Cemented versus cementless femoral stem fixation in primary
- Slides: 9
Cemented versus cementless femoral stem fixation in primary total hip arthroplasty and risk of all-cause revision in a US cohort 9 th Annual International Congress of Arthroplasty Registries (1 st Annual Virtual Congress) November 13 -15, 2020 Matthew P. Kelly, MD Heather A. Prentice, Ph. D, MPH Elizabeth W. Paxton, Ph. D, MA Adrian D. Hinman, MD Monti Khatod, MD NATIONAL IMPLANT REGISTRIES
§ My coauthors and I have no potential conflicts of interest to report 2 NATIONAL IMPLANT REGISTRIES
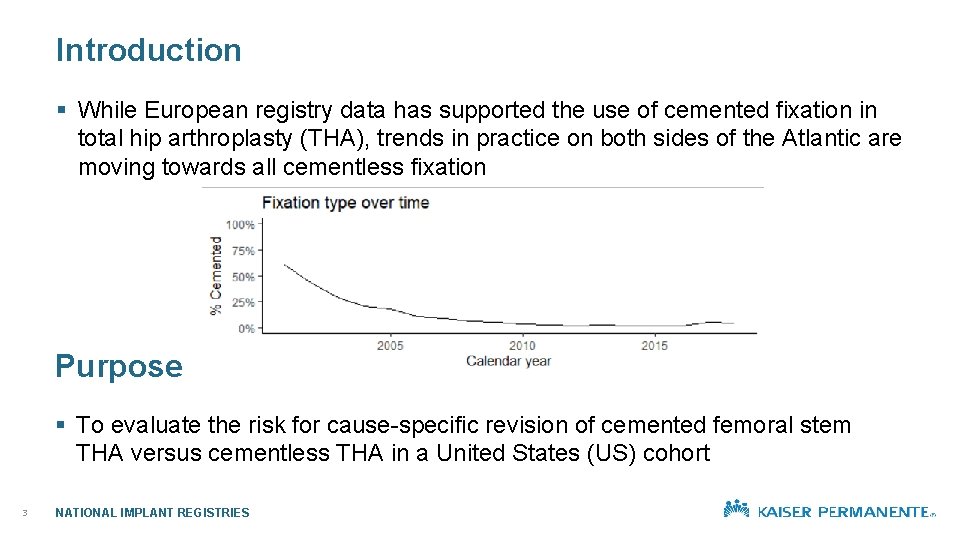
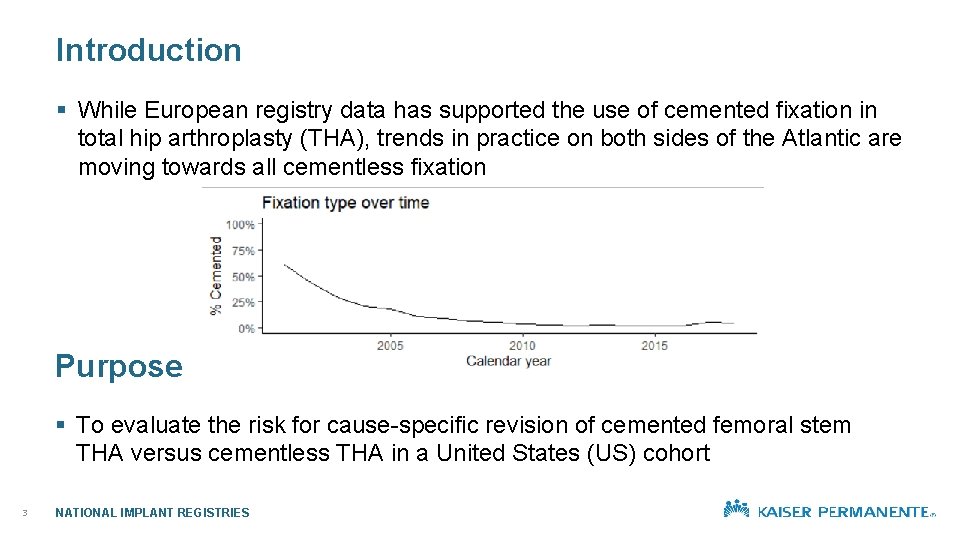
Introduction § While European registry data has supported the use of cemented fixation in total hip arthroplasty (THA), trends in practice on both sides of the Atlantic are moving towards all cementless fixation Purpose § To evaluate the risk for cause-specific revision of cemented femoral stem THA versus cementless THA in a United States (US) cohort 3 NATIONAL IMPLANT REGISTRIES
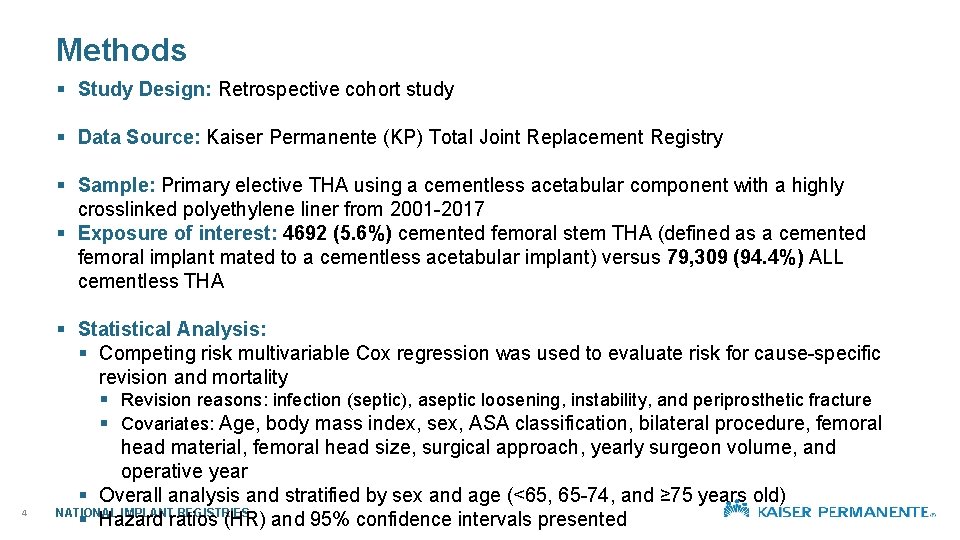
