Assessment and Management of Cellulitis Dr Astrid Arellano
- Slides: 17
Assessment and Management of Cellulitis Dr Astrid Arellano MBBS FRACP Infectious Diseases Physician
Adult Infectious Diseases Physician • • • University of Adelaide Graduate, Advanced training in Perth, WA both in microbiology and infectious diseases Private Practice based in Subiaco Inpatient care at SJOG Subiaco Hospital Public Health Physician at WA TB Control Program Lecturer and Clinical Tutor at Notre Dame University 1/1 Sheen Street Subiaco WA 6008 PH: 6478 9963 FAX: 9389 6531 M: 0421514653
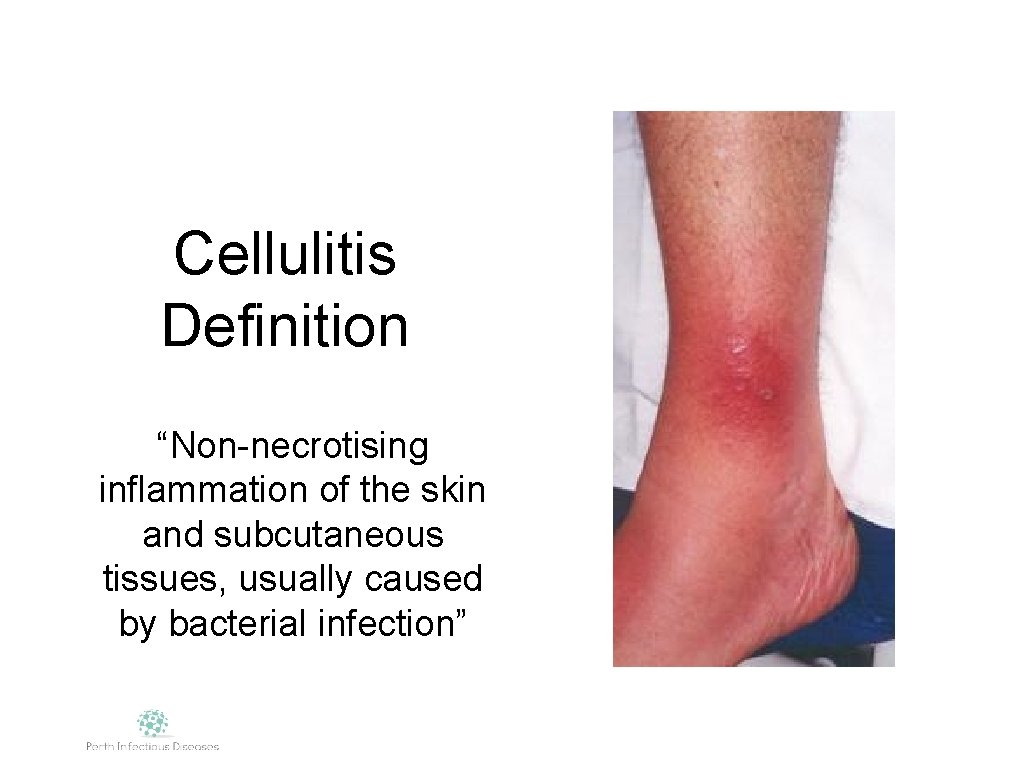
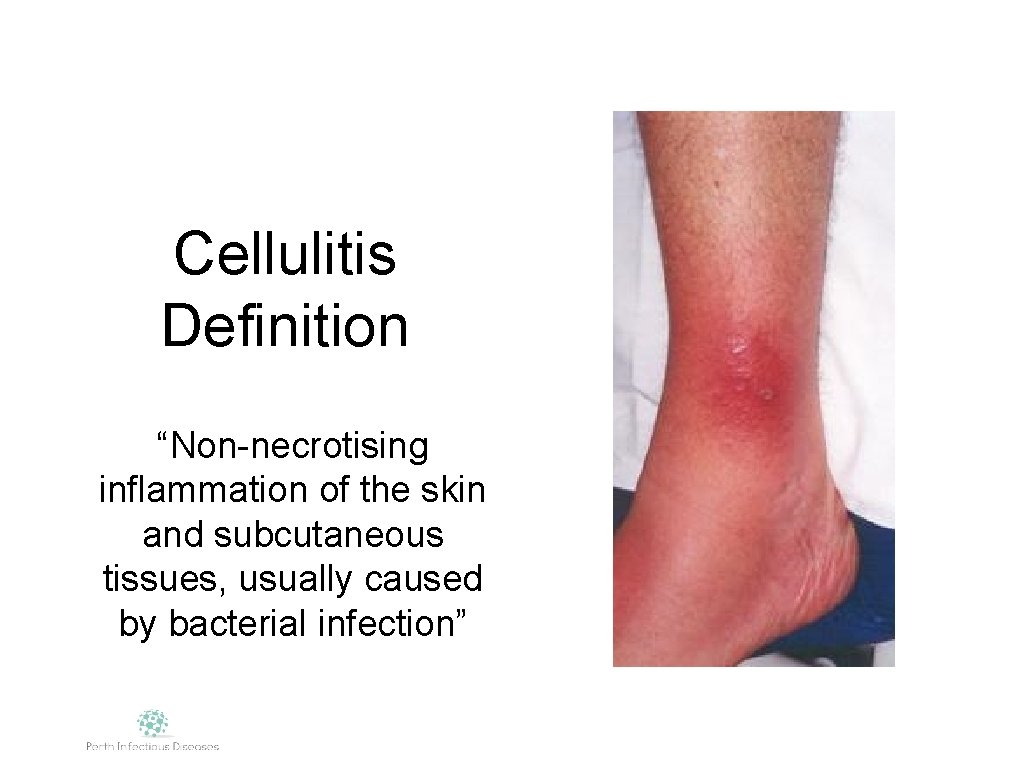
Cellulitis Definition “Non-necrotising inflammation of the skin and subcutaneous tissues, usually caused by bacterial infection”
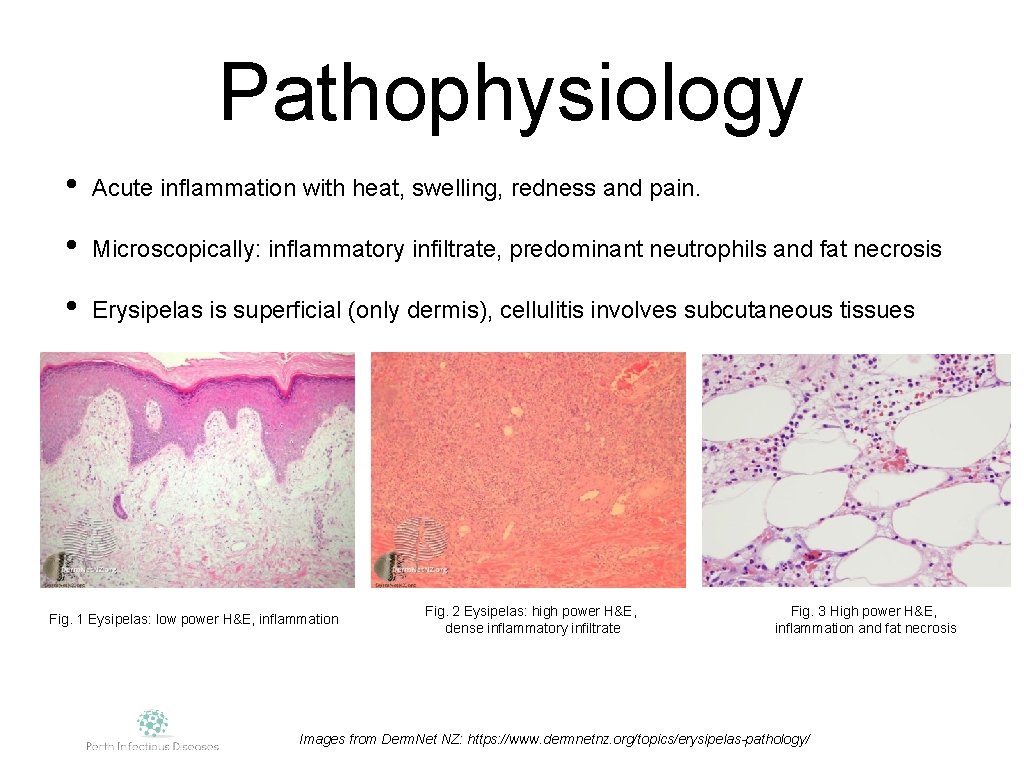
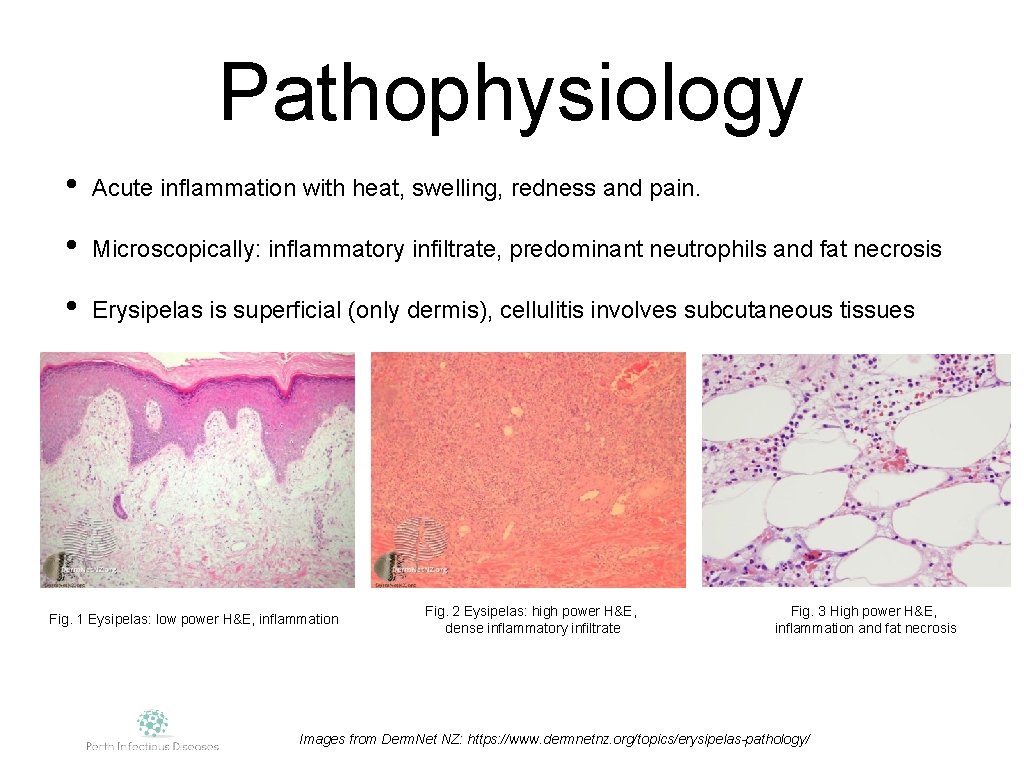
