Centers for Medicare Medicaid Services Physician Quality Reporting
- Slides: 38
Centers for Medicare & Medicaid Services Physician Quality Reporting Initiative (PQRI) Coding for Quality Sylvia W. Publ, MBA, RHIA Special Program Office, Medicare Value Based Purchasing 1
Overview • PQRI Introduction: Information about PQRI • PQRI Tools: Implementing PQRI • PQRI Principles: Understanding the Measures • PQRI Coding: Examples of Measures • PQRI Readiness: Ensuring Success • PQRI 2008 2
PQRI Introduction: Value-Based Purchasing • Value-based purchasing is a key mechanism for transforming Medicare from a passive payer to an active purchaser. – Current Medicare Physician Fee Schedule is based on quantity and resources consumed, NOT quality or value of services. • Value = Quality / Cost – Incentives can encourage higher quality and avoidance of unnecessary costs to enhance the value of care. 3
PQRI Introduction: The Statute • Tax Relief and Healthcare Act (TRHCA) Section 101 Implementation – – – – – Eligible Professionals Quality Measures Form and Manner of Reporting Determination of Successful Reporting Bonus Payment Validation Appeals Confidential Feedback Reports 2008 Considerations Outreach and Education 4
PQRI Introduction: Focus on Quality • PQRI reporting will focus attention on quality of care. – Foundation is evidence-based measures developed by professionals – Measurement enables improvements in care – Reporting is the first step toward pay for performance 5
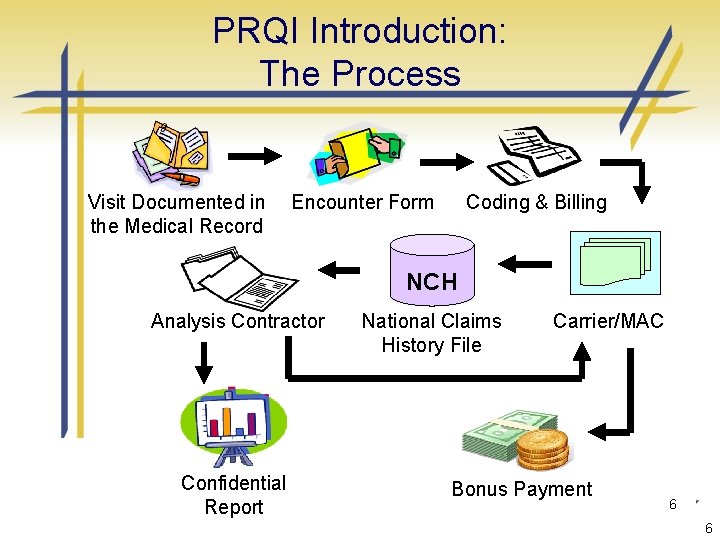
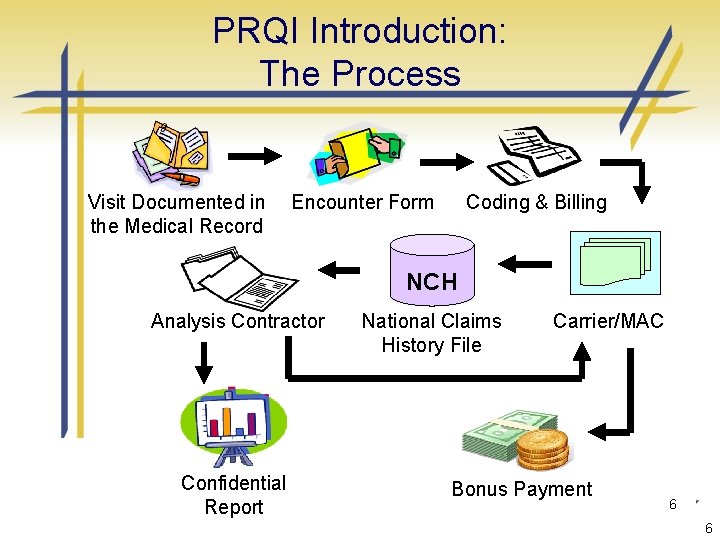
