MA 105 Chapter 3 Managed Health Care Lecture
- Slides: 15
MA 105 Chapter 3: Managed Health Care Lecture Notes Understanding Health Insurance: A Guide to Billing and Reimbursement, 2020, Michelle A. Green.
History of Managed Care pg. 49 Managed care was developed as a way to provide affordable, comprehensive, prepaid health care services to enrollees, also called subscribers or policyholders, who are employees and dependents who join a managed care plan and are also known as beneficiaries in private insurance plans.
Managed Care Organizations pg. ’s 52 -53 Unlike traditional fee-for-service plans, which reimburse providers for individual health care services rendered, managed care is financed according to a method called capitation. Capitation: providers accept pre-established payments for providing health care services to enrollees over a period of time (usually one year). If the physician provides services that cost less than the capitation amount, there is a profit (which the physician keeps). If services provided to subscribers cost more than the capitation amount, the physician loses money.
Primary Care Providers pg. 53 The primary care provider (PCP) is responsible for supervising and coordinating health care services for enrollees and approves referrals to specialists and inpatient hospital admissions (except in emergencies). The PCP services as a gatekeeper by providing essential health services at the lowest possible cost, avoiding nonessential care, and referring patients to specialists.
Quality Assurance & Utilization Management pg. 53 QA Managed care plans that are “federally qualified” and those that must comply with state quality review mandates (laws) are required to establish quality assurance programs. A quality assurance program includes activities that assess the quality of care provided in a health care setting. UR Managed care plans implement utilization management (or utilization review) as a method of controlling health care costs and quality of care. The appropriateness, efficiency, and medical necessity of health care provided to patients is reviewed on a prospective and retrospective basis. Some managed care plans contract out utilization management services to a utilization review organization (URO), an entity that establishes a utilization management program and performs external utilization review services.
Second Surgical Opinions pg. 55 Prior to scheduling elective surgery, managed care plans often require a second surgical opinion (SSO); that is a second physician is asked to evaluate the necessity of surgery and recommend the most economical, appropriate facility in which to perform the surgery (outpatient clinic or doctor’s office versus inpatient hospitalization).