Pathophysiology • Acute inflammation with heat, swelling, redness and pain. • Microscopically: inflammatory infiltrate, predominant neutrophils and fat necrosis • Erysipelas is superficial (only dermis), cellulitis involves subcutaneous tissues Fig. 1 Eysipelas: low power H&E, inflammation Fig. 2 Eysipelas: high power H&E, dense inflammatory infiltrate Fig. 3 High power H&E, inflammation and fat necrosis Images from Derm. Net NZ: https: //www. dermnetnz. org/topics/erysipelas-pathology/
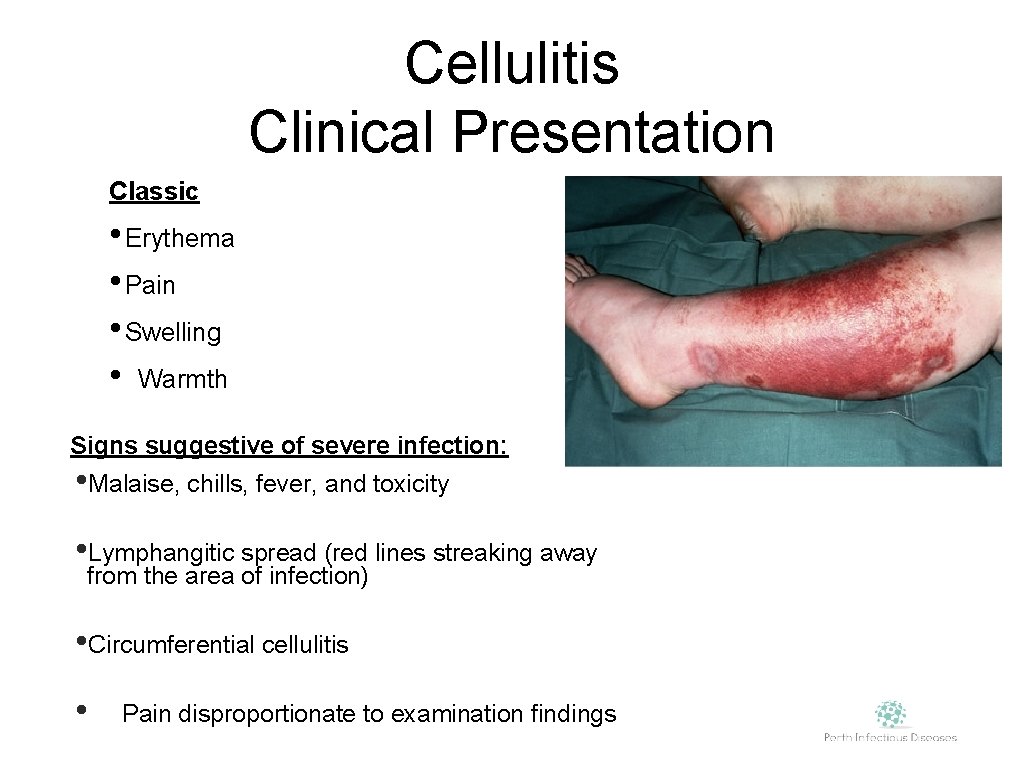
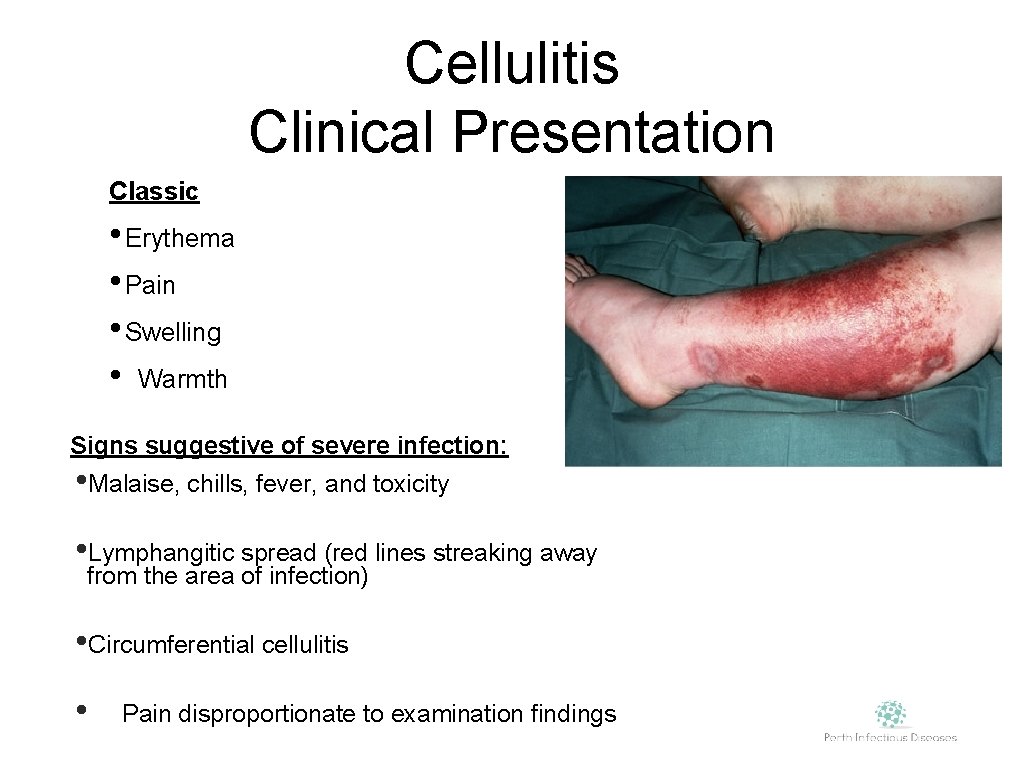
Cellulitis Clinical Presentation Classic • Erythema • Pain • Swelling • Warmth Signs suggestive of severe infection: • Malaise, chills, fever, and toxicity • Lymphangitic spread (red lines streaking away from the area of infection) • Circumferential cellulitis • Pain disproportionate to examination findings
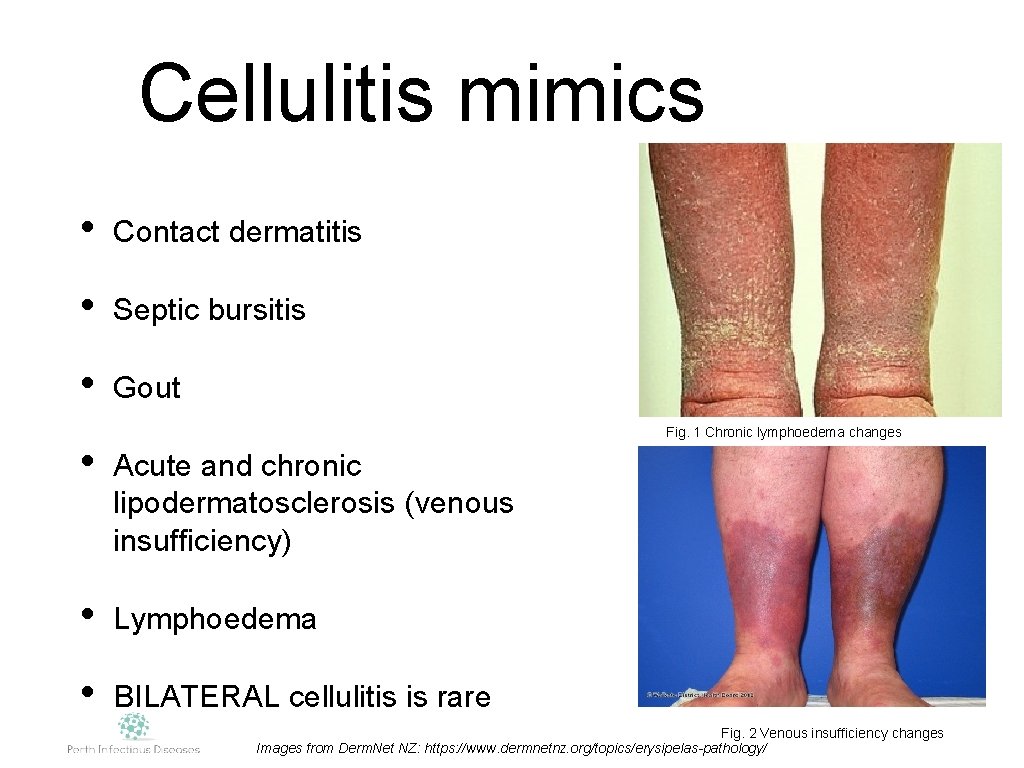
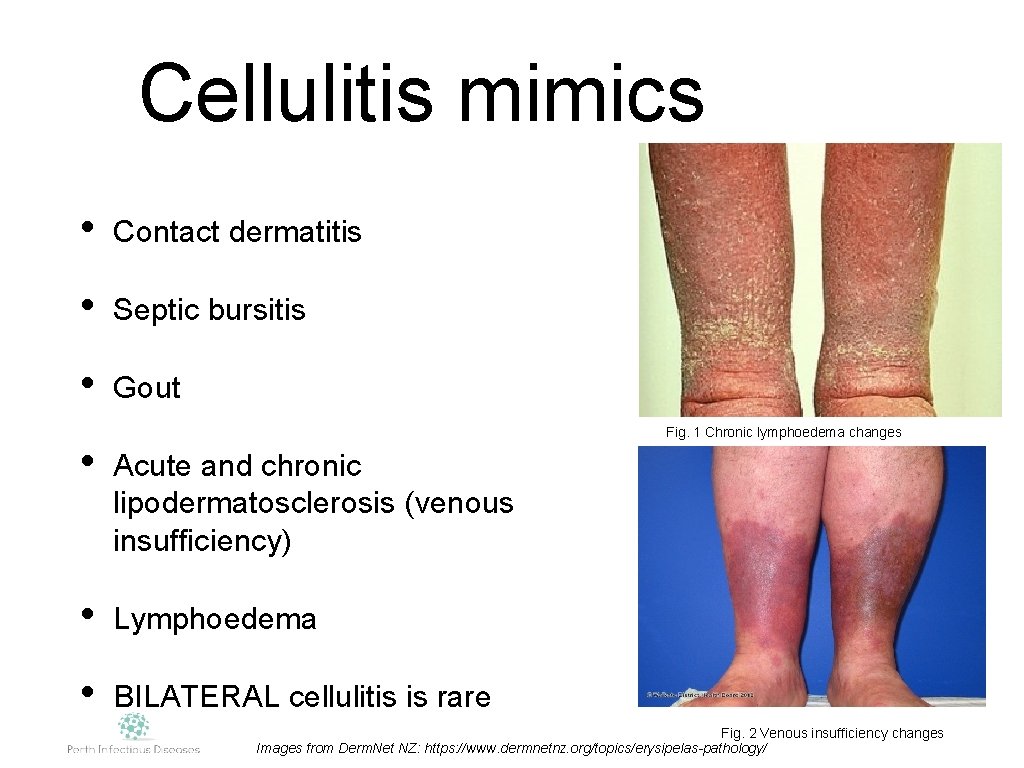
