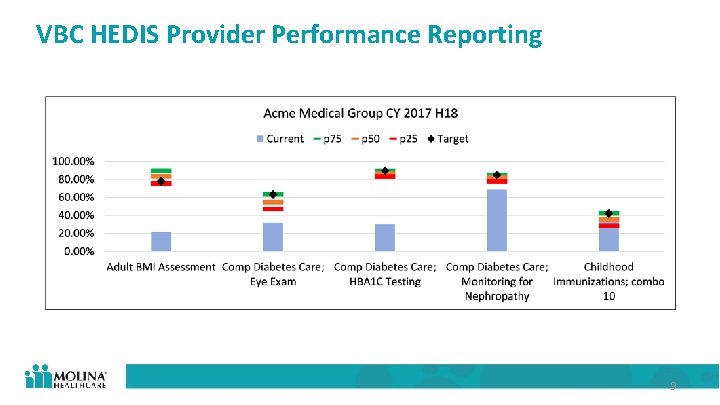
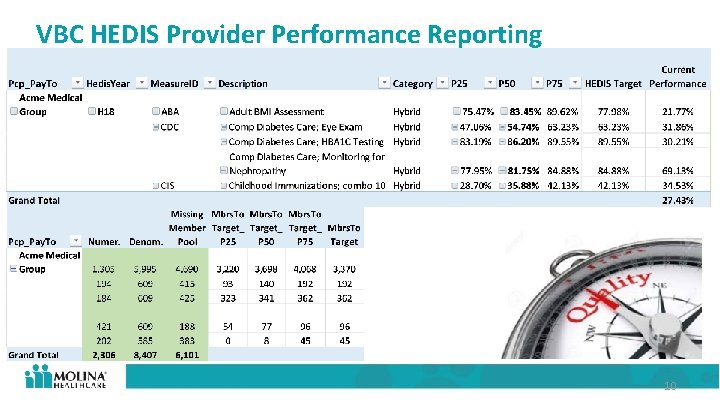
VBC HEDIS Provider Performance Reporting 9
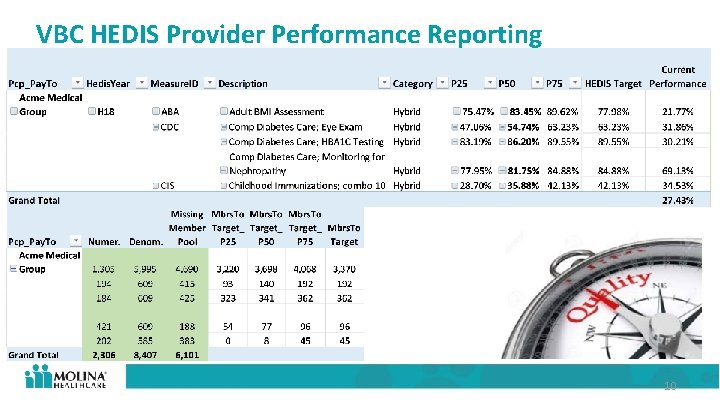
VBC HEDIS Provider Performance Reporting 10
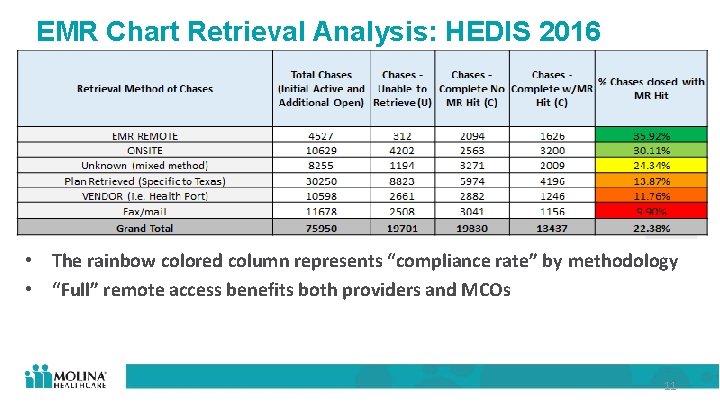
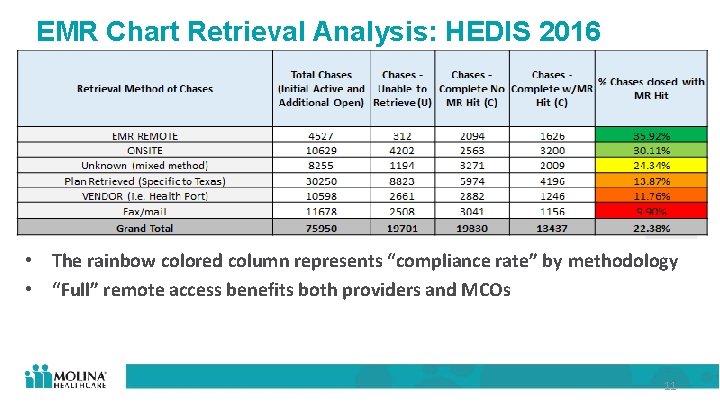
EMR Chart Retrieval Analysis: HEDIS 2016 • The rainbow colored column represents “compliance rate” by methodology • “Full” remote access benefits both providers and MCOs 11
VBC Medical Cost Provider Performance Reporting Key Data Categories • Member Months • Premium • Capitation Amounts • Care Coordination Costs • Inpatient Hospital • Outpatient Hospital • Professional Services • Rx • Incurred But Not Reported Claims • Medical Cost Ratio 12
Future of Strong MCO-Provider Relationships • Open communication on common goals Quadruple Aim • Quality focused approach • Establishing trust and credibility • Focus on the relationship just the contract not 13
Contact information Andrew Nelson Molina Healthcare of Washington Andrew. nelson@molinahealthcare. com 14

Questions?
 Wamss
Wamss Wamss
Wamss Wamss
Wamss Ppo managed care
Ppo managed care Managed care 101
Managed care 101 Care continuum prior authorization
Care continuum prior authorization Apple health managed care plans
Apple health managed care plans Nathan nau dhcs
Nathan nau dhcs Managed care is categorized according to six models
Managed care is categorized according to six models History of managed care
History of managed care Gina stinson
Gina stinson Managed care 101
Managed care 101 Department of managed health care california
Department of managed health care california Cea registry
Cea registry Amcp osu
Amcp osu Primary secondary tertiary health care definition
Primary secondary tertiary health care definition