Physician Incentives pg. 56 Physician incentives include payments made directly or indirectly to health care providers to encourage thme to reduce or limit services (e. g. discharge an inpatient from the hospital more quickly) so as to save money for the managed care plan.
Managed Care Models pg. 56 Managed care can now be categorized according to six models: 1. Exclusive provider organization (EPO) 2. Integrated delivery system (IDS) 3. Health maintenance organization (HMO) a) Direct contract model b) Group model c) Individual (or Independent) practice association (IPA) d) Network model e) Staff Model 4. Point-of-service plan (POS) 5. Preferred provider organization (PPO) 6. Triple option plan
Health Maintenance Organization (HMO) pg. 57 - 58 A health maintenance organization (HMO) is an alternative to traditional group health insurance coverage and provides comprehensive health care services to voluntarily enrolled members on a prepaid basis. HMOs provide preventive care services to promote “wellness” or good health, thus reducing the overall cost of medical care. A primary care provider (PCP) assigned to each subscriber is responsible for coordinating health care services and referring subscribers to other health care providers. There are 5 HMO models 1. Direct contract model 2. Group model 3. Individual practice association 4. Network model 5. Staff model
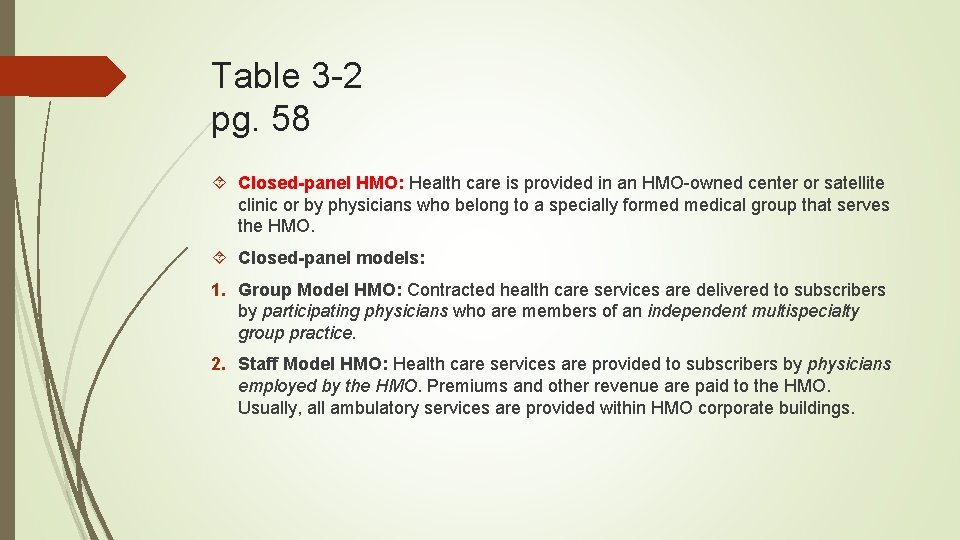
Table 3 -2 pg. 58 Closed-panel HMO: Health care is provided in an HMO-owned center or satellite clinic or by physicians who belong to a specially formed medical group that serves the HMO. Closed-panel models: 1. Group Model HMO: Contracted health care services are delivered to subscribers by participating physicians who are members of an independent multispecialty group practice. 2. Staff Model HMO: Health care services are provided to subscribers by physicians employed by the HMO. Premiums and other revenue are paid to the HMO. Usually, all ambulatory services are provided within HMO corporate buildings.
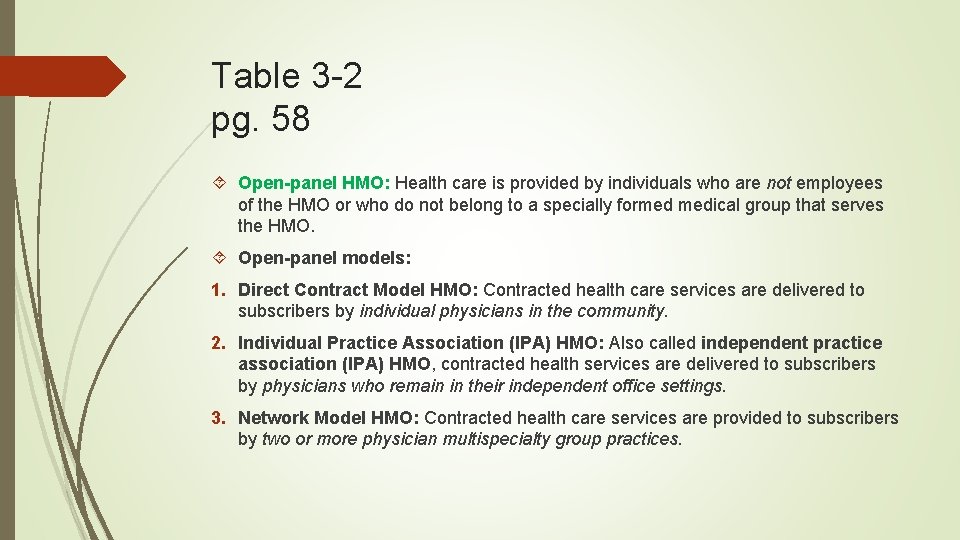
Table 3 -2 pg. 58 Open-panel HMO: Health care is provided by individuals who are not employees of the HMO or who do not belong to a specially formed medical group that serves the HMO. Open-panel models: 1. Direct Contract Model HMO: Contracted health care services are delivered to subscribers by individual physicians in the community. 2. Individual Practice Association (IPA) HMO: Also called independent practice association (IPA) HMO, contracted health services are delivered to subscribers by physicians who remain in their independent office settings. 3. Network Model HMO: Contracted health care services are provided to subscribers by two or more physician multispecialty group practices.