Cellulitis mimics • Contact dermatitis • Septic bursitis • Gout Fig. 1 Chronic lymphoedema changes • Acute and chronic lipodermatosclerosis (venous insufficiency) • Lymphoedema • BILATERAL cellulitis is rare Fig. 2 Venous insufficiency changes Images from Derm. Net NZ: https: //www. dermnetnz. org/topics/erysipelas-pathology/
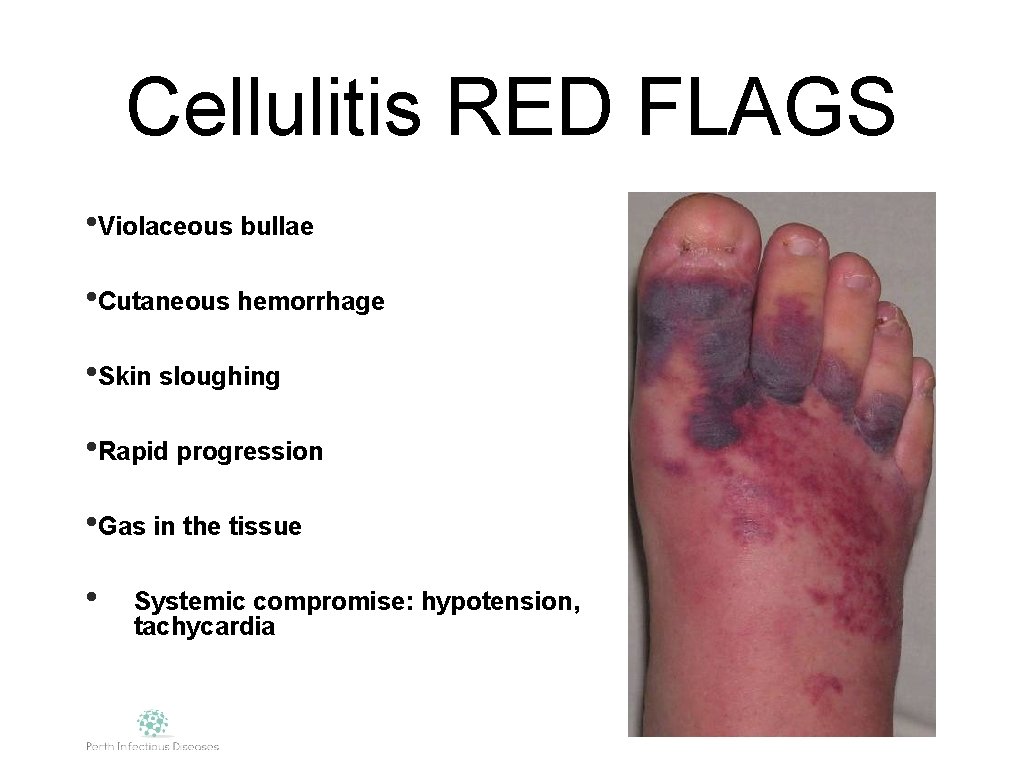
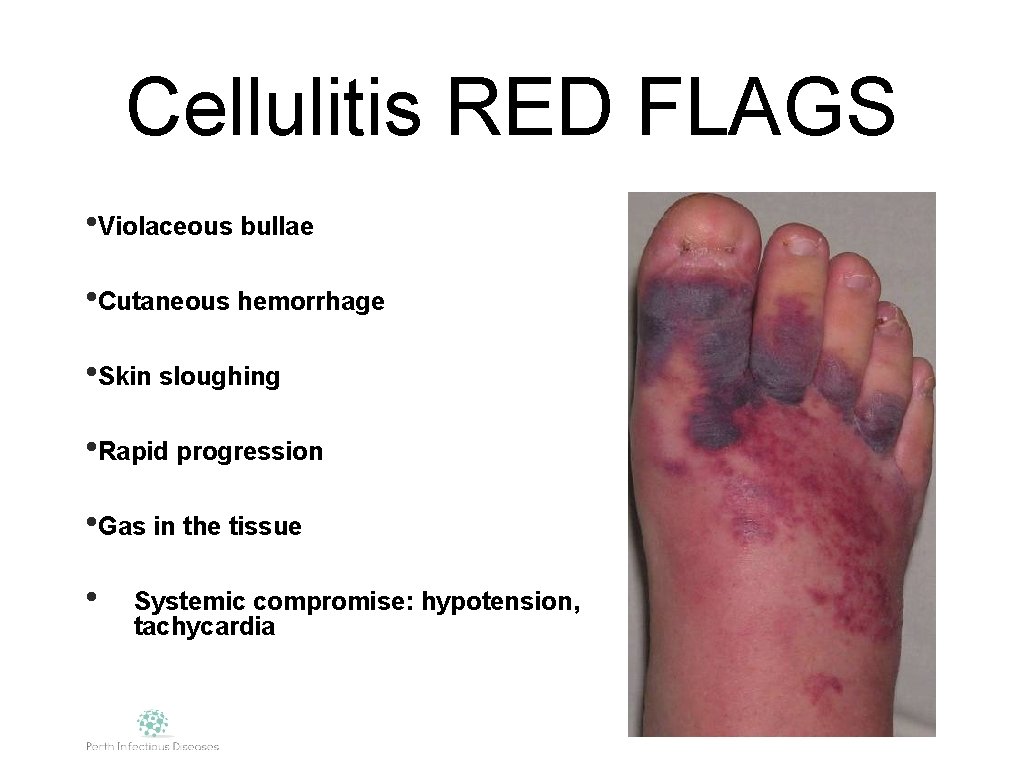
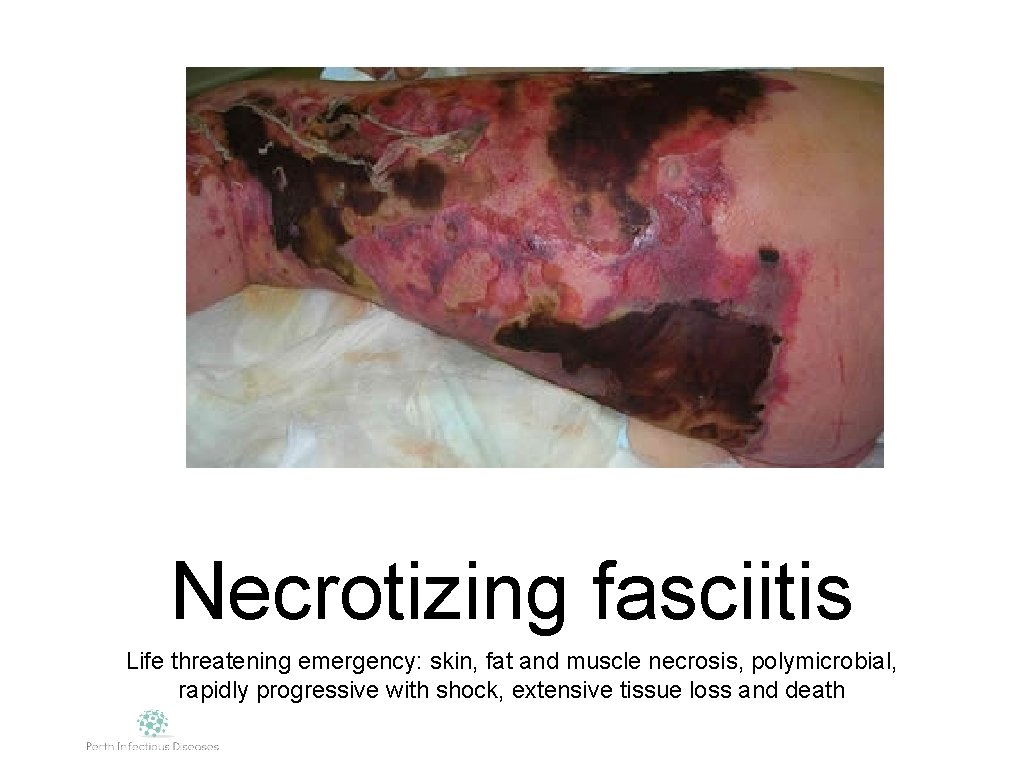
Cellulitis RED FLAGS • Violaceous bullae • Cutaneous hemorrhage • Skin sloughing • Rapid progression • Gas in the tissue • Systemic compromise: hypotension, tachycardia
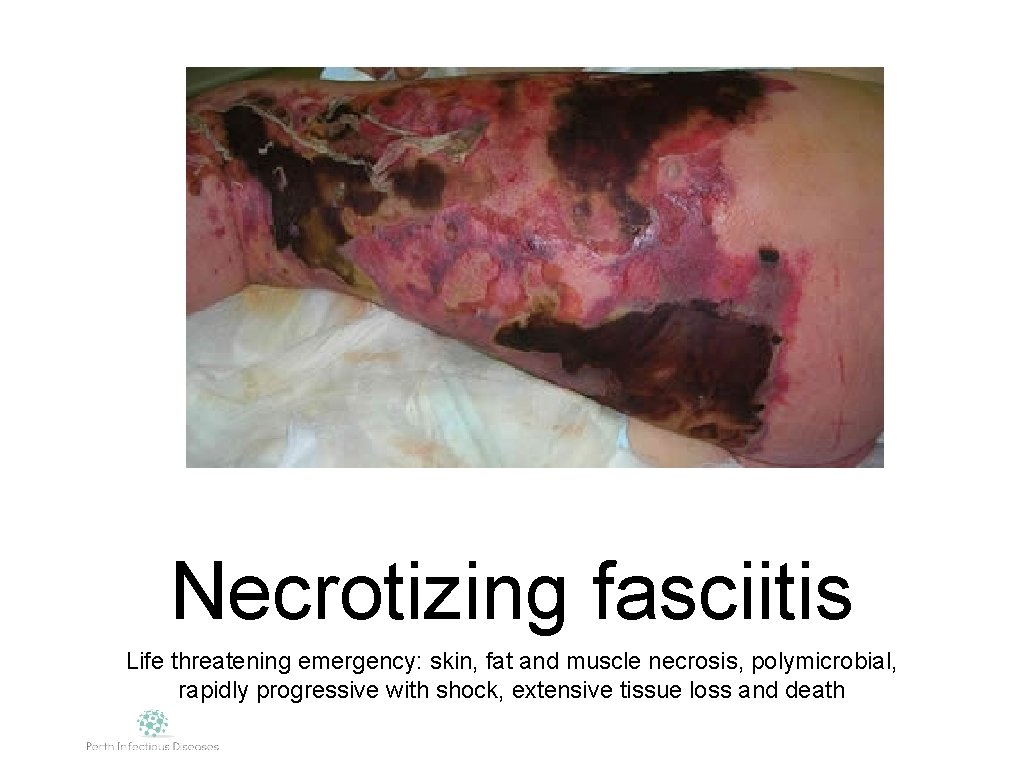
Necrotizing fasciitis Life threatening emergency: skin, fat and muscle necrosis, polymicrobial, rapidly progressive with shock, extensive tissue loss and death
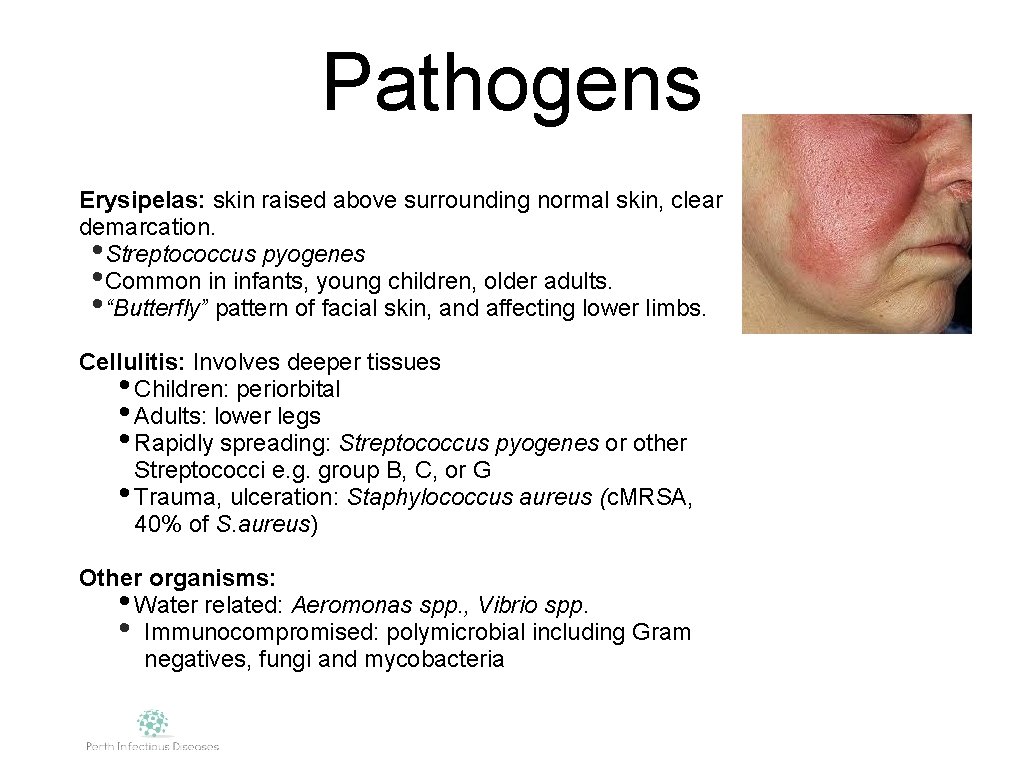
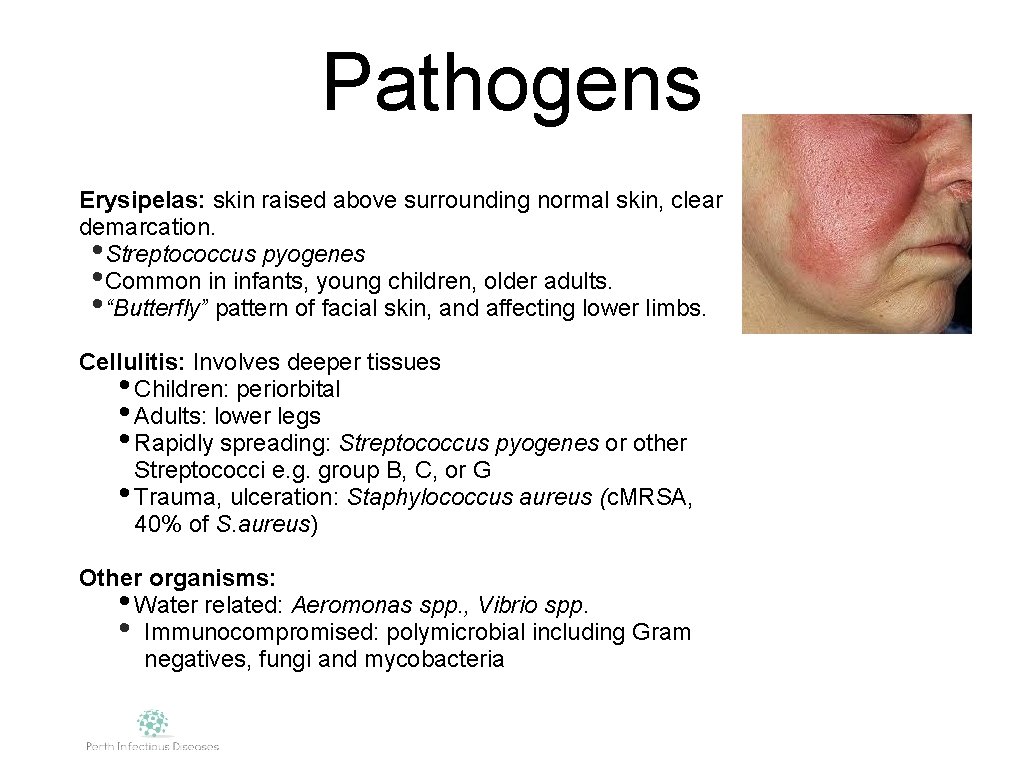