Methods § Study Design: Retrospective cohort study § Data Source: Kaiser Permanente (KP) Total Joint Replacement Registry § Sample: Primary elective THA using a cementless acetabular component with a highly crosslinked polyethylene liner from 2001 -2017 § Exposure of interest: 4692 (5. 6%) cemented femoral stem THA (defined as a cemented femoral implant mated to a cementless acetabular implant) versus 79, 309 (94. 4%) ALL cementless THA § Statistical Analysis: § Competing risk multivariable Cox regression was used to evaluate risk for cause-specific revision and mortality § Revision reasons: infection (septic), aseptic loosening, instability, and periprosthetic fracture § Covariates: Age, body mass index, sex, ASA classification, bilateral procedure, femoral 4 head material, femoral head size, surgical approach, yearly surgeon volume, and operative year § Overall analysis and stratified by sex and age (<65, 65 -74, and ≥ 75 years old) NATIONAL IMPLANT REGISTRIES § Hazard ratios (HR) and 95% confidence intervals presented
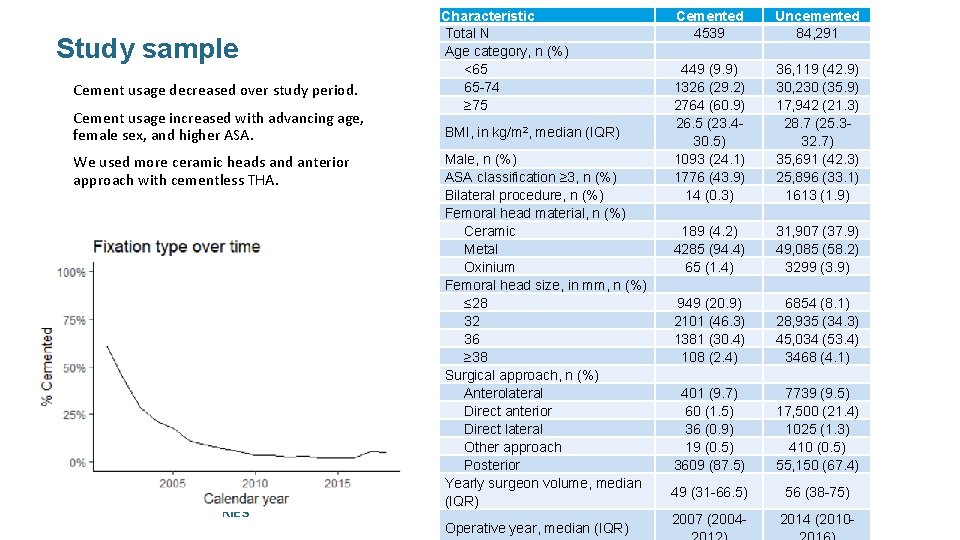
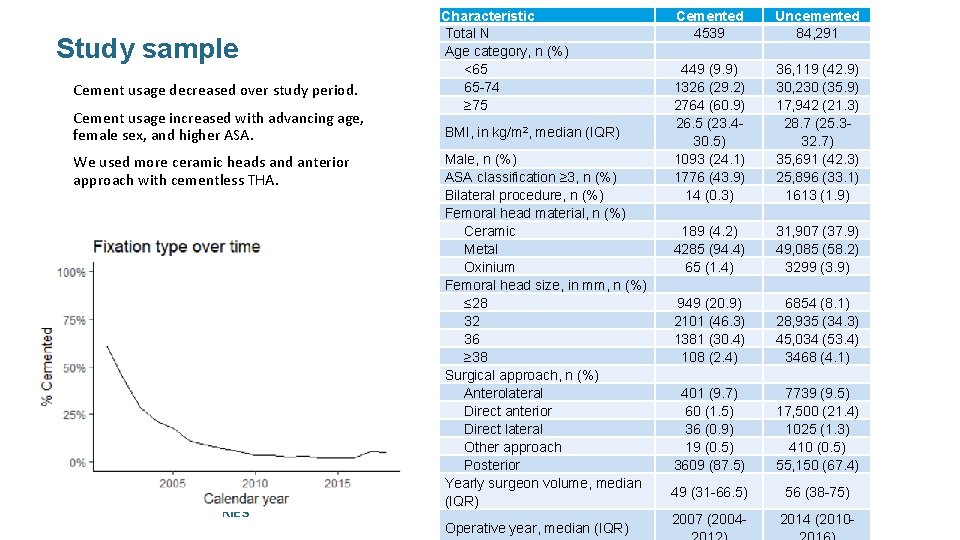