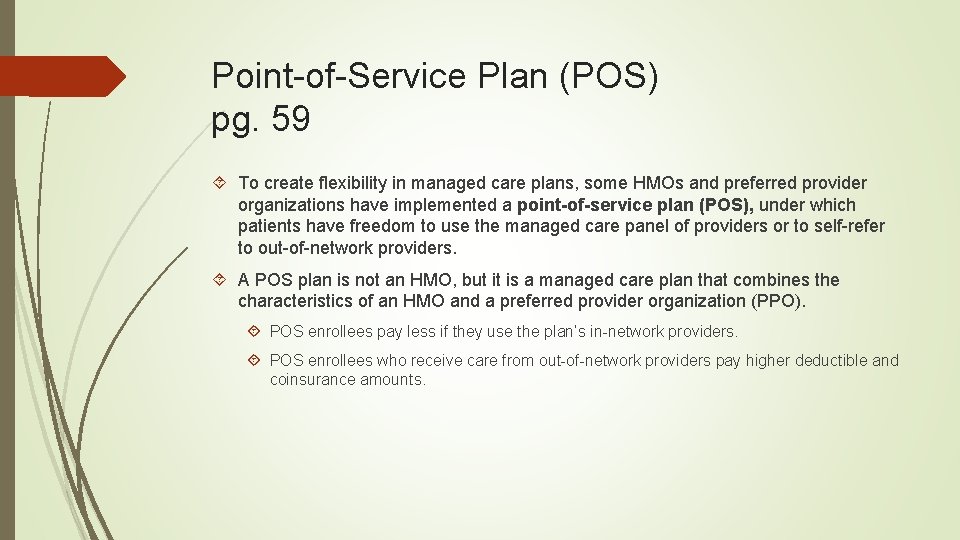
Point-of-Service Plan (POS) pg. 59 To create flexibility in managed care plans, some HMOs and preferred provider organizations have implemented a point-of-service plan (POS), under which patients have freedom to use the managed care panel of providers or to self-refer to out-of-network providers. A POS plan is not an HMO, but it is a managed care plan that combines the characteristics of an HMO and a preferred provider organization (PPO). POS enrollees pay less if they use the plan’s in-network providers. POS enrollees who receive care from out-of-network providers pay higher deductible and coinsurance amounts.
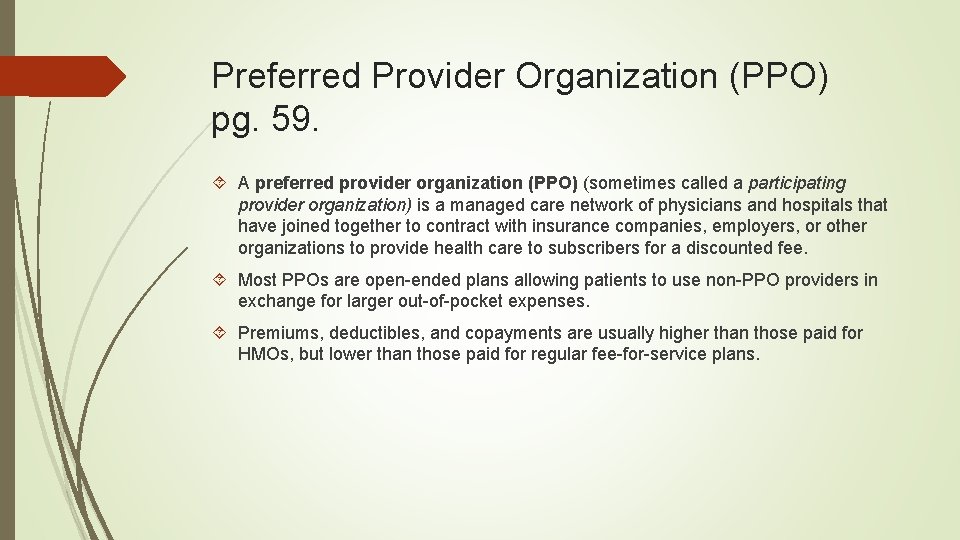
Preferred Provider Organization (PPO) pg. 59. A preferred provider organization (PPO) (sometimes called a participating provider organization) is a managed care network of physicians and hospitals that have joined together to contract with insurance companies, employers, or other organizations to provide health care to subscribers for a discounted fee. Most PPOs are open-ended plans allowing patients to use non-PPO providers in exchange for larger out-of-pocket expenses. Premiums, deductibles, and copayments are usually higher than those paid for HMOs, but lower than those paid for regular fee-for-service plans.