Pathogens Erysipelas: skin raised above surrounding normal skin, clear demarcation. • Streptococcus pyogenes • Common in infants, young children, older adults. • “Butterfly” pattern of facial skin, and affecting lower limbs. Cellulitis: Involves deeper tissues • Children: periorbital • Adults: lower legs • Rapidly spreading: Streptococcus pyogenes or other Streptococci e. g. group B, C, or G • Trauma, ulceration: Staphylococcus aureus (c. MRSA, 40% of S. aureus) Other organisms: • Water related: Aeromonas spp. , Vibrio spp. • Immunocompromised: polymicrobial including Gram negatives, fungi and mycobacteria
Predisposing factors • Damage to skin e. g. trauma, ulcers. • Tinea infection • Fissured dermatitis • Lymphoedema • History of DVT • Vascular surgery • Radiotherapy • Insect bites/scabies
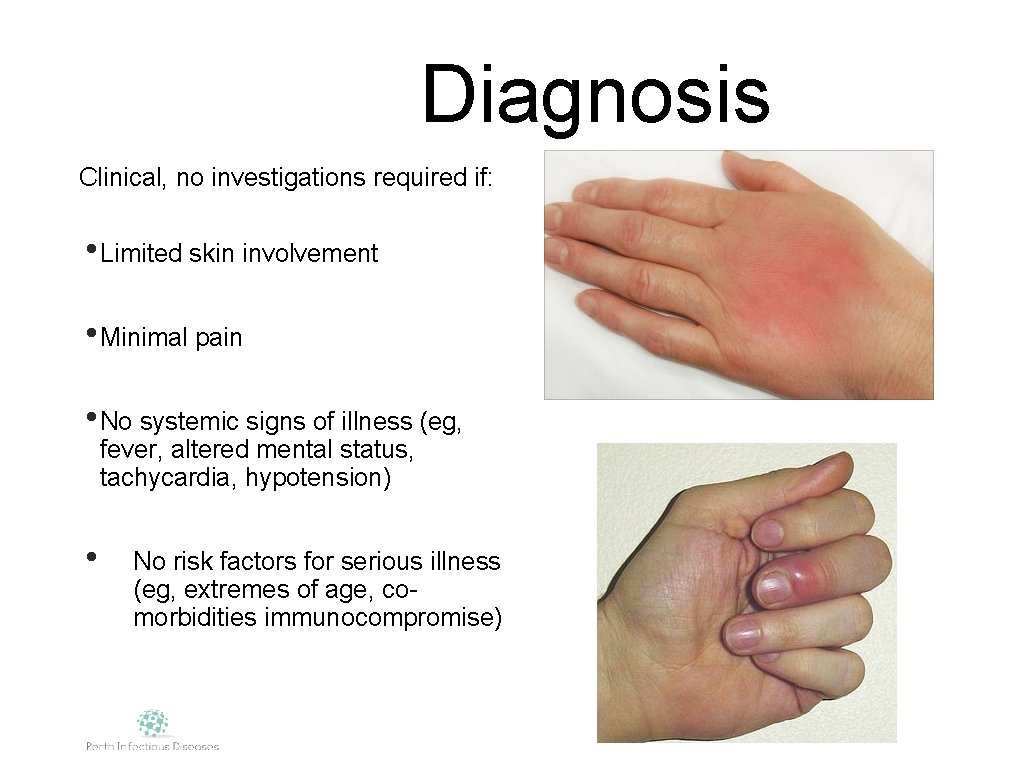
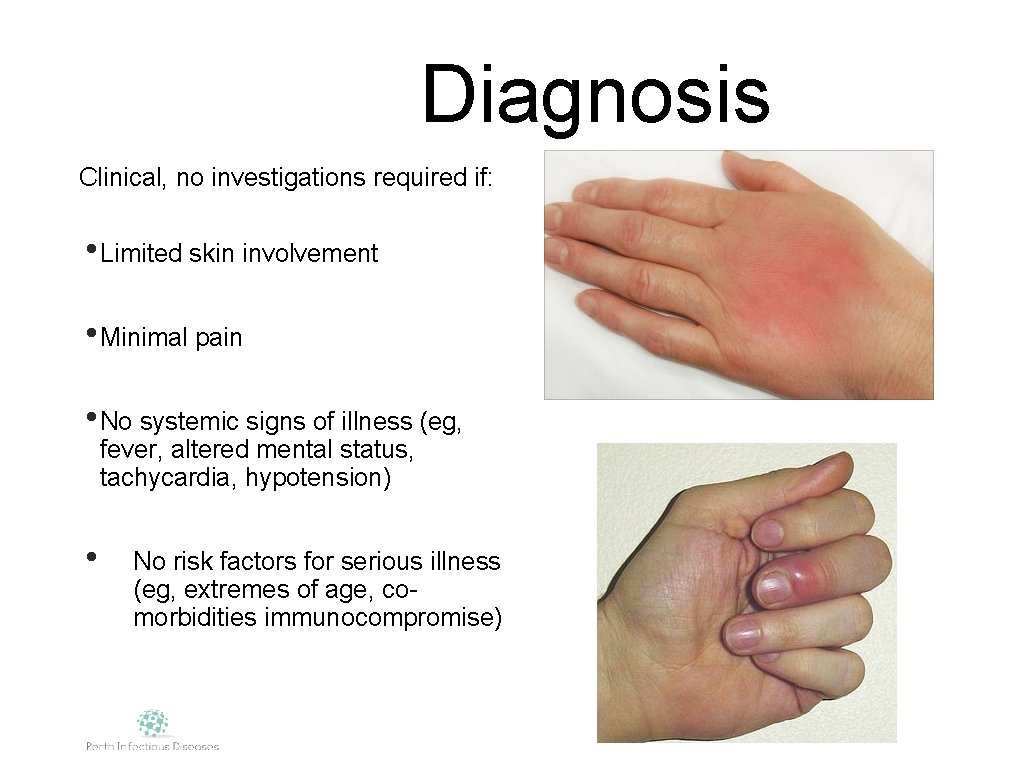