PRQI Introduction: The Process Visit Documented in the Medical Record Encounter Form Coding & Billing NCH Analysis Contractor Confidential Report National Claims History File Carrier/MAC Bonus Payment Procurement Sensitive 6 6
PQRI Introduction: Successful Reporting • Determination of Successful Reporting – Reporting thresholds • If there are no more than 3 measures that apply, each measure must be reported for at least 80% of the cases in which a measure was reportable • If 4 or more measures apply, at least 3 measures must be reported for at least 80% of the cases in which the measure was reportable Procurement Sensitive 7 7
PQRI Introduction: Key Information • Reporting period: Dates of Service between January 1, 2008 through December 31, 2008 • No need to register: just begin reporting • Must be an enrolled Medicare provider (but need not have signed a Medicare participation agreement) • Need to use individual National Provider Identifier (NPI). • Can still participate to practice quality reporting 8
Coding for Quality: PQRI Tools Implementing PQRI 9
PQRI Tools: Where to Begin • Gather information and educational materials from the PQRI web page: www. cms. hhs. gov/pqri on the CMS website. • Gather information from other sources, such as your professional association, specialty society or the American Medical Association. 10
PQRI Tools: The PQRI Website • www. cms. hhs. gov/pqri – – – – Overview CMS Sponsored Calls Statute/Regulations/Program Instructions Eligible Professionals Measures/Codes Reporting Analysis and Payment Educational Resources 11
PQRI Tools: MLN 5640: Coding and Reporting Principles Procurement Sensitive 12 12
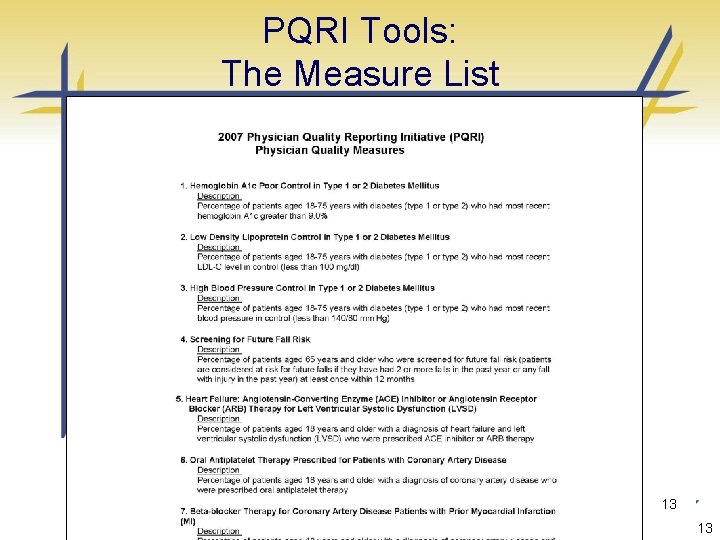
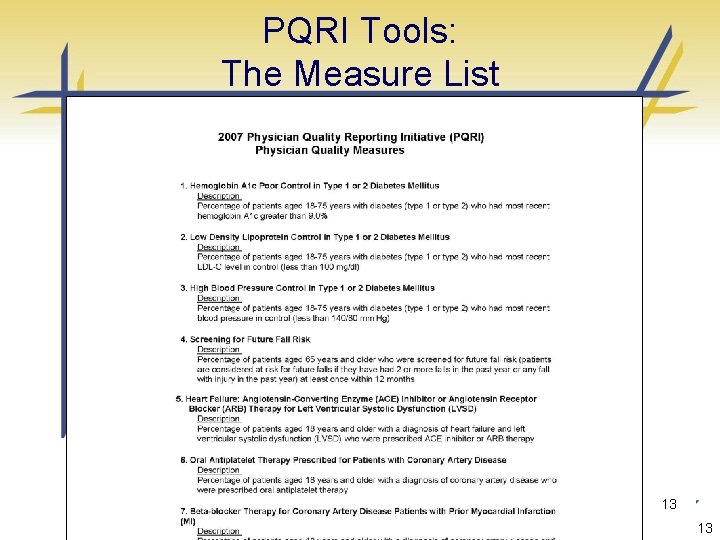