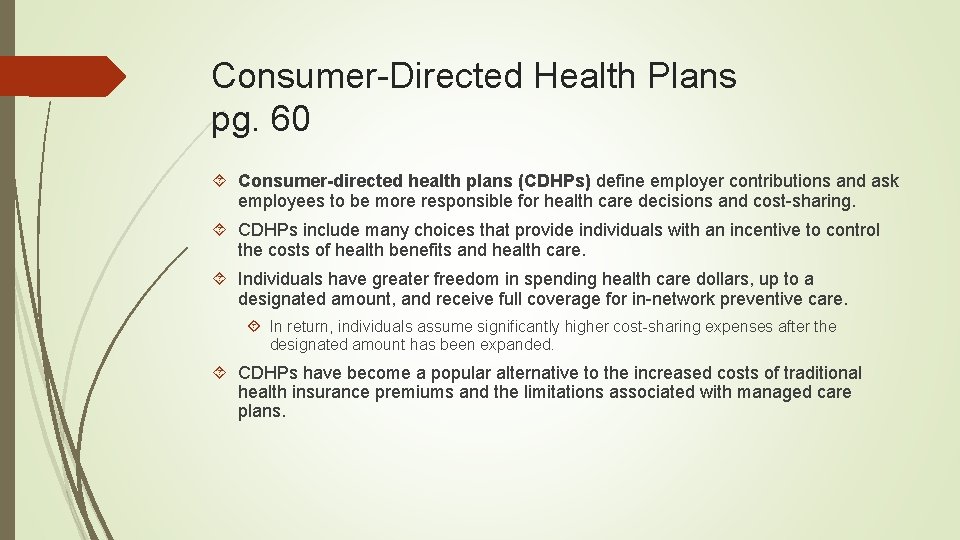
Consumer-Directed Health Plans pg. 60 Consumer-directed health plans (CDHPs) define employer contributions and ask employees to be more responsible for health care decisions and cost-sharing. CDHPs include many choices that provide individuals with an incentive to control the costs of health benefits and health care. Individuals have greater freedom in spending health care dollars, up to a designated amount, and receive full coverage for in-network preventive care. In return, individuals assume significantly higher cost-sharing expenses after the designated amount has been expanded. CDHPs have become a popular alternative to the increased costs of traditional health insurance premiums and the limitations associated with managed care plans.