Diagnosis Clinical, no investigations required if: • Limited skin involvement • Minimal pain • No systemic signs of illness (eg, fever, altered mental status, tachycardia, hypotension) • No risk factors for serious illness (eg, extremes of age, comorbidities immunocompromise)
Systemic signs= Investigations • FBP, CRP, U+E • Blood cultures: Moderate to severe disease (cellulitis complicating lymphoedema) • Orbital Cellulitis (fat and eye muscles) and periorbital (eyelid) cellulitis • Patients with malignancy or chemotherapy • Neutropenia or severe cell-mediated immunodeficiency • Animal bites
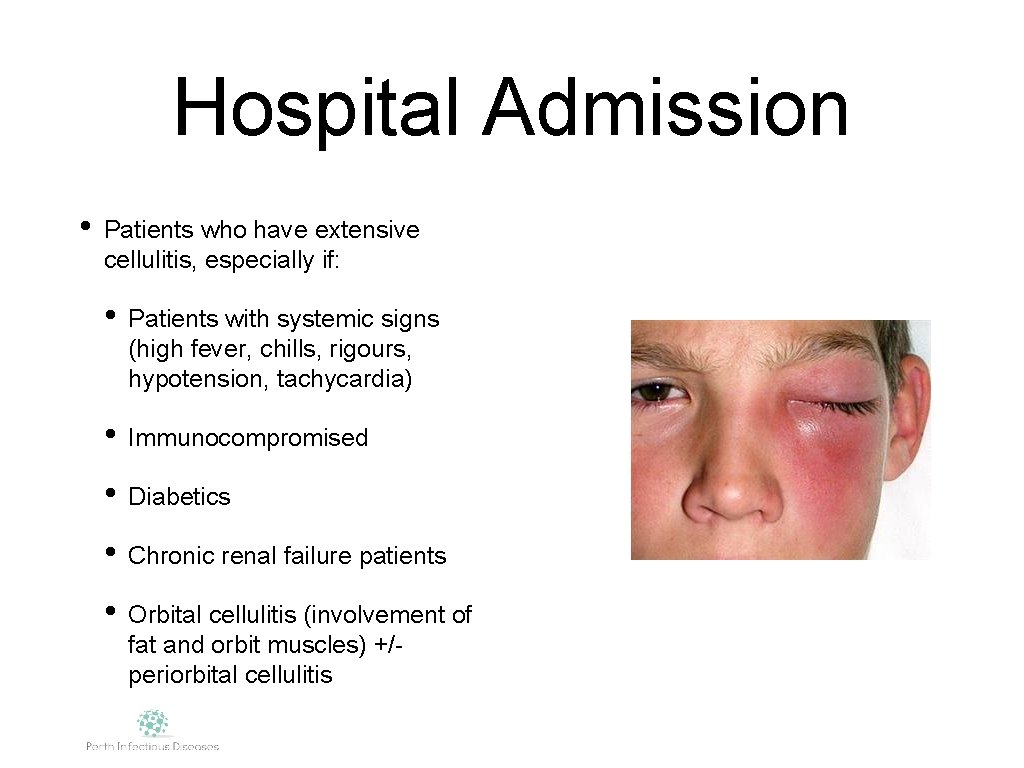
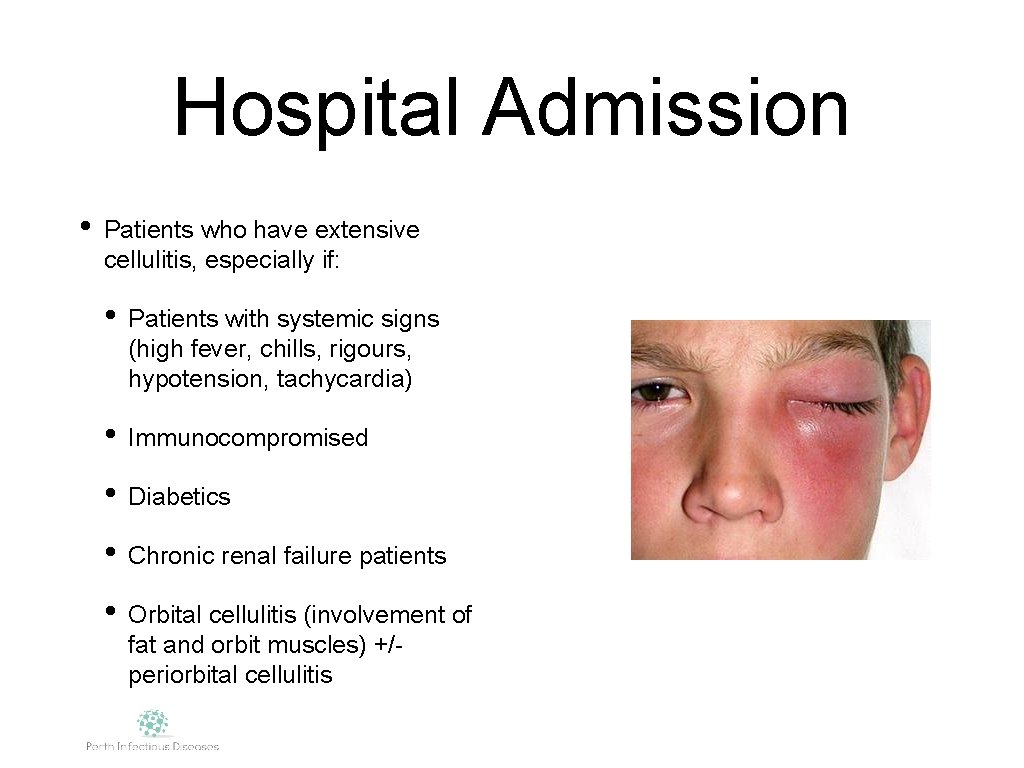
Hospital Admission • Patients who have extensive cellulitis, especially if: • Patients with systemic signs (high fever, chills, rigours, hypotension, tachycardia) • Immunocompromised • Diabetics • Chronic renal failure patients • Orbital cellulitis (involvement of fat and orbit muscles) +/periorbital cellulitis