PQRI Tools: The Measure List Procurement Sensitive 13 13
PQRI Tool Kit: The Measure Finder • Allows for search by multiple parameters – – ICD 9 Codes CPT II Codes HCPCS G- Codes • Links to Data Work Sheets Procurement Sensitive 14 14
PQRI Tools: Coding for Quality A Handbook for PQRI Participation Procurement Sensitive 15 15
PQRI Tools: Coding for Quality A Handbook for PQRI Participation • Selecting measures and preparing to report • PQRI coding and reporting principles for the claims based submission of quality data codes • Sample clinical scenarios for each measure, listed by clinical condition/topic, describes successful reporting (and performance where applicable) • PQRI Glossary • 2007 PQRI Code Master • Sample implementation flow chart 16
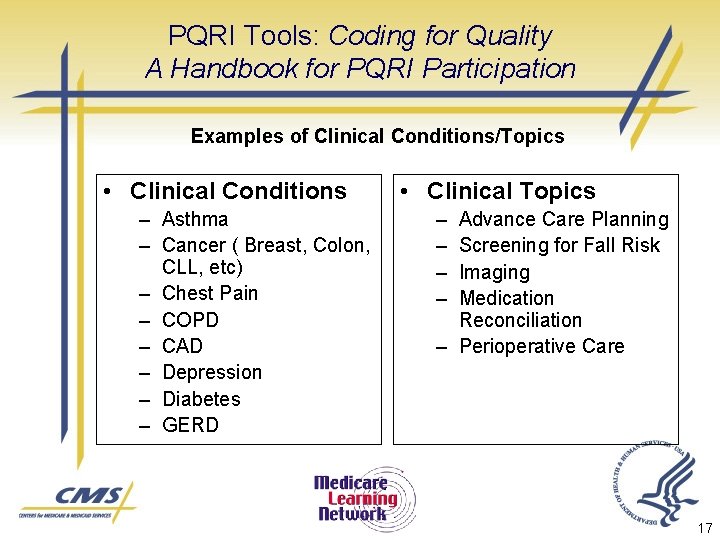
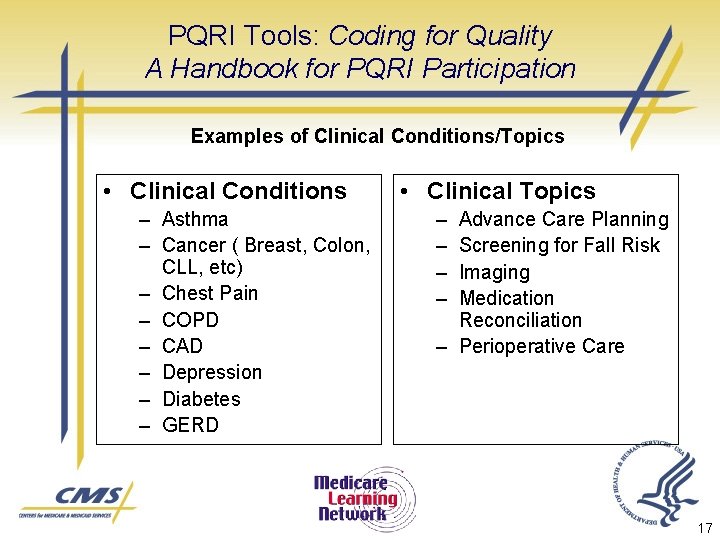
PQRI Tools: Coding for Quality A Handbook for PQRI Participation Examples of Clinical Conditions/Topics • Clinical Conditions – Asthma – Cancer ( Breast, Colon, CLL, etc) – Chest Pain – COPD – CAD – Depression – Diabetes – GERD • Clinical Topics – – Advance Care Planning Screening for Fall Risk Imaging Medication Reconciliation – Perioperative Care 17
PQRI Tools: Measure- specific Data Collection Worksheets • Measure Specific – Measure Description – Worksheet – Coding Specifications 18
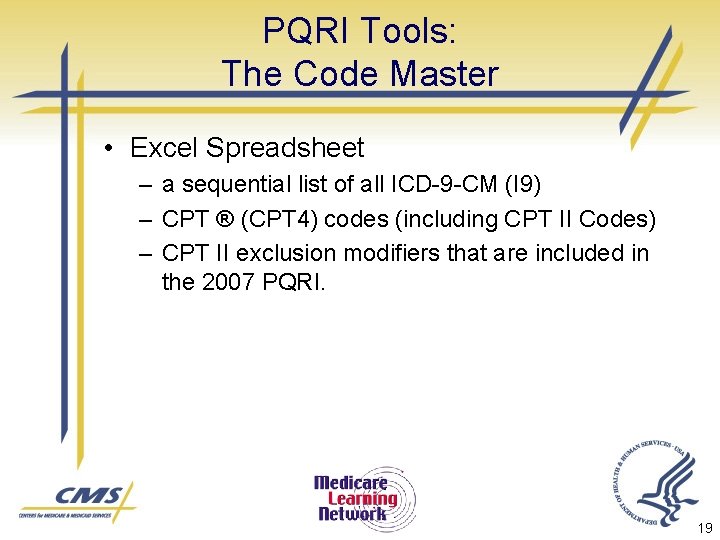
PQRI Tools: The Code Master • Excel Spreadsheet – a sequential list of all ICD-9 -CM (I 9) – CPT ® (CPT 4) codes (including CPT II Codes) – CPT II exclusion modifiers that are included in the 2007 PQRI. 19
Coding for Quality: PQRI Principles Understanding the Measures 20