Study sample Cement usage decreased over study period. Cement usage increased with advancing age, female sex, and higher ASA. We used more ceramic heads and anterior approach with cementless THA. NATIONAL IMPLANT REGISTRIES Characteristic Total N Age category, n (%) <65 65 -74 ≥ 75 BMI, in kg/m 2, median (IQR) Male, n (%) ASA classification ≥ 3, n (%) Bilateral procedure, n (%) Femoral head material, n (%) Ceramic Metal Oxinium Femoral head size, in mm, n (%) ≤ 28 32 36 ≥ 38 Surgical approach, n (%) Anterolateral Direct anterior Direct lateral Other approach Posterior Yearly surgeon volume, median (IQR) Operative year, median (IQR) Cemented 4539 Uncemented 84, 291 449 (9. 9) 1326 (29. 2) 2764 (60. 9) 26. 5 (23. 430. 5) 1093 (24. 1) 1776 (43. 9) 14 (0. 3) 36, 119 (42. 9) 30, 230 (35. 9) 17, 942 (21. 3) 28. 7 (25. 332. 7) 35, 691 (42. 3) 25, 896 (33. 1) 1613 (1. 9) 189 (4. 2) 4285 (94. 4) 65 (1. 4) 31, 907 (37. 9) 49, 085 (58. 2) 3299 (3. 9) 949 (20. 9) 2101 (46. 3) 1381 (30. 4) 108 (2. 4) 6854 (8. 1) 28, 935 (34. 3) 45, 034 (53. 4) 3468 (4. 1) 401 (9. 7) 60 (1. 5) 36 (0. 9) 19 (0. 5) 3609 (87. 5) 7739 (9. 5) 17, 500 (21. 4) 1025 (1. 3) 410 (0. 5) 55, 150 (67. 4) 49 (31 -66. 5) 56 (38 -75) 2007 (2004 - 2014 (2010 - 5