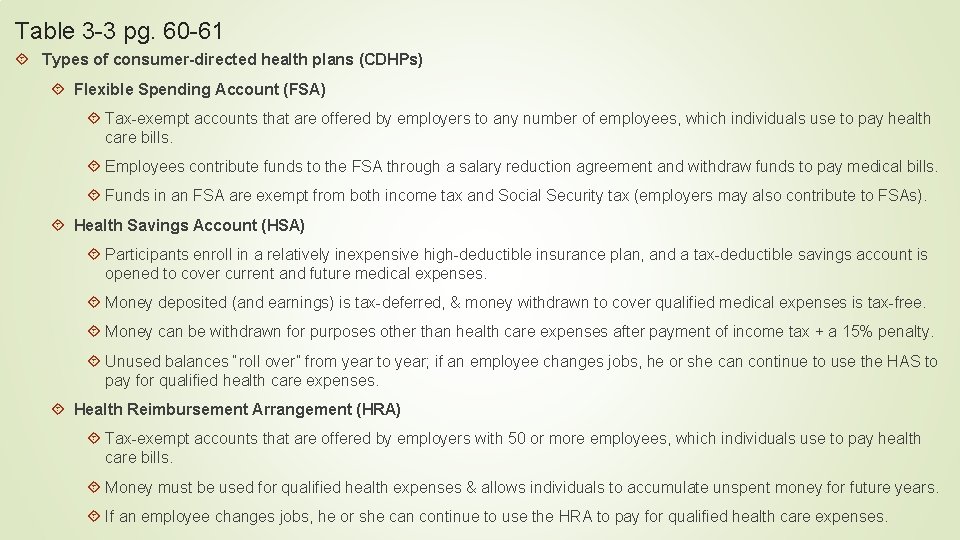
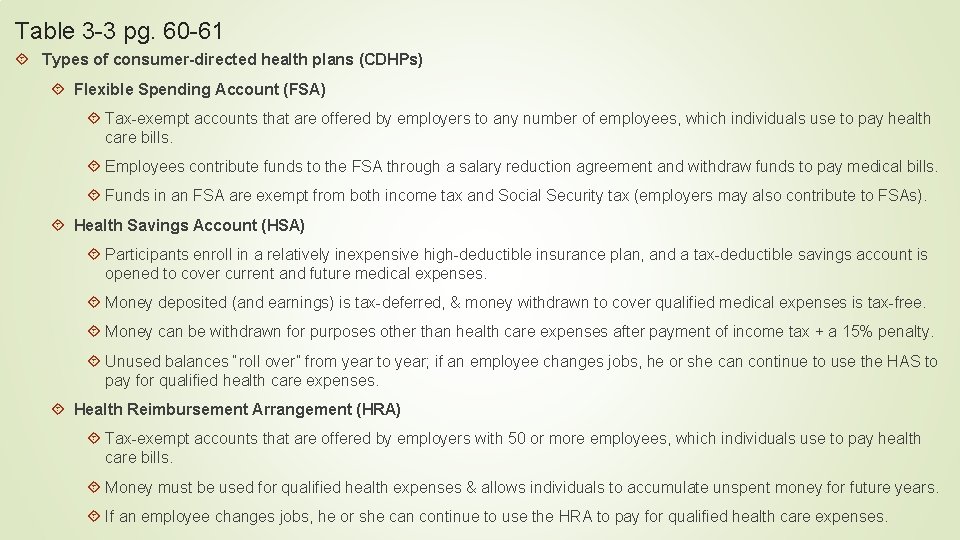
Table 3 -3 pg. 60 -61 Types of consumer-directed health plans (CDHPs) Flexible Spending Account (FSA) Tax-exempt accounts that are offered by employers to any number of employees, which individuals use to pay health care bills. Employees contribute funds to the FSA through a salary reduction agreement and withdraw funds to pay medical bills. Funds in an FSA are exempt from both income tax and Social Security tax (employers may also contribute to FSAs). Health Savings Account (HSA) Participants enroll in a relatively inexpensive high-deductible insurance plan, and a tax-deductible savings account is opened to cover current and future medical expenses. Money deposited (and earnings) is tax-deferred, & money withdrawn to cover qualified medical expenses is tax-free. Money can be withdrawn for purposes other than health care expenses after payment of income tax + a 15% penalty. Unused balances “roll over” from year to year; if an employee changes jobs, he or she can continue to use the HAS to pay for qualified health care expenses. Health Reimbursement Arrangement (HRA) Tax-exempt accounts that are offered by employers with 50 or more employees, which individuals use to pay health care bills. Money must be used for qualified health expenses & allows individuals to accumulate unspent money for future years. If an employee changes jobs, he or she can continue to use the HRA to pay for qualified health care expenses.