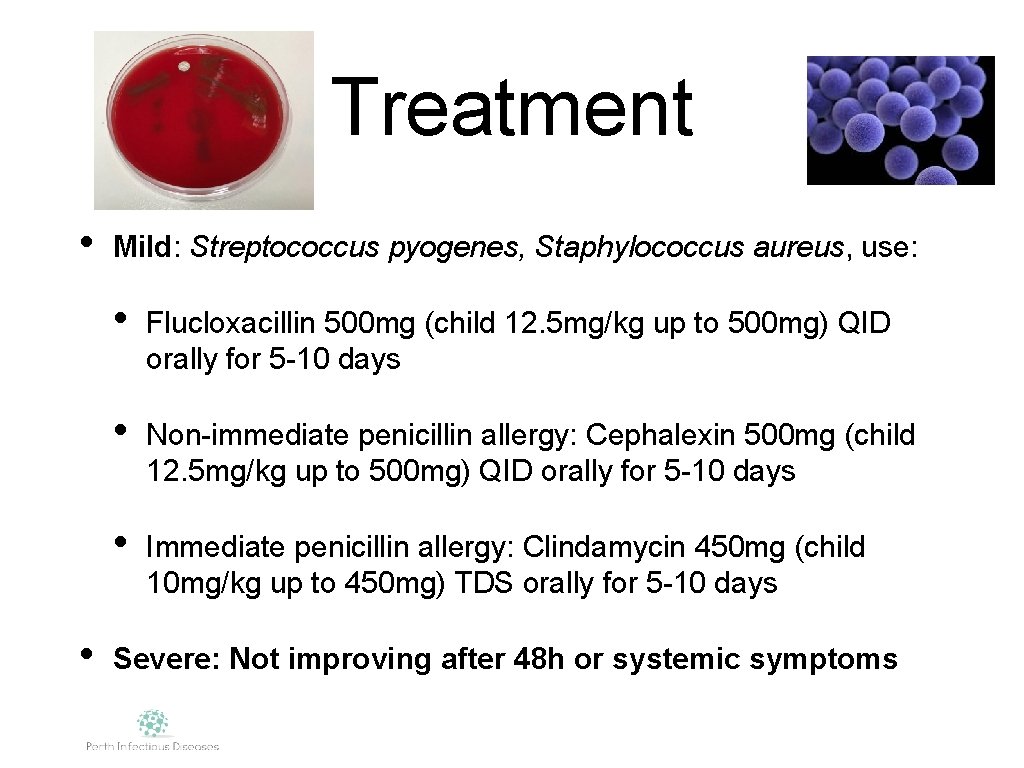
Treatment • • Mild: Streptococcus pyogenes, Staphylococcus aureus, use: • Flucloxacillin 500 mg (child 12. 5 mg/kg up to 500 mg) QID orally for 5 -10 days • Non-immediate penicillin allergy: Cephalexin 500 mg (child 12. 5 mg/kg up to 500 mg) QID orally for 5 -10 days • Immediate penicillin allergy: Clindamycin 450 mg (child 10 mg/kg up to 450 mg) TDS orally for 5 -10 days Severe: Not improving after 48 h or systemic symptoms
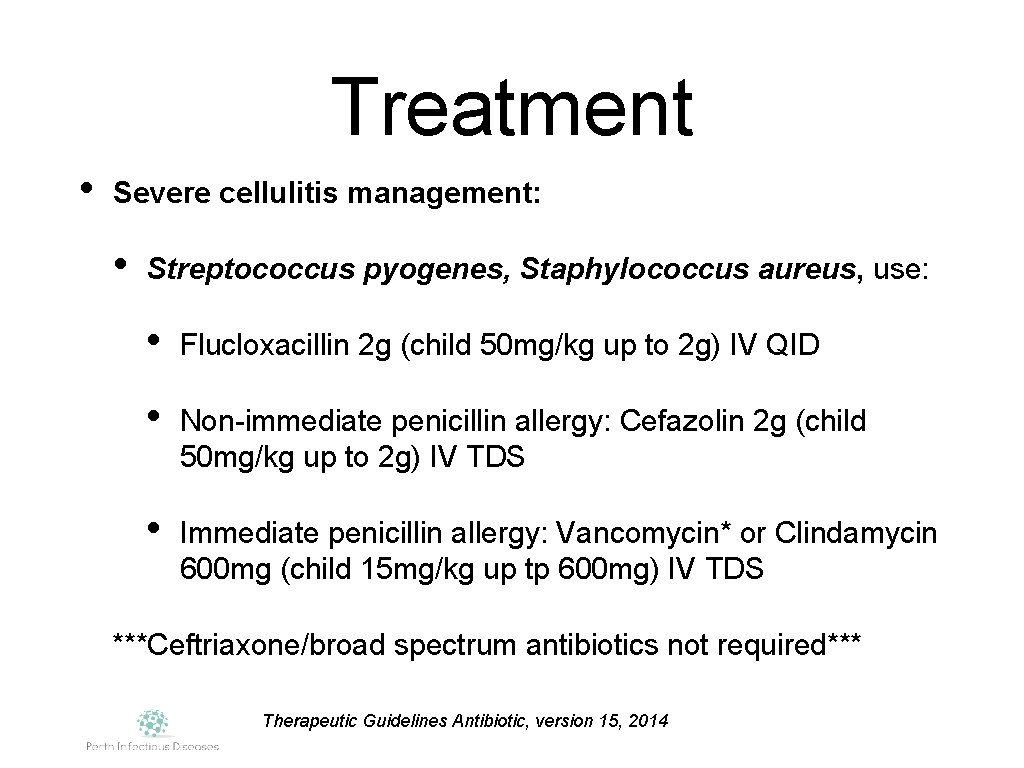
Treatment • Severe cellulitis management: • Streptococcus pyogenes, Staphylococcus aureus, use: • Flucloxacillin 2 g (child 50 mg/kg up to 2 g) IV QID • Non-immediate penicillin allergy: Cefazolin 2 g (child 50 mg/kg up to 2 g) IV TDS • Immediate penicillin allergy: Vancomycin* or Clindamycin 600 mg (child 15 mg/kg up tp 600 mg) IV TDS ***Ceftriaxone/broad spectrum antibiotics not required*** Therapeutic Guidelines Antibiotic, version 15, 2014