Understanding the Measures: Commonalities • 119 unique measures associated with clinical conditions that are routinely represented on Medicare Fee-for-Service (FFS) claims – ICD-9 -CM diagnosis codes – HCPCS codes 21
Understanding the Measures: Scope • The measures address various aspects of quality care – Prevention – Chronic Care Management – Acute Episode of Care Management – Procedural Related Care – Resource Utilization – Care Coordination 22
Understanding the Measures: Construct Clinical action required for reporting and performance ________________ Eligible cases for a measure (the eligible patient population associated with the numerator) 23
Understanding the Measures: Construct CPT II Code or Temporary G Code ________________ ICD-9 -CM and CPT Category I Codes 24
Understanding the Measures: Quality Data Codes Quality-Data Codes translate clinical actions so they can be captured in the administrative claims process 25
Understanding the Measures: Quality Data Codes • Quality-Data Codes can relay that: – The measure requirement was met or – The measure requirement was not met due to documented allowable performance exclusions (i. e. , using performance exclusion modifiers) or – The measure requirement was not met and the reason is not documented in the medical record (i. e. , using the 8 P reporting modifier) 26
Understanding the Measures: The Performance Modifiers • Performance Measure Exclusion Modifiers indicate that an action specified in the measure was not provided due to medical, patient or systems reason(s) documented in the medical record: – 1 P- Performance Measure Exclusion Modifier due to Medical Reasons – 2 P- Performance Measure Exclusion