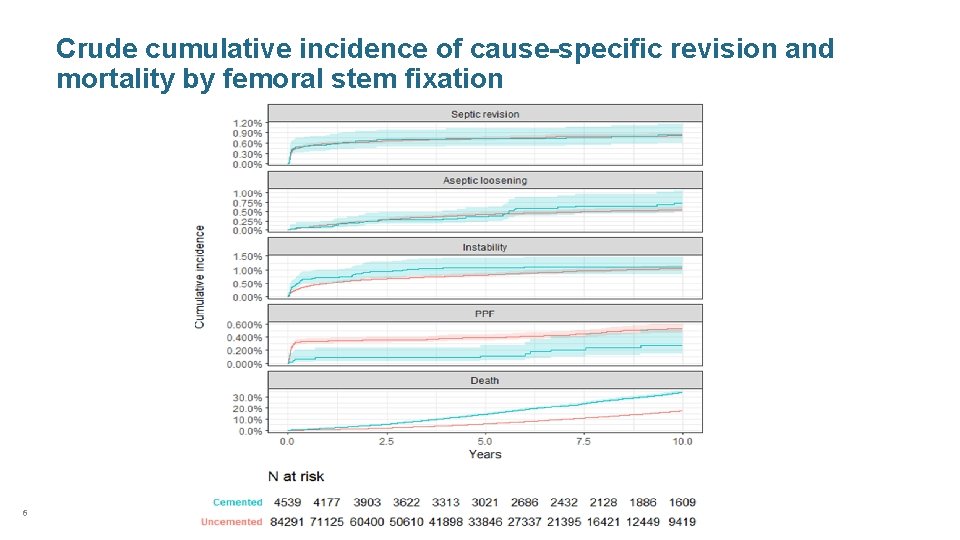
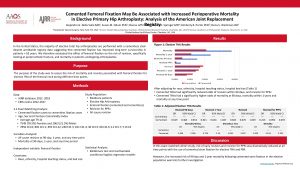
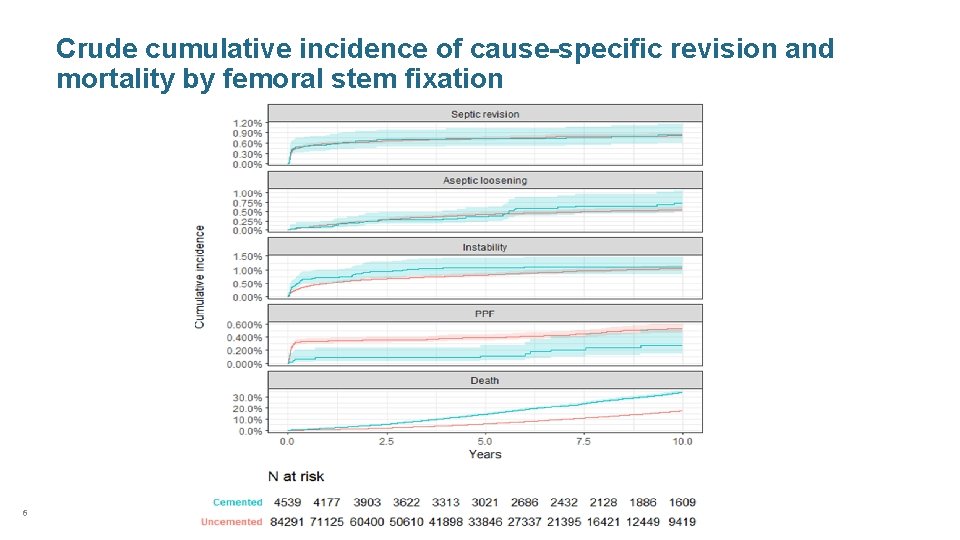
Crude cumulative incidence of cause-specific revision and mortality by femoral stem fixation 6 NATIONAL IMPLANT REGISTRIES
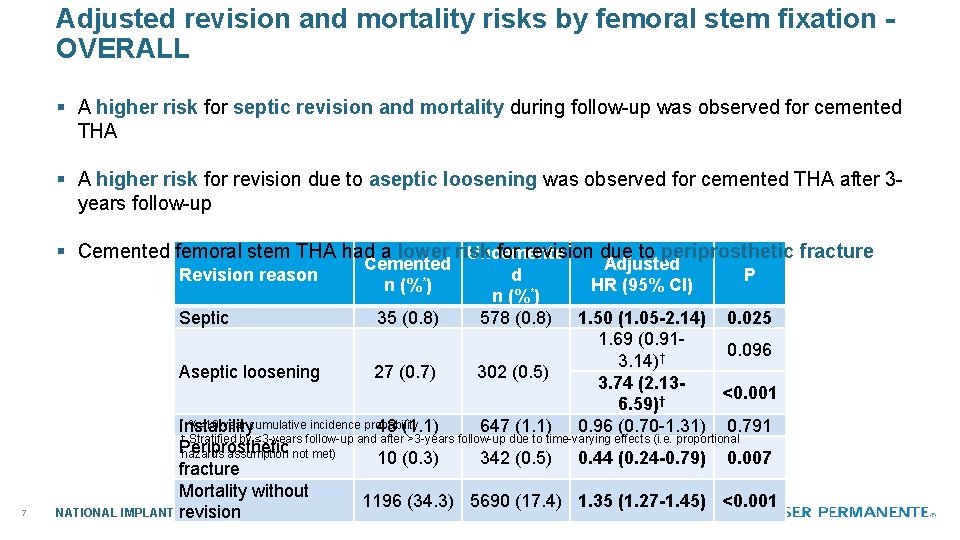
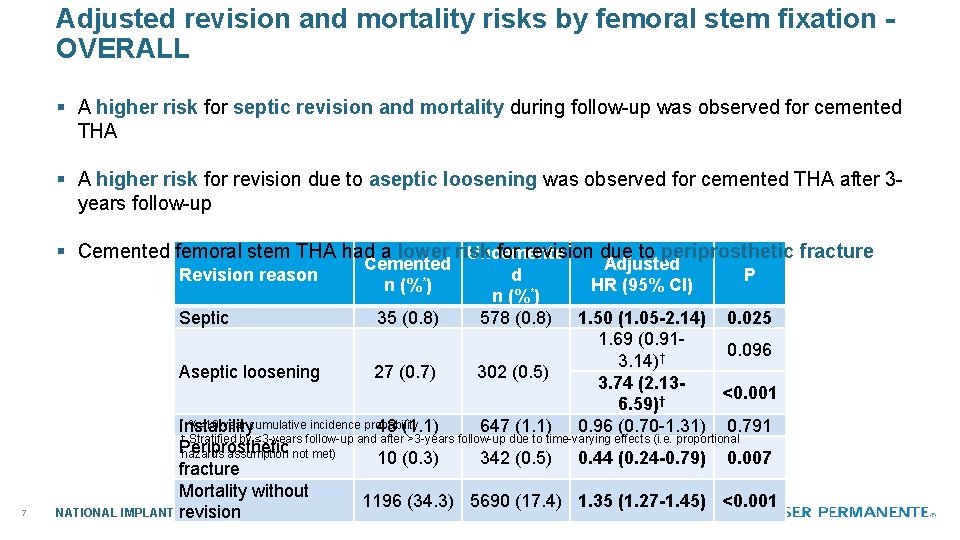
Adjusted revision and mortality risks by femoral stem fixation OVERALL § A higher risk for septic revision and mortality during follow-up was observed for cemented THA § A higher risk for revision due to aseptic loosening was observed for cemented THA after 3 years follow-up § Cemented femoral stem THA had a lower risk for revision due to periprosthetic fracture Uncemente Revision reason 7 Cemented n (%*) Septic 35 (0. 8) d n (%*) 578 (0. 8) Aseptic loosening 27 (0. 7) 302 (0. 5) Adjusted HR (95% CI) P 1. 50 (1. 05 -2. 14) 0. 025 1. 69 (0. 910. 096 3. 14)† 3. 74 (2. 13<0. 001 6. 59)† 0. 96 (0. 70 -1. 31) 0. 791 * %=10 -year cumulative incidence probability Instability 48 (1. 