Hospital in the Home • Administration of IV antibiotics in outpatient setting where IVABs are required for >1 week • Once stable and select patients (independent, no significant co-morbidities), supported home environment, able to attend clinic reviews and blood testing. • Antibiotic regimen: once daily dosing or infusion • Requires log term IV line: PICC line • Convenient for young/working individuals • Nursing Service: Access via AMU, direct admit for adults • SJOG Subiaco Hospital, ID Physicians and Health Choices Nurses
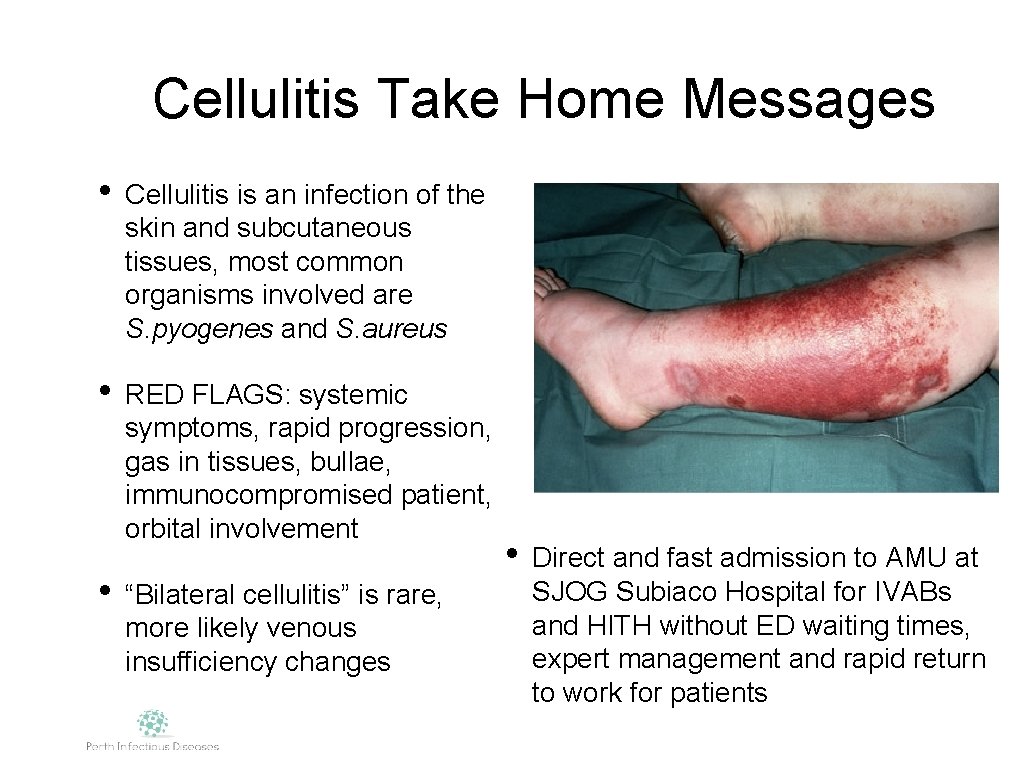
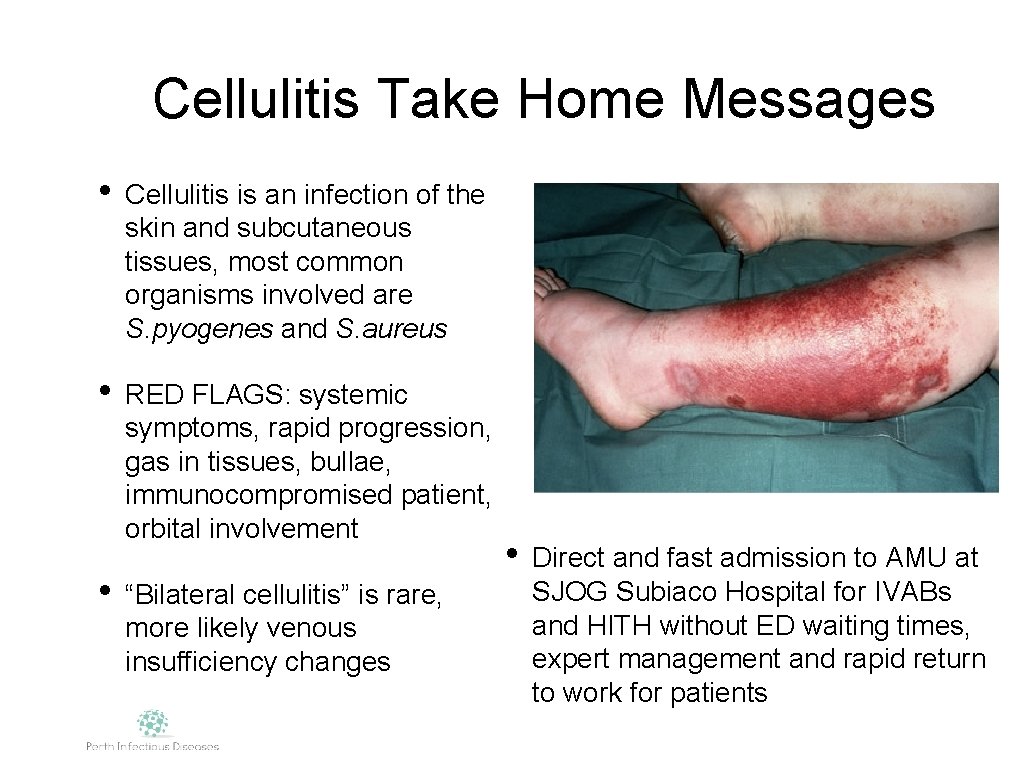
Cellulitis Take Home Messages • Cellulitis is an infection of the skin and subcutaneous tissues, most common organisms involved are S. pyogenes and S. aureus • RED FLAGS: systemic symptoms, rapid progression, gas in tissues, bullae, immunocompromised patient, orbital involvement • “Bilateral cellulitis” is rare, more likely venous insufficiency changes • Direct and fast admission to AMU at SJOG Subiaco Hospital for IVABs and HITH without ED waiting times, expert management and rapid return to work for patients
 Treatment of orbital cellulitis
Treatment of orbital cellulitis Cellulitis nose
Cellulitis nose Preseptal cellulitis
Preseptal cellulitis Conjunctival swelling
Conjunctival swelling Preseptal cellulitis
Preseptal cellulitis Cellulitis
Cellulitis Carbuncle
Carbuncle Lll cellulitis
Lll cellulitis Cellulitis vs abscess
Cellulitis vs abscess Auricle cellulitis
Auricle cellulitis Wilmer arellano fiu
Wilmer arellano fiu Wilmer arellano fiu
Wilmer arellano fiu Arduino pitches.h library
Arduino pitches.h library Wilmer arellano fiu
Wilmer arellano fiu Codigo hsi yuan lu
Codigo hsi yuan lu Arellano bond
Arellano bond Wilmer arellano
Wilmer arellano Wilmer arellano
Wilmer arellano