Modifier used due to Patient Reason – 3 P- Performance Measure Exclusion Modifier used due to System Reason • One or more exclusions may be applicable for a given measure. Certain measures have no applicable exclusion modifiers. Refer to the measure specifications to determine the appropriate exclusion modifiers. 27
Understanding the Measures: The Reporting Modifier • Performance Measure Reporting Modifier facilitates reporting a case when the patient is eligible but the action described in a measure is not performed and the reason is not specified or documented – 8 P- Performance Measure Reporting Modifier- action not performed, reason not otherwise specified 28
Understanding the Measures: Performance Time Frame • Some measures have a Performance Timeframe related to the clinical action that may be distinct form the reporting frequency. – Perform within 12 months – Most Recent • Clinical test result needs to be obtained, reviewed, reported one time. It need not have been performed during the reporting period. 29
Understanding the Measures: Reporting Frequency • Each measure has a Reporting Frequency requirement for each eligible patient seen during the reporting period – Report one-time only – Report once for each procedure performed – Report for each acute episode 30
Coding for Quality: PQRI Coding Examples Of Measures 31
Coding for Quality: Pathology Measures • Breast Cancer patients who have a p. T and p. N category and histologic grade for their cancer • Colorectal cancer patients who have a p. T and p. N category and histologic grade for their cancer. 32
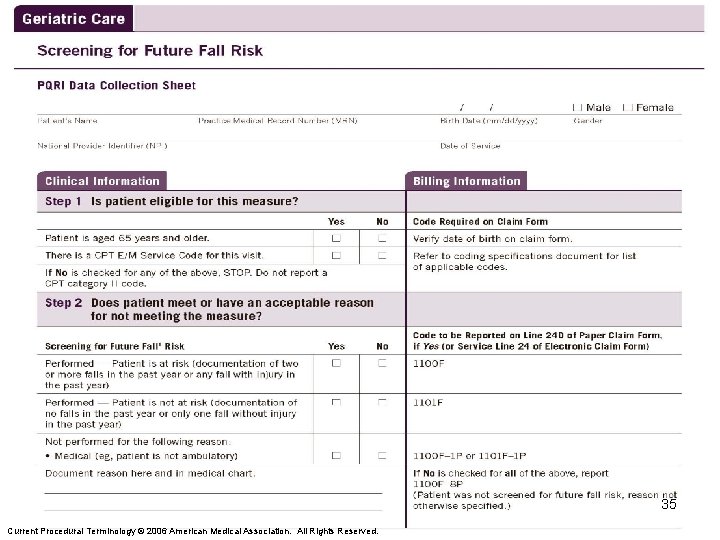
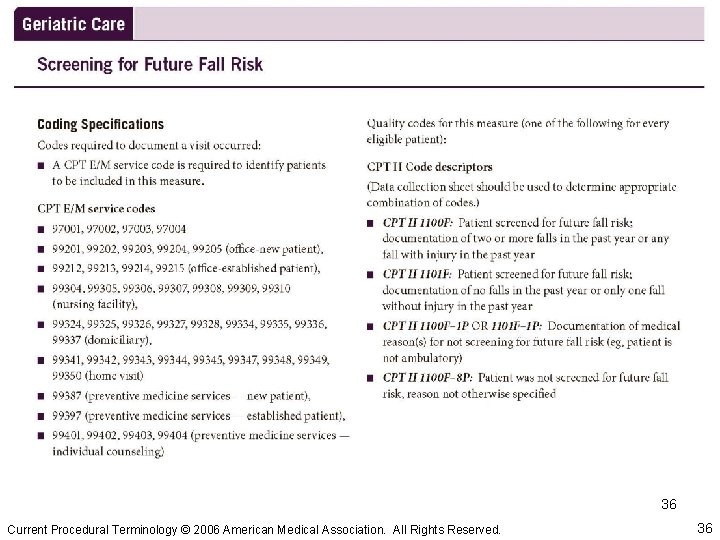