1) 647 (1. 1) † Stratified by ≤ 3 -years follow-up and after >3 -years follow-up due to time-varying effects (i. e. proportional Periprosthetic hazards assumption not met) 10 (0. 3) 342 (0. 5) 0. 44 (0. 24 -0. 79) 0. 007 fracture Mortality without 1196 (34. 3) 5690 (17. 4) 1. 35 (1. 27 -1. 45) <0. 001 NATIONAL IMPLANT REGISTRIES revision
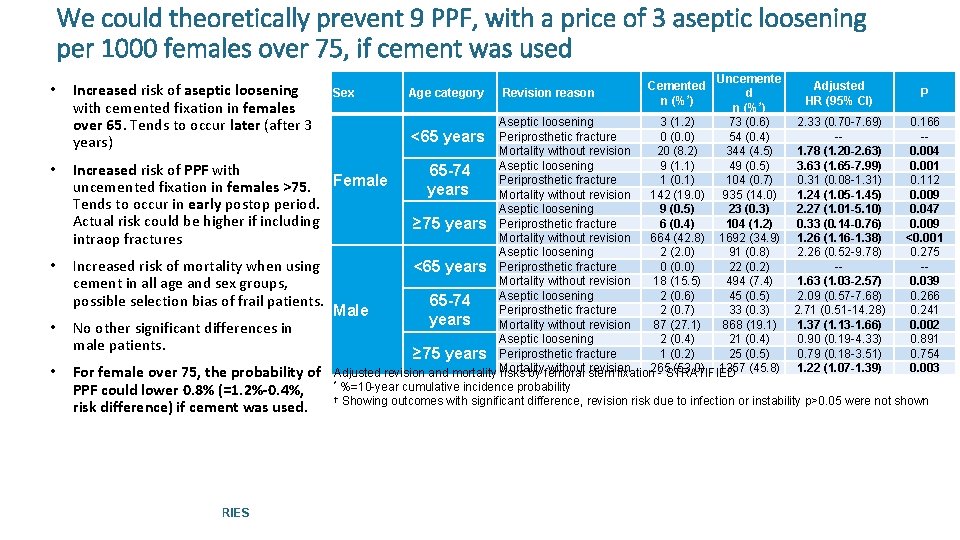
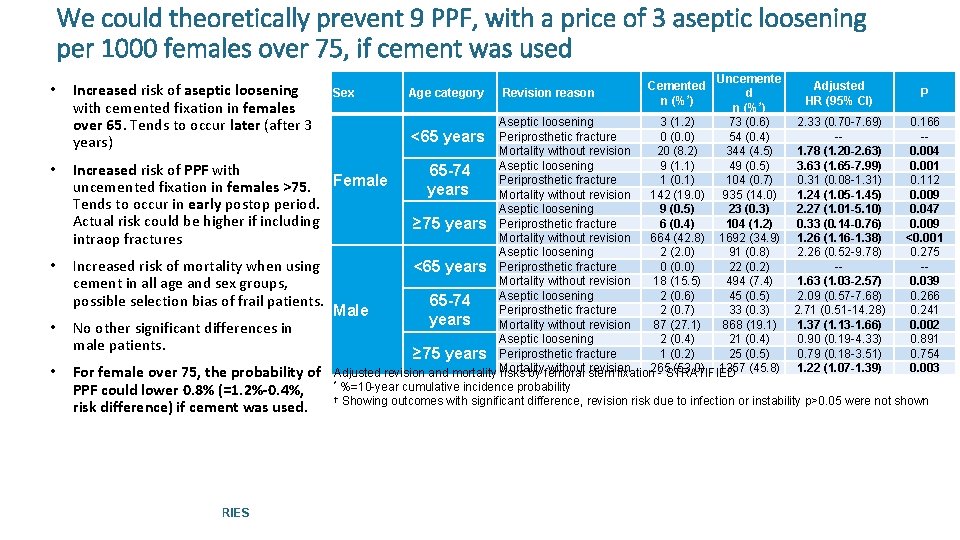
We could theoretically prevent 9 PPF, with a price of 3 aseptic loosening per 1000 females over 75, if cement was used • Increased risk of aseptic loosening with cemented fixation in females over 65. Tends to occur later (after 3 years) • Increased risk of PPF with uncemented fixation in females >75. Tends to occur in early postop period. Actual risk could be higher if including intraop fractures • Increased risk of mortality when using cement in all age and sex groups, possible selection bias of frail patients. • No other significant differences in male patients. • For female over 75, the probability of PPF could lower 0. 8% (=1. 2%-0. 