Coding for Quality: Example #1 - Prevention Measure #4 – Screening for Future Fall Risk 33
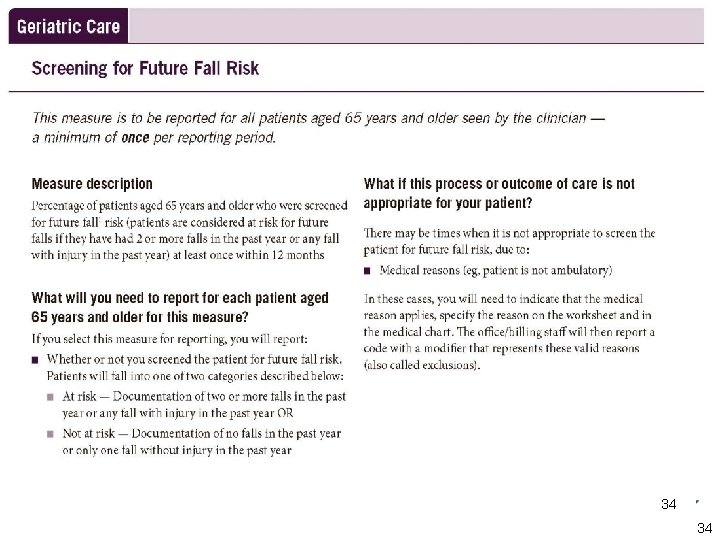
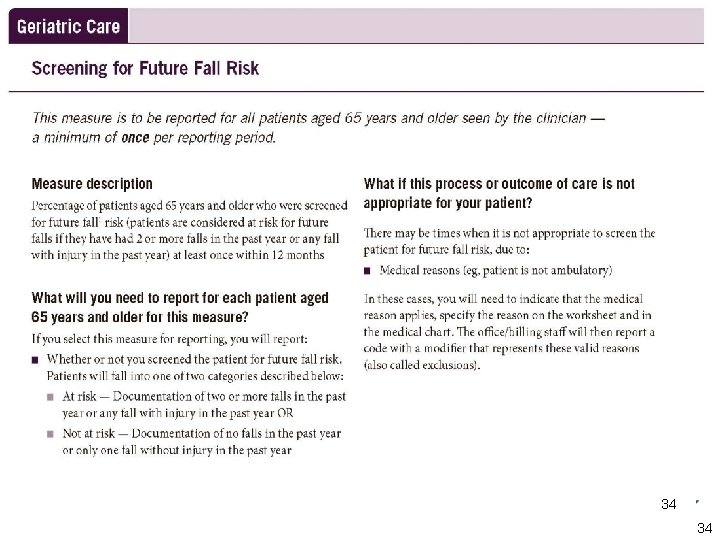
Procurement Sensitive 34 34
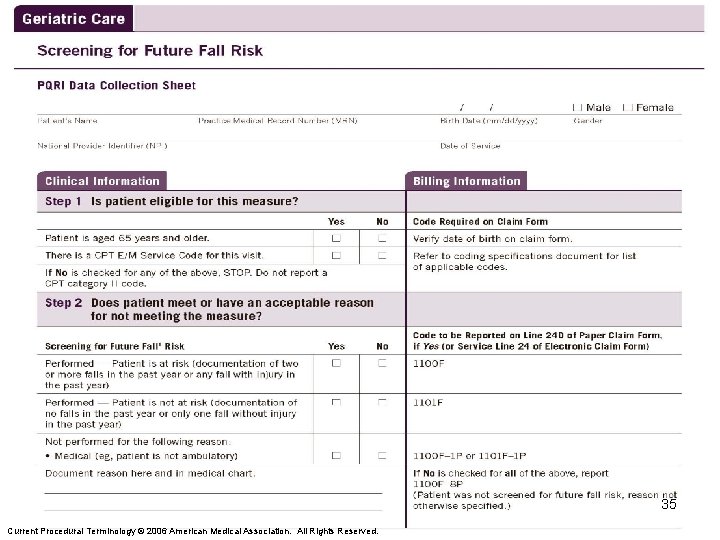
Procurement Sensitive Current Procedural Terminology © 2006 American Medical Association. All Rights Reserved. 35 35
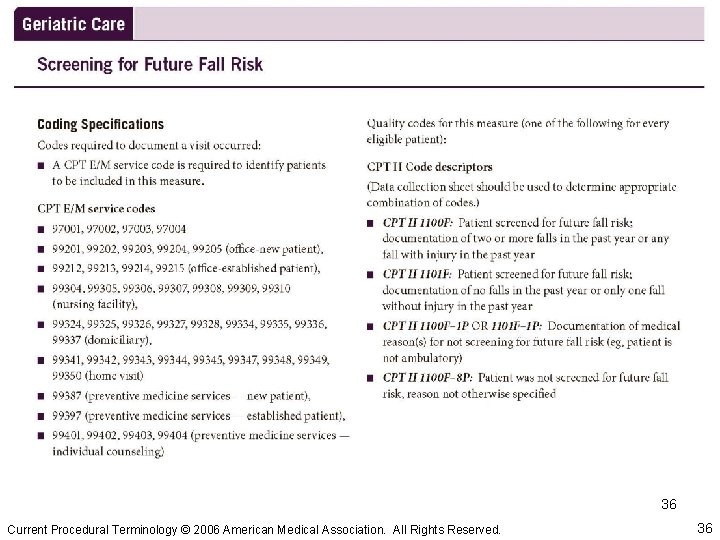
Procurement Sensitive Current Procedural Terminology © 2006 American Medical Association. All Rights Reserved. 36 36
PQRI Reporting: Ensuring Success • Educational Resources – CMS PQRI website contains all publicly available information at: www. cms. hhs. gov/PQRI • Frequently Asked Questions • PQRI Fact Sheet • Medicare Carrier/Medicare Administrative Contractor (MAC) inquiry management 37
Questions? 38
 Medicare vs medicaid washington state
Medicare vs medicaid washington state Medicare medicaid
Medicare medicaid Medicare set aside flow chart
Medicare set aside flow chart Medicare preventive services quick reference
Medicare preventive services quick reference Midas healthcare solutions inc
Midas healthcare solutions inc Sql server report builder
Sql server report builder Fidelity personal trust services
Fidelity personal trust services Sql server reporting services architecture
Sql server reporting services architecture Reporting services 2000
Reporting services 2000 A physician claims that joggers maximum volume
A physician claims that joggers maximum volume Physician reentry program
Physician reentry program Physician consortium for performance improvement
Physician consortium for performance improvement Physician time studies
Physician time studies Physician segmentation and targeting
Physician segmentation and targeting Physician competency reference set
Physician competency reference set Coalition for physician enhancement
Coalition for physician enhancement Physician associate lecturer
Physician associate lecturer Physician sign out
Physician sign out Elisha goodman prayers for financial breakthrough
Elisha goodman prayers for financial breakthrough Maryland physician health program
Maryland physician health program Physician burnout retreat
Physician burnout retreat Physician employment models
Physician employment models Dr. sachin khullar
Dr. sachin khullar Werkplekleren epa
Werkplekleren epa Family medicine fellowship
Family medicine fellowship University of new england physician assistant program
University of new england physician assistant program Physician personas
Physician personas Uscis physician locator
Uscis physician locator Interpretive model of doctor-patient relationship
Interpretive model of doctor-patient relationship Cpoe advantages and disadvantages
Cpoe advantages and disadvantages Oklahoma board of nursing supervising physician
Oklahoma board of nursing supervising physician A physician claims that joggers maximum volume
A physician claims that joggers maximum volume Provider engagement
Provider engagement The good physician treats the disease
The good physician treats the disease Wellstar physicians group
Wellstar physicians group Stanford physician wellness survey
Stanford physician wellness survey Pricewaterhouse
Pricewaterhouse Pa ieb physician certification form
Pa ieb physician certification form Cphp colorado
Cphp colorado