4%, risk difference) if cement was used. NATIONAL IMPLANT REGISTRIES Uncemente Adjusted Sex Age category Revision reason d HR (95% CI) n (%*) Aseptic loosening 3 (1. 2) 73 (0. 6) 2. 33 (0. 70 -7. 69) 0 (0. 0) 54 (0. 4) -<65 years Periprosthetic fracture Mortality without revision 20 (8. 2) 344 (4. 5) 1. 78 (1. 20 -2. 63) Aseptic loosening 9 (1. 1) 49 (0. 5) 3. 63 (1. 65 -7. 99) 65 -74 Periprosthetic fracture 1 (0. 1) 104 (0. 7) 0. 31 (0. 08 -1. 31) Female years Mortality without revision 142 (19. 0) 935 (14. 0) 1. 24 (1. 05 -1. 45) Aseptic loosening 9 (0. 5) 23 (0. 3) 2. 27 (1. 01 -5. 10) Periprosthetic fracture 6 (0. 4) 104 (1. 2) 0. 33 (0. 14 -0. 76) ≥ 75 years Mortality without revision 664 (42. 8) 1692 (34. 9) 1. 26 (1. 16 -1. 38) Aseptic loosening 2 (2. 0) 91 (0. 8) 2. 26 (0. 52 -9. 78) Periprosthetic fracture 0 (0. 0) 22 (0. 2) -<65 years Mortality without revision 18 (15. 5) 494 (7. 4) 1. 63 (1. 03 -2. 57) Aseptic loosening 2 (0. 6) 45 (0. 5) 2. 09 (0. 57 -7. 68) 65 -74 Periprosthetic fracture 2 (0. 7) 33 (0. 3) 2. 71 (0. 51 -14. 28) Male years Mortality without revision 87 (27. 1) 868 (19. 1) 1. 37 (1. 13 -1. 66) Aseptic loosening 2 (0. 4) 21 (0. 4) 0. 90 (0. 19 -4. 33) 1 (0. 2) 25 (0. 5) 0. 79 (0. 18 -3. 51) ≥ 75 years Periprosthetic fracture without stem revision (53. 0) 1357 (45. 8) 1. 22 (1. 07 -1. 39) Adjusted revision and mortality Mortality risks by femoral fixation 265 - STRATIFIED Cemented n (%*) * † P 0. 166 -0. 004 0. 001 0. 112 0. 009 0. 047 0. 009 <0. 001 0. 275 -0. 039 0. 266 0. 241 0. 002 0. 891 0. 754 0. 003 %=10 -year cumulative incidence probability Showing outcomes with significant difference, revision risk due to infection or instability p>0. 05 were not shown 8
Conclusion § Clinical practice in our integrated healthcare system reveals a strong propensity for all cementless implants § In a US THA cohort spanning over 15 years, we observed differences in cause-specific revision risk depending on femoral stem fixation § While the trend towards all cementless fixation continues, there may be a role for cemented femoral fixation in females over age 75 to mitigate risk for revision due to PPF which can cause greater morbidity than revision for aseptic loosening 9 NATIONAL IMPLANT REGISTRIES